ABSTRACT
BACKGROUND
There is limited information on depression in Haitians and this is partly attributable to the absence of culturally and linguistically adapted measures for depression.
OBJECTIVE
To perform a psychometric evaluation of the Haitian-Creole version of the PHQ-9 administered to men who have sex with men (MSM) in the Republic of Haiti.
DESIGN
This study uses a cross-sectional design and data are from the Integrated Behavioral and Biological HIV Survey (IBBS) for MSM in Haiti.
PARTICIPANTS
Inclusion criteria required that participants be male, ≥ 18 years, report sexual relations with a male partner in the last 12 months, and lived in Haiti during the past 3 months. Respondent Driven Sampling was used for participant recruitment.
MAIN MEASURES
A structured questionnaire was verbally administered in Haitian-Creole capturing information on sociodemographics, sexual behaviors, human immunodeficiency virus (HIV) status and depressive symptomatology using the PHQ-9. Psychometric analyses of the translated PHQ-9 assessed unidimensionality, factor structure, reliability, construct validity, and differential item functioning (DIF) across subgroups (age, educational level, sexual orientation and HIV status).
KEY RESULTS
In a study population of 1,028 MSM, the Haitian-Creole version of the PHQ-9 is unidimensional, has moderately high internal consistency reliability (α = 0.78), and shows evidence of construct validity where HIV-positive subjects have greater depression (p = 0.002). There is no evidence of DIF across age, education, sexual orientation or HIV status. HIV-positive MSM are twice as likely to screen positive for moderately severe and severe depressive symptoms compared to their HIV-negative counterparts.
CONCLUSIONS
There is strong evidence for the psychometric adequacy of the translated PHQ-9 screening tool as a measure of depression with MSM in Haiti. Future research is necessary to examine the predictive validity of depression for subsequent health behaviors or clinical outcomes among Haitian MSM.
Keywords: Depression, Haiti, HIV/AIDS, International health, men who have sex with men
INTRODUCTION
Little is known about depressive symptomatology amongst Haitian men who have sex with men (MSM) in the Republic of Haiti. Haitian MSM have been a hidden and stigmatized population since the early days of the acquired immunodeficiency syndrome (AIDS) epidemic,1 and despite 30 years of funded research on human immunodeficiency virus (HIV)/AIDS in Haiti, the emphasis has been on preventing mother-to-child transmission and clinical surveillance of the general population.2 However, recent work on Haitian MSM shows that 30 % of Haitian men living with AIDS in the United States self-report male-to-male sexual contact as their primary route of HIV transmission,3 and the majority of MSM living in Haiti report a bisexual orientation, which means they are able to contribute to a generalized HIV epidemic through bridges between them and heterosexual women in Haiti.4 While both studies provide previously unknown information about Haitian MSM, neither study reports on the mental health status of this population.
A review of the literature shows that depression is highly prevalent amongst MSM when compared to men in the general population;5–8 and MSM are known to be at-high risk for infection with HIV. A meta-analysis reported that HIV-positive gay men are nearly twice as likely to have experienced a recent episode of major depressive disorder as their HIV-negative counterparts,9 and other literature reports that depression is associated with sexual risk behavior,10–16 underutilization of HIV primary care services, 17 poor adherence to antiretroviral therapy,18–27 and lower self-efficacy in one’s ability to take antiretroviral therapy.28,29 Hence, measurement of depression amongst both MSM and HIV infected populations is warranted.
There is little information on the clinical manifestation of depression in Haitians infected with HIV and scant information on the prevalence of depression amongst persons of Haitian ancestry in general 30–36. The paucity of studies may be partly attributable to the absence of culturally and linguistically adapted instruments in the Haitian-Creole language 37,38. The few studies examining the mental health of Haitians have been primarily conducted in the US with questions administered in English 30–33,39.
