ABSTRACT
Background
Interpersonal care (IPC) is increasingly emphasized as health care systems focus on implementing patient-centered care. Language barriers may be a particularly important influence on IPC ratings among rural Spanish-speaking Latinos.
Objective
To examine the associations between provider Spanish fluency and Spanish-speaking patients’ ratings of IPC and between patient-provider language concordance and patient engagement in diabetes self-care activities.
Design
Cross-sectional survey combined with chart reviews.
Setting/Participants
Two hundred fifty Latino adults with diabetes receiving care at safety-net community health centers in two rural California counties.
Main Measures
Using a validated questionnaire, we assessed patient ratings of IPC in three areas: communication, decision-making, and interpersonal style. Patient-provider language concordance was measured by physician self-reported fluency in Spanish. We measured participation in diabetes self-care activities by patient self-report. The survey response rate was 68 %.
Key Results
Patients with language-concordant providers had more favorable IPC ratings (20 % to 41 % of language-discordant patients had optimal scores for IPC scales vs. 35 % to 69 % of language-concordant patients, p < 0.05), except with respect to discrimination. Patients with language-concordant providers reported higher levels of participation in diabetic foot care (1.4 days vs. 0.7 days per week, p value 0.01) compared to patients with language discordance. There was no association between language concordance and participation in other self-care activities.
Conclusion
This study provides evidence that language concordance is independently associated with high IPC scores in rural Latino adults with diabetes. Moreover, this study suggests that language concordance may contribute to improved participation diabetes self-care activities.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-3006-7) contains supplementary material, which is available to authorized users.
KEY WORDS: diabetes, communication, language barriers
INTRODUCTION
A positive provider-patient relationship facilitates higher quality medical care with improved patient satisfaction and health outcomes.1,2 Interpersonal processes of care (IPC) play a crucial role in this relationship and are defined by three elements: communication, interpersonal style, and patient-centered decision making.3–5 IPC is particularly important in chronic disease management, which requires complex monitoring, multiple medications, and behavior change. In particular, effective participation in diabetes self-care requires clear communication and a positive interpersonal relationship between patients and their providers.
Patient characteristics such as race and language influence IPC6,7 and need to be considered to provide high-quality medical care. Approximately 9 % of individuals in the US have limited English proficiency (LEP), defined as speaking English less than “very well” by self-report.8,9 Patient satisfaction and clinical outcomes are worse for this growing segment of the population than for English-speaking individuals.10,11 Patient-provider language concordance can help ameliorate these disparities.12–14 One study found an association among language concordance, cultural competence, and improved ratings of IPC among urban Spanish-speaking patients in hospital-based clinics.7 Further exploring the relationship among language concordance, IPC, and health behaviors is important for improving care for LEP patients.
Spanish speakers represent the largest group of LEP patients in the US and thus are an important population to study the effects of language concordance on IPC and health behaviors.8 Diabetes is a chronic disease that may be particular sensitive to IPC and disproportionately affects Latinos. Latinos in the US not only have a higher prevalence of diabetes but also have worse glycemic control.15–17 Moreover, language barriers are an important predictor of low rates of participation in recommended diabetes self-care activities.18 While limited research indicates that language concordance is associated with higher IPC scores and improved diabetes control,19 studies have not fully explored these associations in different patient populations. Latino populations are heterogeneous with respect to factors such as socioeconomic status, health insurance status, and country of origin.20,21 The results of studies about language concordance have not been validated in LEP Latinos receiving care in rural communities, a growing segment of the Latino population in the US that may benefit in unique ways from having language-concordant providers.22–24
The purpose of this study is to determine the association among patient-provider language concordance, patient ratings of IPC and participation in diabetes self-care activities for Latinos with diabetes receiving care in rural community health centers.
