Abstract
An estimated 17.6 million American households were food insecure in 2012, meaning they were unable to obtain enough food for an active and healthy life. Programs to augment local access to healthy foods are increasingly widespread, with unclear effects on food security. At the same time, the US government has recently enacted major cuts to federal food assistance programs. In this study, we examined the association between food insecurity (skipping or reducing meal size because of budget), neighborhood food access (self-reported access to fruits and vegetables and quality of grocery stores), and receipt of food assistance using the 2008, 2010, and 2012 waves of the Southeastern Pennsylvania Household Health Survey. Of 11,599 respondents, 16.7 % reported food insecurity; 79.4 % of the food insecure found it easy or very easy to find fruits and vegetables, and 60.6 % reported excellent or good quality neighborhood grocery stores. In our regression models adjusting for individual- and neighborhood-level covariates, compared to those who reported very difficult access to fruits and vegetables, those who reported difficult, easy or very easy access were less likely to report food insecurity (OR 0.62: 95 % CI 0.43–0.90, 0.33: 95 % CI 0.23–0.47, and 0.28: 95 % CI 0.20–0.40). Compared to those who reported poor stores, those who reported fair, good, and excellent quality stores were also less likely to report food insecurity (OR 0.81: 95 % CI 0.60–1.08, 0.58: 95 % CI 0.43–0.78, and 0.43: 95 % CI 0.31–0.59). Compared to individuals not receiving food assistance, those receiving Supplemental Nutrition Assistance Program (SNAP) benefits were significantly more likely to be food insecure (OR 1.36: 95 % CI 1.11–1.67), while those receiving benefits from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) (OR 1.17: 95 % CI 0.77–1.78) and those receiving both SNAP and WIC (OR 0.84: 95 % CI 0.61–1.17) did not have significantly different odds of food insecurity. In conclusion, better neighborhood food access is associated with lower risk of food insecurity. However, most food insecure individuals reported good access. Improving diet in communities with high rates of food insecurity likely requires not only improved access but also greater affordability.
Keywords: Environment and public health, Nutrition policy, Hunger, Food assistance
Background
The United States Department of Agriculture (USDA) estimates that in 2012, 17.6 million households were food insecure, meaning they were unable to obtain enough food for an active and healthy life.1 Food insecurity has been linked to increased risk of poor physical and mental health, developmental problems in children, as well as depression and diet-related diseases such as obesity, hypertension, and diabetes in adults.2–8 Traditionally, food insecurity has been addressed through government-funded food assistance programs: the Supplemental Nutrition Assistance Program (SNAP, formerly known as food stamps) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Recently, considerable resources and research have been directed towards improving diet in low-income communities by increasing neighborhood access to fruits, vegetables, and other healthy foods.9 However, it is unknown if programs to increase food access also reduce food insecurity, as food insecure families may be unable to purchase even conveniently located food.
An understanding of the relationship between food access and food insecurity in the USA is urgently needed. With the expiration of increases from the American Recovery and Reinvestment Act of 2009, $5 billion in cuts to SNAP funding went into effect on November 1, 2013. Legislation containing further cuts to SNAP passed in the US Congress in February 2014. These cuts are occurring against the backdrop of increasing numbers of families receiving SNAP, a trend that began with the recession. While food assistance programs are experiencing funding cuts, programs aimed at increasing food access are becoming a major part of local, state, and national public health policy, as well as non-profit organization activity.9–11 Prior research has found that residence in neighborhoods with better food access (e.g., more full-service supermarkets) is associated with healthier diets and less risk of obesity.12–14 However, if local food remains out of reach due to economic constraints, there may be a ceiling beyond which improved food access cannot improve diet or health.