STUDY OBJECTIVES
In this study, the authors conducted a psychometric evaluation of a culturally and linguistically adapted Haitian-Creole version of the PHQ-9. The PHQ-9 is a brief self-report screening instrument for depressive symptomatology that focuses on the nine diagnostic criteria for DSM-IV depressive disorders:40anhedonia, depressed, sleep problems, low energy, appetite problems, low self-esteem, trouble concentrating, psychomotor problem and suicide ideation. In a meta-analytical review, the PHQ-9 has been deemed acceptable for depression screening in a range of settings, countries and populations,41–46 has been rigorously evaluated in multi-ethnic populations showing strong evidence of validity, reliability and utility;47–54 and its psychometric properties have been evaluated in HIV infected populations.47,55,56
Therefore, the authors addressed three major research questions:
What is the reliability of the PHQ-9 amongst a sample of Haitian MSM?
What is the construct validity of the PHQ-9 in relation to HIV status in this population?
Are there any observed differences in item responses across sub-groups (age, educational level, HIV status and sexual orientation) that may be due to differential item functioning (DIF)?
METHODS
Study Design, Recruitment Methodology and Personnel
The Integrated Behavioral and Biological HIV Survey (IBBS) conducted between October and December 2011 used a cross-sectional design and respondent driven sampling (RDS) to recruit the hidden population of MSM throughout Haiti. Biological samples were collected by study personnel trained according to national standards in Haiti,2 and training on the collection of behavioral data was conducted by PSI, a global social marketing company in Haiti. The RDS approach used a system of coupons for recruiting eligible participants, which was initialized with specifically chosen study participants (“seeds”) who assisted in the recruitment at each study site.57 Study personnel evaluated the eligibility of potential study participants when they presented with coupons; then read to participants the informed consent script, the in-depth description of the research procedures (interview, blood sample, HIV testing) and the specific ethical considerations of the study prior to obtaining an informed consent.
Setting: Study Sites
The study was conducted across all ten administratively defined departments in Haiti, with 11 study sites across the nation where networks of MSM existed, or near an accessible safe house where screening and collection of bio-behavioral data were possible.
Participants: Inclusion/Exclusion Criteria
Study participants had to be male, aged 18 years or older, report sexual relations with a male sexual partner in the last 12 months, have lived in Haiti during the past 3 months, be in possession of a recruitment coupon, and know the first and last name of the person (“seed”) who gave them the coupon. However, study personnel did not capture the first or last name of study participants, and did not keep a list of identifiers other than for the 11 “seeds” chosen for each study site.
Study recruits were excluded from the study enrollment for the following reasons: incapable of understanding or giving clear consent (e.g., suspected of being under the influence of drugs or alcohol); already enrolled in the study; currently a peer educator; or having received a coupon from a stranger (does not know his recruiter).
An honorarium [200 Haitian Gourdes ($5 USD)] was given to all study participants who enrolled in the study even if they did not provide a blood sample, to offset their time and travel. Each enrolled participant could recruit up to three other participants; in this case, secondary compensation [100 Haitian Gourdes ($2.50 USD)] was offered for each participant recruited.
Measurement
A structured questionnaire was verbally administered to study participants, capturing information on sociodemographics, sexual behaviors, sexual orientation, number and type of sexual partners, alcohol or drug use, utilization of health services, knowledge and attitudes related to HIV, and rapid HIV testing was performed on all participants who consented. Length of time to complete the survey was approximately 45 min.
Depressive Symptomatology—PHQ-9
Depressive symptomatology was measured using the PHQ-9, which asks whether a symptom has been present more than half the time, over the past two weeks. The instrument uses a Likert type response format ranging from 0 (not at all) to 3 (everyday), and the total score ranges from 0 to 27 with five severity categories: minimal (0–4), mild (5–9), moderate (10–14), moderately severe (15–19) and severe (20–27).40
Translation and Content Validity of the PHQ-9
Forward-backward translation of the PHQ-9 [English to Haitian-Creole] and a content validity analysis were performed by a bilingual/bicultural panel of Haitian experts (professional translator, psychiatrist, social epidemiologist and social worker). Panel members had native knowledge of the cultural beliefs of depression, and the psychiatrist and social worker were familiar with the expressions of depression in the Haitian context based on their clinical practice.30 The bilingual translator performed the initial forward translation of the PHQ-9 from English to Haitian-Creole. Backward translation was performed by the social worker. Differences in translation between the original English and translated English versions were reviewed, and agreement was achieved by consensus with the psychiatrist and social epidemiologist. The vocabulary selected for the translated items incorporated expressions of depressive symptomatology that are familiar and routinely used with Haitian clients. In the final selection of terms, the panel performed a content validity analysis by examining the correspondence between items and the symptom content describing depression.