METHODS
Study Population
We examined cross-sectional survey data collected from Latino adults with diabetes receiving care at a large federally qualified health center (FQHC) with 20 primary care clinics across two counties in rural California. We focused on this agricultural community because of the high prevalence of diabetes and high number of Spanish-speaking LEP patients receiving care at the FQHC. The rates of diabetes in the two study counties are 9.4 % and 9.8 %, respectively, compared to an overall rate of 6.8 % in California.25,26 Sixty percent of patients served by the FQHC clinics are LEP, and Spanish is the most common language represented.
Patients were included in this study if they were 21 years or older, spoke Spanish, were able to identify a personal physician by name, were able to verbally consent to participate in the study, were diagnosed with type 2 diabetes mellitus (based on ICD9 code), and had two or more primary care visits in the past 12 months. Individuals were excluded if they were pregnant or had type 1 diabetes. Eligible patients were randomly sampled from an electronic diabetes registry that included over 90 % of diabetic patients in this health system. We used a cluster sampling design and sampled a maximum of ten patients from each physician. We chose this approach to ensure sampling from a variety of physicians and to optimize the diversity of our study participants.
Data Collection
The survey was administered by telephone to 250 patients between July 2009 and January 2010. Individuals were called up to 15 times to initiate contact and were offered a $20 gift card for their participation. The response rate was 68 %. The survey was administered by bilingual, native Spanish-speaking research staff from the FQHC and assessed demographic information, diabetes care, and IPC ratings. Participants were also asked about comorbid conditions, depressive symptoms, overall health status, and satisfaction with their physician. Survey responses were linked to clinical data from medical charts and the FQHC diabetes registry.
We surveyed 31 primary care physicians practicing in the FQHCs and assessed gender, age, race, specialty, board certification, years in practice, and Spanish language fluency.
Measurements
The primary predictor variable was patient-provider language concordance. Spanish-speaking patients were asked to identify their primary care physician. The physicians were then asked to rate their Spanish fluency on a 5-point scale ranging from excellent to none, using the question, “How would you rate your level of fluency in Spanish?” Categories were collapsed into fluent (defined as “excellent” or “good” self-reported fluency) and non-fluent (defined as “fair,” “poor” or “none”) because of the distribution of our responses and findings from a previous study.7 Language concordance was defined as Spanish-speaking patients whose physicians were fluent in Spanish, and language discordance was defined as Spanish-speaking patients with non-fluent physicians.7
The primary outcome variable was patient rating of IPC, measured using 14 items adapted from the IPC 18-item short form.3 The IPC survey was developed to capture elements of the provider-patient relationship in diverse populations and highlights factors important for minorities, LEP individuals, and individuals of lower socioeconomic status. The survey is composed of several multi-item composite scores and assesses communication, decision-making, and interpersonal style. It has been validated in both English and Spanish in diverse patient groups.3 This study focused on perceptions of the provider; therefore, we excluded four questions from the ICP short form pertaining to office staff.
The communication domain included three multi-item scales (lack of clarity, eliCitation of concerns, and explaining results), the decision-making domain included one scale (working together) with two items, and the interpersonal style domain included two scales (compassionate/respectful and discrimination due to race-ethnicity) with three and two items, respectively. Response options ranged from never to always, resulting in a 1–5 score for each item. Questions assessing communication include, “How often did doctors explain your test results such as blood tests, X-rays, or cancer-screening tests?” and “How often did doctors let you say what you thought was important?” A sample question from the decision-making domain is, “How often did you and your doctors work out a treatment plan together?” A sample question from the interpersonal style domain is, “How often were doctors concerned about your feelings?”