Philadelphia is a city with high rates of poverty and diet-related diseases. In 2011, 28.4 % of the Philadelphia population lived in poverty, well above the US rate of 15.9 %.15 In 2012, 32 % of Philadelphia adults were obese, and 11 % had diabetes.16 Philadelphia is also a center of government and non-profit efforts to improve local food access. The Pennsylvania Fresh Food Financing Initiative, which incentivizes the opening of supermarkets in neighborhoods previously without this resource, began at The Food Trust in Philadelphia and is the model for the national Healthy Food Financing Initiative.17 Other programs include interventions to improve the selection of healthy foods in corner stores and to increase the number of farmers markets.18,19
Amidst a lingering recession, additional cuts to food assistance program, putting even more residents at risk for food insecurity. Therefore, the determinants of food insecurity are particularly relevant for Philadelphia and similar cities with a large proportion of residents living in poverty. The current study examines the relationship between food insecurity, neighborhood food access, and food assistance programs in Philadelphia.
Methods
We analyzed the 2008, 2010, and 2012 waves of the Southeastern Pennsylvania (SEPA) Household Health Survey, a cross-sectional survey administered by the Public Health Management Corporation (PMHC).16 We examined the prevalence of food insecurity, rates of neighborhood food access, rates of food assistance receipt, and the relationship between food insecurity, neighborhood food access, and food assistance receipt. Data were de-identified by the PHMC prior to release; for this reason, the University of Pennsylvania institutional review board provided the study with exempt status. All analyses were conducted in 2013.
Study Sample
The SEPA Household Health Survey is administered every 2 years to a random sample of households in five counties of Southeastern Pennsylvania (Bucks, Montgomery, Chester, Delaware, and Philadelphia). Households are selected using random digit dialing (computerized in the case of landlines and manual in the case of cellular phones), and the survey is conducted by phone. The sample is semi-stratified by “service areas,” groupings of ZIP Codes established by the PHMC to assure adequate representation in all geographic areas in the region. In each of the 3 years examined, approximately 10,000 households participated in the survey. The response rate was 24.8 % in 2008, 24.5 % in 2010, and 22.0 % in 2012. We included respondents from 2008, 2010, and 2012 in Philadelphia County, which has the same borders as the city of Philadelphia and approximately 580,509 households.15
Main Outcome Measure
The primary outcome of interest was food insecurity, defined by whether the respondent had skipped or reduced meal size because of budgetary constraints in the previous 12 months. Between 2000 and 2010, the survey contained a single yes/no question that assessed food security: “In the past 12 months, since (date one year ago) did you or other adults in your household ever cut the size of your meals or skip meals because there was not enough money in the budget for food?” The question was altered to a small degree in 2012 to “In the past 12 months, since (date one 1 ago) did you ever cut the size of your meals or skip meals because there was not enough money in the budget for food?” Both versions of the question are almost identical to a question from the USDA Household Food Security Survey, a previously validated and extensively studied 18-item survey that is the most commonly used measure of food insecurity.20
Independent Variables
The main independent variables were measures of perceived neighborhood food access and food assistance receipt. Since 2008, the survey has assessed food access using the following two questions: (1) “How easy or difficult is it for you to find fruits and vegetables in your neighborhood? Would you say that it is very easy, easy, difficult or very difficult?” and (2) “How would you rate the overall quality of groceries available in the stores in your neighborhood? Would you say it is excellent, good, fair, or poor?” We combined responses to questions about SNAP and WIC into a single variable that categorized households as receiving either (1) no food assistance, (2) SNAP only, (3) WIC only, or (4) SNAP and WIC.
