Abstract
Results from studies involving exposure to road traffic noise and risk of hypertension are diverse and have seldom reached statistical significance. This study was designed with the aim of investigating whether there is any association between road traffic noise and prevalence of hypertension in an urban adult population. Similar studies have never been reported from India. A cross-sectional study was performed on 909 adults (533 female and 376 male) aged 18–80 years residing in close proximity to roadways in Asansol City. Time-weighted equivalent noise level (Lden) was estimated using a standard modeling platform. Odds for hypertension in relation to traffic noise exposure were estimated by univariate and multifactorial logistic regression. The adjusted odds ratio (OR) for self-reported hypertension was 1.99 (95 % confidence interval (CI) 1.66–2.39) per 5 dB(A) increase of Lden (range 55.1–77.9). A gender-related risk difference was observed among the male (OR 1.81 (1.42–2.31)) and female (OR 2.18 (1.66–2.88)) respondents. For increase in 9 years of age, the odds of hypertension risk increased by 60 % (OR 1.66 (1.43–1.91) among those exposed above Lden 60 dB(A). Vulnerable subgroups were female aged 35–54 years and male aged 45–54 years. The study suggests that a threshold exposure to road traffic noise at Lden > 65 dB(A) for men and Lden > 60 dB(A) in women may be associated with the occurrence of hypertension.
Keywords: Road traffic noise, Hypertension, Blood pressure, Exposure-response relationship, Public health, Environmental risk
Introduction
Urban road traffic is a major source of community noise in both developed and developing countries, and exposure to noise from traffic streams is a growing concern to public health. The World Health Organization addresses noise from the transportation sector as a significant contributor to the environmental burden of disease,1 as chronic exposure to high levels of road traffic noise has been linked to long term, non-auditory physiological disorders such as hypertension and ischemic heart disease.2,3 The pathway linking noise exposure to hypertension may be facilitated through the sympathetic and endocrine stress response model with consequent critical changes in the vascular system with long-term manifestations as cardiovascular diseases.4 Epidemiological studies have documented the association between hypertension and road traffic noise exposure (LAeq24 > 55 dB(A)) in European population.5–7 A recent meta-analysis reported a very modest significant association between road traffic noise and hypertension5 although pooled odds ratio (OR, 95 % CI) was 1.03 (1.01–1.06) per 5 dB(A) increase in LAeq.
Previous studies have recognized the increased risk of hypertension among populations exposed to higher road traffic noise, although the results are mostly heterogeneous.3,5,6 A quantitative relationship built on this hypothesis is somewhat wanting. Reported studies are mostly ambiguous about defining a threshold noise level above which hypertension risk may be predicted. Majority of the results are heterogeneous because of inconsistency in the study design, including subgroup, covariate selection, use of effect modifiers, outcome, and exposure assessment including the type of noise indicator used and group of the exposed and referent groups.2,4 Similar studies in populations other than European is relatively unknown,8 and additionally, none have not been reported in India.
Hypertension is internationally accepted as a significant risk factor for cardiovascular diseases which is associated to disability and premature fatality.9 It has been documented that about 13.5 % deaths worldwide are attributable to hypertension with a prevalence rate of >40 % in the adult population.10 In India, the occurrence of hypertension has been reported at 20.6 % in men and 20.9 % in women with projections of 22.9 and 23.6 % for year 2025, respectively.11 The age-standardized (≥20 years) rate of hypertension is reported to be 30.7 % in the urban regions of western India. Recognition of noise as a risk factor for hypertension is typically wanting from documented noise-health research in Asian countries including India, where urbanization, infrastructural, and transportation sectors have seen momentous intensification during the last few decades. In India, evaluation of health outcomes potentially associated with noise emanation has by far limited to annoyance studies only.12
The aim of this study was to further investigate the association between exposure to residential road traffic noise and occurrence of hypertension in an adult subpopulation of Asansol City in western India. Analysis of gender- and age-specific variability in this relation was also intended.
Methods
Study Design and Respondents
A cross-sectional pilot study was designed and administered on a small sample of adult population residing in close proximity (100 m) from major roadways in Asansol. Adult residents (>18 years) and dwelling in their present household in the last 1 year were inducted for the interview process with prior consent. A comparable appraisal was conducted on a different subpopulation (referent group) dwelling far away from major roads and traffic. Roads with an hourly flow of 400–2000 vehicles (low to moderate traffic) were marked as referent areas and those with >2000 vehicles were designated as potentially higher-exposure locale. Based on a projected prevalence of 20 % hypertensive cases in this subpopulation of the study area and an absolute precision of 5 % with design effect of 1, the requisite sample size was estimated to be 246. For high study accuracy, the actual sample size intended was five times the estimated size at 1000 subjects, and based on this, 1100 households were identified. Among those approached, 119 refused and/or were not available for the study. The final sample which consented to participating in the interview consisted of 909 (533 female and 376 male) individuals, giving a response rate of 82.64 % and a study power of >90 %. Data collection was achieved by a house-to-house personnel visit by trained research personnel using a structured questionnaire. The survey was planned for a citywide evaluation primarily focused on public health, environmental exposures, and disease profile. The anonymous questionnaire broadly consisted of four segments. The first segment was related to sociodemography and living condition, the second segment included exposure-related queries, the third segment was related to lifestyle condition, while the last segment consisted of anthropometric data and disease status of the participants.