We assessed participation in recommended self-care activities using the Summary of Diabetes Self-Care Activities survey. This measure has been validated in both Spanish and English in adults with type 2 diabetes and asks patients to report their level of participation in several aspects of diabetes care (diet, exercise, foot care, blood glucose monitoring, and medication adherence).27,28
The Patient Health Questionnaire-2 (PHQ-2) was used to capture depressive symptoms.29 Health status was measured by asking participants, “In general, would you say your health is: excellent, very good, good, fair, or poor?” Due to distribution of results, health status responses were collapsed into three categories: (1) excellent/good/very good, (2) fair, and (3) poor. Demographic information was collected on age (in years), gender (male or female), education (0–6 years, 7–11 years, and 12 or more years), marital status (married/living with someone, yes/no), birthplace (US, Mexico, or other), yearly household income (0–12,499 dollars, 12,000–17,499 dollars, 17,500–24,999 dollars, and 25,000 dollars or more) and health insurance status (having any insurance yes/no). Number of primary care visits (in the last 12 months), length of time with diabetes (years), and current use of insulin were also measured.
Clinical variables were obtained from the diabetes registry, including LDL-cholesterol (LDL-c), hemoglobin A1C (A1C), blood pressure, weight, and height. Prescription medications, diagnoses of depression, hypertension, and high cholesterol were obtained from the medical chart. Receipt of processes of diabetes care such as receipt of foot examination, retinal examination, and flu shots was also abstracted from the medical chart.
Statistical Analysis
Frequencies were calculated for categorical variables, and means and standard deviations were reported for continuous variables. The mean and standard deviation were calculated for each IPC scale score. The corresponding Cronbach’s alpha values were calculated to estimate the internal consistency reliability of each scale.30 IPC multi-item composite measures were calculated as continuous scores (1–5) and had positively skewed distributions. As in prior studies, due to the skewed distribution of the results, IPC scores were then dichotomized into (1) optimal scores (defined as a value of 5 for most items except “lack of clarity” and “discriminated,” which had optimal scores of 1, and (2) sub-optimal scores (defined as values less than 5 for all items except for “lack of clarity” and “discriminated,” which had suboptimal scores greater than 1).7
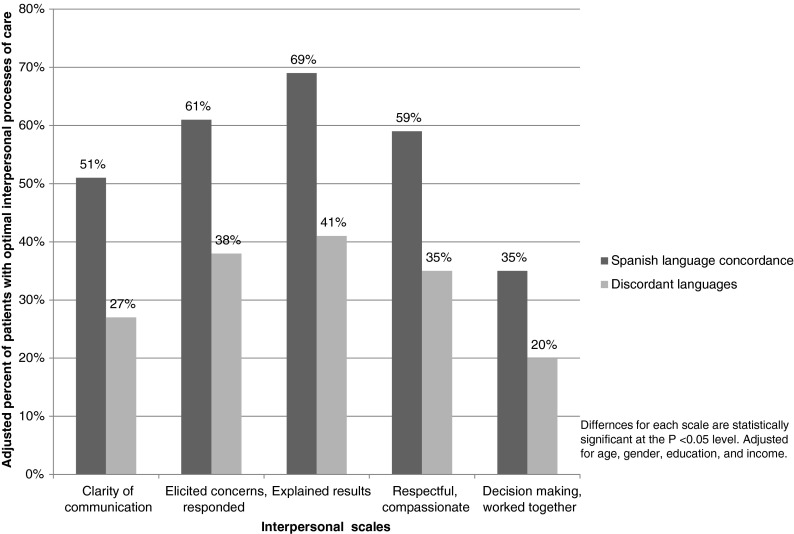
One-way analysis of variance (ANOVA) tests were used to compare patient characteristics and mean IPC scores between language-concordant and language-discordant patient groups (Tables 1 and 2). We used multivariable logistic regressions to estimate the odds ratios and to predict the adjusted percent with optimal IPC scores, controlling for age, gender, education, and income (Fig. 1). Adjusted predicted percentages provide a clear illustration of the marginal differences between groups. We selected factors hypothesized to influence IPC measures in prior research.3,7,31 The percent of patients with optimal adjusted IPC scores were calculated, and language-concordant and language-discordant groups were compared.
Table 1.