Other independent variables included sociodemographics, survey year, and geographic area within the city. Demographics included age (divided into five groups, 18–39, 40–49, 50–59, 60–74, ≥75 years old), gender (male or female), and race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic/Latino of any race, Asian, biracial/multiracial, Native American, and other). To examine socioeconomic status, we used a variable that categorized households according to the federal poverty level (those with income >200 % of the federal poverty level, 150–200 % of the federal poverty level, 100–150 % of the federal poverty level, and <100 % of the federal poverty level). The PHMC calculates this variable based on income and household size. If a respondent’s income was missing (20.7 % in 2008, 23.5 % in 2010, 18.1 % in 2012), the variable was imputed by the PHMC using employment status of the main wage earner, Medicaid status, and educational level. To define geographic area, we used the PHMC-defined neighborhood areas. In Philadelphia, there are 45 neighborhoods which are aggregates of contiguous census tracts. Geographic area poverty level was also determined by calculating the percent of the population below 100 and 200 % of the federal poverty level in each PHMC-defined neighborhood using pooled 2007–2011 American Community Survey data.21 Variables of interest were complete for 93 % of respondents (11,599/12,476 unweighted respondents). Respondents with incomplete information were excluded from the analysis.
Statistical Analyses
We used chi-square tests to compare food insecurity rates between groups, and food access among those with and without food insecurity. We then developed a logistic regression model to examine the association between food insecurity and the key determinants of interest. The dependent variable was whether or not the respondent was food insecure. We included as independent variables food access, receipt of food assistance, age, gender, race/ethnicity, socioeconomic status, and survey year. For the food access variables, we used those with poor access as the referent groups (those who found it very difficult to find fruits and vegetables in the neighborhood and reported poor quality groceries, respectively). To adjust for time-invariant characteristics of different geographic areas, a geographic area fixed effect was included. Given the large number of neighborhoods included in the model, results of geographic fixed effect terms are not shown, but are available from the corresponding author. As a sensitivity analysis, we repeated the analyses adjusting for geographic area poverty level instead of the geographic area fixed effect. In addition, we performed separate regressions for 2008 along with 2010, and 2012 only, given the change in the question regarding food insecurity between the 2010 and 2012 waves. We compared the results of these two regressions to each other and to the full model including all years.
All analyses incorporated survey strata and balancing weights, to adjust for over- and under-representation within the survey sample. A P value ≤0.05 was considered statistically significant. All analyses were performed using Stata, Version 12 (Copyright 1985–2011, StataCorp LP).
Results
Across the three survey waves, there were 11,599 respondents from Philadelphia included in the current study (Table 1). Overall, 16.7 % of respondents reported food insecurity: 16.8 % of the population in 2008, 15.0 % in 2010, and 18.6 % in 2012.