Statistical Analyses
Descriptive Statistics
Univariate statistics were generated and ceiling/floor effects were considered substantial if ≥ 20 % of subjects scored at the upper-most or bottom-most end of the PHQ-9 scale.58,59 Internal consistency reliability was assessed using Cronbach's alpha statistic.60 Ordinary least squares and multivariable regression were used to determine the association between the PHQ-9 score and HIV status. Ordinal logistic regression, using the proportional odds model, was used to predict PHQ-9 severity categories using HIV status, while adjusting for age, education and sexual orientation. The measure of magnitude consisted of the odds ratio with 95 % confidence intervals. Stata v12 61 and Microsoft Excel 62 were used to analyze the data.
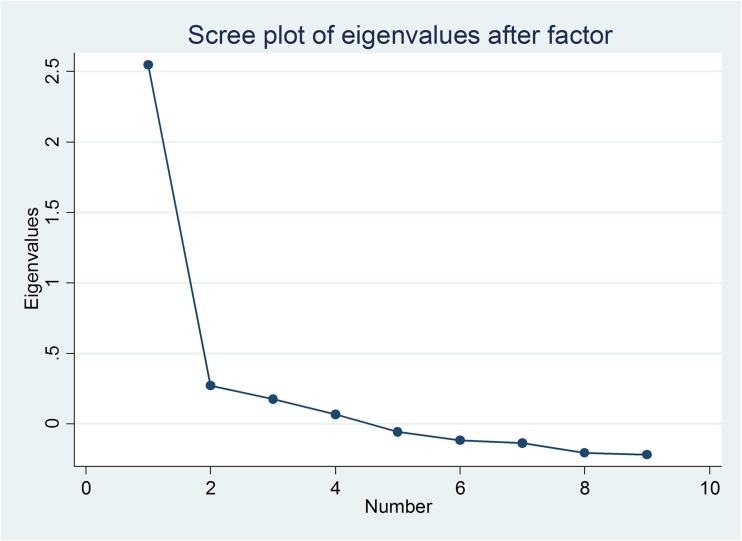
Factor Analysis
The principal factor method, with promax rotation, was used to identify the unobservable ‘latent’ factors that underlie or explain the set of observed variables.63–65 A scree plot of the positive eigenvalues of the adjusted correlation matrix was generated to determine if one or more factors accounted for most of the common variances among the nine items.66 Item discrimination was assessed with corrected item-total correlations.67
Differential Item Functioning
Drawing a parallel from the field of epidemiology to the field of psychometrics, the evaluation of uniform DIF and nonuniform DIF are analogous to confounding and effect modification, respectively (Personal Communication, Crane P, 2003). Evidence of DIF was defined using optimal cutoff values of an odd’s ratio > 2.0 or < 0.50.68–70
DIF was evaluated using logistic regression to predict item responses, controlling for the total scale score (unidimensional underlying construct) across the following: dichotomous categories for HIV Status (0 = negative; 1 = positive); polychotomous categories for sexual orientation (0 = homosexual, 1 = bisexual, 2 = heterosexual and 3 = transsexual); ordinal categories for age groups (0 = 18-24 years; 1 = 25-29 years; 2 = 30-44 years) and educational levels (0 = alphabetization; 1 = primary; 2 = secondary and 3 = superior). For example, the uniform DIF model for HIV status included an individual item of the PHQ-9 as the dependent variable, with the total PHQ-9 score and HIV status as independent variables, having 2° of freedom [PHQ9-Itemi = PHQ9-Score + HIV Status]; whereas the nonuniform DIF model added an interaction term to this equation [PHQ9-Itemi = PHQ9-Score + HIV Status + (PHQ9-Score* HIV Status)], having 3 of freedom.
