Abstract
Wandering spleen is a rare clinical entity characterized by splenic hypermobility resulting from laxity or maldevelopment of the suspensory splenic ligaments. The spleen can “wander” or migrate into various positions within the abdomen or pelvis due to this ligamentous laxity. It is usually detected between 20 and 40 years of age, and is more common in women. The clinical presentation of a wandering spleen is variable, it could present as an asymptomatic, incidentally detected, abdominal or pelvic mass, or as an acute abdomen secondary to splenic torsion. Diagnosis in an emergent setting can be challenging as it is a rare cause of acute abdomen and does not produce any symptoms until splenic torsion has occurred. We present and discuss a case of ectopic, torsed spleen resulting in complete infarction of the spleen and severe hepatic vascular compromise, diagnosed by ultrasound, confirmed by computed tomography and effectively managed by splenectomy.
Keywords: Wandering spleen, Ectopic spleen, Torsion, Infarction, Acute abdomen, Ultrasound, Computed tomography
CASE REPORT
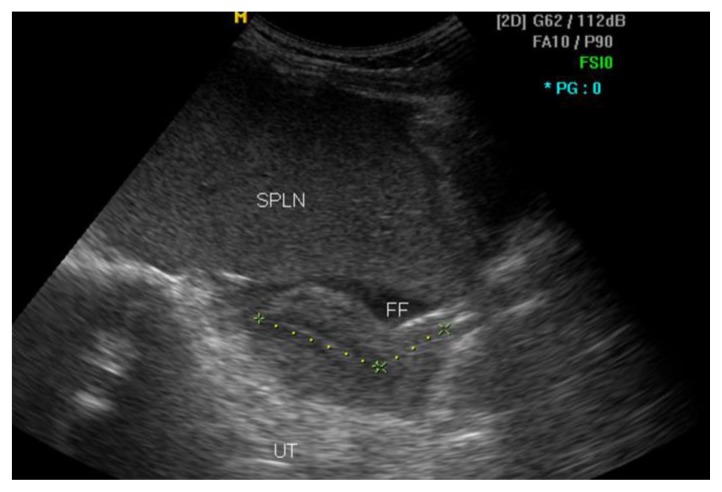
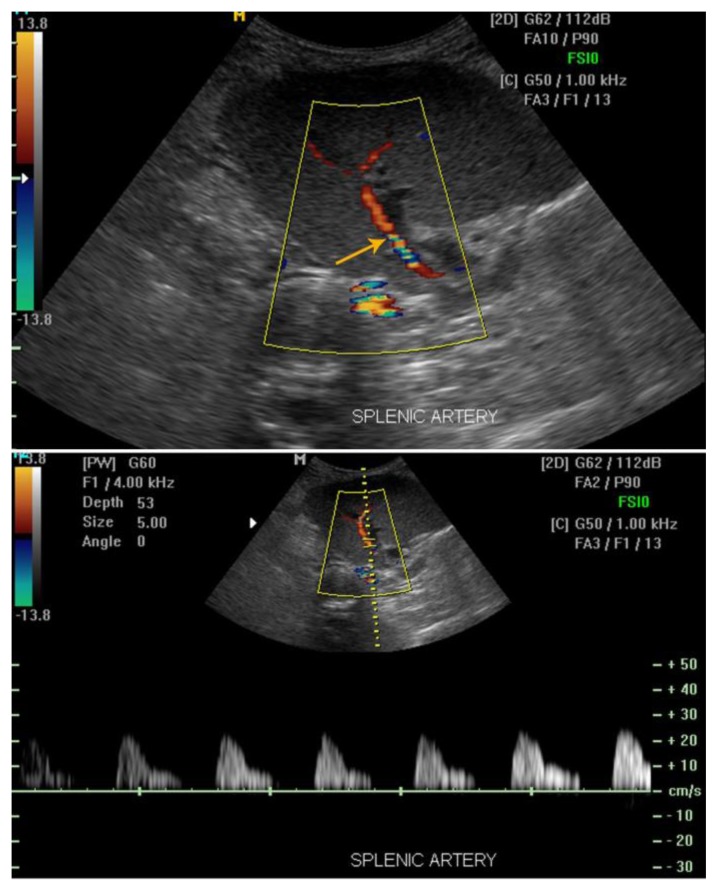
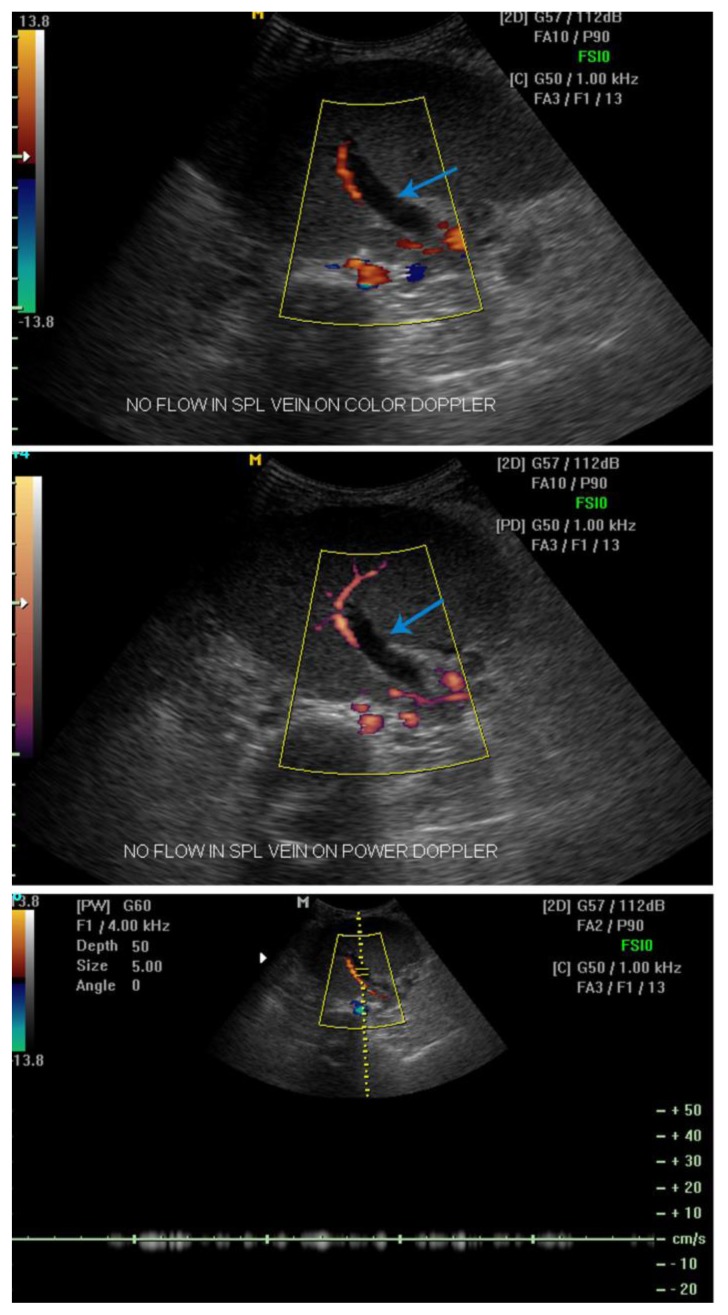
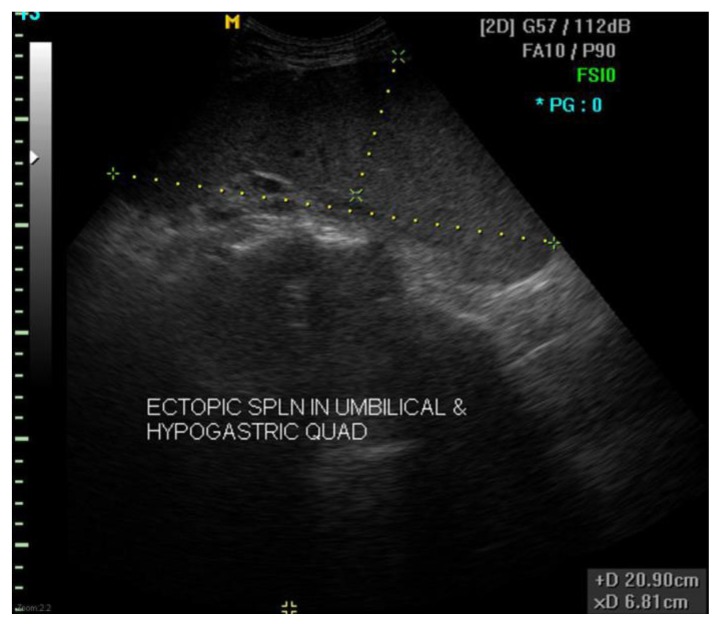
A 29 year old woman presented to our emergency unit with intermittent, low grade abdominal pain for 2 weeks which worsened in the last 3 days, the pain was poorly localized around the periumbilical and left lower quadrant of the abdomen, was non-colicky and non-radiating