TABLE 1.
Sociodemographic characteristics, food assistance status, and food insecurity status of Philadelphia survey respondents (n = 11,599)
| Characteristic | Survey respondents, % | Reporting food insecurity, % |
|---|---|---|
| Age group, years old | ||
| 18–39 | 38.2 | 18.6 |
| 40–49 | 16.0 | 21.9 |
| 50–59 | 21.7 | 19.3 |
| 60–74 | 15.8 | 9.9 |
| ≥75 | 8.3 | 4.3 |
| Gender | ||
| Female | 55.7 | 18.0 |
| Male | 44.3 | 15.2 |
| Race/ethnicity | ||
| White | 41.5 | 12.3 |
| Black | 40.3 | 18.4 |
| Hispanic/Latino | 12.3 | 26.7 |
| Asian | 3.2 | 7.8 |
| Biracial/multiracial | 1.8 | 25.0 |
| Native American | 0.5 | 24.2 |
| Other | 0.4 | 25.1 |
| Food assistance | ||
| None | 74.9 | 12.6 |
| SNAP only | 17.7 | 31.0 |
| WIC only | 2.8 | 23.7 |
| SNAP + WIC | 4.6 | 24.2 |
| Income, percentage of FPL | ||
| >200 % | 57.9 | 9.0 |
| 150–200 % | 9.8 | 21.3 |
| 100–150 % | 10.8 | 22.4 |
| <100 % | 21.4 | 32.6 |
FPL federal poverty line
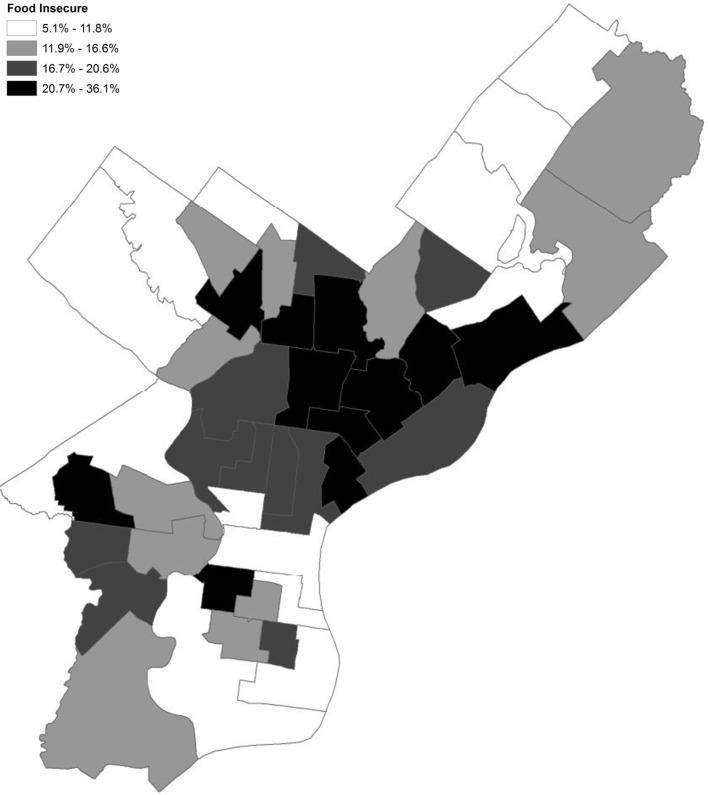
In bivariate analyses, the prevalence of food insecurity differed between age (p < 0.001), gender (p = 0.004), racial/ethnic (p < 0.001), food assistance (p < 0.001), and income (p < 0.001) groups (Table 1), and geographic area (Fig. 1). The prevalence of food insecurity in Philadelphia geographic areas ranged from 5.1 to 36.1 % (Fig. 1). Of those who reported food insecurity, 56.3 % were not receiving any type of food assistance.
FIG. 1.
Unadjusted prevalence of food insecurity by neighborhood of Philadelphia.
Of those who reported food insecurity, 79.4 % found it easy or very easy to find fruits and vegetables in their neighborhood and 60.6 % reported excellent or good quality groceries in their neighborhood (Table 2). Among the food secure, 93.2 % found it easy or very easy to find fruits and vegetables and 79.9 % reported excellent or good quality groceries in their neighborhood.
TABLE 2.
Neighborhood food access among food insecure and food secure survey respondents
| Survey respondents, % | Food insecure respondents, % | Food secure respondents, % | P valuea | |
|---|---|---|---|---|
| How easy or difficult is it for you to find fruits and vegetables in your neighborhood? | ||||
| Very easy | 55.4 | 40.3 | 58.4 | <0.001 |
| Easy | 35.5 | 39.1 | 34.8 | |
| Difficult | 6.5 | 12.9 | 5.2 | |
| Very difficult | 2.6 | 7.8 | 1.6 | |
| How would you rate the overall quality of groceries available in the stores in your neighborhood? | ||||
| Excellent | 33.2 | 20.7 | 35.7 | <0.001 |
| Good | 43.5 | 40.0 | 44.2 | |
| Fair | 17.7 | 27.2 | 15.8 | |
| Poor | 5.1 | 11.4 | 3.8 | |
| No store | 0.5 | 0.8 | 0.5 | |
aComparing neighborhood food access between food insecure and food secure respondents
In the fully adjusted model (Table 3), compared to those who reported very difficult access to fruits and vegetables, those who reported difficult, easy, or very easy access were less likely to report food insecurity (OR 0.62: 95 % CI 0.43–0.90, 0.33: 95 % CI 0.23–0.47, and 0.28: 95 % CI 0.20–0.40). Compared to those who reported poor quality groceries in their neighborhood, those who reported fair, good, or excellent quality groceries were less likely to report food insecurity (OR 0.81: 95 % CI 0.60–1.08, 0.58: 95 % CI 0.43–0.78, and 0.43: 95 % CI 0.31–0.59). For both of these variables, the odds of food insecurity decreased in a monotonic fashion as food access improved.