Characteristics of study participants by language concordance
| Characteristics of study participants | Sample (n = 250) | Language discordant (n = 120) | Language concordant (n = 128) | P-value |
|---|---|---|---|---|
| Age, mean years (SD) | 54.4 (12.5) | 53.1 (13.1) | 55.2 (12.4) | 0.21 |
| Female (%) | 58.0 | 53.2 | 66.7 | 0.03 |
| Education | ||||
| 0–6 years completed (%) | 60.7 | 75.4 | 53.5 | 0.001 |
| 7–11 years completed (%) | 20.5 | 13.5 | 23.3 | |
| 12 or more years completed (%) | 18.8 | 11.1 | 23.2 | |
| Married or living with someone (%) | 76.8 | 80.2 | 74.8 | 0.49 |
| Birthplace | ||||
| USA (%) | 17.3 | 4.8 | 28.8 | <0.001 |
| Mexico (%) | 78.7 | 91.3 | 67.8 | |
| Other country (%) | 4.0 | 4.0 | 3.4 | |
| Yearly household income | ||||
| 0–12,499 dollars (%) | 31.0 | 32.9 | 30.0 | 0.89 |
| 12,500–17,499 dollars (%) | 24.4 | 24.7 | 23.8 | |
| 17,500–24,999 dollars (%) | 23.2 | 23.5 | 22.5 | |
| 25,000 dollars or more (%) | 21.4 | 18.8 | 23.8 | |
| Insured, any coverage (%) | 57.1 | 50.8 | 62.1 | 0.08 |
| Self-reported health status | ||||
| Excellent/very good/ good (%) | 23.7 | 20.5 | 27.7 | 0.18 |
| Fair (%) | 65.3 | 70.5 | 58.9 | |
| Poor (%) | 10.9 | 9.0 | 13.4 | |
| Primary care visits (mean)* | 3.77 | 3.75 (2.3) | 3.78 (2.4) | 0.90 |
| High cholesterol (%) | 77.7 | 80.5 | 75.8 | 0.34 |
| Hypertension (%) | 77.6 | 78.7 | 76.3 | 0.64 |
| PHQ-2 score, mean (SD)† | 1.76 (0.86) | 1.6 (0.7) | 1.9 (0.9) | 0.01 |
| Years with diabetes, mean, (SD) | 10.5 (9.8) | 12.2 (12.6) | 9.4 (9.6) | 0.003 |
| Current Insulin use (%) | 14.8 | 15.8 | 14.4 | 0.77 |
*Defined as the number of visits with a primary care physician in the 12 months prior to the interview
†PHQ = Patient Health Questionnaire
Table 2.
Unadjusted mean values for IPC scale items for total sample (N = 250) and by language concordance
| Domain scale* | α | Total sample | Language concordant | Language discordant | P-Value†† |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| Communication | |||||
| Lack of clarity† (2 items) | 0.82 | 2.01 (0.98) | 1.80 (0.88) | 2.24 (1.04) | <0.001 |
| Elicited concerns, responded (3 items) | 0.89 | 4.27 (0.91) | 4.42 (0.80) | 4.18 (0.94) | 0.03 |
| Explained results (2 items) | 0.91 | 4.18 (1.02) | 4.36 (0.85) | 4.03 (1.12) | 0.008 |
| Decision making | |||||
| Decided together (2 items) | 0.89 | 3.09 (1.41) | 3.32 (1.35) | 2.89 (1.31) | 0.02 |
| Interpersonal style | |||||
| Compassionate, respectful (3 items) | 0.79 | 4.30 (0.80) | 4.46 (0.69) | 4.18 (1.41) | 0.007 |
| Discriminated† (2 items) | 0.81 | 1.03 (0.18) | 1.02 (0.11) | 1.04 (0.23) | 0.22 |
*All measures are on a scale of 1–5
†High equals worse IPC
††Corresponds to comparison of mean ratings between language-concordant and -discordant groups calculated by one-way analysis of variance
α = alpha, internal consistency reliability of items in scales
Figure 1.