in nature. Her past history did not reveal any predisposing factors to thrombosis; she was a non-smoker with no history of oral contraceptive use, blood disorders or recent travelling. However, she did give history of a similar vague, recurrent lower abdominal pain 2 years ago. On physical examination, her body temperature was 38°C, heart rate 85 beats/min, and blood pressure 120/70 mmHg. On palpation, there was diffuse guarding in the abdomen with no rebound tenderness. A firm, tender mass was palpable in the left lower abdomen. Routine biochemical parameters were normal except for mild leukocytosis (15,000/mm3) and anemia (hemoglobin 9.7 g/dL). Urinary analysis was normal. During ultrasonography, spleen was not located in the left hypochondrium, it was found in the lower abdomen and pelvis, to the left of the midline, in close proximity of the urinary bladder and uterus with its hilum oriented laterally towards the right side [fig 1]. The spleen was enlarged, reaching 21cm along its longitudinal axis. It was diffusely hypoechoic with altered echotexture suggesting vascular congestion. Color doppler imaging (CDI) with spectral analysis revealed normal color flow in splenic artery with spectral waveform showing diminished diastolic flow [fig 2a,b]. The splenic vein showed no flow on color, power doppler & spectral imaging [fig 3a,b,c]. Minimal free fluid was present in the pelvis [Fig 1]. Based on the US findings, a diagnosis of ectopic spleen, with venous occlusion secondary to torsion was made.