TABLE 3.
Odds of food insecurity among Philadelphia survey respondents (n = 11,599)
| Characteristic | OR (95 % CI) | P value |
|---|---|---|
| Neighborhood food access | ||
| Fruit and vegetable availability | ||
| Very difficult | Ref. | |
| Difficult | 0.62 (0.43–0.90) | 0.01 |
| Easy | 0.33 (0.23–0.47) | <0.001 |
| Very easy | 0.28 (0.20–0.40) | <0.001 |
| Quality of groceries in neighborhood stores | ||
| Poor | Ref. | |
| Fair | 0.81 (0.60–1.08) | 0.15 |
| Good | 0.58 (0.43–0.78) | <0.001 |
| Excellent | 0.43 (0.31–0.59) | <0.001 |
| No store | 0.93 (0.42–2.05) | 0.85 |
| Food Assistance | ||
| None | Ref. | |
| SNAP only | 1.36 (1.11–1.67) | 0.003 |
| WIC only | 1.17 (0.77–1.78) | 0.47 |
| SNAP + WIC | 0.84 (0.61–1.17) | 0.31 |
| Other characteristics | ||
| Age group, years old | ||
| 18–39 | Ref. | |
| 40–49 | 1.23 (1.01–1.49) | 0.04 |
| 50–59 | 1.13 (0.94–1.37) | 0.20 |
| 60–74 | 0.49 (0.40–0.62) | <0.001 |
| ≥75 | 0.20 (0.14–0.28) | <0.001 |
| Gender | ||
| Male | Ref. | |
| Female | 1.05 (0.901–1.22) | 0.52 |
| Race/ethnicity | ||
| White | Ref. | |
| Black | 0.94 (0.75–1.17) | 0.58 |
| Hispanic/Latino | 1.12 (0.85–1.48) | 0.14 |
| Asian | 0.39 (0.21–0.72) | 0.003 |
| Biracial/multiracial | 1.54 (0.95–2.51) | 0.08 |
| Native American | 1.58 (0.71–3.54) | 0.27 |
| Other | 1.78 (0.57–5.60) | 0.33 |
| Income, percentage of FPL | ||
| >200 % | Ref. | |
| 150–200 % | 2.56 (2.02–3.23) | <0.001 |
| 100–150 % | 2.70 (2.16–3.38) | <0.001 |
| <100 % | 3.76 (3.03–4.66) | <0.001 |
| Survey year | ||
| 2008 | Ref. | |
| 2010 | 0.87 (0.74–1.02) | 0.08 |
| 2012 | 1.13 (0.95–1.35) | 0.17 |
Ref Referent group, FPL federal poverty line
Compared to individuals not receiving food assistance, those receiving SNAP were significantly more likely to be food insecure (OR 1.36: 95 % CI 1.11–1.67). However, those receiving WIC (OR 1.17: 95 % CI 0.77–1.78) and those receiving both SNAP and WIC (OR 0.84: 95 % CI 0.61–1.17) did not have significantly different odds of food insecurity than those who were not receiving food assistance. Compared to respondents aged 18–39 years old, older individuals, aged 60–74 years old and 75 years or older, had a significantly lower risk of food insecurity (OR 0.49: 95 % CI 0.40–0.62 and OR 0.20: 95 % CI 0.14–0.28, respectively).
Results from the sensitivity analysis, adjusting for geographic area poverty level instead of a geographic area fixed effect, yielded similar results. Results from additional analyses that looked at 2008 and 2010 together, and 2012 on its own, were also similar.
