Abstract
Safety-net hospitals rely on Disproportionate Share Hospital (DSH) payments to help cover uncompensated care costs and underpayments by Medicaid (known as Medicaid shortfalls). The Affordable Care Act (ACA) anticipates that insurance expansions will increase safety-net hospitals’ revenues, and reduces DSH payments accordingly. We examined the impact of the ACA’s Medicaid DSH reductions on California public hospitals’ financial stability by estimating how total DSH costs (uncompensated care costs and Medicaid shortfalls) will change as a result of insurance expansions and the offsetting DSH reductions. Decreases in uncompensated care costs due to the ACA insurance expansion may not match the ACA’s DSH reductions because of the high number of residually uninsured patients, low Medicaid reimbursement, and medical cost inflation. Taking these three factors into account, we estimate that California public hospitals’ total DSH costs will increase from $2.044 billion in 2010 to $2.363 billion in 2019, with unmet DSH costs of $1.381 billion to $1.537 billion.
Safety-net hospitals care for the most vulnerable patients in our health care system. In California, 20 acute care public hospitals anchor the safety net, providing a large share of statewide inpatient and outpatient hospital care to the uninsured (44 percent and 65 percent respectively) and to Medicaid patients (18 percent of inpatient and 34 percent of outpatient care).1 These hospitals operate more than half of California’s Level 1 Trauma Centers and one-quarter of the state’s burn centers, and lead regional disaster response. All are teaching hospitals, training thousands of future doctors, nurses, and allied health professionals.
Many of these hospitals are located in low-income communities with few privately insured patients. Overall, 18 percent of their discharges are for the uninsured and 41 percent are covered by Medicaid.1 Many of California’s public hospitals are financially vulnerable because of this heavy burden of uncompensated care and the state’s historically low Medicaid reimbursement rates,2 which result in Medicaid shortfalls (the amount that Medicaid payments fall short of actual hospital costs for care).
One of the primary purposes of the Affordable Care Act (ACA) is to expand health insurance coverage. California is aggressively implementing the ACA, with 1.5 million uninsured residents already enrolling in Medicaid under the expansions or deemed eligible.3 The extent to which safety-net hospitals will retain their newly insured patients is not known. In previous Medicaid expansions, some patients left the safety net and sought care at private hospitals instead.4 However, after the recent insurance expansion in Massachusetts, safety-net hospitals retained inpatient volume and gained outpatient visits.5 To ensure that the ACA increases Medicaid patient volumes (and thus revenues) at California safety-net hospitals, the state passed legislation that: 1) requires Medicaid Managed Care plans to preferentially assign newly eligible Medicaid patients to county health systems and 2) increases Medicaid payments to county hospitals to cover 100 percent of costs (“cost-based reimbursement”) for newly eligible Medicaid individuals under the ACA.6 However, public hospitals in the state will continue to receive lower reimbursement rates and experience Medicaid shortfalls for previously eligible Medicaid individuals, which include children, pregnant women, parents, and the expensive elderly and disabled populations.
California’s public safety-net hospitals depend heavily on federal Medicaid Disproportionate Share Hospital (DSH) payments, which are supplemental payments to hospitals that treat large numbers of low-income patients, to offset uncompensated care costs and Medicaid shortfalls. Currently, the federal government disburses $11.5 billion annually in DSH payments to states, of which $1.1 billion is directed to California.7 Without DSH payments and with no other actions or adjustments by public hospitals, states or counties to offset DSH declines, the average operating margin of safety-net hospitals nationwide would fall from +2.3 percent to −6.1 percent.8
In California, DSH payments to public hospitals currently only meet part of their “total DSH costs,” which include the uncompensated care costs and Medicaid shortfalls that the hospitals report to claim DSH funds. Their residual DSH costs that are not met by DSH payments are covered by county and state funding.
The ACA’s authors assumed that the expansion of insurance coverage would generate increased revenue for safety-net hospitals, decreasing their need for DSH payments. To help cover the cost of Medicaid expansion, the ACA progressively reduces Medicaid DSH payments. DSH reductions were scheduled to begin in 2014 under the ACA, but Congress recently delayed the DSH cuts twice under the Bipartisan Budget Act of 2013 and the Protecting Access to Medicare Act of 2014. They will now start at $1.8 billion nationwide (16 percent of current federal DSH spending) in 2017 and reach $4.7 billion (41 percent of current spending) for fiscal years 2018 through 2020 and $5 billion by 2023. The cuts were extended through fiscal year 2024, when they are slated to drop to $4.4 billion.
Previous national analysis suggested large statewide average reductions in DSH payments but did not evaluate how these reductions will specifically affect safety-net hospitals.9 We examined the impact of the new policy on the financial stability of California safety-net hospitals by 1) modeling how many newly eligible Medicaid patients will remain at safety-net hospitals following the expansions, 2) projecting the hospitals’ uncompensated care costs and Medicaid shortfalls in 2019 after the ACA’s insurance expansion under different Medicaid payment scenarios and 3) estimating the extent to which California’s DSH allocation will meet the hospitals’ total DSH costs in 2019.
Study Data and Methods
Our analysis focuses on the 20 acute care public hospitals that received 98.5 percent of California’s Medicaid DSH allocation in 2010. This total includes 14 county hospitals and six University of California hospitals (Exhibit 1). We excluded the one public rehabilitation hospital whose utilization and costs patterns are substantially different from California’s other public hospitals.
EXHIBIT 1.
