Abstract
Three large randomized trials are described from the Cancer Information Service Research Consortium (CISRC). Three web-based multimedia programs are being tested to help newly diagnosed prostate (Project 1) and breast cancer patients (Project 2) make informed treatment decisions and breast cancer patients prepare for life after treatment (Project 3). Project 3 is also testing a telephone callback intervention delivered by a cancer information specialist. All participants receive standard print material specific to each project. Preliminary results from the two-month follow-up interviews are reported for the initial wave of enrolled participants, most of whom were recruited from the Cancer Information Service (1-800-4-CANCER) telephone information program (Project 1 = 208, Project 2 = 340, Project 3 = 792). Self-reported use of the multimedia program was 51%, 52% and 67% for Projects 1–3, respectively. Self-reported use of the print materials (read all, most or some) was 90%, 85% and 83% for Projects 1–3, respectively. The callback intervention was completed by 92% of Project 3 participants. Among those using the CISRC interventions, perceived utility and benefit was high, and more than 90% would recommend them to other cancer patients. Five initial lessons learned are presented that may help inform future cancer communications research.
In this paper we describe a program of research testing three web-based multimedia programs to help newly diagnosed prostate and breast cancer patients make informed treatment decisions (Projects 1 and 2, respectively) and breast cancer patients prepare for life after treatment (Project 3). In addition, Project 3 is testing a telephone callback intervention in conjunction with the multimedia program. Each randomized trial is being conducted by the Cancer Information Service Research Consortium (CISRC) in collaboration with the National Cancer Institute’s (NCI) Cancer Information Service (CIS) (Marcus et al, 1998, 2005). Also included are preliminary descriptive results obtained from the two month follow-up assessments to illustrate several initial lessons learned regarding utilization of the interventions and their perceived utility and benefit.
Rationale for the CISRC Research Studies
Advances in breast and prostate cancer treatment modalities and options, as well as cancer patients’ increasing desire to participate in decision-making about treatment choices (Degner et al, 1997; Keating et al, 2002; Halvorsen, 2010; Stalmeier et al, 2007), suggest the need to develop new tools and resources to support these decisions. This is particularly true given that patients who are more involved in decision-making are likely to be more satisfied and may have better health outcomes (Keating et al, 2010; Stewart, 1995). Although ideally patients and physicians should share in this decision-making process (Institute of Medicine, 2001), insufficient information and time have been identified as major barriers to effective patient-physician communication (Shepherd et al, 2008). Studies also indicate that cancer patients have distinct information needs throughout the cancer care trajectory, that their information needs change with time and are modified by treatment-related events (Rees and Bath, 2000). However, this information is often presented in sophisticated medical terms that may be difficult for the average patient to understand. Patients may also have to resolve contradictory opinions from physicians of different specialties, and treatment options are rarely explored within the broader context of a patient’s life.
Several patient decision aids have been developed to help cancer patients make informed treatment decisions and to increase their involvement in the decision-making process (O’Connor et al, 1999, 2009; Diefenbach and Butz, 2004; Fagerlin et al, 2004; Jibaja-Weiss et al, 2006). Both implicit and explicit approaches have been used (Jibaja-Weiss et al, 2006; Whelan et al, 2004; Bryce et al, 2004). Implicit approaches are typically non-interactive, describing treatment options, benefits and risks. Explicit approaches, in addition to providing treatment information, employ interactive exercises to help maximize congruence between patients’ values and their treatment preferences. Software programs are considered optimal mediums for incorporating value-clarification exercises into decision support programs (Llewellyn-Thomas, 1995). For Projects 1 and 2, the interactive multimedia programs incorporate an explicit approach to values clarification. Both of these multimedia programs use a software environment built on the Prostate Interactive Education System (PIES) to help prostate cancer patients make informed decisions about treatment (Diefenbach and Butz, 2004). PIES uses the metaphor of a virtual health center to organize and present information that consists of a library, doctors’ offices and a conference room to review treatment choices. The design principles employed in PIES (i.e., the metaphor, extensive interactivity and the use of graphics and video) guided the design of both multimedia programs.
Project 3 addresses the challenges women with breast cancer face during the re-entry phase immediately following completion of primary treatments (Mullan, 1985). The re-entry transition from patient to survivor is an understudied and challenging period for survivors. During this time, they no longer interact frequently with the medical team and may lose the accompanying sense of guidance and security. Survivors often express concerns about cancer recurrence and the pace at which treatment side effects will diminish, since they and their interpersonal network may hope for a relatively rapid return to life as usual. A growing literature indicates that completion of cancer treatments can produce life disruption (Hou et al, 2010; Henselmans et al, 2010), and the exigencies of adjusting to a “new” normal (National Cancer Institute, 2002) may leave women with breast cancer searching for information that is not provided proactively (Chen and Siu, 2001; Luker et al, 1996; Wilson et al, 2000). Importantly, breast cancer patients who report difficulty in accessing cancer information experience lower quality of life, which can be improved by increasing self-efficacy in dealing with health-related issues (Arora et al, 2002).
Themes in challenges and information needs accompanying re-entry are similar across clinical, qualitative, and empirical reports (Stanton et al 2005a), including management of emotions and existential issues (e.g., fear of recurrence, life priorities), physical recovery, interpersonal relationships, and practical concerns (e.g., employment). However, few randomized trials have been directed toward preparing individuals with cancer for this pivotal phase, although findings are promising for psychoeducational interventions for women with breast cancer (Marcus et al, 2010; Scheier et al, 2005; Stanton et al, 2002, 2005b) and cognitive-behavioral stress management for men with prostate cancer (Penedo et al, 2004). The Project 3 intervention builds on our previous research to prepare breast cancer patients for what to expect during re-entry and to promote active coping skills to manage the challenges of re-entry.
Theoretical Foundations
Five key cognitive-social constructs provide the theoretical foundations for this research. These constructs encompass: 1) cancer-relevant interpretations, 2) beliefs and expectations about cancer treatment and disease outcomes, 3) cancer-relevant goals and values, 4) cancer-relevant affective and emotional states, and 5) self-regulatory competencies and skills for decision making and for generating and maintaining goal-oriented behaviors relevant to cancer decision-making and adjustment (Miller et al, 1996, 2009; Janz and Becker, 1984; Leventhal, 1970; Bandura, 1989).
How individuals perceive the personal relevance of health information is central to a number of health behavior theories and has been used to predict health-protective decisions and actions (Leventhal, 1970; Gritz and Bastani, 1993; Leventhal et al, 1992, 1993). Similarly, outcome beliefs and expectations have been key variables in self-regulation theory and the Health Belief Model (Janz and Becker, 1984; Leventhal, 1970). Studies have also demonstrated the importance of personal goals and values in health decision-making and adaptation (Rotter, 1954; Fischhoff et al, 1982; O’Connor et al, 2003; Holmes-Rovner, 2007; Woolf et al, 2005; Woolf, 1997) as well as the perceived costs and health consequences of not engaging in a health protective behavior (Edwards, 1954; Ronis 1992; Sutton, 1982). Personal values and goals are particularly important in regard to “preference sensitive” decisions (O’Connor et al, 2003), which are those in which the benefit-to-harm ratio is unclear. Making these decisions is, to a large extent, dependent on the individual’s prototypic cognitive-social profile, as is the case for patients engaging in follow-up actions after cancer diagnosis and treatment (O’Connor et al, 1997, 2003, 2004). Our basic premise is that providing these theory-based preparatory and skills-oriented information and strategies will improve self-efficacy (Bandura, 1997, 1981; Bandura et al, 1997), thereby decreasing cancer-specific distress as well as improving other relevant outcomes (described below).