Adjusted percent of participants with optimal interpersonal processes of care (IPC) by language concordance. Black bars = patient-provider language concordance; gray bars = patient-provider language discordance. IPC multi-item composite measure scores were calculated as continuous scores (1 – 5), had positively skewed distributions, and were dichotomized into (1) optimal scores (defined as a value of 5 for most items except “lack of clarity” and “discriminated,” which had optimal scores of 1, and (2) suboptimal scores (defined as values less than 5 for all items except for “lack of clarity” and “discriminated,” which had suboptimal scores of greater than 1)
We also conducted bivariate analysis using one-way ANOVA to evaluate whether language concordance was associated with greater participation in diabetes self-care activities.
To demonstrate that any observed association with IPC scores was not due to a cut point artifact, we computed our estimates using linear regression models, one for each scale, which included IPC scores as continuous variables. STATA 11.1 (College Station, TX) was used for all analyses.
RESULTS
The mean age of respondents was 54.4 ± 12.5 years. Most respondents were female (58 %), had less than a high school education (81.2 %), were married (76.8 %), were born in Mexico (78.7 %), and had annual incomes of less than $25,000 (78.6 %). Fifty-seven percent had health insurance and most reported fair to poor health status (76.3 %). Many participants had hypertension (69 %) and hyperlipidemia (78 %). The mean A1C, blood pressure, and LDL-c were 7.8 % (SD 1.8), 128/75 mmHg (SD18/11), and 96.7 (SD 18.5), respectively. The average time since diagnosis of diabetes was 10.5 years, and 14.8 % of respondents required insulin at the time of the study. Forty-eight percent of individuals had language-concordant providers (Table 1).
The response rate for the physician survey was 90 %. Of the 28 physicians that completed the survey, 93 % were board certified and 64 % were family physicians. Their mean age was 48 ± 11 years with 9 ± 9 years of clinical experience. The majority (68 %) were female and a minority (9 %) were Latino.
IPC scores of patients were skewed, with most respondents giving favorable scores for each domain. Cronbach’s alpha values for the domains ranged from 0.79 to 0.89, indicating good internal consistency reliability of questions. Patient-provider language concordance was associated with better IPC scores across the domains of communication, decision-making, and interpersonal style. Language-concordant providers were more likely to be viewed as communicating clearly (p < 0.001), eliciting and responding to concerns (p = 0.03), and explaining results (p = 0.008). Patients with language-concordant providers were more likely to feel that they were involved in the decision-making process (p = 0.02) and were more likely to view their provider as respectful and compassionate (p = 0.007). Patient-provider language concordance did not impact patient perception of discrimination (Table 2).
Differences in IPC scores between language-concordant and -discordant individuals persisted after adjusting for age, gender, education, and income. Language-concordant individuals were more likely than language-discordant individuals to have optimal adjusted IPC scores regarding clarity of communication, eliciting concerns, explaining results, being respectful, and being compassionate and working together. The predicted percent of patients with optimal adjusted IPC scores for these items ranged from 20 % to 41 % for language-discordant patients and 35 % to 69 % for language-concordant patients, and all differences were statistically significant (p < 0.05) (Fig. 1).
In the sensitivity analyses, the statistically significant association between language concordance and IPC scores persisted in the expected direction when we analyzed IPC scores as continuous variables and adjusted the regression models with the same pre-specified covariates used in the main analyses.
In bivariate analysis of language concordance and diabetes self-care, there was a statistically significant association between language concordance and higher participation in foot care (1.4 days vs. 0.7 days, p value 0.01). However, bivariate analysis of language concordance showed no association with healthy eating (5.2 vs. 5.3 days, p value 0.64), exercise (3.4 vs. 3.3 days, p value 0.44), self-monitoring (4.8 vs. 4.6 days, p value 0.44), or medication adherence (6.8 vs. 6.8 days, p value 0.65) (online Appendix).
DISCUSSION
In this study of Spanish-speaking rural Latinos with diabetes, we found that Spanish fluency of a provider is independently associated with better patient-reported IPC ratings. We also found that language concordance is associated with greater participation in foot care, but not greater participation in other recommended diabetes self-care activities. These results suggest that access to bilingual providers results in better care experiences and may also result in greater self-care among LEP Latinos in rural settings.