Characteristics Of Twenty Acute Care Public Hospitals In California, 2010
| Acute and rehabilitation discharges | Outpatient visits | ||||||
|---|---|---|---|---|---|---|---|
| Hospital | Medicaid DSH payment ($) |
Total | Medicaid (%) |
Uninsured (%) |
Total | Medicaid (%) |
Uninsured (%) |
| Alameda County | 72,534,623 | 10,895 | 53.7 | 30.9 | 344,674 | 42.8 | 31.9 |
| Arrowhead Regional | 63,713,538 | 20,293 | 54.0 | 22.1 | 206,032 | 49.6 | 33.6 |
| Contra Costa Regional | 49,716,756 | 8,479 | 41.4 | 32.4 | 463,503 | 32.5 | 22.0 |
| Kern | 51,462,718 | 11,878 | 61.4 | 20.6 | 154,343 | 52.2 | 34.4 |
| LA County and USC | 211,818,105 | 33,412 | 47.1 | 33.4 | 532,596 | 33.4 | 49.6 |
| LA County Olive View–UCLA | 69,826,356 | 14,414 | 56.2 | 33.1 | 223,950 | 26.4 | 57.3 |
| LA County Harbor-UCLA | 90,224,869 | 23,068 | 52.3 | 31.1 | 306,518 | 34.5 | 52.2 |
| Natividad | 11,269,421 | 7,904 | 59.8 | 9.7 | 134,676 | 52.5 | 20.5 |
| Riverside County Regional | 58,321,999 | 24,013 | 45.5 | 17.3 | 268,466 | 37.4 | 41.4 |
| San Francisco General Hospital | 67,987,426 | 14,794 | 38.8 | 16.3 | 472,704 | 39.0 | 27.6 |
| San Joaquin General Hospital | 30,971,675 | 8,601 | 62.0 | 19.1 | 181,943 | 48.9 | 29.4 |
| San Mateo | 25,133,524 | 2,822 | 39.7 | 17.7 | 265,725 | 38.4 | 30.5 |
| Santa Clara Valley | 105,937,912 | 23,433 | 54.6 | 21.7 | 868,366 | 50.8 | 27.3 |
| Santa Monica-UCLA | 6,759,435 | 16,099 | 14.0 | 4.0 | 94,636 | 9.2 | 7.4 |
| UC Davis | 43,853,262 | 27,980 | 31.0 | 8.0 | 927,057 | 7.8 | 2.1 |
| UC Irvine | 47,886,558 | 16,389 | 35.2 | 9.6 | 415,462 | 35.2 | 9.6 |
| UCLA Ronald Reagan | 9,377,472 | 24,695 | 21.9 | 2.8 | 703,575 | 7.2 | 1.9 |
| UC San Diego | 43,746,761 | 24,183 | 27.7 | 14.6 | 434,945 | 13.2 | 9.1 |
| UC San Francisco | 17,869,905 | 30,563 | 25.5 | 2.5 | 806,404 | 14.1 | 0.6 |
| Ventura County | 28,053,446 | 13,878 | 48.9 | 19.5 | 181,825 | 36.5 | 24.6 |
| Total | 1.106 billion | 361,745 | 41.2 | 17.8 | 8,027,819 | 29.3 | 21.3 |
SOURCE: Medicaid DSH payment data: California Department of Health Care Services; patient demographics: California Office of Statewide Health Planning and Development Patient Discharge Data; utilization and payer mix: hospitals' Chief Financial Officers; all other data: California Office of Statewide Health Planning and Development Hospital Annual Financial Data.
The primary outcome was the “total DSH costs,” or the costs reported by public hospitals that are eligible for DSH payments. These include uncompensated care costs (including charity care and excluding bad debt) as well as shortfalls in payments for Medicaid Managed Care and Medicaid psychiatric care delivered in inpatient and outpatient settings.
To estimate total DSH costs in 2019, we first established estimates of 2019 encounters by: 1) projecting inpatient and outpatient encounters in 2019 based on current utilization and accounting for changes in insurance status under the ACA as well as for overall population growth; and 2) refining these projections by applying estimates of patient retention obtained from the public hospitals’ Chief Financial Officers. We then estimated the costs or shortfalls associated with these encounters by: 3) calculating current costs or shortfalls per inpatient and outpatient encounter; 4) applying inflation estimates to project 2019 costs per encounter; and 5) multiplying projected encounters by projected costs or shortfalls per encounter to estimate total DSH costs in 2019.
Next, we used the DSH regulation released by the Centers for Medicaid and Medicare Services10 to estimate California’s DSH reduction in 2019 under the ACA. We subtracted the final DSH allocation from the total DSH costs to determine the “residual DSH costs” of California’s public hospitals that were not covered by DSH payments.
Future Utilization and Total DSH Costs
To project the number of 2019 encounters, we used hospital-reported counts of Medicaid and uninsured patient discharges and outpatient visits in 2010. We then applied regional estimates of insurance take-up under ACA expansions based on the UC Berkeley/UCLA California Simulation of Insurance Markets (CalSIM) model to project shifts in insurance coverage in 2019 among each hospital’s current patient population.11 These take-up estimates take into account behavior by individuals and companies in response to provisions of the ACA, including insurance expansions. We adjusted for expected changes in inpatient admissions due to changes in insurance status, but assumed changes in insurance status would not affect outpatient visits. We inflated both inpatient and outpatient projected encounters to account for expected population growth.12
To establish a starting point or benchmark for our model of patient encounters, we first estimated the number of inpatient and outpatient encounters in 2019 at each hospital assuming that hospitals retained all of their current patients (regardless of changes in insurance status due to the ACA). Then, we asked safety-net hospitals’ Chief Financial Officers to estimate the percent of their projected inpatient admissions and outpatient visits they expected their hospital to retain in 2019 for each payer type. They were instructed to base their estimates on expected market competition, extent of contracting with managed care plans, and any internal analysis. In the model presented here, our projections are adjusted for their estimates.