Research Methodology
Research Design
The CIS was established by NCI in 1975 to provide accurate, up-to-date cancer information to all segments of the U.S. population (Bright, 2007). Highly trained information specialists provide cancer information to patients and their family members who contact the CIS via telephone (1-800-4-CANCER), LiveHelp (an online instant messaging service) and by email. When the three CISRC research projects were launched in 2008, the CIS network consisted of three contact centers and was the single point-of-entry for study enrollment. At the completion of the usual service call to 1-800-4-CANCER, information specialists invited callers to learn more about the CISRC project for which they may be eligible. If interested, callers completed a brief baseline telephone interview appended to their usual service call, where final eligibility was determined, the study was described, and informed consent was obtained.
In December 2009, NCI awarded a new CIS contract that consolidated the three contact centers into one national contact center. During the extended transition period that followed, the CIS was no longer able to continue with study enrollment. The CISRC then established its own call center for recruitment at the University of Colorado Cancer Center, where callers received the same recruitment information, baseline interview and informed consent protocol, as well as a referral to the CIS. To promote calls to this new recruitment center, an aggressive outreach campaign was subsequently implemented (Figure 1).
FIGURE 1.
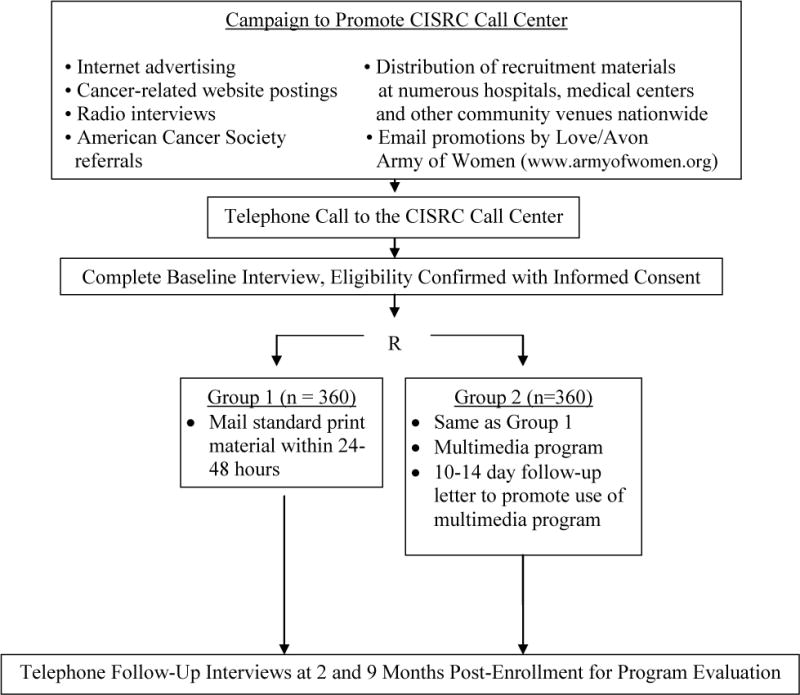
Overview of Research Design for Projects 1 and 2. Project 3 includes Groups 1 and 2 as shown in Figure 1 as well as a third randomized group (n=360) that receives the Group 2 intervention targeted to breast cancer survivors and a telephone callback intervention. The latter consists of a single callback at 10–14 days post-enrollment.
As indicated in Figure 1, Projects 1 and 2 share the same two-group randomized design, where Group 1 receives a standard print material intervention, while Group 2 also receives the multimedia program specific to each project and a follow-up letter prompt to use the multimedia program. Immediately after completion of the baseline interview, callers are randomized to Group 1 or Group 2. Within 24–48 hours, participants receive by mail the standard print material (Group 1) or the standard print material plus the URL for the web-based multimedia program (Group 2). A CD version of the program is also included in the Group 2 mailing, along with instructions for accessing the web-based version of the program. For Project 1, the standard NCI print materials include What You Need to Know About Prostate Cancer and Treatment Choices for Men with Prostate Cancer. For Project 2, the NCI print materials are What You Need to Know About Breast Cancer and Surgery Choices for Women with Early Stage Breast Cancer.
The research design for Project 3 is identical to Projects 1 and 2, with one key difference: a third group was added to test a telephone callback intervention as part of a randomized three-group “stepped” design. Thus, while Groups 1 and 2 are the same as Projects 1 and 2, Group 3 receives standard print material, the multimedia program and follow-up letter prompt as well as the callback intervention, with the latter consisting of one callback that occurs 10–14 days following study enrollment. During the period when the CIS contact centers recruited participants, the callback intervention was conducted by CIS information specialists. When the CISRC call center was activated, the callback intervention was transferred to counseling staff of the Cancer Information and Counseling Line (CICL) (Marcus et al, 2002). Standard NCI print materials used in Project 3 are Facing Forward: Life After Cancer Treatment and What You Need to Know About Breast Cancer.
Patient Eligibility
For all projects, eligibility criteria include a diagnosis of nonmetastatic cancer, access to a computer (either personally or with the assistance of a family member or friend), English-speaking, and providing telephone informed consent. For Projects 1 and 2, eligibility is limited to breast (female) and prostate cancer patients who are still making treatment decisions, while Project 3 is limited to female breast cancer patients who are within six weeks of completing primary therapy or within six months after primary therapy (i.e., surgery, radiotherapy, chemotherapy).
Baseline and Follow-Up Assessments
To avoid disrupting standard service at the CIS as well as adding to respondent burden, the baseline telephone interviews appended to the usual service calls focused mainly on determining eligibility and securing informed consent. These same baseline interviews were used at the CISRC recruitment center.
Telephone follow-up interviews occur at two and nine months post-enrollment. Included are standardized measures assessing the primary endpoints and hypothesized mediator and moderator variables for each project. Across all projects, these include cancer-specific distress assessed by intrusive thoughts (Horowitz et al, 1979; Sundin and Horowitz, 2002), anxiety and depressive symptoms (Zigmond and Snaith, 1983; Bjelland et al, 2002), coping self-efficacy (Penedo et al, 2003), communication with health care providers (Schag et al, 1990, 1993; Ganz et al, 1990) and various project-specific assessments of functional health status, fatigue, vitality and quality of life (Esper et al, 1997; Brady et al, 1997; Yellen et al 1997; Ware et al, 1996; Ganz et al, 1995; Broadbent et al, 2006). Additional assessments include decisional self-efficacy (Bunn and O’Connor, 1996; Cranney et al, 2002), conflict and regret (O’Connor et al, 1999; O’Connor, 1995; Brehaut et al, 2003) for Projects 1 and 2, and benefit-finding (Antoni et al, 2001) and fear of recurrence (Stanton et al, 2001, 2002; Krishnan et al, 2001) for Project 3. The follow-up interviews also include project-specific questions regarding use of the print materials, and use and perceived utility of the multimedia programs and the callback intervention.
Overview of Multimedia Program Development, Content and Interactivity
A comprehensive literature review and identification of NCI-vetted content served as the foundation for the information in the three multimedia software programs. The developmental process also included conceptual, literacy and cultural appropriateness review, user testing, and usability testing. Guided by literacy and patient education experts, all new and existing materials were produced with a 7th grade reading level obtained through plain language evaluation.
User testing gathered audience response to the overall approach, specific software elements, appeal of characters, and multi-media components. Usability testing participants, guided by NCI usability guidelines (http://usability.gov/index.html), reviewed the final prototype using the “task analysis” method. During the usability interview, patient’s real-time expressions were recorded to monitor the process of task completion. Final program modifications were implemented to avoid navigational difficulties or errors detected during testing. Development and testing of the multimedia programs took about 19 months.