This is the first study of its kind to focus on the impact of patient-provider language concordance in rural Latino patients. Rural Latinos are an understudied yet growing population in the US.22–24 Due to their predominantly agricultural and mostly seasonal employment as well as other contextual circumstances, they have unique health care needs and face unique barriers in accessing health services.20,32 Thus, the effect of language concordance may be particularly important for improving health for this subgroup of Latinos.
Our findings are consistent with comparable studies that demonstrate the positive influence of language concordance on IPC and patient satisfaction for Spanish speakers seeking care in urban clinics.4,7,14 In our study, patients with Spanish-speaking providers gave more favorable IPC ratings for all components measured other than discrimination. Language is essential for optimal communication and decision-making, and shared language likely affects the ability to express compassion and respect. On the other hand, physicians working in the safety net may be more likely to express dedication to caring for the underserved and thus may be less likely to discriminate based on race-ethnicity regardless of Spanish fluency.33 In addition to physician characteristics, health system factors, such as access to interpreters, likely play an important role in patient ratings of IPC for this patient population.
Previous research has shown that language concordance improves medication adherence and receipt of health education.13,34 Studies also demonstrate that language concordance can have a positive impact on health.11,19,35 A cross-sectional study of a diabetes population receiving care at a Kaiser HMO found that Latinos with language-concordant providers were less likely to have poorly controlled diabetes, defined as an A1C > 9 %.11
Relatively little of the variation in glycemic control in people with diabetes is attributable to individual physician-level factors.36,37 In contrast, patient participation in self-care plays an important role in disease control and in preventing complications.38 Not unexpectedly, our study suggests that language concordance promotes improved participation in diabetes self-care. This is consistent with previous research showing an association between participation in self-care and ratings of patient-provider communication.18,39
It is unclear why the impact of language concordance was limited to improved participation in foot care in our study. Factors other than language ability of the provider may have a substantial impact on participation in other diabetes self-care activities in our study population. It is possible that even the language-discordant providers had high enough IPC scores to provide adequate patient education for most self-care activities. This could be because of organizational cultural competence programs, access to professional interpreters and bilingual staff, as well as a diabetes education program.40 These system-level effects may increase participation in self-care for all patients regardless of the ability of a provider to speak Spanish fluently.
Our study has limitations. This study is cross sectional; therefore, we can only test the associations between language concordance, IPC scores, and participation in diabetes self-care activities rather than establishing a causal relationship. Unmeasured factors other than language of the provider could impact IPC scores and health behaviors. We did not measure provider language fluency objectively and relied on self-report. Although we found some impact of language concordance on a validated self-reported diabetes self-care scale, we did not have objective measures of diabetes self-care. Our study population was predominately low income, so the findings may not be generalizable to other Spanish-speaking Latino patients with diabetes or non-Latino LEP patients.
Moreover, this study was powered primarily to detect an association between language concordance and IPC scores, our primary pre-specified analysis. Therefore, our ability to test for associations between language concordance and diabetes self-care was limited.
This is the first study to explore the relationship among language concordance, IPC measures, and participation in diabetes self-care for rural, low income, Spanish-speaking patients. Our study supports that shared language is important for establishing a high-quality patient-physician relationship. This finding supports steps to create a more diverse physician workforce, to promote development of language skills in physicians, and to encourage use of trained interpreters. Additional adequately powered studies are needed to clarify the presence and strength of the relationship between language concordance and participation in self-care activities and to study the impact of language concordance on objective measures of diabetes self-care, process, and outcomes, such as A1C. Defining IPC processes and factors external to the physician-patient interaction that effect chronic disease management will also be important for creating effective interventions to ensure high-quality care for LEP patients.