The identification of the sampling sites was taken up after a preliminary traffic analysis was conducted in 30 locations. Data collected from sampling points along roads were used for noise modeling (center of road segment between intersections). Residential zone within 100-m radius of the sampling stations was used for household survey. The participants from the two different areas (exposed and referent) were further grouped into different noise exposure categories according to the façade Lden levels. Those living in areas where Lden was <60 dB(A) were marked as the referent group, whereas those with façade Lden levels greater than 60 dB(A) were the exposed group. The interview and data collection took place from June to November 2012.
Assessment of Hypertension and Potential Confounders
Hypertension (high blood pressure) was identified as self-reported diagnosis by a qualified medical practitioner within the last 1 year. Subjects with persistent hypertension and using antihypertensive medications were marked as positive cases. Cases was defined as an affirmative response to two questions: (a) “During the last five years have you been diagnosed with any of these diseases COPD, Diabetes, Kidney Disease, High Total Cholesterol/Heart Disease/High Blood Pressure?” and (b) “During the last one year have you been diagnosed with Hypertension/High Blood Pressure?” Confirmation of hypertensive case was further verified by the last available prescription at the time of interview. A photocopy of the record was requested, which was later verified by a specialist. A hypertensive was marked as a case if the prescription recorded blood pressure level showing either stage 1 (140–159/90–99 mmHg) or stage 2 (≥160/≥100 mmHg).
Information concerning conventional and potential risk factors of hypertension that can confound the association was collected during the survey. Data were collected on gender, age, marital status, education level, physical activity during leisure time (sedentary—not/never active at all; moderately active—weekly/fortnightly workout, run, etc.; active—daily workout, etc.), smoking habits, alcohol consumption (sometimes—weekly/fortnightly or socially; frequently—more than four times a week, 60 to >180 ml of whisky (42 % alcohol)), self-reported stress (dissatisfaction/expectation due to job satisfaction/targets, financial issues, family/marital, health related, etc.), employment, presence of other chronic diseases (diabetes, coronary, pulmonary, or renal), family history of cardiovascular disease below 60 years, and body mass index (BMI). BMI was calculated from body weight (kg) and height (m2) measured during the household visit. Particulars of other variables like bedroom window orientation (facing road or others), house ownership, residence period, noise sensitivity (low—not or minimum sensitivity to noise events; medium—some to moderate reactions; high—highly reactive to even small noise events), noise annoyance, neighborhood satisfaction, and dwelling type (apartment—ground/first floor and higher floors; others—standalone houses, company-provided quarters) were also recorded.
Assessment of Noise Exposure
Outdoor road traffic noise levels during 2012 were estimated for all participant dwellings, using the CORTN13 model using the SoundPLAN Essential-2 (Braunstein-Berndt, GmbH, Germany). The modeled noise was validated with actual field-monitored levels. The noise indicator chosen for this study was the 24 hourly, time-weighted Lden which takes into account the separate exposure periods of the day, evening, and night with appropriate penalties for evening and night time emissions. Traffic data from field was entered into the software along with a digitized base map of the study area to generate noise maps as well as noise levels for selected locations where participants resided. Participants dwelling close to one of the sampling stations were grouped into a similar noise exposure level when individual residential noise was near matching. For this study, the participants’ level of noise exposure was grouped into two categories (<60 dB(A)) according to the facade Lden levels. The choice of 60 dB(A) as cutoff point was due the fact that, firstly, it was close to the median Lden value (62.5 dB(A)) and, secondly, most studies have reported a value of 60 dB(A) for similar investigations.3,4
Statistical Analysis
For quantitative variables like age, BMI, period of residence, and Lden, the Shapiro-Wilk test was used for normality assessment. The test yielded p values of less than 0.001 for all the variables, indicating the absence of any normal distribution. Based on this, the Wilcoxon signed rank sum test for these four variables was performed. Categorical data were subjected to the chi-square (χ2) test to compare between the two exposure groups.
Univariate logistic regression analysis was performed using relevant covariates in relation to hypertension. Those giving significant associations and also those deemed to have potential biological relation with the outcome, even though not significant in the univariate analysis, were used for further model adjustment. The association between road traffic noise (Lden), entered either as a continuous or as a categorical variable (5 dB(A) interval), and the odds of hypertension was investigated using bivariate (model 1) and multivariate (model 2 and model 3) logistic regression separately for each gender. Model 1 was unadjusted. Model 2 was adjusted for age, BMI, other chronic disease, and family history of cardiovascular disease for both genders. Model 3 was adjusted for self-reported mental stress/tension, bedroom window orientation, and smoking habits for males. Since smoking was not reported by any female respondents, the final model was adjusted for physical activity and residence period additionally. Stratified analysis for exposure (residential) period, categorized in three groups of <10, 10–20, and >20 years, was conducted after controlling for potential confounders. Results are presented as odds ratios (OR) with 95 % confidence intervals (95 % CI). Two-tailed statistical significance was evaluated by using a p of <0.05. Statistical analysis was conducted using the STATA package (32 bit) for Windows, version 11.2 (Stata Corp LP, College Station, TX, USA).