Figure 1.
29 yr old female patient with ectopic, torsed & infarcted spleen. Sagittal US image shows the ectopic spleen in lower abdomen and pelvis, just superior to urinary bladder. It was diffusely hypoechoic with altered echotexture and its hilum facing right laterally. Minimal surrounding free fluid (FF) was present.
(GE Logiq 200 PRO, 3.5 MHz abdominal curved array transducer )
Figure 2.
29 yr old female patient with ectopic, torsed & infarcted spleen. (2a) Splenic artery (yellow arrow) has normal color flow but (2b) abnormal spectral waveform with diminished diastolic flow.
(GE Logiq 200 PRO, 3.5 MHz abdominal curved array transducer )
Figure 3.
29 yr old female patient with ectopic, torsed & infarcted spleen. (3a,b,c). No flow is seen within the splenic vein (blue arrow) on spectral Doppler. Note, some Doppler noise is noted without appreciable Doppler color flow or spectral wave pattern.
(GE Logiq 200 PRO, 3.5 MHz abdominal curved array transducer )
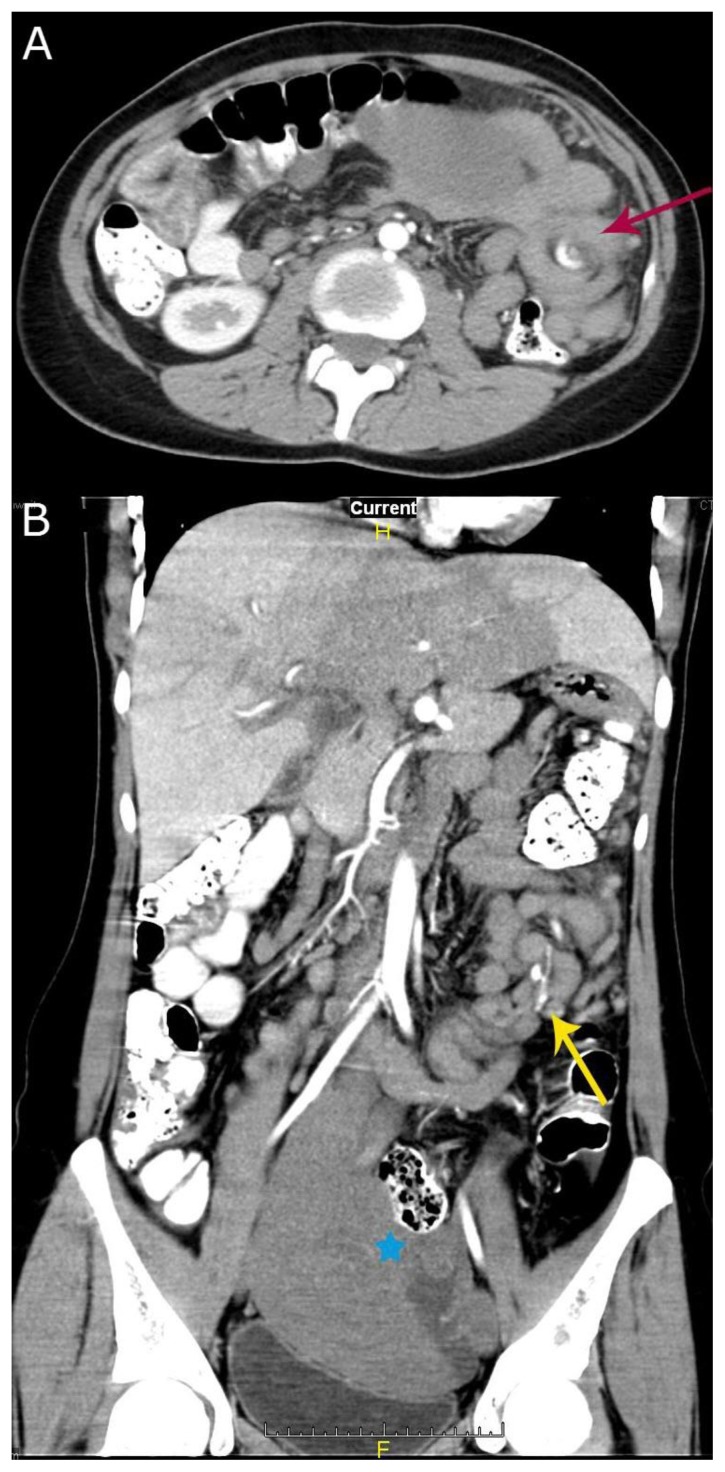
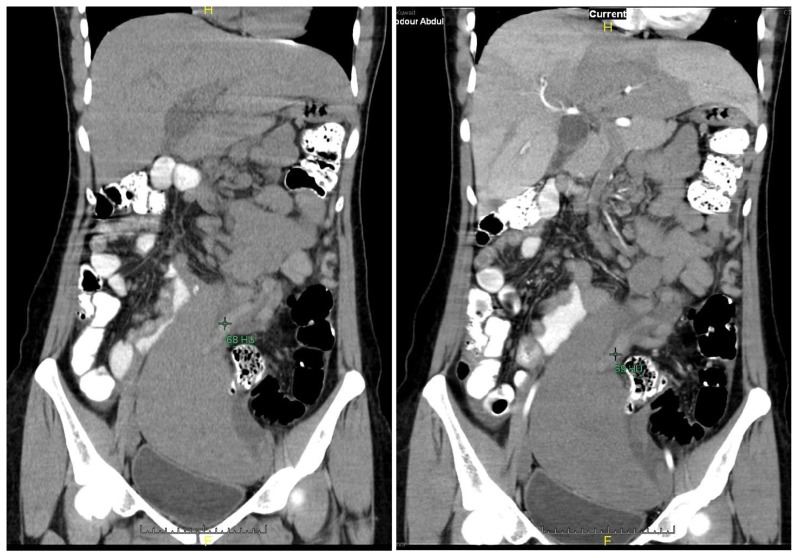
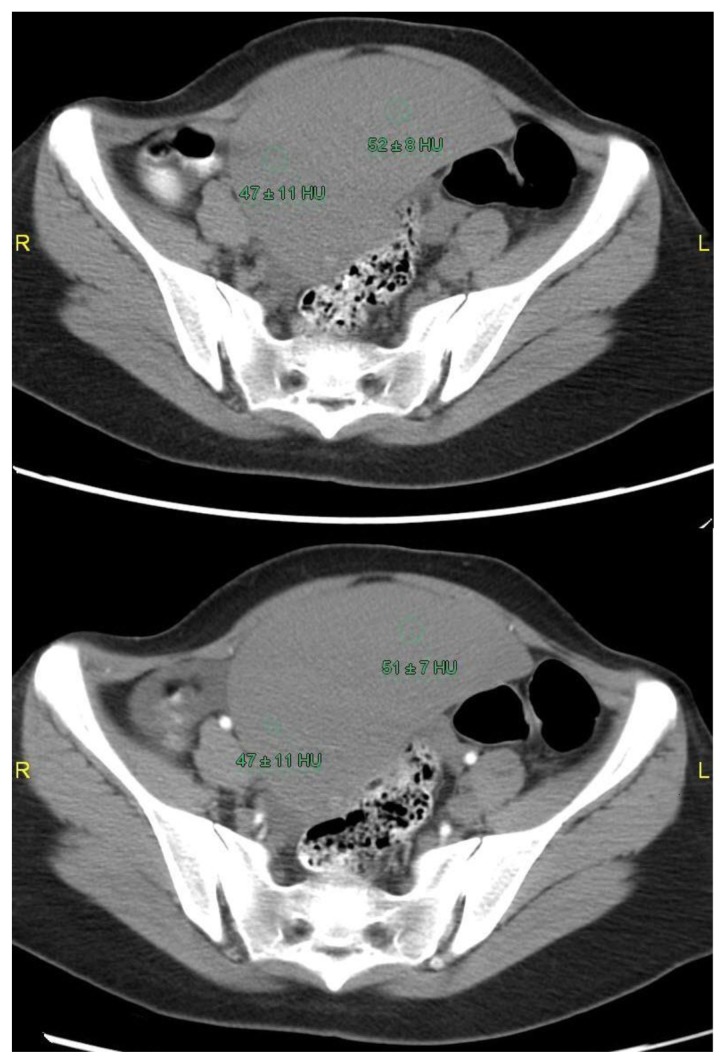
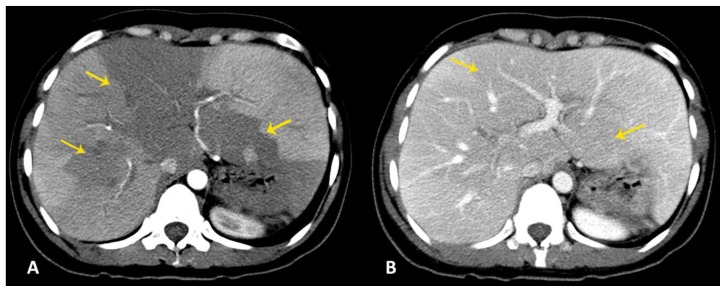