BIOETHICS
The study protocol was approved by the Haitian Bioethics Committee in Port-au-Prince, Haiti. The Office of Human Research Protection at the Harvard School of Public Health granted an institutional review board (IRB) exemption waiver for analyses of the de-identified data set.
RESULTS
Participant Characteristics
A total of 1,080 men who have sex with men participated in the study. After data entry, 52 questionnaires were removed from analysis, either because of very incomplete data or non-eligibility. Of the remaining 1,028 MSM, the mean age is 23.2 years (SD ± 5.2, range 18–45). Almost 60 % (N = 615) of the study participants completed secondary education; and sexual orientation is reported as homosexual (45.2 %), bisexual (47.4 %), heterosexual (4.7 %) and transsexual (1.9 %).
Scale Statistics, Reliability and Differential Item Functioning
Univariate statistics show a mean depression score ( =6.6) and the prevalence of moderately severe and severe symptomatology is 7.1 % (higher score indicating greater severity of depression) (Table 1). There were no ceiling or floor effects observed, with 8.9 % (n = 91) of study participants having a minimum score of 0, and 0.001 % (n = 1) with a maximum score of 27. The Cronbach coefficient alpha for the PHQ-9 is α = 0.78, confirming a moderately high level of internal consistency. The reliability coefficient suggests that a large proportion of the scale’s total variance is attributed to a common source.
=6.6) and the prevalence of moderately severe and severe symptomatology is 7.1 % (higher score indicating greater severity of depression) (Table 1). There were no ceiling or floor effects observed, with 8.9 % (n = 91) of study participants having a minimum score of 0, and 0.001 % (n = 1) with a maximum score of 27. The Cronbach coefficient alpha for the PHQ-9 is α = 0.78, confirming a moderately high level of internal consistency. The reliability coefficient suggests that a large proportion of the scale’s total variance is attributed to a common source.
Table 1.
Psychometric Properties of the PHQ-9 and Severity Categories for Depressive Symptomatology
| N | Properties | |||||
|---|---|---|---|---|---|---|
| Total Observations | 1028 | |||||
| Mean (±SD) | 6.6 (±4.8) | |||||
| Min | 0 | |||||
| Max | 27 | |||||
| Skewness | 0.8 | |||||
| Kurtosis | 3.5 | |||||
| Chronbach Alpha | 0.78 | |||||
| PHQ-9 Severity Categories | N | % | HIV+ | % | HIV - | % |
| Minimal (0-4) | 378 | 36.8 | 46 | 27.2 | 283 | 37.1 |
| Mild (5-9) | 411 | 40.0 | 72 | 42.6 | 308 | 40.4 |
| Moderate (10-14) | 166 | 16.2 | 30 | 17.8 | 125 | 16.4 |
| Moderately Severe (15-19) | 62 | 6.0 | 18 | 10.7 | 41 | 5.4 |
| Severe (20-27) | 11 | 1.1 | 3 | 1.8 | 6 | 0.8 |
| Total | 1028 | 100.0 | 169 | 763 | ||
| Prevalence of Moderately Severe or Severe | 73 | 7.1 | 47 | 12.4 | 21 | 6.2 |
| HIV + vs. HIV- [Odds Ratio (95 % CI)] | 2.2 (1.3-3.7) | |||||
*HIV status was not available for all study participants
A stratified analysis across age, education, and sexual orientation assessed representative reliability. Reliability across age groups (18–24, 25–29, and 30–44) ranges from α = 0.75 to α = 0.79. Across education, for those receiving more formal education (primary, secondary and superior), reliability ranges from α = 0.77 to α = 0.80. For the subgroup achieving less than formal education (alphabetization), reliability is lowest at α = 0.48; however, this is a sample of only 13 persons. Across sexual orientation, reliability ranges from α = 0.61 to α = 0.82.