Results
Among the 909 who consented for the study, 59 % were female. The mean age of the sample population was 41.2 ± 14.7 years. Twenty-three percent of the respondents were exposed to residential noise level Lden > 60–65 dB(A), 25 % to 65–70 dB(A) and 19 % to above 70 dB(A). The risk factors like sociodemographics, lifestyle, disease status, and exposure variables, stratified by the presence or absence of hypertension and gender, are reported in Table 1.
TABLE 1.
Basic characteristics of the study subjects stratified by self-reported doctor-diagnosed hypertension and gender
| Characteristics | All subjects (n = 909) | Male (n = 376) | Female (n = 533) | ||||
|---|---|---|---|---|---|---|---|
| Stratum by hypertension | |||||||
| No (n = 291) | Yes (n = 85) | p a | No (n = 457) | Yes (n = 76) | p a | ||
| Lden (mean ± SD)b | 63.5 ± 6.6 | 63.0 ± 6.6 | 67.0 ± 6.3 | <0.001 | 62.6 ± 6.4 | 66.6 ± 6.4 | <0.001 |
| Agec (mean ± SD)b | 41.2 ± 14.7 | 40.6 ± 14.4 | 50 ± 14 | <0.001 | 38 ± 14 | 52.4 ± 10.7 | <0.001 |
| Education level (%)d | |||||||
| Primary | 10.5 | 7.2 | 17.7 | 0.009 | 10.1 | 18.4 | 0.098 |
| Secondary | 27.3 | 27.5 | 18.8 | 28.7 | 27.6 | ||
| Tertiary | 62.2 | 65.3 | 63.5 | 61.2 | 54.0 | ||
| Employed (%)d | 40.9 | 61.5 | 70.6 | 0.126 | 25.2 | 23.7 | 0.783 |
| Marital status (%)d | |||||||
| Married | 73.3 | 72.2 | 70.6 | 0.003 | 72.2 | 86.8 | <0.001 |
| Never married | 20.2 | 22.0 | 12.9 | 23.2 | 4.0 | ||
| Separated/widow | 6.5 | 5.8 | 16.5 | 4.6 | 9.2 | ||
| BMI (mean ± SD)b | 24.6 ± 3.8 | 24.5 ± 3.7 | 25.5 ± 3.8 | 0.083 | 24.3 ± 3.8 | 25.6 ± 4.2 | 0.010 |
| Physical activity (%)d | |||||||
| Sedentary | 66.3 | 60.1 | 61.2 | 0.965 | 68.5 | 82.9 | 0.020 |
| Moderate | 18.3 | 23.4 | 23.5 | 15.1 | 11.8 | ||
| Active | 15.4 | 16.5 | 15.3 | 16.4 | 5.3 | ||
| Smoking habits (%)d | |||||||
| Never | 73.6 | 35.4 | 38.8 | 0.600 | 100 | 100 | - |
| Ex-smoker | 3.6 | 8.3 | 10.6 | - | - | ||
| Current | 22.8 | 56.7 | 50.6 | - | - | ||
| Alcohol intake (%)d | |||||||
| Never | 75.0 | 38.5 | 43.5 | 0.674 | 100 | 100 | - |
| Sometimes | 12.0 | 29.2 | 28.2 | - | - | ||
| Frequently | 13.0 | 32.3 | 28.3 | - | - | ||
| Chronic diseasese (%)d | 29.7 | 28.2 | 48.2 | 0.001 | 22.5 | 57.9 | <0.001 |
| Family CVDf (%)d | 11.7 | 10.7 | 11.8 | 0.772 | 11.2 | 18.4 | 0.073 |
| Noise sensitivity (%)d | |||||||
| Low | 37.8 | 40.2 | 27.1 | 0.029 | 38.9 | 34.2 | 0.734 |
| Moderate | 38.5 | 35.4 | 50.6 | 37.9 | 40.8 | ||
| High | 23.7 | 24.4 | 22.3 | 23.2 | 25.0 | ||
| Self-reported mental stress (%)d | |||||||
| Low | 60.8 | 58.4 | 45.9 | <0.001 | 64.1 | 67.1 | 0.473 |
| Moderate | 26.4 | 30.2 | 23.5 | 25.6 | 19.7 | ||
| High | 12.8 | 11.4 | 30.6 | 10.3 | 13.2 | ||
| Residencec (mean ± SD)b | 21.6 ± 11 | 21.5 ± 11 | 21.8 ± 10 | 0.903 | 20.9 ± 10 | 26 ± 10 | <0.001 |
| Satisfied with neighborhood (%)d | |||||||
| No | 48.3 | 46.1 | 56.5 | 0.233 | 47.3 | 54.0 | 0.558 |
| Neutral | 30.6 | 30.9 | 25.9 | 31.7 | 27.6 | ||
| Yes | 21.1 | 23.0 | 17.6 | 21.0 | 18.4 | ||
| House ownership (%)d | 40.9 | 49.8 | 55.3 | 0.375 | 33.9 | 32.9 | 0.862 |
| Dwelling type (%)d | |||||||
| Apartment | 27.9 | 26.5 | 30.6 | 0.453 | 28.0 | 30.3 | 0.686 |
| Others | 72.1 | 73.5 | 69.4 | 72.0 | 69.7 | ||
| Bedroom window (%)d | |||||||
| Facing road | 59.3 | 58.1 | 76.5 | 0.002 | 57.1 | 57.9 | 0.898 |
| Facing others | 40.7 | 41.9 | 23.5 | 42.9 | 42.1 | ||
BMI body mass index in kg/m2, SD standard deviation
aDifference between stratum
bWilcoxon signed rank test of the difference between the stratum
cAge and residence in years. L den is the 24-h time-weighted noise level in dB(A)
dChi-square test of the difference between the stratum
eDiabetes, COPD, high total cholesterol, coronary heart disease, and renal ailments