Contrast enhanced Computed Tomography (CT) of the abdomen and pelvis was performed 6 hours later to evaluate the splenic pedicle and parenchyma. CT also revealed the enlarged, ectopic spleen in the lower abdomen and pelvis, displacing adjacent bowel loops and indenting the superior surface of the urinary bladder [fig 4b]. The splenic vascular pedicle had a classic whorled appearance in the axial images, it had twisted five times by 1800 degrees [fig 4a,b]. The hilum was now oriented in the left lateral plane instead of right lateral secondary to a 180 degree twisting or untwisting in the interim [figs 5,4b]. The splenic vein was dilated and hyperattenuating on non-contrast CT, and showed with no enhancement on post contrast imaging [fig 6a,b] representing thrombosis due to vascular stasis resulting from torsion. The splenic parenchyma also showed no enhancement following contrast administration except for capsular rim enhancement, denoting total splenic infarction [fig 7a,b]. The liver had large areas of hypoattenuation in the right & left lobes [fig 8a,b], denoting abnormal hepatic perfusion secondary to compromised portal venous supply resulting from torsion of the splenoportal confluence. Small filling defects (thrombosis) were noted in the segmental branches of the right & left portal veins (Fig 9). Due to the CT findings of extensive twisting of the splenic vascular pedicle and complete splenic infarction, the patient was managed surgically and she underwent splenectomy.