Four hospitals did not supply retention estimates; for these we applied retention estimates from a comparable public hospital that had reported their own estimates. We selected comparable public hospitals based on the same ownership (county or University of California) and similar payer mix.
To calculate the current average costs or shortfalls per inpatient and outpatient encounter, we used data on the uncompensated care costs per uninsured encounter and on the shortfalls (difference between revenues and costs) per Medicaid encounter from audited hospital financial reports for fiscal year 2010. We adjusted these hospital-specific average costs and shortfalls per encounter for projected inflation in health care costs to generate 2019 cost estimates (3.7 percent inflation in 2011 and 4.3 percent annually from 2012 through 2019).13,14
Finally, we multiplied our projection of each hospital’s number of inpatient and outpatient encounters for 2019 by that hospital’s average costs and shortfalls per encounter, to estimate the 2019 total DSH costs for each hospital.
DSH Reduction and Final DSH Allocation
In September 2013, the Centers for Medicare and Medicaid Services (CMS) released a regulation that would have guided the reduction of Medicaid DSH payments across states in 2014 and 2015.15 As noted, the DSH cuts have since been delayed by Congress. CMS intends to revisit this regulation before the DSH cuts take effect in 2017. Because the current CMS regulation represents the most current information available and reflects extensive calculations and stakeholder engagement by CMS staff including responses to 87 public comments, we simulated the impact on California’s DSH reduction and final DSH allocation assuming the regulation continues unchanged until 2019.
The DSH regulation divides states into two groups: 17 “low DSH” states and 33 “regular DSH” states (including California) based on the size of each state’s DSH allotment relative to its total Medicaid expenditures. For instance, to qualify as a “low DSH” state, the state’s DSH allotment had to have been less than 3 percent of the state’s total Medicaid expenditures in 2000. The regulation then specifies a method for reducing each state’s initial DSH allocation by calculating how the states within each group compares on three equally weighted factors: 1) the state’s percentage of uninsured; 2) how well the state targets DSH payments to hospitals with high percentages of Medicaid inpatients, and 3) how well the state targets DSH payments to hospitals with high levels of uncompensated care. Under this formula, California, a “regular DSH” state, will experience greater DSH reductions if other regular DSH states have large residual uninsured populations or improve their targeting of DSH payments to safety-net hospitals.
We used the planned 2014 DSH reductions from the regulation, as well as other available relevant data, to simulate the size of California’s DSH reductions in 2019. In 2014, California would have experienced a relatively small DSH reduction because it targets DSH narrowly to hospitals with heavy uncompensated care burdens (just 4 percent of the state’s hospitals). We model two alternative scenarios for 2019 to address uncertainty about whether other states will seek to minimize their DSH reductions by improving their DSH targeting to hospitals with high levels of uncompensated care. Scenario A assumes that other states do not change their DSH targeting, so California’s proportion of the total national DSH reduction would remain relatively small. Scenario B assumes that other states improve their DSH targeting. As a result, California would experience a greater share of the total national DSH reduction. We describe in detail how we estimated the DSH reductions for each scenario in the online Supplemental Appendix.16
Use of patient level data was reviewed and approved by the UCLA and state institutional review boards.
Limitations
Our study has several limitations. Our results may not be generalizable because we focus on a single state that is likely to face relatively smaller DSH reductions because it already targets DSH narrowly to safety-net hospitals. We used projections of future increases in health care costs from the Medicare Board of Trustees, which take into account the recent slowdown in health care spending. If health care spending accelerates and inflation is greater than we modeled based on best available estimates, total DSH costs as well as residual uncompensated care costs and shortfalls could be significantly larger than our projections. In addition, we assume that hospitals’ operations and existing cost structures will largely remain the same. If safety-net hospitals become more efficient, however, it could decrease their total DSH costs and residual DSH costs. We also had to assume that changes in insurance status would not affect the volume of outpatient visits due to limitations in our data. Because patients who obtain Medicaid are likely to increase their outpatient visits, we probably underestimated outpatient costs. We do not believe that our conservative outpatient cost estimates substantially changed our total cost estimates because inpatient costs accounted for a much greater share of total costs. Finally, our analysis assumes that the current DSH regulation is extended to 2019 unchanged. However, CMS is likely to revisit the regulation and could alter the DSH reduction formula. Our projections are based on the most current information available but will need to be revised if or when the formula is altered.