Discussion
Over one in six survey respondents in Philadelphia (16.7 %) were food insecure. This is likely to be an underestimate, given that the single question used on the survey asks about a relatively severe component of food insecurity and is less sensitive than the multi-component measure used to obtain national estimates. Increases in neighborhood food access were found to be associated with a lower risk of food insecurity. However, a majority of food insecure residents reported easy or very easy access to fruits and vegetables and excellent or good quality grocery stores. Many food insecure individuals were not receiving food assistance, and many individuals receiving food assistance remained food insecure. These findings raise questions about the ability of food access programs that focus only on location to fully address the needs of those living in poverty.
Previous research on diet and health has largely looked at the relationships between neighborhood food access and diet, neighborhood food access and diet-related diseases, and food insecurity and diet-related diseases.2,3,5,7,12,13,22 Studies examining the relationship between neighborhood characteristics, such as food access, and food insecurity are few. A study employing survey and mapping data in a low-income population of residents of Toronto, Canada, found that proximity to a local food outlet did not reduce the risk of household food insecurity and there was no association between a respondent’s perception of adequate food access and the respondent’s food security status.23 Our study’s contrasting findings may be attributable to differences between Philadelphia and Toronto, and between Canadian and US food prices and social policies affecting low-income families. One potential explanation for the relationship between access and food insecurity we found is that lack of neighborhood food access increases the costs of food shopping requiring funds and time for transportation, thereby increasing the risk of food insecurity. If this scenario is accurate, then programs to increase local food access could improve food security status by decreasing the costs of obtaining food. However, in the current study, we also found that the majority of food insecure respondents reported easy or very easy access to fruits and vegetables and excellent or good quality grocery stores in their neighborhood. This means that even though they had good access to quality grocery stores, fruits, and vegetables, they were still reducing the size of their meals and skipping meals due to financial constraints. Increasing proximity to healthy foods may not change the diets of people in this group, because they are unable to afford foods that are accessible already.
Consistent with other work, those receiving SNAP were at higher risk of food insecurity than those not receiving food assistance.1,24 This is explained by the fact that those who are more likely to participate are also more likely to have certain health and financial characteristics that predispose them towards food insecurity. Of note, of the respondents who reported food insecurity, 56.3 % stated they were not receiving any food assistance, a strikingly high proportion. Several factors can explain this finding. Many individuals suffering from food insecurity may not qualify for SNAP or WIC. Alternatively, individuals who are eligible may be unaware that they are eligible, have difficulty with the application process, or opt not to participate. In the USA, SNAP participation rates among eligible individuals were estimated at 66 % in 2009, 74 % in 2010, and 79 % in 2011.25 In addition, prior research suggests that individuals do not reliably disclose whether they participate in SNAP on surveys, meaning our analysis likely underestimates true rates of food assistance coverage.26,27
Those receiving WIC, or both SNAP and WIC, had similar odds of food insecurity to those receiving no food assistance. There are several possible interpretations of this finding. One is that WIC, either alone or in combination with SNAP, protects against food insecurity. Another possible interpretation is that those who are likely to receive WIC have similar rates of food insecurity to those who are likely to receive no food assistance (which is lower than those receiving SNAP). The qualifying income for SNAP is lower than that for WIC, thus it is plausible that those receiving SNAP benefits only would have higher rates of food insecurity.