Electronic supplementary material
(DOC 28 kb)
Acknowledgments
Dr. Detz is supported by the Institutional National Science Research Award fellowship at UCLA (grant no. T32-HP-19001). Dr. Moreno is supported by the Robert Wood Johnson Foundation Clinical Scholars® Program at UCLA, by the UCLA Resource Center for Minority Aging Research/Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA grant P30AG021684 (PI Mangione), and by the California Endowment. Dr. Mangione’s effort is supported in part by the UCLA Robert Wood Johnson Clinical Scholars Program® and the US Department of Veterans Affairs (grant no. 67799), the University of California, Los Angeles, Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA grant P30-AG021684, and from the NIH/NCATS UCLA CTSI grant no. UL1TR000124 and the Barbara A. Levey and Gerald S. Levey Endowed Chair in Medicine. Dr. Morales’s effort was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award no. UL1TR000423. The content does not necessarily represent the official views of the NIA or the NIH. We acknowledge Marilu Isiordia for her assistance with data collection.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
References
- 1.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 2.Hsiao CJ, Boult C. Effects of quality on outcomes in primary care: a review of the literature. Am J Med Qual. 2008;23(4):302–310. doi: 10.1177/1062860608315643. [DOI] [PubMed] [Google Scholar]
- 3.Stewart AL, Napoles-Springer AM, Gregorich SE, Santoyo-Olsson J. Interpersonal processes of care survey: patient-reported measures for diverse groups. Health Serv Res. 2007;42(3 Pt 1):1235–1256. doi: 10.1111/j.1475-6773.2006.00637.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Napoles AM, Gregorich SE, Santoyo-Olsson J, O'Brien H, Stewart AL. Interpersonal processes of care and patient satisfaction: do associations differ by race, ethnicity, and language? Health Serv Res. 2009;44(4):1326–1344. doi: 10.1111/j.1475-6773.2009.00965.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saultz JW, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004;2(5):445–451. doi: 10.1370/afm.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernandez A, Schillinger D, Grumbach K, et al. Physician language ability and cultural competence. An exploratory study of communication with Spanish-speaking patients. J Gen Intern Med. 2004;19(2):167–174. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan C. Language Use in the United States: 2011, American Community Survey Reports: United States Census Bureau;2013
- 9.The National CLAS Standards. US Department of Health and Human Services Office of Minority Health. http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15. Accessed Aug 2014
- 10.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2011;26(2):170–176. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green AR, Ngo-Metzger Q, Legedza AT, Massagli MP, Phillips RS, Iezzoni LI. Interpreter services, language concordance, and health care quality. Experiences of Asian Americans with limited English proficiency. J Gen Intern Med. 2005;20(11):1050–1056. doi: 10.1111/j.1525-1497.2005.0223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ngo-Metzger Q, Sorkin DH, Phillips RS, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007;22(Suppl 2):324–330. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schenker Y, Karter AJ, Schillinger D, et al. The impact of limited English proficiency and physician language concordance on reports of clinical interactions among patients with diabetes: the DISTANCE study. Patient Educ Couns. 2010;81(2):222–228. doi: 10.1016/j.pec.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lasater LM, Davidson AJ, Steiner JF, Mehler PS. Glycemic control in English- vs Spanish-speaking Hispanic patients with type 2 diabetes mellitus. Arch Intern Med. 2001;161(1):77–82. doi: 10.1001/archinte.161.1.77. [DOI] [PubMed] [Google Scholar]
- 16.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: US trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med. 2009;150(8):505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 17.Mainous AG, 3rd, Diaz VA, Koopman RJ, Everett CJ. Quality of care for Hispanic adults with diabetes. Fam Med. 2007;39(5):351–356. [PubMed] [Google Scholar]