Study Results
Total DSH Costs
California’s public safety-net hospitals had total DSH costs of $2.044 billion in 2010, of which $1.106 billion was met by DSH payments. The residual DSH costs of $937 million were covered by other county and state funding sources.17
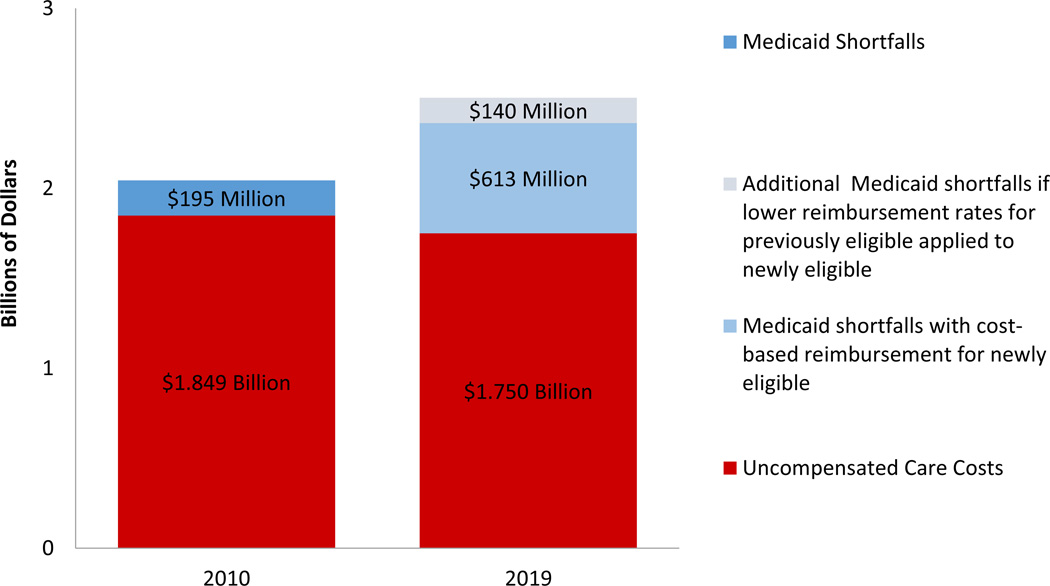
If the ACA had not passed, we estimate that the total DSH costs of these hospitals would have risen to $3.816 billion in 2019 because medical cost inflation would have increased the costs of care for the uninsured and Medicaid shortfalls. The ACA will reduce the uncompensated care costs at California’s safety-net hospitals by $1.313 billion compared to costs in the absence of the law. We project that total DSH costs under ACA will still rise to $2.363 to $2.503 billion in 2019 (Exhibit 2).
EXHIBIT 2.
Total Disproportionate-Share Hospital (DSH) Costs of Twenty Acute Care Public Hospitals In California, 2010 And 2019
SOURCE: Authors’ analysis of data from California Office of Statewide Health Planning and Development; public hospitals’ Chief Financial Officers, California Simulation of Insurance Markets (CalSIM) Model (Note 10 in text), and California Department of Finance (Note 11 in text).
NOTES: 2019 Medicaid shortfalls are calculated under two payment scenarios. In the first, California continues "cost-based reimbursement," which pays county hospitals 100 percent of costs for the newly Medicaid eligible under Affordable Care Act, resulting in lower Medicaid shortfalls. In the second, California changes its policy and applies the lower reimbursement rates for the exising eligible to the newly eligible, resulting in greater total Medicaid shortfalls.
Under the ACA, uncompensated care costs for the uninsured are projected to decrease from $1.849 billion in 2010 to $1.750 billion in 2019. Conversely, shortfalls in Medicaid payments will rise substantially from $195 million in 2010 to $613 million by 2019 under the law. Medicaid shortfalls in California will be restricted to previously eligible Medicaid individuals because of California’s recent policy of cost-based reimbursement for the newly Medicaid eligible. However, if California changes this policy and applies the lower reimbursement rates for the existing eligible to the newly eligible, projected shortfalls will reach $753 million in 2019. This policy change becomes more likely after 2016, when the full 100 percent federal match for new Medicaid patients is reduced to 95 percent, eventually decreasing to 29 percent by 2020.
DSH Reduction and Final DSH Allocation
We estimate that California’s initial 2019 DSH allocation (before ACA reductions) would have been $1.290 billion. If the CMS regulation is continued unchanged, we project that California’s final DSH allocation in 2019 will be $982 million under Scenario A (no states change their DSH targeting). Under Scenario B (states improve their DSH targeting), California’s final DSH allocation is projected to fall to $826 million.
Residual DSH Costs
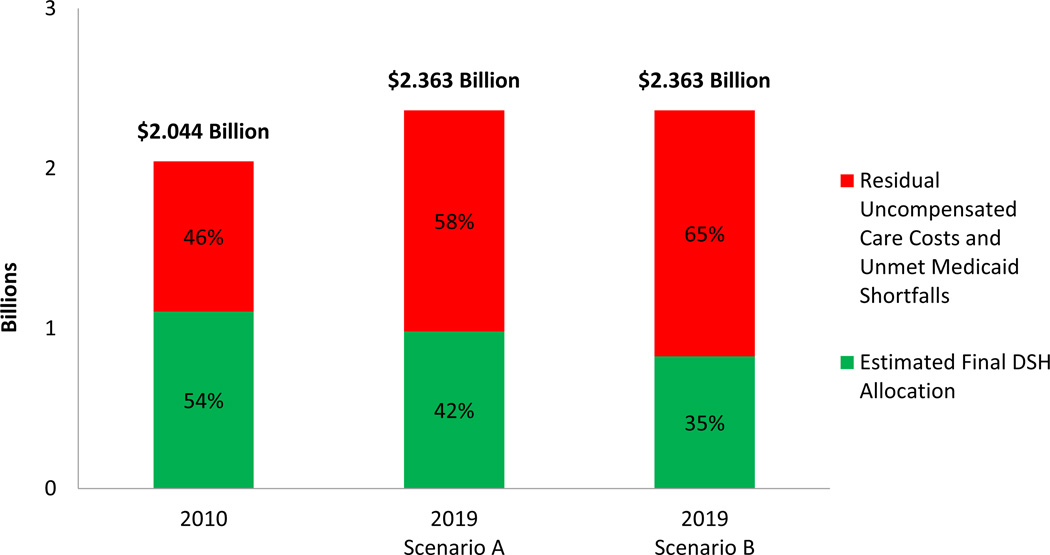
In 2010, California’s DSH allocation of $1.106 billion met 54 percent of the public hospitals’ total DSH costs. Under California’s new policy of reimbursing county hospitals for 100 percent of costs of the newly eligible Medicaid population, California’s estimated final DSH allocation in 2019 will meet 42 percent and 35 percent of the hospitals’ total DSH costs under Scenario A and Scenario B respectively (Exhibit 3).