This study has several limitations. This is an observational study employing cross-sectional survey data, and there may be unmeasured variables confounding the association between neighborhood food access, food assistance receipt, and food insecurity. This study focuses on a specific city, Philadelphia, and thus it is unclear if results can be generalized to other cities. This survey employed a single question asking about food insecurity that had a minor wording change over time, and thus results are not directly comparable with other studies of food insecurity, which have employed multiple questions. There are currently multiple instruments used to measure neighborhood food access, with a lack of consistency across literature evaluating the effects of such environmental factors on health.28 The proportion of respondents reporting perceived inadequate food access in this sample was lower than estimates based on objective evaluations of Philadelphia food outlets.19 This discrepancy is consistent with other evaluations indicating that self-reported measures may underestimate true lack of access to healthy foods.29
While those living in higher access areas were at lower risk of food insecurity, even after controlling for neighborhood-level factors, most of those who were food insecure reported easy or very easy access to fruits and vegetables and excellent or good quality grocery stores in their neighborhood. Therefore, in the absence of policies and programs that allow families living in poverty to afford healthy foods, interventions that increase food access may not improve diet and decrease risk of diet-related diseases. Programs aimed at improving diet in low-income communities with high rates of food insecurity should focus not only on location but also on affordability, especially as cuts to food assistance programs threaten to increase food insecurity and poverty.30 Examples of such interventions include WIC farmer’s market coupons, which are issued on top of regular monthly benefits. In order to improve health in low-income communities disproportionately affected by diet-related diseases, it is essential to combine efforts to make sure that healthy food is accessible and that families can afford enough to eat.
Acknowledgments
The authors would like to thank Christopher Wirtalla for assistance with developing Stata programming. V.L.M. was supported with funding from the Division of General Internal Medicine Matt Slap Award from the Perelman School of Medicine at the University of Pennsylvania and the National Institutes of Health Institutional Training Grant 5-T32-HP-100296-20-00.
References
- 1.Coleman-Jensen A, Nord M, Singh A. Household food security in the United States in 2012. http://www.ers.usda.gov/publications/err-economic-research-report/err155.aspx#.UqUp4ZNeuw0. United States Department of Agriculture, Economic Research Service. Published September 2013. Accessed September 12, 2013.
- 2.Lee JS, Frongillo EA., Jr Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. J Nutr. 2001;131(5):1503–9. doi: 10.1093/jn/131.5.1503. [DOI] [PubMed] [Google Scholar]
- 3.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–10. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haering SA, Syed SB. Community food security in the United States: a survey of the relevant scientific literature. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health, Center for a Livable Future; 2009.
- 5.Bawadi HA, Ammari F, Abu-Jamous D, Khader YS, Bataineh S, Tayyem RF. Food insecurity is related to glycemic control deterioration in patients with type 2 diabetes. Clin Nutr. 2012;31(2):250–4. doi: 10.1016/j.clnu.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 6.Gucciardi E, Vogt JA, DeMelo M, Stewart DE. Exploration of the relationship between household food insecurity and diabetes in Canada. Diabetes Care. 2009;32(12):2218–24. doi: 10.2337/dc09-0823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107(11):1952–61. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Seligman HK, Jacobs EA, Lopez A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233–8. doi: 10.2337/dc11-1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brownson RC, Haire-Joshu D, Luke DA. Shaping the context of health: a review of environmental and policy approaches in the prevention of chronic diseases. Annu Rev Public Health. 2006;27:341–70. doi: 10.1146/annurev.publhealth.27.021405.102137. [DOI] [PubMed] [Google Scholar]
- 10.IOM (Institute of Medicine) Accelerating Progress in Obesity Prevention . Solving the weight of the nation. Washington, DC: The National Academies Press; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q. 2009;87(1):123–54. doi: 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Auchincloss AH, Mujahid MS, Shen M, Michos ED, Whitt-Glover MC, Diez Roux AV. Neighborhood health-promoting resources and obesity risk (the multi-ethnic study of atherosclerosis) Obesity (Silver Spring) 2013;21(3):621–8. doi: 10.1002/oby.20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 14.Ploeg MV, Breneman V, Farrigan T, et al. Access to affordable and nutritious food - measuring and understanding food deserts and their consequences: report to Congress.http://www.ers.usda.gov/publications/ap-administrative-publication/ap-036.aspx. United States Department of Agriculture, Economic Research Service. Published June 2009. Accessed September 12, 2013.
- 15.The Pew Charitable Trusts. Philadelphia Research Initiative. Philadelphia 2013: the state of the city. http://www.pewtrusts.org/our_work_report_detail_wide.aspx?id=85899461859. Published March 2013. Accessed September 16, 2013.