Figure 2 provides an example from Project 1 of the main page for the multimedia program, which is also representative of Projects 2 and 3. As shown, the software is divided into four modules (Library, Patient Stories, Doctor’s Office and the Notebook). Each of the three versions of the software uses the same platform, design and metaphors. Users first encounter a Virtual Information Specialist who provides an overview of the software and how to navigate through it. Users can then complete a short needs assessment, with the software providing navigational suggestions as appropriate.
FIGURE 2.
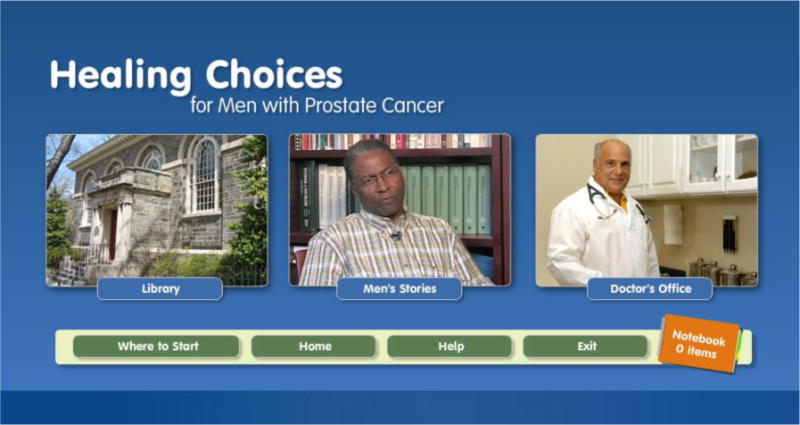
Screen Shot of Main Page for Project 1 Multimedia Program: Healing Choices for Men with Prostate Cancer. (Color figure available online.)
Users may select any of the links that will take them to specific modules. The Library includes books on relevant topics containing over 100 pages of text and graphics. The Doctor’s Office includes a module highlighting effective provider-patient communication, questions to ask your provider, videos of doctors answering frequently asked questions (Projects 1 and 2) and a treatment summary and survivorship care plan (Project 3). The Notebook allows patients to record and store information they deem relevant while reading books from the library. Once patients access the notebook they can sort and rank the stored information according to their perceived importance (e.g., the pros and cons of each treatment option for Projects 1 and 2, or action steps to maintain their health for Project 3. The software also includes a tracking system to record participants’ usage patterns. Finally, patient stories (videos) were used to highlight actual patient perspectives, drawing upon previous research indicating the effectiveness of narrative communication in cancer prevention and control (e.g., Kreuter et al., 2007; Wise et al, 2007). In addition, our experience with PIES and formative research conducted by the team indicated that patients liked to listen to survivors’ experiences. We selected survivors who represented a number of ethnicities and different treatment choices (Project 1 and Project 2) or survivorship experiences post-treatment (Project 3). Each 5–6 minute video represents actual survivor experiences and were not investigator-constructed vignettes. Survivors received a list of topics and were asked to speak about them. These talking points were designed to assist survivors in re-creating and sharing their treatment decision-making process (e.g., the factors that were important in their decision) or experiences when transitioning into survivorship post treatment, as well as how emotionally stressful this period of time was in their life.
Overview of the Callback Intervention
During the Project 3 callback intervention, information specialists follow a computerized script that normalizes information-seeking needs of patients after treatment and then solicits questions in four life domains: physical recovery, emotions, talking with others, and practical issues. Questions are answered using available NCI-approved materials and the multimedia program. The information specialist also provides a prompt to use the multimedia program and other resources, including the CIS or CICL.
Sample Size, Response Rates and Statistical Analysis
The preliminary results reported below were obtained from the initial wave of participants recruited from September 2008 to May 2010 who also completed the two-month follow-up interviews. Among those participants who were eligible for these interviews, the response rates were 77% for Project 1 (n = 208), 73% for Project 2 (n = 340), and 88% for Project 3 (n = 792). Given the descriptive focus of this preliminary analysis, frequency distributions are reported by project along with associated sample sizes.
Results
Sample Characteristics
Enrolled participants were mainly non-Hispanic White (70% for Project 1, 73% for Project 2 and 91% for Project 3), although nearly 20% were African American for Projects 1 and 2 (19% and 17%, respectively). Virtually all participants had at least a high school education, with a high percentage reporting a four-year college degree or above (47% for Project 1, 45% for Project 2 and 69% for Project 3). The average age of participants was 65.2 for Project 1 (SD = 8.7), 56.2 for Project 2 (SD = 10.9) and 53.6 for Project 3 (SD = 10.1). This sociodemographic profile mirrors the sociodemographic characteristics of callers to the CIS (Ward et al, 1998; Squires et al, 2005), with the CIS enrolling the vast majority of participants included in this report (97% for Project 1, 91% for Project 2 and 95% for Project 3).
Use of Standard Print Material
A high percentage of participants reported reading some, most or all of the standard print materials (Table 1), ranging from 83% (Project 3) to 90% (Project 1). Also noteworthy is that access to the multimedia program in Project 1 (Group 2) and Project 3 (Groups 2 and 3) did not diminish reading some, most or all of these materials when compared to Group 1. For Project 2, there was a modest difference favoring Group 1 vs. Group 2 (88% vs. 82%).
TABLE 1.
Percent Reporting Use of Standard Print Material at Two Months Follow-Up
| Project 1 | Project 2 | Project 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
How Much of the Print Material was Read? |
Group 1 (n = 99) |
Group 2 (n = 109) |
Total (n = 208) |
Group 1 (n = 176) |
Group 2 (n = 164) |
Total (n = 340) |
Group 1 (n = 270) |
Group 2 (n = 260) |
Group 3 (n = 262) |
Total (n = 792) |
| All | 40.4 | 48.6 | 44.7 | 42.6 | 36.6 | 39.7 | 41.9 | 33.5 | 35.1 | 36.9 |
| Most | 31.3 | 22.9 | 26.9 | 31.3 | 28.0 | 29.7 | 27.0 | 30.8 | 32.4 | 30.1 |
| Some | 16.2 | 20.2 | 18.3 | 14.2 | 17.1 | 15.6 | 15.2 | 16.5 | 17.2 | 16.3 |
| Little | 5.1 | 4.6 | 4.8 | 5.7 | 7.9 | 6.8 | 8.1 | 7.3 | 6.1 | 7.2 |
| None | 3.0 | 2.8 | 2.9 | 4.0 | 9.1 | 6.5 | 4.1 | 9.6 | 6.9 | 6.8 |
| Don’t Know | 4.0 | 0.9 | 2.4 | 2.3 | 1.2 | 1.8 | 3.7 | 2.3 | 2.3 | 2.8 |
Use and Perceived Utility of the Multimedia Programs
About 50% of participants in Projects 1 and 2 reported using the multimedia program, compared to 67% for Project 3, Groups 2 and 3 combined (Table 2). Among those who reported using the program, a high percentage reported use of one or more hours: 69% for Project 1, 79% for Project 2 and 80% for Project 3. Across all projects, most participants reported no problems in finding the information they were seeking, ranging from 86% (Project 1) to 94% (Project 2).
TABLE 2.