Figure 4.
29 yr old female patient with ectopic, torsed & infarcted spleen. (a). Axial post contrast CT scan in the arterial phase shows classic whorled appearance of twisted splenic vascular pedicle (red arrow) in the axial image, containing engorged non-enhanced splenic vein and enhanced splenic artery. (b) Coronal reconstructed CT image in the arterial phase shows multiple (five) twists of the splenic vascular pedicle, the splenic hilum (blue asterix) is facing left laterally.
(Siemens SOMATOM Definition Flash, kVp 120, mA 772, 5 mm slice thickness, Pitch 1.375:1, 100 cc of Visipaque 320 IV, 900ml diluted gastrograffin Orally, in arterial phase)
Figure 5.
29 yr old female patient with ectopic, torsed & infarcted spleen. Sagittal ultrasound image in left lower abdomen shows the ectopic, enlarged spleen with the splenic hilum facing right laterally.
(GE Logiq 200 PRO, 3.5 MHz abdominal curved array transducer )
Figure 6.
29 yr old female patient with ectopic, torsed & infarcted spleen. (a). Coronal reformatted non-enhanced CT image shows dilated, hyperdense (68HU), thrombosed splenic vein. (b). Coronal reformatted post contrast CT image shows no significant change in the CT HU of the splenic vein confirming its thrombosis.
(Siemens SOMATOM Definition Flash, kVp 120, mA 772, 5 mm slice thickness, Pitch 1.375:1, 100 cc of Visipaque 320 IV, 900ml diluted gastrograffin Orally, in precontrast & arterial phase)
Figure 7.
29 yr old female patient with ectopic, torsed & infarcted spleen. (a) Pre and (b) post contrast axial CT images show no definite change in the attenuation of the splenic parenchyma denoting complete infarction. Enhancing rim of the splenic capsule is seen.
(Siemens SOMATOM Definition Flash, kVp 120, mA 772, 5 mm slice thickness, Pitch 1.375:1, 100 cc of Visipaque 320 IV, 900ml diluted gastrograffin Orally, in precontrast & arterial phase)
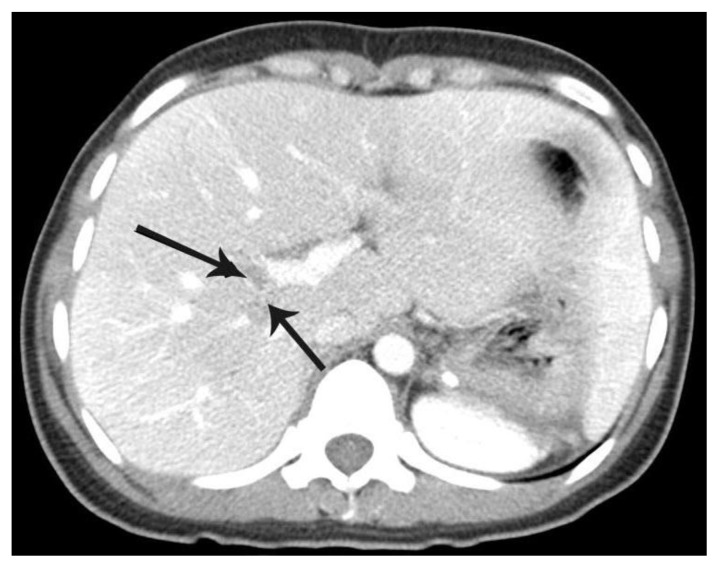
Figure 8.