fFamily history of cardiovascular disease before the age of 60 years
Hypertensive cases were confirmed in 17.7 % of the participants. Among males, the prevalence was 22.6 %, and among females, it was 14.3 % (χ2 = 10.54; p = 0.001). Hypertensive and non-hypertensive subjects differed significantly in age, marital status, and other presence of chronic diseases. Additionally, males differed significantly for education level, noise sensitivity, mental stress, and bedroom window orientation. Female subjects, in addition, differed significantly for physical activity and residence period. Results of logistic regression (univariate and multivariate) for the association of hypertension with relevant risk factors and other variables are presented in Table 2.
TABLE 2.
Association of risk factors and sociodemographic variables with hypertension in male and female subjects
| Factors | Male (n = 376) | Female (n = 533) | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate OR (95 % CI) | p | Adjusteda OR (95 % CI) | p | Univariate OR (95 % CI) | p | Adjusteda OR (95 % CI) | p | |
| Age | 1.04 (1.03–1.06) | <0.001 | 1.06 (1.03–1.08) | <0.001 | 1.07 (1.05–1.09) | <0.001 | 1.05 (1.03–1.08) | <0.001 |
| Marital status | 1.33 (0.93–1.91) | 0.124 | 1.36 (0.90–2.07) | 0.142 | 0.70 (0.43–1.14) | 0.136 | 0.67 (0.41–1.10) | 0.112 |
| BMI | 1.07 (1.01–1.14) | 0.044 | 1.11 (1.03–1.19) | 0.009 | 1.09 (1.03–1.17) | 0.006 | 1.05 (0.97–1.13) | 0.257 |
| Chronic diseases | 2.38 (1.45–3.90) | 0.001 | 1.58 (0.86–2.88) | 0.137 | 4.73 (2.85–7.83) | <0.001 | 2.96 (1.59–5.49) | 0.001 |
| Satisfaction | 0.77 (0.56–1.06) | 0.103 | 0.82 (0.57–1.17) | 0.273 | 0.86 (0.62–1.18) | 0.335 | 0.96 (0.67–1.37) | 0.817 |
| Education level | 0.77 (0.54–1.09) | 0.142 | 0.78 (0.52–1.18) | 0.248 | 0.73 (0.53–1.02) | 0.073 | 1.18 (0.79–1.77) | 0.408 |
| Physical activity | 0.96 (0.70–1.33) | 0.810 | 1.12 (0.77–1.63) | 0.562 | 0.55 (0.36–0.85) | 0.003 | 0.65 (0.40–1.06) | 0.083 |
| Noise sensitivity | 1.20 (0.88–1.65) | 0.244 | 1.00 (0.70–1.43) | 0.994 | 1.12 (0.82–1.53) | 0.495 | 1.14 (0.81–1.62) | 0.454 |
| Mental stress | 1.72 (1.26–2.35) | 0.001 | 2.24 (1.55–3.26) | <0.001 | 1.00 (0.70–1.43) | 0.989 | 1.23 (0.80–1.88) | 0.339 |
| Residence period | 1.01 (0.98–1.03) | 0.848 | 0.99 (0.96–1.01) | 0.295 | 1.05 (1.02–1.07) | <0.001 | 1.02 (1.00–1.05) | 0.156 |
| Bedroom window | 2.35 (1.35–4.08) | 0.002 | 2.70 (1.46–5.02) | 0.002 | 1.03 (0.63–1.69) | 0.898 | 1.28 (0.73–2.25) | 0.389 |
| Family CVD | 1.12 (0.52–2.39) | 0.774 | 1.27 (0.53–3.05) | 0.598 | 1.80 (0.94–3.44) | 0.089 | 1.64 (0.77–3.51) | 0.200 |
| Smoking habitsb | 0.90 (0.70–1.16) | 0.427 | 0.85 (0.64–1.15) | 0.297 | ||||
OR (95 % CI) odds ratio (95 % confidence interval), BMI body mass index (kg/m2)
aAdjusted by the other variables presented in the table
bSmoking not reported by any female participants
Gender disparity in the risk factors in relation to hypertension was noted. Higher OR resulted for the presence of other chronic disease, bedroom window orientation, and mental stress. The OR improved when the univariate model was adjusted with bedroom window orientation (by 15 %) and stress (by 30 %). A slight increase was also observed in the OR after adjustment for BMI. For females, a notably higher OR was observed, when other chronic diseases were used as predictor. The other factors like residence period and BMI were significantly associated in the univariate models only. Physical activity was also observed to be significantly associated with a decrease in the risk hypertension. Among the female participants dwelling in the noisy areas (Lden range <60–77.9 dB(A)), a significant association between noise exposure and hypertension was noted, in comparison to males (Table 3).