Use and Perceived Utility of the Multimedia Programs Reported at Two Months Follow-Up
| Project 1 | Project 2 | Project 3 | ||||
|---|---|---|---|---|---|---|
| % | N | % | N | % | N | |
| Self-reported use | 51.4 | 109 | 51.8 | 164 | 66.7 | 522 |
| How much time | 3.6 | 56 | 2.4 | 85 | 2.9 | 348 |
| < 15 minutes | 19.6 | 56 | 15.3 | 85 | 16.4 | 348 |
| 15–30 minutes | 68.7 | 56 | 78.8 | 85 | 79.9 | 348 |
| ≥ 1 hour | ||||||
| How easy to find information (% easy) | 85.7 | 56 | 94.1 | 85 | 92.2 | 348 |
| Increased knowledge (% agree) |
94.6 | 56 | 90.6 | 85 | 74.4 | 348 |
| Increased confidence (% agree) |
89.3 | 56 | 80.0 | 85 | 80.1 | 348 |
| Helped make TX decisions (% agree) |
85.7 | 56 | 70.6 | 85 | … | … |
| Helped adjust to life post-treatment (% agree) |
… | … | … | … | 76.4 | 348 |
| Would recommend to others (% agree) |
92.9 | 56 | 91.8 | 85 | 93.7 | 348 |
More than 90% of Project 1 and Project 2 participants who reported using the multimedia program indicated that it increased their knowledge, compared to 74% of Project 3 participants. High ratings were also reported for increased confidence (80% – 89% across all projects). The multimedia program also received positive ratings in providing assistance in making treatment decisions, which were somewhat higher for Project 1 compared to Project 2 (86% vs. 71%). About 75% of Project 3 participants reported that the multimedia program helped them adjust to life after treatment. More than 90% across all projects indicated that they would recommend the multimedia program to others.
When non-users were asked why they did not use the multimedia program, the most prevalent reasons for Project 1 (n = 47) were no computer access (30%), no need (17%), technical problems with the computer or website (15%), no time or too busy (13%), and did not know how to use the multimedia program (9%). For Project 2 (n = 74), the most prevalent reasons were no time or too busy (30%), no computer access (27%), and no need (11%), with only 3% reporting technical problems with the computer or website. For Project 3 (n = 166), the most frequent reasons were no time or too busy (47%), no computer access (14%), no need (10%), and technical problems with the computer or website (10%). For Projects 2 and 3, only a very small percentage of non-users (less than 2%) reported that they did not know how to use the multimedia programs.
As noted previously, the Group 3 callback intervention for Project 3 was intended to prompt use of the multimedia program as well as respond to new questions or concerns that may have occurred following study enrollment. Ninety percent of Group 3 participants indicated that they received the callback, and of these, 87% reported receiving the reminder to use the multimedia program. Among those assigned the callback intervention (Group 3), self-reported use of the multimedia program was 71%, compared to 62% for those not assigned the callback (Group 2). The percentage of non-users reporting specific barriers to utilization were similar across groups in Project 3.
Use and Perceived Utility of the Callback Intervention
Based on project records, 92% of Project 3 participants who were assigned the callback intervention (n = 262) actually received the callback, which mirrors self-reports (90%) obtained during the two-month interviews. Less than 2% refused the callback, less than 2% had a non-working or wrong telephone number, while 4% did not complete the callback because they reached maximum attempts (six attempts) for completing this intervention.
About 65% of participants who reported receiving the callback indicated that they discussed questions or concerns related to breast cancer (Table 3). Of these participants, 83% reported that all or most (61%) or some (22%) of the information they were seeking was provided, 77% reported that the callback increased their knowledge, 75% indicated an increase in self-confidence, and 72% felt that the callback helped them adjust to life after treatment. Over 90% recommended that the callbacks be continued as a service program. Among those who recommended continuing this intervention, 55% felt that more than one callback should occur, with the number ranging from two to 12.
TABLE 3.
Perceived Utility of the Project 3 Callback Intervention Reported at Two Months Follow-Up
| % | |
|---|---|
| Discussed questions/concerns about breast cancer (% yes) | 66.11 |
| How much information looking for did you actually receive: | |
| All/most | 61.52 |
| Some | 21.8 |
| Little/None | 16.7 |
| Increased knowledge (% agree) | 76.92 |
| Increased confidence (% agree) | 75.02 |
| Helped adjust to life post-treatment (% agree) | 71.82 |
| Recommend continuing as usual service program (% agree) | 91.72 |
| Among those who recommended callbacks: | |
| Recommended 1 callback | 40.63 |
| Recommended 2+ callbacks | 54.5 |
| Don’t know | 4.9 |
Denominator = Group 3 participants (n=262) who reported receiving callback intervention (n=236 or 90%)
Denominator = Group 3 participants who reported discussing breast cancer questions/concerns (n=156)
Denominator = Group 3 participants who recommended continuing callback as service program (n=143)
Discussion
Although the findings included in this report are preliminary, several themes can be inferred as initial lessons learned.
Lesson One
When cancer patients use well-designed and authoritative multimedia programs specifically developed for them, they can report high levels of use and perceived benefit
Among those who reported using the CISRC multimedia programs, the majority reported use of one hour or more, and most reported benefits in terms of increased knowledge and self-confidence, as well as assistance in making treatment decisions and preparing for life post-treatment. More than 90% of users across projects would recommend the CISRC multimedia programs to others.
Lesson Two
Utilization of web-based multimedia programs may be less than optimal within randomized trials, even when access to a computer is an eligibility criterion
The percentage of participants who reported not using the multimedia programs ranged from 33% (Project 3) to nearly 50% (Projects 1 and 2). Others have reported similar findings of less than optimal utilization of Internet-based programs for tobacco control (Buller et al, 2008a), healthy dietary practices (Buller et al, 2008b), physical activity (Leslie et al, 2005), colorectal and prostate cancer screening (Fleisher et al, in press; Allen et al, 2010), and mental health (Farvolden et al, 2005; Chrisstensen et al, 2004a,b). Given that interactive, multimedia platforms for behavioral and psychoeducational interventions can offer enhanced opportunities for personalized learning and behavior change, low utilization of this new communication technology represents a significant challenge for future research (Buller et al, 2008b; Fleisher et al, in press; Eysenbach, 2005).
Among the factors that may account for low utilization are technology problems (e.g., insufficient bandwidth, slow Internet connections) and inadequate technical support (Buller et al, 2008a; Hall et al, 2001). Neither of these issues would seem to apply to this research, where the multimedia programs were provided via the Internet and on CDs with technical support available from a well-publicized toll-free CISRC HelpDesk. Concerns about functionality of the web-based programs also do not appear compelling. The vast majority of users across all projects reported easy navigation in finding the information they were seeking, and only a small percentage of non-users reported that they did not know how to use the multimedia programs or that technical problems were encountered. It would also seem that we can discount the concern that participants did not perceive a need for the information provided. When non-users were asked why they did not use the multimedia programs, lack of need was mentioned by less than 20% of non-users in Project 1, and only about 10% in Projects 2 and 3. Even more revealing is that use of the standard print materials was high, exceeding 80% across all projects.
Among the most prevalent reasons cited for non-use was the lack of access to a computer, especially for newly diagnosed prostate (30%) and breast cancer (27%) patients. The corresponding percentage for Project 3 was 14%. In the three CISRC trials, access to a computer (as an eligibility criterion) was defined as including facilitated access provided by family, friends and others. Thus, it seems plausible that concerns about access may reflect, at least in part, a reluctance to seek facilitated access from others.