EXHIBIT 3.
California’s Estimated Final Disproportionate-Share Hospital (DSH) Allocation As A Proportion Of Total DSH Costs, Assuming Cost-Based Reimbursement For Those Newly Eligible For Medicaid, 2010 And 2019
SOURCE: Authors’ analysis of data from California Office of Statewide Health Planning and Development; public hospitals’ Chief Financial Officers, Centers for Medicare and Medicaid Servies (Note 9 in text), California Simulation of Insurance Markets (CalSIM) Model (Note 10 in text), and California Department of Finance (Note 11 in text).
NOTES: “Total DSH costs” are the total uncompensated care costs and Medicaid shortfalls reported by the public hospitals to claim DSH payments. Total DSH costs are broken out into the amount of the DSH allocation, and the residual DSH costs after the DSH allocation is applied. This analysis assumes California continues "cost-based reimbursement," which pays county hospitals 100 percent of costs for the newly eligible Medicaid population under Affordable Care Act.
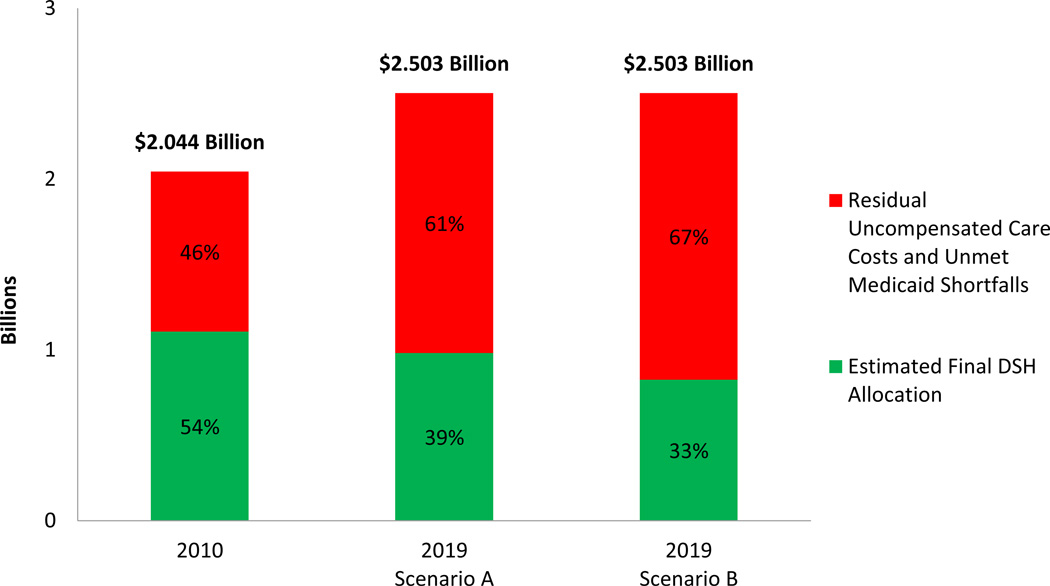
If California changes its cost-based reimbursement policy and applies its lower Medicaid reimbursement rates for the previously eligible to the newly eligible in 2019, California’s estimated final DSH allocation in 2019 will only meet 39 percent of the hospitals’ total DSH costs under Scenario A and 33 percent under Scenario B (Exhibit 4) in 2019.
EXHIBIT 2.
California’s Estimated Final Disproportionate-Share Hospital (DSH) Allocation As A Proportion Of Total DSH Costs, Assuming Lower Reimbursement Rates For Those Newly Eligible For Medicaid, 2010 And 2019
SOURCE: Authors’ analysis of data from California Office of Statewide Health Planning and Development; public hospitals’ Chief Financial Officers, Centers for Medicare and Medicaid Servies (Note 9 in text), California Simulation of Insurance Markets (CalSIM) Model (Note 10 in text), and California Department of Finance (Note 11 in text).
NOTES: This analysis assumes that California changes its current cost-based reimbursement policy for county hospitals and instead applies its lower Medicaid reimbursement rates for the previously eligible Medicaid population to the newly eligible Medicaid population under Affordable Care Act.
Discussion
Based on our analysis of current policy and trends, safety-net hospitals in California could face $1.381 billion to $1.537 billion in residual uncompensated care costs and Medicaid shortfalls in 2019. This assumes the DSH reductions are implemented as currently proposed and the state continues cost-based payments for newly Medicaid eligible patients. These residual DSH costs would be substantially greater than the $937 million covered by other county and state funding sources in 2010, creating a DSH funding gap for California safety-net hospitals.