TABLE 3.
Association between the prevalence of hypertension and road traffic noise exposure stratified by gender
| L den, dB(A) (range 55.1–77.9) | Hypertensive (n) | Model 1 OR (95 % CI) | p a | Model 2 OR (95 % CI)b | p c | Model 3 OR (95 % CI)d | p c | |
|---|---|---|---|---|---|---|---|---|
| Female | <60e | 6.6 % (181) | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 |
| ≥60 | 18.2 % (352) | 3.13 (1.64–5.97) | 5.03 (2.43–10.4) | 4.81 (2.32–9.98) | ||||
| Male | <60e | 11.1 (117) | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 |
| ≥60 | 27.8 (259) | 3.08 (1.63–5.83) | 3.36 (1.72–6.55) | 4.05 (1.20–8.22) | ||||
OR (95 % CI) odds ratio (95 % confidence interval)
aUnivariate logistic regression
bAdjusted additionally for age, BMI, other chronic diseases, and family history of CVD
cMultivariate logistic regression
dAdjusted additionally for physical activity and residence period in females and self-reported mental stress, bedroom window orientation towards road, and smoking habits in males
eReferent level
Adjusting the univariate model with age, BMI, other chronic disease, and family history of cardiovascular disease (CVD), an obvious increase in OR (60.7 %) was observed. Additional adjusting (model 3) with physical activity and residence period did not provide any significant change (<10 %) in the OR. Among the two variables, the period of residence at the current location was observed to be the more important factor in the final model. For males, the univariate and adjusted model (model 2) did not differ much. However, the OR increased by about 20.5 % in the final model (model 3) when fully adjusted for the model 2 variables and further with stress, bedroom window orientation, and smoking habits. Among the three predictors, smoking (0.3 %) and stress (6 %) were noted to have a low influence on the model, while bedroom window orientation was a significant predictor. Overall, female respondents had a significantly higher (50 %) OR for hypertension in comparison to males when adjusted for age, BMI, other chronic diseases, and family history of cardiovascular disease. Gender variation in relation to hypertension and exposure to noise was lower in the fully adjusted model (19 %).
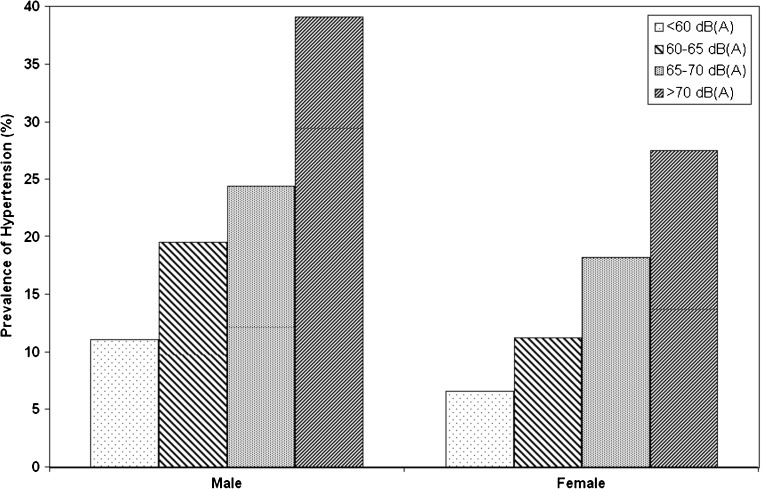
Multivariate logistic regression using noise as continuous variable resulted in OR of 1.99 (1.66–2.39) per 5-dB(A) increment in Lden. The outcome is suggestive of an association between exposure to road traffic noise and prevalence of hypertension in the adult subpopulation. A trend was observed showing an increase in the OR with higher noise exposure category (Table 4). A rise in the risk of hypertension among females exposed to higher noise level is observed, and although a trend is suggested, the confidence intervals are wide at higher noise levels. The prevalence of hypertension in relation to noise exposure level by gender is presented in Fig. 1.
TABLE 4.