For Project 1, a lack of time or being too busy was not reported as a major barrier to utilization (13%). For Project 2 (30%), and even more so for Project 3 (47%), this did emerge as a key barrier. Prostate cancer patients were older than the breast cancer samples and perhaps more likely to be retired. In addition, the window of opportunity to use the multimedia program to help make treatment decisions could be greater for prostate cancer patients (i.e., they are frequently advised that treatment decisions need not be made immediately because prostate cancer tumors are often slow-growing). For Project 3, the high percentage of non-users reporting this barrier may indicate that cancer survivors post-treatment are less likely to be faced with urgent or time-sensitive decisions as they transition back to employment and other life activities.
Lesson Three
Interpersonal interventions, even those involving only a single contact, can have high perceived utility and benefit within a web-based multimedia environment
This lesson learned applies to the Project 3 callback intervention, where refusal rates were extraordinarily low (<2%) and reach exceeded 90%. Even though participants had access to the multimedia program, nearly 70% of those who reported receiving the callback also reported having questions or concerns that were discussed during the callback. Nearly 85% of these participants reported that at least some of the information they were seeking was provided during the callback, 61% reported that most or all of this information was acquired, and 90% felt that the callback should be continued as a service program. Especially noteworthy is that more than half of those who used the single callback to discuss their questions and concerns were left wanting more callbacks.
Lesson Four
This lesson is offered as a constructive response to the second lesson mentioned above: interpersonal reminders to use new, web-based communication technology can be effective, as illustrated by the Project 3 callback intervention. Not only did the vast majority of Group 3 participants recall receiving this prompt as part of the callback protocol (87%), but this reminder seemed to resonate with participants, with a corresponding increase in reported use of the multimedia program from 62% (Group 2, no callback) to 71%.
Lesson Five
Print materials can remain resilient even within a web-based multimedia environment
The vast majority of participants across all projects reported reading at least some of the print materials, far surpassing the utilization rates reported for the multimedia programs. This finding, which has also been reported previously (Fleisher et al, in press), begs the key question as to why participants would favor the print materials over state-of-the-science multimedia programs that offer such compelling and attractive features as interactivity and video. As noted above, perhaps one reason has to do with the older age of the target population, where direct (non-mediated) access to the Internet or comfort level in using this technology is likely to be lower when compared to the general population (PewInternet, 2010). Also noteworthy is that access to the multimedia program URLs was provided in a letter that accompanied the print material in each trial. Why would participants take the extra time to access the multimedia program if well-designed and authoritative print materials at their fingertips provide the information they are seeking?
If convenience and/or comfort level is driving this preference for print materials, perhaps we should embrace this dynamic for the current generation of adult cancer patients and survivors. Instead of conceptualizing print materials as a less sophisticated alternative to new multimedia communication technology, we might look to synergize print materials with this new technology. Thus, going forward in our research, we might conceptualize print materials as the “first responders” to the information-seeking needs of many if not most adult cancer patients, and design print materials so that they serve as a conduit for using multimedia interventions to further enhance personalized learning and tailored information-seeking. If this recommendation has merit, perhaps we should also consider moving away from simplistic comparative efficacy trials that compare print materials vs. new communication technology, or, as in the case of the CISRC, attempt to evaluate the value added contribution of new communication technology above and beyond stand-alone print materials. Perhaps we should design and test interventions for the current generation of cancer patients and survivors that systematically and thoughtfully blend the two modalities in a synergistic and complementary fashion.
Finally, several important study limitations should be emphasized. These results are preliminary, derived from the initial wave of participants enrolled in the three randomized trials. The sociodemographic profile of the three study samples (mainly non-Hispanic white and highly educated) could also limit the generalizability of findings. Most study participants received standard service from the CIS before receiving the CISRC interventions, which could limit the need for these interventions as well as their utilization and perceived benefit. In addition, these findings are based on participant self-reports that may be susceptible to measurement error in the opposite direction (i.e., over-reporting of intervention use and benefit). However, while appropriate caution should be exercised when interpreting these findings, the results obtained from this analysis are sufficiently striking that they may help inform the next generation of health-related intervention research, especially research that uses new, interactive communication technology.
Acknowledgments
The authors acknowledge the other members of the CISRC research team: Kuang-Yi Wen (Fox Chase Cancer Center, Philadelphia, Pennsylvania, USA), Ellen Berman (Lockheed Martin, Health Applications, Rockville Maryland, USA), Meg Rebull (University of Colorado Cancer Center, Denver, Colorado, USA), Jeff Consoer (Department of Anesthesiology, School of Medicine, University of Colorado, Denver Colorado, USA), Kathleen Garrett (University of Colorado Cancer Center, Denver, Colorado, USA), Alexandra Jorge (Departments of Psychology & Psychiatry/Biobehavioral Sciences, Jonsson Comprehensive Cancer Center, University of California Los Angeles, Los Angeles California, USA), Nihal Mohamed (Mount Sinai School of Medicine, New York New York, USA), Mary E. Ropka (Fox Chase Cancer Center, Philadelphia, Pennsyvlania, USA, and School of Medicine, University of Virginia, Charlottesville Virginia, USA), Nancy S. Zbaren (National Cancer Institute Cancer Information Service Contact Center, Fred Hutchinson Cancer Research Center, Seattle Washington, USA), and Julie Kornfeld (Department of Epidemiology and Public Health, University of Miami Miller School of Medicine, Miami Florida, USA).
This research was supported by grant: 5P01CA057586 from the National Cancer Institute (NCI) of the National Institutes of Health. The accuracy of the information and the interpretations and conclusions reported herein are the sole responsibility of the authors and not the NCI. The design, development and production of the CISRC multimedia programs was performed by the NCI-funded Behavioral Core Facility of the Fox Chase Cancer Center (P30CA06927). Programming of the baseline interviews and distribution of all CISRC intervention materials was performed by Lockheed Martin, Rockville, Maryland. The telephone follow-up interviews were conducted by the NCI-funded Survey Research Shared Resource of the University of Colorado Cancer Center. We gratefully acknowledge and salute the cancer patients and survivors who voluntarily gave of their time and effort to make this research possible. We also gratefully acknowledge the cancer information specialists and management staff at the three participating CIS call centers who were indispensible collaborators in this research, as well as the counselors of the Cancer Information and Counseling Line, University of Colorado at Denver, who are now delivering the Project 3 callback intervention. Finally, special thanks are extended to those who collaborated in patient recruitment to the three CISRC studies, including the American Cancer Society and Love/Avon Army of Women.
Contributor Information
ALFRED C. MARCUS, University of Colorado Cancer Center, University of Colorado, Denver Colorado, USA
MICHAEL A. DIEFENBACH, Mount Sinai School of Medicine, New York New York, USA
ANNETTE L. STANTON, Department of Psychology & Psychiatry/Biobehavioral Sciences, Jonsson Comprehensive Cancer Center, University of California Los Angeles, Los Angeles California, USA
SUZANNE N. MILLER-HALEGOUA, Fox Chase Cancer Center, Philadelphia, Pennsylvania, USA
LINDA FLEISHER, Fox Chase Cancer Center, Philadelphia, Pennsylvania, USA.
PETER C. RAICH, Denver Health and Hospital Authority, Denver Colorado, USA
MARION E. MORRA, Yale School of Nursing, New Haven Connecticut, USA
ROSEMARIE SLEVIN PEROCCHIA, Memorial-Sloan-Kettering Cancer Center, New York New York, USA.
ZUNG VU TRAN, University of Colorado Cancer Center, University of Colorado, Denver Colorado, USA.
MARY ANNE BRIGHT, Cancer Information Service, National Cancer Institute, Bethesda Maryland, USA.