By expanding coverage, the ACA will substantially decrease the size of the uninsured population. But, because health care costs keep rising due to inflation, the law will have less impact than expected on the amount of uncompensated care costs at safety-net hospitals. California will further bolster safety-net hospital finances by implementing cost-based reimbursement for the newly Medicaid eligible. Despite these positive trends for safety-net hospitals, total DSH costs will grow after implementation of the ACA, primarily because of the expected growth in health care costs due to inflation.
California will likely have a large remaining uninsured population of 3.1 to 4 million Californians in 2019.18 Uncompensated care costs for this population will rise due to inflation in health care costs. In addition, approximately 2.5 million Californians were previously eligible for Medicaid before the ACA18 (including children, pregnant women, parents, and the elderly and disabled population) but not enrolled because of barriers and lack of information. Due to California’s extensive advertising and outreach, many of these previously eligible individuals have already enrolled in Medicaid.3 Because cost-based reimbursement only applies to the newly Medicaid eligible population under the ACA, county hospitals will receive lower reimbursement rates for these previously eligible Medicaid individuals, which will increase Medicaid shortfalls.
Policy Implications
Over the past decade, DSH payments have lagged behind hospitals’ DSH costs because the payments increased at rates lower than health care cost inflation. The Affordable Care Act’s DSH reductions greatly accelerate this trend. After ACA implementation, the DSH funding gap will widen as the DSH reductions are phased in and total DSH costs rise, primarily due to inflation. Therefore, the rate of health care spending growth will help determine the size of the DSH funding gap for safety-net hospitals.
Economists disagree on whether the slowdown in health care spending from 2007 to the present was due to the recession or was driven by structural changes in health care delivery that will continue to contain costs after the recession.19,20 Cutler and Sahni contend that factors such as decreases in prescription drug expenditures, fewer developments in imaging technology, and improved provider efficiency driven in part by ACA provisions, such as penalties for high readmission rates and hospital-acquired infections, contributed to the slowdown.21 The ACA also launched a multitude of demonstrations and pilot programs including Accountable Care Organizations and bundled payments that could generate cost savings.
To improve quality and contain costs, California also created a Delivery System Reform Incentive Pool (DSRIP) for its public hospitals under its most recent Section 1115 Medicaid waiver.22 DSRIP provides up to $3.3 billion over five years in matching federal funds to California safety-net hospitals that implement projects in four categories: infrastructure development, innovation and redesign, population-focused improvement, and urgent improvements in care. Many of these projects aim to decrease readmissions and reduce hospital-acquired infections. By deploying DSRIP funds to become more efficient, these hospitals may decrease their total DSH costs.
However, if health care spending accelerates as the economy recovers despite these initiatives, federal and state policymakers may need to consider more comprehensive legislation to control health care costs.
California safety-net hospitals may be better positioned to absorb the DSH reductions than hospitals in other states because they rely on a patchwork of county, state, and federal funding streams in addition to DSH payments.23 California counties have a legal obligation to provide health care to their indigent populations, which strengthens the safety net24 The state allocates sales tax revenues and vehicle license fees directly to the counties to fund indigent care and help them meet this obligation..23 Some counties also contribute county tax revenues. However, this funding has not kept pace with inflation and the state is implementing steep cuts in the sales tax revenues and fees that it distributes to counties for indigent care in the next few years.6 As local and state funding has decreased, California has obtained additional federal funding including $6 billion for inpatient Medicaid supplemental payments to private hospitals from July 2011 to the end of 2013.25. Policymakers could close the DSH funding gap by increasing state or county subsidies or working with CMS to restructure other federal supplemental payments such as the inpatient Medicaid supplemental payments.
Finally, California’s future DSH funding gap will depend on any revisions that CMS makes to the DSH reduction formula when it revisits the regulation. If CMS increases the weight of the state’s percentage of uninsured in the formula, then California would experience a greater DSH reduction and a larger DSH funding gap. Conversely, if CMS increases the weight of a state's effectiveness in directing its DSH payments, then California is likely to absorb a smaller DSH reduction and face a smaller DSH funding gap.
Although California’s safety-net hospitals face challenges, the situation may be much worse in other states that do not expand Medicaid. The Affordable Care Act’s DSH reductions were based on the premise that all states would expand Medicaid, covering an additional 17 million low-income individuals.26 The Supreme Court’s decision that Medicaid expansion is optional for states27 is expected to result in at least six million fewer Americans obtaining Medicaid.26 If states, such as Texas and Louisiana, with many DSH-dependent safety-net hospitals continue to opt out of Medicaid expansion, their hospitals may experience DSH reductions similar to California without the counter-balancing increase in Medicaid revenue and decrease in uncompensated care costs.28
Safety-net hospital leaders and state policymakers could consider several strategies to close their DSH funding gaps. First, hospital leaders in states that widely distribute DSH funds could work with policymakers to target DSH payments more effectively to safety-net hospitals in order to minimize their state’s DSH reductions and protect these hospitals.
Second, states that expand Medicaid under the ACA could adopt California’s policy of paying higher reimbursement rates to safety-net hospitals for the newly eligible Medicaid population. This policy is politically attractive because it would take advantage of 100 percent federal funding and would not require any state funds in the first three years of ACA implementation. To pursue this, the state would need to obtain approval from CMS. Beyond 2016, states would need to cover a small proportion of the cost because federal funding for the newly Medicaid eligible will slowly phase down to 90 percent in 2020.