- 16.Public Health Management Corporation. Community Health Database. http://www.chdbdata.org/. Accessed October 1, 2012.
- 17.Karpyn A, Manon M, Treuhaft S, Giang T, Harries C, McCoubrey K. Policy solutions to the ‘grocery gap’. Health Aff (Millwood) 2010;29(3):473–80. doi: 10.1377/hlthaff.2009.0740. [DOI] [PubMed] [Google Scholar]
- 18.The Food Trust and Get Healthy Philly. Philadelphia’s healthy corner store initiative, 2010-2012. Published 2012. http://thefoodtrust.org/uploads/media_items/hcsi-y2report-final.original.pdf. Accessed November 19, 2013.
- 19.The Philadelphia Department of Public Health, Get Healthy Philly. Walkable access to healthy food in Philadelphia, 2010-2012. Published March 2013. http://www.phila.gov/health/pdfs/Food_access_report.pdf. Accessed September 18, 2013.
- 20.Bickel, G, Nord, M, Price, C, Hamilton, W, Cook, J. Measuring food security in the United States. Guide to measuring household food security. Revised 2000. http://www.fns.usda.gov/fsec/files/fsguide.pdf. Published March 2000. Accessed October 26, 2012.
- 21.U.S. Census Bureau. American Community Survey, 2007-2011. http://factfinder.census.gov/home. Accessed November 23, 2013.
- 22.Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: a review of food deserts literature. Health Place. 2010;16(5):876–84. doi: 10.1016/j.healthplace.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 23.Kirkpatrick SI, Tarasuk V. Assessing the relevance of neighbourhood characteristics to the household food security of low-income Toronto families. Public Health Nutr. 2010;13(7):1139–48. doi: 10.1017/S1368980010000339. [DOI] [PubMed] [Google Scholar]
- 24.Coleman-Jensen A, Nord M, Andrews M, and Carlson S. Household food security in the United States in 2011. http://www.ers.usda.gov/publications/err-economic-research-report/err141.aspx#.UqU2YJNeuw0. Published September 2012. Accessed October 3, 2012.
- 25.Cunnyngham K, Sukasih A, Castner L. Mathematica Policy Research. Empirical Bayes shrinkage estimates of state Supplemental Nutrition Assistance Program participation rates in 2009-2011 for all eligible people and the working poor. http://www.fns.usda.gov/empirical-bayes-shrinkage-estimates-state-supplemental-nutrition-assistance-program-participation-3. Published March 2014. Accessed April 12, 2014.
- 26.Kreider B, Pepper JV, Gunderson C, Jolliffe D. Identifying the effects of SNAP (food stamps) on child health outcomes when participation is endogenous and misreported. J Am Stat Assoc. 2012;107(499):958–75. doi: 10.1080/01621459.2012.682828. [DOI] [Google Scholar]
- 27.Meyer BD, Mok WKC, Sullivan JX. Under-reporting of transfer in household surveys: its nature and consequences. Working paper 15181. http://www.nber.org/papers/w15181. National Bureau of Economic Research. Published July 2009. Accessed October 29, 2012
- 28.Saelens BE, Glanz K. Work group I: measures of the food and physical activity environment: instruments. Am J Prev Med. 2009;36(4 Suppl):S166–70. doi: 10.1016/j.amepre.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 29.Moore LV, Diez Roux AV, Franco M. Measuring availability of healthy foods: agreement between directly measured and self-reported data. Am J Epidemiol. 2012;175(10):1037–44. doi: 10.1093/aje/kwr445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Health Impact Project. The Robert Wood Johnson Foundation and The Pew Charitable Trusts. White paper: health impact assessment of proposed changes to the supplemental nutrition assistance program. Published July 2013. http://www.rwf.org/en/reserach-publication/find-rwf-research/2013/7/health-impact-assesment-of-proposed-changes-to-the-supplement.html. Accessed September 11, 2013.