29 yr old female patient with ectopic, torsed & infarcted spleen. (a) Axial CT image shows large areas of hypoattenuation in the liver (yellow arrows), more pronounced in the arterial phase than (b) portovenous phase, denoting abnormal hepatic perfusion secondary to compromised portal venous supply resulting from torsion of the splenoportal confluence. (Siemens SOMATOM Definition Flash, kVp 120, mA 772, 5 mm slice thickness, Pitch 1.375:1, 100 cc of Visipaque 320 IV, 900ml diluted gastrograffin Orally, in arterial & portovenous phase)
Figure 9.
29 yr old female patient with ectopic, torsed & infarcted spleen. Axial CT image in the porto-venous phase, at the level of branching of main portal trunk, showing filling defects at the bifurcation of the right portal vein (black arrows) denoting thrombosis.
(Siemens SOMATOM Definition Flash, kVp 120, mA 772, 5 mm slice thickness, Pitch 1.375:1, 100 cc of Visipaque 320 IV, 900ml diluted gastrograffin Orally, in portovenous phase)
Imaging findings were confirmed during laparotomy and revealed an infarcted spleen with a long (about 40 cm), twisted pedicle causing venous outflow obstruction. The splenic artery was patent and pulsatile. Following splenectomy, her postoperative course was uneventful.
DISCUSSION
Etiology & demographics
Wandering or ectopic spleen is very uncommon. Its true incidence remains unknown, with studies reporting a 0.5% incidence in splenectomies and only under 500 cases documented in published literature [1,2]. It can be congenital or acquired. It is fifteen times more common in females, usually detected between 20 and 40 years of age [12,13]. Children comprise one-third of all cases [13]. If symptomatic in childhood, it is more common in males.
The spleen is held in its normal position by the gastrosplenic, splenorenal, splenocolic and phrenocolic ligaments [3]. The congenital or acquired laxity of these peritoneal attachments of the spleen results in splenic hypermobility, leading to a wandering or ectopic spleen [1,7–9]. Embryologic basis of congenital laxity is incomplete fusion of dorsal mesogastrium with the peritoneum overlying the left kidney [10]. Multiparity, hormonal effects of pregnancy leading to laxity of ligaments & abdominal wall, trauma and splenomegaly are some of the proposed causes of acquired increase in splenic mobility [1,9,11,3].
Clinical & imaging findings
The ectopic spleen may be normal in size or enlarged. It usually comes to medical attention as a palpable abdominal mass or when the spleen undergoes torsion [14]. Patients with wandering spleen complicated by torsion of its pedicle may have acute, chronic or intermittent symptoms. The presenting symptoms depend on the degree of torsion, which can range from 90 to 2160 degrees (1/4 to 12 twists) [10]. Chronic or intermittent milder degrees of torsion merely causes vascular congestion and splenomegaly [13]. Splenic infarction with possible involvement of related viscera can occur with multiple twists. Acute torsion presents as an acute abdomen and may be confused with the far more common appendicitis, ovarian torsion, ruptured ectopic or diverticulitis. Pain is due to stretching of the splenic capsule and local peritonitis [11]. Intermittent and less severe abdominal pain results from recurrent torsion and spontaneous detorsion. The correct and early diagnosis of wandering spleen is important because of catastrophic complications such as infarction, gangrene, splenic abscess and pancreatic necrosis [13]. Reported complications of ectopic spleen range from splenic congestion to torsion, infarction, injury to adjacent organs secondary to torsion (gastric volvulus, gastrointestinal obstruction, celiac axis occlusion, acute pancreatitis, pancreatic necrosis) and traumatic rupture due to loss of ribcage protection in lower abdomen & pelvis [3,4, 5, 6].
Clinical diagnosis is difficult. The hematological and biochemical investigations are usually non-specific. Non-invasive imaging procedures such as Ultrasound (US), CT and Magnetic resonance imaging (MRI) are diagnostic [1,15]. Plain abdominal radiographs and barium studies are nonspecific. Although scintigraphy can localize the ectopic spleen, it is expensive and not widely available [16,4]. Angiography can also localize the ectopic spleen and diagnose splenic torsion, but is invasive and not essential for diagnostic purposes. The precise preoperative diagnosis can be established by US and CT [17]. US demonstrates the absence of splenic tissue in left upper quadrant and localizes its ectopic position. Doppler sonography of the splenic parenchyma and vessels can be used to evaluate their flow status [18]. Infarcted spleen however, can appear normal or have an altered echotexture or appear hyperechoic by US [19]. The drawbacks of US include limitation by bowel gas, difficulty in demonstrating the twisted pedicle, the varied appearances of splenic infarction and inability to accurately assess status of adjacent viscera. CT overcomes these deficiencies. Splenic vessels and surrounding fat in a whorled appearance by CT indicates torsion [7,20]. If torsion is complicated by infarction, CT shows partially or completely unenhanced spleen. In chronic torsion, a thick pseudocapsule can be observed [18]. CT also demonstrates secondary findings, such as ascites and entrapment of adjoining viscera secondary to torsion.