Finally, safety-net hospital leaders in states opting out of Medicaid expansion may need to seek additional county and state subsidies or federal Medicaid supplemental payments to fill their DSH funding gaps. Georgia’s governor is considering a “state bailout” for safety-net and rural hospitals that would replace all or part of the federal DSH funds that will be lost under the ACA.29
Conclusion
While the Affordable Care Act will reduce the number of uninsured and expand access to health care, the DSH reductions included in the Act combined with ongoing health care cost inflation will create funding gaps that must be filled to ensure the financial stability of safety-net hospitals. Safety-net hospital leaders will need to develop strategies to close funding gaps that account for differences in their local political environments, financial conditions, geography, and payer mix.
Supplementary Material
Acknowledgments
This research was funded by the Robert Wood Johnson Foundation's Clinical Scholars Program. Anna Davis was supported by the National Institutes of Health's National Center for Advancing Translational Science Grant to the University of California Los Angeles (UCLA), Clinical and Translational Science Institute (Grant No. TL1TR000121). Jack Needleman and Dylan Roby received support for the creation of the UC Berkeley and UCLA California Simulation of Insurance Markets (CalSIM) model from the California Endowment and Covered California. Needleman also received support from the Robert Wood Johnson Foundation's Investigator Awards in Health Policy Research program. David Zingmond was supported by the American Cancer Society (Grant No. RSGI-11-005-01-CPHPS). The authors thank the chief financial officers, reimbursement directors, and other staff of California’s public hospitals for providing data and completing surveys. The authors are grateful to Arthur Kellermann and Mitchell Katz for helpful advice on study design and comments on earlier versions of this article. The authors thank Kim Belshe, Andrew Bindman, David Carlisle, Patrick Dowling, and Allan Wecker for their contributions to the study design. The authors gratefully the assistance with data analysis of Xiao Chen, Greg Watson, and Rachel Louie.
Biographies
Katherine Neuhausen (klneuhausen@vcu.edu) is the director of delivery sytem reform in the Office of Health Innovation and a clinical assistant professor in the Department of Family Medicine and Population Health, Virginia Commonwealth University, in Richmond.
Anna C. Davis is a PhD graduate student in the Department of Health Policy and Management, Fielding School of Public Health, University of California, Los Angeles (UCLA).
Jack Needleman is a professor in the Department of Health Policy and Management, Fielding School of Public Health, UCLA.
Robert H. Brook is a professor of medicine and public health in the David Geffen School of Medicine and the Jonathan and Karin Fielding School of Public Health and Co-Director of the Robert Wood Johnson Foundation Clinical Scholars Program, UCLA. He is the distinguished chair in health services at RAND and a professor in the Pardee RAND Graduate School.
David Zingmond is an assistant professor in residence in the Division of General Internal Medicine and Health Services Research, David Geffen School of Medicine, UCLA.
Dylan H. Roby is an assistant professor in the Department of Health Policy and Management and the director of health economics and evaluation research at the Center for Health Policy Research, both in the Fielding School of Public Health, UCLA.
NOTES
- 1.Sacramento (CA): OSHPD; 2011. Oct, [cited 2014 Mar 1]. Author's analysis of California Office of Statewide Health Planning and Development Hospital Annual Financial Data 34th and 35th years [Internet] Available from: http://www.oshpd.ca.gov/HID/Products/Hospitals/AnnFinanData/CmplteDataSet/index.asp. [Google Scholar]
- 2.Zuckerman S, Williams AF, Stockley KE. Trends in Medicaid physician fees, 2003–2008. Health Aff (Millwood) 2009;28:w510–w519. doi: 10.1377/hlthaff.28.3.w510. [DOI] [PubMed] [Google Scholar]
- 3.Covered California. [cited 2014 Mar 1];Strong enrollment numbers released by Covered California and Department of Health Care Services [press release on the Internet] 2014 Feb 19; Available from: http://news.coveredca.com/2014/02/strong-enrollment-numbers-released-by.html#more. [Google Scholar]
- 4.Gaskin DJHJ, Freeman VG. Are urban safety-net hospitals losing low-risk Medicaid maternity patients? Health Serv Res. 2001;36:25–51. [PMC free article] [PubMed] [Google Scholar]
- 5.Ku L, Jones E, Shin P, Byrne FR, Long SK. Safety-net providers after health care reform: lessons from Massachusetts. Arch Intern Med. 2011;171:1379–1384. doi: 10.1001/archinternmed.2011.317. [DOI] [PubMed] [Google Scholar]
- 6.California State Assembly Bill No. 85; 2013. Article 6.6, Medicaid expansion under the federal Affordable Care Act.