References
- Allen JD, Othus MK, Hart A, Jr, Tom L, Li Y, Berry D, Bowen D. A randomized trial of a computer-tailored decision aid to improve prostate cancer screening decisions: results from the take the wheel trial. Cancer Epidemiol Biomarkers Prev. 2010 Sep;19(9):2172–86. doi: 10.1158/1055-9965.EPI-09-0410. Epub 2010 Aug 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology. 2001;20:20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- Arora NK, Johnson P, Gustafson DH, McTavish F, Hawkins RP, Pingree S. Barriers to information access, perceived health competence, and psychosocial health outcomes: Test of a mediation model in a breast cancer sample. Patient Education and Counseling. 2002;47:37–46. doi: 10.1016/s0738-3991(01)00170-7. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-Efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social learning theory of aggression. J Commun. 1978;28(3):12–29. doi: 10.1111/j.1460-2466.1978.tb01621.x. [DOI] [PubMed] [Google Scholar]
- Bandura A. The assessment and predictive generality of self-percepts of efficacy. Journal of Behavioral Therapy and Experimental Psychiatry. 1981;13(3):195–199. doi: 10.1016/0005-7916(82)90004-0. [DOI] [PubMed] [Google Scholar]
- Bandura A. Human agency in social cognitive theory. American Psychologist. 1989;44(9):1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- Bandura A, Adams NE, Beyer J. Cognitive processes mediating behavioral change. Journal of Personality and Social Psychology. 1977;35(3):125–39. doi: 10.1037//0022-3514.35.3.125. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, et al. Reliability and validity of the Functional Assessment of Cancer Therapy – Breast quality-of-life instrument. Journal of Clinical Oncology. 1997;15:974–986. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- Brehaut JC, O’Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E, Feidman-Steward D. Validation of a decision regret scale. Medical Decision Making. 2003;23(4):282–292. doi: 10.1177/0272989X03256005. [DOI] [PubMed] [Google Scholar]
- Bright MA. The National Cancer Institute’s Cancer Information Service: A premiere cancer information and education resource for the nation. J Cancer Educ. 2007;22:S2–S7. doi: 10.1007/BF03174340. [DOI] [PubMed] [Google Scholar]
- Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosom Res. 2006;60:631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Bryce CL, Angus DC, Switala J, Roberts MS, Tsevat J. Health status vs. utilities of patients with end-stage liver disease. Quality of Life Research. 2004;13:773–782. doi: 10.1023/B:QURE.0000021685.83961.88. [DOI] [PubMed] [Google Scholar]
- Buller DB, Borland R, Woodall WG, Hall JR, Hines JM, Burris-Woodall P, et al. Randomized trials on Consider This, a tailored, Internet-delivered smoking prevention program for adolescents. Health Educ Behav. 2008a;35:260–281. doi: 10.1177/1090198106288982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buller DB, Woodall WG, Zimmerman DE, Slater MD, Heimendinger J, Waters E, et al. Randomized trial on the 5-A-Day, the Rio Grande Way website, a web-based program to improve fruit and vegetable consumption in rural communities. Journal of Health Communication. 2008b;13:220–249. doi: 10.1080/10810730801985285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunn H, O’Connor A. Validation of client decision-making instruments in the context of psychiatry. Canadian Journal of Nursing Research. 1996;28:13–27. [PubMed] [Google Scholar]
- Chen X, Siu LL. Impact of the media and the Internet on oncology: Survey of cancer patients and oncologists in Canada. Journal of Clinical Oncology. 2001;19:4291–4297. doi: 10.1200/JCO.2001.19.23.4291. [DOI] [PubMed] [Google Scholar]
- Chrisstensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the Internet: Randomized controlled trial. BMJ. 2004a;328(7):265. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Korten AE, Brittliffe K, Groves C. A comparison of changes in anxiety and depression symptoms of spontaneous users and trial participants of a cognitive behavior therapy website. J Med Internet Res. 2004b;6(4):e46. doi: 10.2196/jmir.6.4.e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cranney A, O’Connor A, Jacobsen MJ, Tugwell P, Adachi JD, Ooi DS, et al. Development and pilot testing of a decision aid for postmenopausal women with osteoporosis. Patient Education and Counseling. 2002;47:245–255. doi: 10.1016/s0738-3991(01)00218-x. [DOI] [PubMed] [Google Scholar]
- Degner LF, Kristjanson LJ, Bowman D, et al. Information needs and decisional preferences in women with breast cancer. J Am Med Assoc. 1997;177:1485–1492. [PubMed] [Google Scholar]
- Diefenbach MA, Butz BP. A multimedia interactive education system for prostate cancer patients: development and preliminary evaluation. Journal of Medical Internet Research. 2004;6(1):e3. doi: 10.2196/jmir.6.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards KC. Pruritus in melancholia. British Medical Journal. 1954;25(4903):1527–1529. doi: 10.1136/bmj.2.4903.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esper P, MO F, Chodak G, Sinner M, Cella D, Pienta KJ. Measuring Quality of life in men with prostate cancer using the Functional Assessment of Cancer Therapy-Prostate (FACT-P) instrument. Urology. 1997;50(6):920–928. doi: 10.1016/S0090-4295(97)00459-7. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. The law of attrition. Journal of Medical Internet Research. 2005;7:e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerlin A, Rovner A, Stableford S, Jentoft C, Wei J, Holmes-Rovner M. Patient education materials about the treatment of early-stage prostate cancer: A critical review. Annals of Internal Medicine. 2004;4:9, 721–728. doi: 10.7326/0003-4819-140-9-200405040-00012. [DOI] [PubMed] [Google Scholar]
- Farvolden P, Denisoff E, Selby P, Bagby RM, Rudy L. Usage and longitudinal effectiveness of a web-based self-help cognitive behavioral therapy program for panic disorder. J Med Internet Res. 2005;7(1):e7. doi: 10.2196/jmir.7.1.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischhoff B, Goitein B, Shapira Z. The experienced utility of expected utility approaches. In: Feather N, editor. Expectancy, Incentive and Action. Hillsdale NJ: Erlbaum; 1982. pp. 315–339. [Google Scholar]
- Fleisher L, Kandadai V, Keenan E, Miller SM, Devarajan K, Ruth KL, et al. Build it and will they come? Unexpected findings from a study on a web-based intervention to improve colorectal cancer screening. Journal of Health Communication. doi: 10.1080/10810730.2011.571338. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz PA, Schag CC, Cheng H. Assessing the quality of life: A study in newly diagnosed breast cancer patients. Journal of Clinical Epidemiology. 1990;43:75–86. doi: 10.1016/0895-4356(90)90059-x. [DOI] [PubMed] [Google Scholar]
- Ganz PA, Day R, Ware JE, Redmond C, Fisher B. Baseline quality-of-life assessment in the National Surgical Adjuvant Breast and Bowel Project Breast Cancer Prevention Trial. Journal of the National Cancer Institute. 1995;87:1372–1382. doi: 10.1093/jnci/87.18.1372. [DOI] [PubMed] [Google Scholar]
- Gritz ER, Bastani R. Cancer prevention–behavior changes: the short and the long of it. Preventive Medicine. 1993;22(5):676–88. doi: 10.1006/pmed.1993.1061. [DOI] [PubMed] [Google Scholar]
- Hall JR, Ax B, Brown M, Buller DB, Woodall WG, Borland R. Challenges to producing and implementing the Consider This web-based smoking prevention and cessation program. Electronic Journal of Communication. 2001;11:3–4. Retrieved from http://www.cios.org/www/ejc/v11n3.htm. [Google Scholar]
- Halvorsen PA. What information do patients need to make a medical decision? Med Decis Making. 2010;30:11S–13S. doi: 10.1177/0272989X10381349. [DOI] [PubMed] [Google Scholar]
- Henselmans I, Helgeson VS, Seltman H, de Vries J, Sanderman R, Ranchor AV. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychol. 2010;29:160–168. doi: 10.1037/a0017806. [DOI] [PubMed] [Google Scholar]