In our case, the patient presented with abdominal pain due to extensive splenic torsion. B-mode & doppler US diagnosed the ectopic, torsed spleen. The splenic infarctions were not evident by sonography. Contrast-enhanced CT gave detailed pre-operative information regarding degree of torsion and non-viable spleen. Additionally, in our patient, the change in direction of splenic hilum in the CT images when compared to the US study, within a span of few hours, highlights the dynamic intrabdominal torsing/detorsing capacity of such an enlarged organ. To our knowledge, the imaging findings of abnormal hepatic perfusion secondary to severe hepatic vascular compromise, have not been depicted in previously published literature. While US is diagnostic, CT is required for complete evaluation in a patient having ectopic spleen complicated by torsion. It is invaluable in deciding the further course of management in these patients, whether splenopexy or splenectomy.
Treatment & prognosis
Incidentally detected ectopic spleen, regardless of the patient’s age, is managed by splenopexy [21]. Splenic infarction following torsion is treated by splenectomy [22,23]. In the pediatric age group, due to the physiological importance of spleen and to avoid the dreaded complication of post splenectomy sepsis, an early diagnosis in ectopic torsed spleen is preferred, before the onset of infarction [3,24].
To summarize, patients with torsion of wandering spleen can present with symptoms ranging from acute to subacute or chronic. This was a case of extensively torsed, completely infarcted ectopic spleen associated with extensive hepatic vascular compromise, presenting as an acute abdomen. US is diagnostic, however CT is mandatory for preoperative assessment of this rare condition. In spite of its uncommon prevalence, wandering spleen must be kept in mind as a differential in young adult females of reproductive age group age presenting with pelvic mass or pain.
TEACHING POINT
Congenital or acquired laxity of peritoneal attachments of the spleen results in splenic hypermobility. CT is invaluable prior to surgical intervention to detect potential complications like torsion & infarction. Incidentally detected ectopic spleen, regardless of the patient’s age, is managed by Splenopexy. Splenic infarction following torsion is treated by splenectomy.
Table 1.
Summary table of wandering or ectopic spleen
| Etiology | Congenital or acquired laxity of the suspensory splenic peritoneal ligaments. |
| Incidence | 0.5% incidence in splenectomies. Only under 500 cases documented in published literature |
| Gender ratio | In children : M>F In adults: F>M |
| Age predilection | Females in reproductive age group ( 20 to 40 yrs) |
| Risk factors | In acquired cases: Multiparty, Trauma, Splenomegaly |
| Treatment | Splenopexy or splenectomy |
| Prognosis | Good prognosis if diagnosed promptly with early surgical intervention. |
| Complications | Torsion +/− Infarction of ectopic spleen, Rupture of ectopic spleen following trauma, injury to adjoining organs secondary to torsion (gastric volvulus, gastrointestinal obstruction, celiac axis occlusion, acute pancreatitis, pancreatic necrosis). |
| Imaging Findings | X-ray:
|
US:
| |
CT :
| |
MRI
| |
Angiography
| |
Scintigraphy
|
Table 2.
Differential diagnosis table of wandering spleen
| Differential Diagnosis | US | CT | MRI |
|---|---|---|---|
| Ectopic spleen |
|
|
|
| Appendicitis |
|
Inflamed appendix visualized +/− appendicolith. | Inflamed, dilated appendix with wall edema (T1 hypointense, T2 hyperintense) & appendicoliths (T1 & T2 hypointense). |
| Ovarian mass/cyst |
|
Ovary not visualized separately from the mass or cyst. | Best imaging modality to characterize ovarian masses/cysts. |
| Diverticulitis |
|
Diverticula easily detected in the colon. Inflamed diverticula with surrounding fat stranding or abscess formation seen. | Inflamed diverticula seen as T2 hypointense outpouching from the colonic wall. |
| Ruptured ectopic pregnancy |
|
|
|
ABBREVIATIONS
- CDI
Color Doppler Imaging
- CT
Computed Tomography
- FF
Free fluid
- HU
Hounsfield units
- MRI
Magnetic Resonance Imaging
- US
Ultrasound
REFERENCES
- 1.Gayer G, Zissin R, Apter S. CT findings in congenital anomalies of the spleen. Br J Radiol. 2001;74:767–772. doi: 10.1259/bjr.74.884.740767. [DOI] [PubMed] [Google Scholar]