Association between the prevalence of hypertension and road traffic noise exposure stratified by gender and exposure levels
| L den, dB(A) (range 55.1–77.9) | Prevalence of hypertension (n = 909) (%) | All | Male | Female |
|---|---|---|---|---|
| OR (95 % CI)a | OR (95 % CI)a | OR (95 % CI)a | ||
| L den-5 (continuous) | 17.7 | 1.99 (1.66–2.39) | 1.81 (1.42–2.31) | 2.18 (1.66–2.88) |
| <60b | 8.4 | 1.00 | ||
| 60–65 | 14.6 | 2.20 (1.21–4.03) | 1.93 (0.84–4.45) | 2.57 (1.06–6.23) |
| 65–70 | 20.7 | 3.90 (2.20–6.91) | 2.85 (1.29–6.29) | 5.48 (2.37–12.67) |
| ≥70 | 33.2 | 8.24 (4.63–14.6) | 6.25 (2.90–13.51) | 10.64 (4.40–25.7) |
OR (95 % CI) odds ratio (95 % confidence interval)
aAdjusted for age, BMI, other chronic disease, family history of CVD
bReferent level
FIG. 1.
Prevalence of hypertension in relation to noise exposure level by gender.
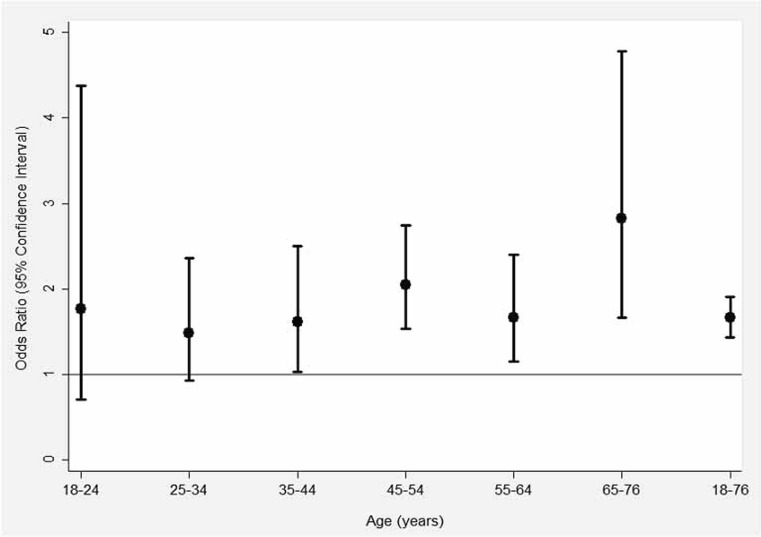
A significant OR of 1.66 (1.43–1.91) was observed for all participants (range 18–76 years), while gender-wise, females in higher age groups were more at risk (1.80 (1.45–2.23) than males (1.50 (1.24–1.82)). It was observed that a vulnerable subgroup with a significant association between hypertension and noise exposure was at 45–54 years. The graphical representation of the association between exposure to traffic noise and prevalence of hypertension in terms of age groups is given in Fig. 2. Stratification of the residence period (<10, 10–20, and <20 years) for model adjustment yielded no significant results. Individually, taking <10 years of residence as a latency period, an OR of 1.44 (0.80–2.62) and 1.52 (0.90–2.56) was observed for 10–20 and <20 years, respectively. However, results were not significant, but a higher risk of hypertension in relation to road traffic noise exposure was noted among female participants residing for 10–20 years while among males for >20 years.
FIG. 2.
Association between exposure to traffic noise and prevalence of hypertension in terms of age groups.
Discussion
In the present cross-sectional study, we found that exposure to residential road traffic noise was significantly associated with prevalence of hypertension in an adult urban subpopulation. Participants, with a minimum of 1-year residence at the current location at the time of this study and exposed to road traffic noise level (Lden) in the range of <60 to 80 dB(A), had a nearly double odds of risk for hypertension than those exposed to noise less than 60 dB(A). The risk was nearly 2.2 times for females and 1.8 times in males. A recent meta-analysis reported a positive and significant relationship between road traffic noise exposure and prevalence of hypertension.6 The pooled OR was 1.03 (95 % CI 1.01–1.06) per 5 dB(A) of increase of noise levels, although no threshold for an effect outcome could be established. Results from this study may further improve this evidence by obtaining a statistically significant association. A major difference for this study may be pointed to the fact that most of the previous studies have shown that male subjects are at higher risk, while this study suggests that females at are higher risk of arterial hypertension in relation to traffic noise exposure. Previous studies have suggested a greater risk of arterial hypertension for higher noise categories in excess of 60 dB(A), although statistical significance was rarely achieved and estimates were mostly heterogeneous.14–16 A previous study by Bluhm17 reported a linear exposure outcome association between traffic noise (per 5 dB(A)) and prevalence of hypertension with an adjusted OR of 1.38. A study by Bendokeina,18 examining the risk of hypertension related to residential road traffic noise exposure among reproductive-aged women, reported an effect estimate at noise levels of 51–60 dB(A) (OR = 1.03; 95 % CI 0.72–1.49) and at >61 dB(A) (OR 1.94, 95 % CI 1.01–3.72). The effect was more noticeable among women aged 30–45. Overall, this study shows that a significant association between road traffic noise exposure and the prevalence of hypertension among non-European populations may exist. A study by Chang8 reported a significantly higher prevalence of hypertension (adjusted OR = 2.15, 95 % CI = 1.08–4.26) in exposure above 82.2 dB(A) in central Taiwan. There was a significant increasing trend between noise levels and outcome prevalence. The significant result may be attributed to the fact that the 24-h time-weighted noise index, Lden, was used in this study, which may be of better prediction power than the period-fixed (16 or 8 h) equivalent noise indicators. A study by de Kluizenaar19 using Lden reported significant associations in the fully adjusted model (OR = 1.31) and subcohort (OR = 1.35) per 10 dB(A).