- Holmes-Rovner M. International patient decision aid standards (IPDAS): Beyond decision aids to usual design of patient education materials. Health Expectations. 2007;10:103–107. doi: 10.1111/j.1369-7625.2007.00445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective distress. Psychosomatic Medicine. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hou WK, Law CC, Yin J, Fu YT. Resource loss, resource gain, and psychological resilience and dysfunction following cancer diagnosis: A growth mixture modeling approach. Health Psychol. 2010;29:484–495. doi: 10.1037/a0020809. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health Care System for the 21st Century. Washington, D.C.: National Academy Press; 2001. [Google Scholar]
- Janz NK, Becker MH. The Health Belief Model: A decade later. Health Education Quarterly. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Jibaja-Weiss ML, Volk R, Fridman LC, Granchi TS, Neff N, Spann SJ, Robinson LK, Aoki N, Beck R. Preliminary testing of a just-in-time, user-defined values clarification exercise to aid lower literate women in making informed breast cancer treatment decisions. Health Expectations. 2006;9:218–231. doi: 10.1111/j.1369-7625.2006.00386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keating NL, Guadagnoli E, Landrum MB, Borbas C, Weeks JC. Treatment decision making in early-stage breast cancer: should surgeons match patients’ desired level of involvement. J Clin Oncol. 2002;20:1473–1479. doi: 10.1200/JCO.2002.20.6.1473. [DOI] [PubMed] [Google Scholar]
- Keating NL, Landrum MB, Arora NK, Malin JL, Ganz PA, van Ryn M, Weeks JC. Cancer patient’s roles in treatment decisions: Do characteristics of the decision influence roles. J Clin Oncol. 2010;28:4364–4370. doi: 10.1200/JCO.2009.26.8870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan L, Stanton AL, Collins CA, Liston VE, Jewell WR. Form or function? 2. Objective cosmetic functional correlates of quality of life in women treated with breast-conserving surgical procedures and radiotherapy. Cancer. 2001;91:2282–2287. [PubMed] [Google Scholar]
- Kreuter MW, Green MD, Cappella JN, Slater MD, Wise ME, Storey D, Clar EM, O’Keefe DJ, Erwin DO, Holmes K, Hinyard LJ, Houston T, Woolley S. Narrative Communication in Cancer Prevention and Control: A framework to guide research and application. Annals of Behavioral Medicine. 2007;33(3):221–235. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- Leslie E, Marshall AL, Owen N, Bauman A. Engagement and retention of participants in a physical activity website. Prev Med. 2005;40(1):54–59. doi: 10.1016/j.ypmed.2004.05.002. [DOI] [PubMed] [Google Scholar]
- Leventhal H. Findings and theory in the study of fear communications. Advances in Experimental Social Psychology. 1970;5:119–186. [Google Scholar]
- Leventhal H, Diefenbach M, Levanthal E. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cognitive Therapy and Research. 1992;16(2):143–163. [Google Scholar]
- Leventhal EA, Suls J, Leventhal H. Hierarchical analysis of coping: evidence from life-span studies. In: Krohne HW, editor. Attention and Avoidance. Seattle, WA: Hogrefe & Huber; 1993. pp. 71–98. [Google Scholar]
- Llewellyn-Thomas HA. Patients health-care decision making: a framework for descriptive and experimental investigations. Medical Decision Making. 1995;15:101–106. doi: 10.1177/0272989X9501500201. [DOI] [PubMed] [Google Scholar]
- Luker KA, Beaver K, Leinster SJ, et al. Information needs and sources of information for women with breast cancer: a follow-up study. J Adv Nurs. 1996;23:487–495. doi: 10.1111/j.1365-2648.1996.tb00010.x. [DOI] [PubMed] [Google Scholar]
- Marcus AC, Morra ME, Bettinghaus E, Crane LA, Cutter G, Davis S, et al. The Cancer Information Service Research Consortium: An emerging laboratory for cancer control research. Prev Med. 1998;27(5):S3–S15. doi: 10.1006/pmed.1998.0245. [DOI] [PubMed] [Google Scholar]
- Marcus AC, Garrett KM, Kulchak-Rahm A, Barnes D, Dortch W, Juno S. Telephone counseling in psychosocial oncology: A report from the Cancer Information and Counseling Line. Patient Educ Couns. 2002;46:267–275. doi: 10.1016/s0738-3991(01)00163-x. [DOI] [PubMed] [Google Scholar]
- Marcus AC, Morra ME, Bright MA, Fleisher L, Kreps G, Perocchia R. The CIS model for collaborative research in health communications: A brief retrospective from the current generation of research. Journal of Health Communication. 2005;10:235–245. doi: 10.1080/10810730500263612. [DOI] [PubMed] [Google Scholar]
- Marcus AC, Garrett KM, Cella D, Wenzel L, Brady MJ, Fairclough D, Pate-Willig M, Barnes D, Powell-Emsbo S, Kluhsman BC, Crane L, Sedlacek S, Flynn PJ. Can telephone counseling post-treatment improve psychosocial outcomes among early stage breast cancer patients? Psycho-Oncology. 2010;19(9):923–32. doi: 10.1002/pon.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller SM, Shoda Y, Hurley K. Applying cognitive-social theory to health-protective behavior: Breast self-examination in cancer screening. Psychological Bulletin. 1996;119(1):70–94. doi: 10.1037/0033-2909.119.1.70. [DOI] [PubMed] [Google Scholar]
- Miller SM, Roussi P, Daly M, Buzaglo JS, Sherman KA, Godwin AK, et al. Enhanced counseling for women undergoing BRCA1/2 testing: Impact on subsequent decision making about risk prevention behaviors. Health Education and Behavior; Special Issue on Genetic Risk. 2005 doi: 10.1177/1090198105278758. [DOI] [PubMed] [Google Scholar]
- Mullan F. Re-entry: The educational needs of the cancer survivor. Health Educ Q. 1985;10(suppl):88–94. [PubMed] [Google Scholar]
- Miller SM, Bowen DJ, Croyle RT, Rowland J, editors. Handbook of Cancer Control and Behavioral Science: A Resource for Researchers, Practitioners and Policy Makers. Washington DC: American Psychological Association; 2009. [Google Scholar]
- National Cancer Institute. Facing Forward Series: Life After Cancer Treatment. Bethesda, MD: 2002. (NIH Publication No. 10-2424). [Google Scholar]
- O’Connor AM. Validation of a decisional conflict scale. Medical Decision Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- O’Connor AM, Llewellyn-Thomas HA, Sawka C, Pinfold SP, To T, Harrison DE. Physicians’ opinions about decision aids for patients considering systemic adjuvant therapy for axillary-node negative breast cancer. Patient Education and Counseling. 1997;30(2):143–53. doi: 10.1016/s0738-3991(96)00948-2. [DOI] [PubMed] [Google Scholar]
- O’Connor AM, Fiset V, Degrasse C, Graham ID, Evans W, Stacey D, et al. Decision aids for patients considering options affecting cancer outcomes: Evidence of efficacy and policy implications. J Natl Cancer Inst Monogr. 1999;25:67–80. doi: 10.1093/oxfordjournals.jncimonographs.a024212. [DOI] [PubMed] [Google Scholar]
- O’Connor AM, Legare F, Stacy D. Risk communication in practice: the contribution of decision aids. BMJ. 2003;327(7417):736–40. doi: 10.1136/bmj.327.7417.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor AM, Llewellyn-Thomas HA, Flood BA. Modifying unwarranted variations in health care: Shared decision making using patient decision aids (A review of the evidence base for shared decision making) Health Affairs. 2004:63–72. doi: 10.1377/hlthaff.var.63. [DOI] [PubMed] [Google Scholar]
- O’Connor AM, Bennett CL, Stacey D, Barry M, Col NF, Eden KB, Entwistle VA, Fiset V, Holmes-Rovner M, Khangura S, Llewellyn-Thomas H, Rovner D. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD001431. doi: 10.1002/14651858.CD001431.pub2. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR, Gonzalez JS, Molton I, Carver CS, Antoni MH, et al. Perceived stress management skill mediates the relationship between optimism and positive mood following radical prostatectomy. Health Psychology. 2003;22:220–222. [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR, Molton I, Gonzalez JS, Kinsinger D, Roos BA, Carver CS, Schneiderman N, Antoni MH. Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer. 2004;100:192–200. doi: 10.1002/cncr.11894. [DOI] [PubMed] [Google Scholar]
- PewInternet. Generations 2010: A Project of the PewResearchCenter. http://pewinternet.org/Reports/2010/Generations-2010.aspx.