- 18.Karter AJ, Ferrara A, Darbinian JA, Ackerson LM, Selby JV. Self-monitoring of blood glucose: language and financial barriers in a managed care population with diabetes. Diabetes Care. 2000;23(4):477–483. doi: 10.2337/diacare.23.4.477. [DOI] [PubMed] [Google Scholar]
- 19.Hacker K, Choi YS, Trebino L, et al. Exploring the impact of language services on utilization and clinical outcomes for diabetics. PLoS One. 2012;7(6):e38507. doi: 10.1371/journal.pone.0038507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arcury TA, Quandt SA. Delivery of health services to migrant and seasonal farmworkers. Annu Rev Public Health. 2007;28:345–363. doi: 10.1146/annurev.publhealth.27.021405.102106. [DOI] [PubMed] [Google Scholar]
- 21.Daviglus ML, Talavera GA, Aviles-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. Jama. 2012;308(17):1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blewett LA, Smaida SA, Fuentes C, Zuehlke EU. Health care needs of the growing Latino population in rural America: focus group findings in one midwestern state. J Rural Health. 2003;19(1):33–41. doi: 10.1111/j.1748-0361.2003.tb00539.x. [DOI] [PubMed] [Google Scholar]
- 23.Villarejo D. The health of US hired farm workers. Annu Rev Public Health. 2003;24:175–193. doi: 10.1146/annurev.publhealth.24.100901.140901. [DOI] [PubMed] [Google Scholar]
- 24.Wu S, Ridgely MS, Escarce JJ, Morales LS. Language access services for Latinos with limited English proficiency: lessons learned from Hablamos Juntos. J Gen Intern Med. 2007;22(Suppl 2):350–355. doi: 10.1007/s11606-007-0323-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diamant AL, Babey SH, Hastert TA, Brown ER. Diabetes: the growing epidemic. Policy Brief UCLA Cent Health Policy Res. 2007;(PB2007-9):1–12 [PubMed]
- 26.Diabetes in California Counties: Prevalence, Risk Factors and Resources. Sacramento, CA: California Diabetes Control Program, California Department of Health Services 2005
- 27.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 28.Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med. 2003;18(8):624–633. doi: 10.1046/j.1525-1497.2003.31968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 30.Nunnally JC., Jr . Psychometric Methods. New York: McGraw-Hill; 1978. [Google Scholar]
- 31.Stewart AL, Napoles-Springer A, Perez-Stable EJ. Interpersonal processes of care in diverse populations. Milbank Q. 1999;77(3):305–339. doi: 10.1111/1468-0009.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwarte L, Samuels SE, Capitman J, Ruwe M, Boyle M, Flores G. The Central California Regional Obesity Prevention Program: changing nutrition and physical activity environments in California's heartland. Am J Public Health. 2010;100(11):2124–2128. doi: 10.2105/AJPH.2010.203588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Odom Walker K, Ryan G, Ramey R, et al. Recruiting and retaining primary care physicians in urban underserved communities: the importance of having a mission to serve. Am J Public Health. 2010;100(11):2168–2175. doi: 10.2105/AJPH.2009.181669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25(11):1172–1177. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mehler PS, Lundgren RA, Pines I, Doll K. A community study of language concordance in Russian patients with diabetes. Ethn Dis. 2004;14(4):584–588. [PubMed] [Google Scholar]
- 36.Hofer TP, Hayward RA, Greenfield S, Wagner EH, Kaplan SH, Manning WG. The unreliability of individual physician "report cards" for assessing the costs and quality of care of a chronic disease. JAMA J Am Med Assoc. 1999;281(22):2098–2105. doi: 10.1001/jama.281.22.2098. [DOI] [PubMed] [Google Scholar]
- 37.Krein SL, Hofer TP, Kerr EA, Hayward RA. Whom should we profile? Examining diabetes care practice variation among primary care providers, provider groups, and health care facilities. Health Serv Res. 2002;37(5):1159–1180. doi: 10.1111/1475-6773.01102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabet Metab Disord. 2013;12(1):14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17(4):243–252. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Jaimes FN, Batts F, Noguera C, Guerrero L, Moreno G. Implementation of language assessments for staff interpreters in community health centers. J Health Care Poor Underserved. 2013;24(3):1002–1009. doi: 10.1353/hpu.2013.0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 28 kb)