For detecting and defining a threshold noise exposure level above which hypertension can be observed with a statistical significance, Lden was used in increment of 5 dB(A) as the independent exposure variable. A noise level of 67.5 dB(A) for exposed males and 62.5 dB(A) for females is suggested from this study. A previous study20 reported a threshold of 83 dB(A) using the measured Leq-8h (9:00–17:00 hours), which lowered to 80 dB(A) after adjusting with the total traffic rate. Traffic flow characteristics were not used in our study, since noise index was directly modeled using traffic data inputs and thus would greatly collaborate with it. It should be mentioned that the issue of air pollutants related to movement may be an influencing factor in the noise-hypertension relation link.16
The association of exposure to road traffic noise and hypertension among susceptible subgroups is mostly limited to gender. Age-subgroup vulnerability and cause-effect link in relation to noise exposure are somewhat limited. Our study found a significant gender difference between residential road traffic noise exposure and prevalence of hypertension. We found the risk to be higher among female participants. Similar results were also reported, where the adjusted OR for hypertension was 1.71 (95 % CI = 1.17–2.50) per 5 dBA among women.18 Among other reasons, including the concept of more time at residence, which is more marked in this study population and difference in hormones, sensitivity and post-menstrual effects, a stressful marital life, and low employment, could be significant predictors for Indian women. Interestingly, in contrast to previous studies using smoking and drinking habit as confounders, for this study, none of the female participants reported to have these habits, which may influence the outcome. The threshold age for an increased risk of hypertension was lower for female subjects in comparison to males. The issue of more residential hours at home and noise sensitivity among females may be conservatively cited as a reason with caution.
Positives of the study included control of a large number of relevant covariates, group comparisons, stratified analysis, and adjusted of models to minimize confounding. Analysis was conducted separately for male and female subjects, as gender differences in arterial hypertension in relation to noise exposure have been reported previously. Further noise exposure was assessed objectively using modeling technique and incorporating GIS for more accurate residential noise levels. This study used a weighted 24 hourly average exposure index, Lden, as against the conventional Lday 6–22 hour outdoor noise, used for most studies. The Lden index provides a better average for the entire 24 hourly exposure with penalties of 5 and 10 for evening and night time. This study used extensive individual information, which yielded better control of established risk factors of arterial hypertension. A large set of potential confounders were included for this study. This study also studied the exposure period of traffic noise and suggests a significant trend between noise levels and prevalence of arterial hypertension outcome.
This study may also have some limitations that should be considered. Firstly, indoor noise measurements were not undertaken, although nearest façade noise was estimated using suitable model platform. Secondly, hearing ability was not taken into account, although the support for a link between hearing ability and cardiovascular disease is lacking. Thirdly, occupational noise exposure, shift work, and physical workload were not assessed. Exposure at the workplace may have some influence on the association between residential noise exposure and hypertension.21 Fourthly, the outcome disease for this present investigation was a self-report of doctor diagnosis, which may introduce some bias and cause disease misclassification due to incorrect knowledge or non-reporting. Bias could be attributed to non-reporting of the outcome in the presence of the disease or lack of knowledge about it due to occurrence of mild symptoms. However, over-reporting is possible, as subjects with mild stress symptoms may have reported an outcome. However, it has been reported that self-administered questionnaires may have good accuracy to confirm hypertension.1,20 Fifthly, family history of cardiovascular disease may be misreported, although explanation for the variable was provided to each subject during data collection. Finally, data regarding endogenous variables, possible habituation, and coping strategies were not controlled for. Endogenous risk factors like blood cholesterol, glucose levels, cortisol, etc., directly related to coronary heart disease, were left out from this study. Another important confounder or effect modifier of the noise-cardiovascular effect association is air pollutants. Combined assessment of noise and air pollutants in studies of road traffic noise and cardiovascular disease is a key issue.22 For the present study, air pollution was not assessed for possibly confounding. But recent studies were consistent in suggesting that both air pollution and noise are likely independent risk factors of cardiovascular disease.22 However, misclassification of exposure may be considered since the variations in noise level related to building floor heights were not considered. This study suggests that the Lden noise index be used for exposure assessment for cardiovascular disease endpoints. The association was a bit high for the female subjects. This could be attributed to hormonal characteristics, longer period of stay at their residence, or due to chance or different patterns in misclassification of exposure.13
Conclusions
The findings from the present study are consistent with the hypothesis of an association between exposure to higher levels of road traffic noise and risk of hypertension. In conclusion, this cross-sectional study among a small adult urban subpopulation of Asansol City, residing in close proximity to roads, suggests a significant association between exposure to higher levels of noise and prevalence of self-reported hypertension, in comparison to those residing further away from main roads. The association was marginally higher among the female participants. The generalizability of the study results may be dealt cautiously, keeping in mind the limitations mentioned, the exclusion of subjects under 18 years, and the sociodemographic, environmental, lifestyle, and geographical condition of the study area when comparing with previous studies.