- Rees CE, Bath PA. The information needs and source preferences of women with breast cancer and their family members. J Advanced Nursing. 2000;31:833–841. doi: 10.1046/j.1365-2648.2000.01341.x. [DOI] [PubMed] [Google Scholar]
- Ronis DL. Conditional health threats: Health beliefs, decisions and behaviors among adults. Health Psychology. 1992;11(2):127–134. doi: 10.1037//0278-6133.11.2.127. [DOI] [PubMed] [Google Scholar]
- Rotter JB. Social Learning and Clinical Psychology. Englewood Cliffs, NJ: Prentice-Hall; 1954. [Google Scholar]
- Schag CC, Heinrich RL, Aadland R, Ganz PA. Assessing problems of cancer patients: Psychometric properties of the Cancer Inventory of Problem Situations. Health Psychology. 1990;9:83–102. doi: 10.1037//0278-6133.9.1.83. [DOI] [PubMed] [Google Scholar]
- Schag CAC, Ganz PA, Polinsky ML, Freol C, Hirji K, Peterson L. Characteristics of women at risk for psychosocial distress in the year after breast cancer. Journal of Clinical Oncology. 1993;11:783–793. doi: 10.1200/JCO.1993.11.4.783. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Helgeson VS, Schulz R, Colvin S, Berga S, Bridges MW, Knapp J, Gerszten K, Pappert WS. Interventions to enhance physical and psychological functioning among younger women who are ending nonhormonal adjuvant treatment for early-stage breast cancer. Journal of Clinical Oncology. 2005;23:4298–4311. doi: 10.1200/JCO.2005.05.362. [DOI] [PubMed] [Google Scholar]
- Shepherd HL, Tattersall MH, Butow PN. Physician-identified factors affecting patient participation in reaching treatment decisions. J Clin Oncol. 2008;26:1724–1731. doi: 10.1200/JCO.2007.13.5566. [DOI] [PubMed] [Google Scholar]
- Squires L, Rutten LJF, Treiman K, Bright MA, Hesse B. Cancer patient’s information needs across the cancer care continuum: Evidence from the Cancer Information Service. Journal of Health Communication. 2005;10:15–34. doi: 10.1080/10810730500263620. [DOI] [PubMed] [Google Scholar]
- Stalmeier PF, van Tol-Geerdink JJ, van Lin NJ, Schimmel E, Huizenga H, van Daal WA, Leer JW. Doctors’ and patients’ preferences for participation and treatment in curative prostate cancer radiotherapy. J Clin Oncol. 2007;25:3096–3100. doi: 10.1200/JCO.2006.07.4955. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Krishnan L, Collins CA. Form or function? 1. Subjective cosmetic and functional correlates of quality of life in women treated with breast-conserving surgical procedures and radiotherapy. Cancer. 2001;91:2273–2281. [PubMed] [Google Scholar]
- Stanton AL, Danoff-Burg S, Sworowski LA, Collins CA, Branstetter AD, Rodriguez-Hanley A, Kirk SB, Austenfeld JL. Randomized, controlled trial of written emotional expression and benefit-finding in breast cancer patients. Journal of Clinical Oncology. 2002;20:4160–4168. doi: 10.1200/JCO.2002.08.521. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Ganz PA, Rowland JH, Meyerowitz BE, Krupnick JL, Sears SR. Promoting adjustment following treatment for cancer. Cancer. 2005a;104(11 Suppl):2608–2613. doi: 10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Ganz PA, Kwan L, Meyerowitz BE, Bower JE, Krupnick JL, Rowland JH, Leedham B, Belin TR. Outcomes from the Moving Beyond Cancer psychoeducational, randomized, controlled trial with breast cancer patients. Journal of Clinical Oncology. 2005b;23:6009–6018. doi: 10.1200/JCO.2005.09.101. [DOI] [PubMed] [Google Scholar]
- Stewart MA. Effective physician-patient communication and health outcomes: A review. Can Med Assoc J. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- Sundin EC, Horowitz MJ. Impact of Event Scale: Psychometric properties. British Journal of Psychiatry. 2002;180:205–209. doi: 10.1192/bjp.180.3.205. [DOI] [PubMed] [Google Scholar]
- Sutton RL. Adjuvant Care. Cutis. 1982;29(6):591. [PubMed] [Google Scholar]
- Ward JAD, Baum S, Ter Maat J, Thomsen CA, Maibach EW. The value and impact of the Cancer Information Service Telephone Service. Part 4. Journal of Health Communication. 1998;3(Suppl):50–70. doi: 10.1080/108107398127256. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller S. A 12-item short-form health survey (SF-12): Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Whelan T, Levine M, Willan A, et al. Effect of a decision aid on knowledge and treatment decision making for breast cancer surgery: a randomized trial. Journal of the American Medical Association. 2004;292:435–441. doi: 10.1001/jama.292.4.435. [DOI] [PubMed] [Google Scholar]
- Wilson SE, Andersen MR, Meischke H. Meeting the needs of rural breast cancer survivors: what still needs to be done. J Women’s Health and Gender-Based Medicine. 2000;9:667–677. doi: 10.1089/15246090050118198. [DOI] [PubMed] [Google Scholar]
- Wise M, Han JY, Shaw B, McTavish F, Gustafson DH. Effects of using online narrative and didactic information on healthcare participation for breast cancer patients. Patient Education and Counseling. 2008;70:348–356. doi: 10.1016/j.pec.2007.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH, Chan EC, Harris R, Sheridan SL, Braddock CH, Kaplan RM, et al. Promoting informed choice: transforming health care to dispense knowledge for decision making. Ann Intern Med. 2005;143(4):293–300. doi: 10.7326/0003-4819-143-4-200508160-00010. [DOI] [PubMed] [Google Scholar]
- Woolf SH. Shared decision-making: the case for letting patients decide which choice is best. J Fam Pract. 1997;45(3):205–208. [PubMed] [Google Scholar]
- Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement systems. J Pain Symptom Manage. 1997;13:63–74. doi: 10.1016/s0885-3924(96)00274-6. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]