- 2.Kinori I, Rifkin MD. A truly wandering spleen. J Ultrasound Med. 1988;7(2):101–5. doi: 10.7863/jum.1988.7.2.101. [DOI] [PubMed] [Google Scholar]
- 3.Zarrintan S, Jamali F, Tubbs RS, et al. wandering spleen presenting as a pelvic mass: case report and review of the literature. Folia Morphol. 2207;66:152–154. [PubMed] [Google Scholar]
- 4.Lin CH, Wu SF, Lin WC, et al. Wandering spleen with torsion and gastric volvulus. J Formos Med Assoc. 2005;104:755–758. [PubMed] [Google Scholar]
- 5.Rosin D, Bank I, Gayer G. Laproscopic splenectomy for torsion of wandering spleen associated with celiax axis occlusion. Surg Endosc. 2002;16:1110. doi: 10.1007/s00464-001-0078-3. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez R, Lobert P, Herman R. Wandering spleen causing gastric outlet obstruction and pancreatitis. Pediatr Radiol. 2010;40(Suppl 1):S89–S91. doi: 10.1007/s00247-010-1756-x. [DOI] [PubMed] [Google Scholar]
- 7.Swischuk LE, Williams JB, John SD. Torsion of wandering spleen: the whorled appearance of the pedicle on CT. Pediatr Radiol. 1993;23:476–477. doi: 10.1007/BF02012458. [DOI] [PubMed] [Google Scholar]
- 8.Larsen WJ. Development of the gastrointestinal tract. In: Larsen WJ, editor. Human Embryology. 2nd ed. New York, NY: Churchill Livingstone; 1997. pp. 229–259. [Google Scholar]
- 9.Yakan S, Telciler KE, Denecli AG. Acute torsion of a wandering spleen causing acute abdomen. Hong Kong J Emerg Med. 2011;18:34–36. [Google Scholar]
- 10.Herman TE, Siegel MJ. CT of acute splenic torsion in children with wandering spleen. AJR Am J Roentgenol. 1991;156:151–153. doi: 10.2214/ajr.156.1.1898552. [DOI] [PubMed] [Google Scholar]
- 11.Peitgen K, Schweden K. Management of intermittent splenic torsion (“wandering spleen”): a review. Eur J Surg. 1995;161:49–52. [PubMed] [Google Scholar]
- 12.Sayeed S, Koniaris LG, Kovach SJ, Hirokawa T. Torsion of a wandering spleen. Surgery. 2002 Sep;132(3):535–536. doi: 10.1067/msy.2002.119494. [DOI] [PubMed] [Google Scholar]
- 13.Desai DC, Hebra A, Davidoff AM, Schnaufer L. Wandering spleen: a challenging diagnosis. South Med J. 1997;90:439–443. doi: 10.1097/00007611-199704000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Soleimani M, Mehrabi A, Kashfi A, Fonouni H, Buchler MW, Kraus TW. Surgical treatment of patients with wandering spleen: report of six cases with a review of the literature. Surg Today. 2007;37(3):261–269. doi: 10.1007/s00595-006-3389-0. [DOI] [PubMed] [Google Scholar]
- 15.Deux Jean-François, Salomon Laurent, Barrier Alain, et al. Acute Torsion of Wandering Spleen: MRI Findings. AJR. 2004;182:1607–1608. doi: 10.2214/ajr.182.6.1821607. [DOI] [PubMed] [Google Scholar]
- 16.Baykara M, Karahan OI, Coskun A. Case report: acute abdomen and pelvic mass due to torsion of wandering spleen [in Turkish] Tani Girisim Radyol. 2003;9:105–107. [PubMed] [Google Scholar]
- 17.Bakir B, Poyanli A, Yekeler E. Acute torsion of wandering spleen: imaging findings. Abdom Imaging. 2004;29:707–709. doi: 10.1007/s00261-004-0174-7. [DOI] [PubMed] [Google Scholar]
- 18.Arda K, Kizilkanat K, Celik M, et al. Intermittent torsion of a wandering spleen in a child: the role of MRI in diagnosis. JBR-BTR. 2004;87:70–72. [PubMed] [Google Scholar]
- 19.Danaci M, Belet UM, Yalin TR, et al. Power Doppler Sonographic Diagnosis of Torsion in a Wandering Spleen. Journal of clinical ultrasound. 2000;28(5):246–248. doi: 10.1002/(sici)1097-0096(200006)28:5<246::aid-jcu6>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 20.Taori K, Ghonge N, Prakash A. Wandering spleen with torsion of vascular pedicle. Abdom Imaging. 2004;29:479–481. doi: 10.1007/s00261-003-0142-7. [DOI] [PubMed] [Google Scholar]
- 21.Zandi B, Zandi N. Wandering Spleen Presenting as an Asymptomatic Pelvic Mass: A Case Report. Iran J Radiol. 2008;5(3):141–144. [Google Scholar]
- 22.Balm R, Willekens FGJ. Torsion of wandering spleen. Eur J Surg. 1993;159:249–251. [PubMed] [Google Scholar]
- 23.Gordan DH, Burrell MI, Levin DC, Mueller CF, Becker JA. Wandering spleen: the radiological and clinical spectrum. Radiology. 1977;125:39–46. doi: 10.1148/125.1.39. [DOI] [PubMed] [Google Scholar]
- 24.Breisch EA, Krous HF. Autoinfarcted Wandering Spleen and Fatal Pneumococcal Sepsis in an Infant. Pediatric and Developmental Pathology. 2005;8:132–135. doi: 10.1007/s10024-004-7082-2. [DOI] [PubMed] [Google Scholar]