Acknowledgments
The authors express sincere thanks to the Teacher-in-charge, B.B. College (BBC/RD/ENV/02), Asansol; Chairman, West Bengal Pollution Control Board; and Chairman, Asansol Mines Board of Health for support. The contributions of the household surveyors from VBU are highly acknowledged.
References
- 1.Burden of Disease from Environmental Noise—Quantification of Healthy Life Years Lost in Europe; WHO Regional Office for Europe: Copenhagen, Denmark, 2011.
- 2.Babisch W. The noise/stress concept, risk assessment and research needs. Noise Health. 2002;4:1–11. [PubMed] [Google Scholar]
- 3.Babisch W. Transportation noise and cardiovascular risk: updated review and synthesis of epidemiological studies indicate that the evidence has increased. Noise Health. 2006;8:1–29. doi: 10.4103/1463-1741.32464. [DOI] [PubMed] [Google Scholar]
- 4.Babisch W. Transportation noise and cardiovascular risk: Review and synthesis of epidemiological studies, dose-effect curve and risk estimation. WaBoLu-Hefte 01/06. Dessau, Berlin, Brandenburg: Umweltbundesamt; 2006. [Google Scholar]
- 5.Van Kempen EE, Babisch W. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens. 2012;30:1075–1186. doi: 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- 6.Davies H, Kamp IV. Noise and cardiovascular diseases: a review of the literature 2008–2011. Noise Health. 2012;14:287–291. doi: 10.4103/1463-1741.104895. [DOI] [PubMed] [Google Scholar]
- 7.Bodin T, Albin M, Ardö J, Stroh E, Stroh P, Björk J. Road traffic noise and hypertension: results from a cross-sectional public health survey in southern Sweden. Environ Health. 2009;8:1–10. doi: 10.1186/1476-069X-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang TY, Liu CS, Bao BY, Li SF, Chen TI, Lin YJ. Characterization of road traffic noise exposure and prevalence of hypertension in central Taiwan. Sci Total Environ. 2011;409:1053–1057. doi: 10.1016/j.scitotenv.2010.11.039. [DOI] [PubMed] [Google Scholar]
- 9.Global health risks: mortality and burden of disease attributable to selected major risks. WHO Press, WHO: Geneva, Switzerland 2009.
- 10.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 11.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–78. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 12.Banerjee D. Research on road traffic noise and human health in India: review of literature from 1991–current. Noise Health. 2012;14:113–118. doi: 10.4103/1463-1741.97255. [DOI] [PubMed] [Google Scholar]
- 13.The Calculation of Road Traffic Noise, Department of Transport Welsh Office. HMSO: London, London; 1988.
- 14.Dratva J, Phuleria HC, Foraster M, et al. Transportation noise and blood pressure in a population-based sample of adults. Environ Health Perspect. 2004;120:50–55. doi: 10.1289/ehp.1103448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jarup L, Babisch W, Houthuijs D, et al. HYENA study team. hypertension and exposure to noise near airports: the HYENA study. Environ Health Perspect. 2008;13:329–333. doi: 10.1289/ehp.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Belojevic G, Jakovljevic BD, Stojanov VJ, Slepcevic VZ, Paunovic KZ. Nighttime road-traffic noise and arterial hypertension in an urban population. Hypertens Res. 2008;31:775–781. doi: 10.1291/hypres.31.775. [DOI] [PubMed] [Google Scholar]
- 17.Bluhm LG, Berglind N, Nordling E, Rosenlund M. Road traffic noise and hypertension. Occup Environ Med. 2007;64:122–126. doi: 10.1136/oem.2005.025866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bendokiene I, Grazuleviciene R, Dedele A. Risk of hypertension related to road traffic noise among reproductive-age women. Noise Health. 2011;13:371–377. doi: 10.4103/1463-1741.90288. [DOI] [PubMed] [Google Scholar]
- 19.de Kluizenaar Y, Gansevoort RT, Miedema HM, de Jong PE. Hypertension and road traffic noise exposure. Occup Environ Med. 2007;49:484–492. doi: 10.1097/JOM.0b013e318058a9ff. [DOI] [PubMed] [Google Scholar]
- 20.Barregard L, Bonde E, Ohrstrom E. Risk of hypertension from exposure to road traffic noise in a population-based sample. Occup Environ Med. 2009;66:410–415. doi: 10.1136/oem.2008.042804. [DOI] [PubMed] [Google Scholar]
- 21.Van Kempen EE, Kruize H, Boshuizen HC, Ameling CB, Staatsen BA, de Hollander AE. The association between noise exposure and blood pressure and ischemic heart disease: a meta-analysis. Environ Health Perspect. 2002;110:307–317. doi: 10.1289/ehp.02110307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foraster M. Is it traffic-related air pollution or road traffic noise, or both? Key questions not yet settled! Int J Public Health. 2013;58:647–648. doi: 10.1007/s00038-013-0500-3. [DOI] [PubMed] [Google Scholar]