- 7.Centers for Medicare and Medicaid Services. Medicaid Program; Disproportionate Share Hospital allotments and Institutions for Mental Diseases Disproportionate Share Hospital limits for FY 2012, and preliminary FY 2013 Disproportionate Share Hospital allotments and limits. Fed Regist. 2013;78(144):45217–45231. [Google Scholar]
- 8.Zaman O, Cummings L, Laycox S. America's safety net hospitals and health systems, 2010: Results of the annual NAPH hospital characteristics survey [Internet] Washington (DC): National Association of Public Hospitals; 2012. May, [cited 2014 Mar 1]. Available from: http://www.naph.org/Main-Menu-Category/Publications/Safety-Net-Financing/2010-NAPH-Characteristics-Report.aspx?FT=.pdf. [Google Scholar]
- 9.Graves JA. Medicaid expansion opt-outs and uncompensated care. N Engl J Med. 2012;367:2365–2367. doi: 10.1056/NEJMp1209450. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Medicare and Medicaid Services. Medicaid Program; State Disproportionate Share Hospital allotment reductions; final rule. Fed Regist. 2013;78(181):57293–57313. [PubMed] [Google Scholar]
- 11.UC Berkeley Center for Labor Research and Education and UCLA Center for Health Policy Research. California Simulation of Insurance Markets (CalSIM) version 1.8: methodology &11 assumptions [Internet] Berkeley (CA): UC Berkeley and UCLA; 2013. Mar, [cited 2014 Mar 1]. Available from: http://healthpolicy.ucla.edu/publications/Documents/PDF/calsim1.8methods.pdf. [Google Scholar]
- 12.California Department of Finance. Report P-2: population projections by race/ethnicity and 5-year age groups, 2010–2060 [Internet] Sacramento (CA): California Department of Finance; 2013. Jan, [cited 2014 Mar 1]. Available from: http://www.dof.ca.gov/research/demographic/reports/projections/P-2/ [Google Scholar]
- 13.Hartman M, Martin AB, Benson J, Catlin A. National health spending in 2011: overall growth remains low, but some payers and services show signs of acceleration. Health Aff (Millwood) 2013;32:87–99. doi: 10.1377/hlthaff.2012.1206. [DOI] [PubMed] [Google Scholar]
- 14.Lew JL, Harris S, Sebelius K, et al. Baltimore (MD): Centers for Medicare and Medicaid Services; 2013. May 31, [cited 2014 Mar 1]. 2013 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. [Internet] Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/Downloads/TR2013.pdf. [Google Scholar]
- 15.Centers for Medicare and Medicaid Services. Medicaid Program; State Disproportionate Share Hospital allotment reductions; proposed rule. Fed Regist. 2013;78(94):28551–28569. [PubMed] [Google Scholar]
- 16.The online Supplemental Appendix is available by clicking on the Supplemental Appendix link in the box to the right of the article online.
- 17.McMahon T, Newman M. California Health Care Almanac. California's health care safety net: a complex web [Internet] Oakland, CA: California HealthCare Foundation; 2013. Apr, [cited 2014 Mar 1]. Available from: http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/C/PDF%20CAHealthCareSafetyNetComplexWeb.pdf. [Google Scholar]
- 18.Lucia L, Jacobs K, Dietz M, Graham-Squire D, Pourat N, Roby D. After millions of Californians gain health coverage under the Affordable Care Act, who will remain uninsured [Internet]? Berkeley (CA): UC Berkeley Center for Labor Research and Education and UCLA Center for Health Policy Research; 2012. Sep, [cited 2013 Mar 1]. Available from: http://laborcenter.berkeley.edu/healthcare/aca_uninsured12.pdf. [Google Scholar]
- 19.Martin A, Lassman D, Whittle L, Catlin A and the National Health Expenditure Accounts Team. Recession contributes to slowest annual rate of increase in health spending in five decades. Health Aff (Millwood) 2011;31:11–22. doi: 10.1377/hlthaff.2010.1032. [DOI] [PubMed] [Google Scholar]
- 20.Levine M, Buntin M. Why Has Growth in Spending for Fee-for-Service Medicare Slowed? Washington, D.C.: Congressional Budget Office; 2013. Aug, [Google Scholar]
- 21.Cutler DM, Sahni NR. If slow rate of health care spending growth persists, projections may be off by $770 billion. Health Aff (Millwood) 2013 May;32:841–850. doi: 10.1377/hlthaff.2012.0289. [DOI] [PubMed] [Google Scholar]
- 22.Harbage P, King ML. A bridge to reform: California's Medicaid Section 1115 waiver [Internet] Sacramento, CA: California HealthCare Foundation; 2012. Oct, [cited 2014 Mar 1]. Available from: http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/B/PDF%20BridgeToReform1115Waiver.pdf. [Google Scholar]
- 23.Belshe K, McConville S. Rethinking the state-local relationship: health care [Internet] Sacramento, CA: Public Policy Institute of California; 2013. Feb, [cited 2014 Mar 1]. Available from: http://www.chcf.org/publications/2012/10/bridge-to-reform. [Google Scholar]
- 24.California HealthCare Foundation. California's safety net: the role of counties in overseeing care [Internet] Oakland, CA: CHCF; 2009. Dec, [cited 2014 Mar 1]. Available from: http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/C/PDF%20CASafetyNetRoleCountiesInCare.pdf. [Google Scholar]
- 25.California State Senate Bill 335; 2011. Medi-Cal: Hospitals Quality Assurance Fee.
- 26.Congressional Budget Office. Washington (DC): CBO; 2012. Jul, [cited 2014 Mar 1]. Estimates for the insurance coverage provisions of the Affordable Care Act updated for the recent Supreme Court decision [Internet] Available from: http://www.cbo.gov/sites/default/files/cbofiles/attachments/43472-07-24-2012-CoverageEstimates.pdf. [Google Scholar]
- 27.National Federation of Independent Business. 2427810. Sebelius, 567 U.S., 2012 WL. 2012 Jun 28;
- 28.Price CC, Eibner C. For states that opt out of Medicaid expansion: 3.6 million fewer insured and $8.4 billion less in federal payments. Health Aff (Millwood) 2013;32:1030–1036. doi: 10.1377/hlthaff.2012.1019. [DOI] [PubMed] [Google Scholar]
- 29.Jones WC. Hospitals could get state bailout. The Newnan Times-Herald. 2014 Jan 15; [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.