Factor Analysis and Differential Item Functioning
A scree plot was used to establish the number of distinct factors (Fig. 1). Results show one dominant dimension with a large decrease between the first and second eigenvalues and small decreases thereafter, suggesting unidimensionality, required to assess DIF. Factor loadings ranged from 0.45 to 0.60 (i.e., above the 0.40 cutoff) (Table 2). The corrected item-total correlations show how each individual item is correlated with the scale computed only from the other eight items, and this ranges from 0.38 to 0.52. “Low energy” was the most highly endorsed item (mean 1.14).
Figure 1.
Scree Plot of Eigenvalues after Factor Analysis
Table 2.
Factor Analysis
| Item number | PHQ-9 Questions | Factor Loading | Item-total Correlation | Item Mean | Item SD |
|---|---|---|---|---|---|
| 1 | Anhedonia | 0.45 | 0.40 | 0.59 | 0.76 |
| 2 | Depressed | 0.59 | 0.53 | 0.73 | 0.87 |
| 3 | Sleep problems | 0.50 | 0.46 | 0.82 | 0.91 |
| 4 | Low energy | 0.53 | 0.48 | 0.91 | 0.95 |
| 5 | Appetite problems | 0.49 | 0.45 | 0.89 | 0.97 |
| 6 | Low self esteem | 0.60 | 0.53 | 0.84 | 0.91 |
| 7 | Trouble concentrating | 0.55 | 0.50 | 0.69 | 0.86 |
| 8 | Psychomotor problems | 0.55 | 0.50 | 0.62 | 0.89 |
| 9 | Suicide ideation | 0.55 | 0.44 | 0.47 | 0.80 |
Results show no evidence of DIF across HIV status, age, education or sexual orientation (Table 3). We purposefully selected an effect size cut-point (odds ratio > 2.0 or < 0.50) to define a meaningful level of item bias, similar to other authors.68–70 We did so to take the emphasis off the p value and focus on the measure of association; and the results in Table 3 show no odds ratio that meets the effect size cut-point, which suggests no evidence of DIF.
Table 3.
Differential Item Functioning Across Age, Education, Sexual Orientation and HIV Status
| Age | Education | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uniform | Nonuniform | Uniform | Nonuniform | |||||||||
| OR | CI | p | OR | CI | p | OR | CI | p | OR | CI | p | |
| Q1 | 1.09 | (0.91–1.32) | 0.35 | 1.00 | (0.96–1.05) | 0.48 | 1.71 | (1.37–2.13) | < 0.001 | 1.05 | (1.00–1.09) | < 0.0 |
| Q2 | 1.19 | (0.99–1.43) | 0.06 | 1.02 | (0.98–1.07) | 0.31 | 0.96 | (0.74–1.23) | 0.73 | 1.03 | (0.97–1.10) | 0.26 |
| Q3 | 1.04 | (0.87–1.25) | 0.65 | 1.00 | (0.96–1.04) | 0.91 | 1.13 | (0.91–1.39) | 0.26 | 1.00 | (0.96–1.05) | 0.88 |
| Q4 | 1.00 | (0.83–1.21) | 0.94 | 1.03 | (0.98–1.08) | 0.21 | 0.83 | (0.67–1.02) | 0.08 | 1.00 | (0.95–1.15) | 0.91 |
| Q5 | 1.03 | (0.86–1.23) | 0.72 | 1.03 | (0.99–1.08) | 0.11 | 1.12 | (0.91–1.38) | 0.28 | 1.02 | (0.97–1.06) | 0.45 |
| Q6 | 1.00 | (0.82–1.22) | 0.96 | 0.95 | (0.91–0.99) | 0.02 | 0.90 | (0.71–1.12) | 0.34 | 1.00 | (0.96–1.05) | 0.85 |
| Q7 | 0.84 | (0.68–1.04) | 0.12 | 0.95 | (0.90–0.99) | <0.03 | 1.22 | (0.99–1.51) | 0.06 | 0.99 | (0.94–1.03) | 0.6 |
| Q8 | 1.01 | (0.82–1.24) | 0.92 | 0.98 | (0.93–1.03) | 0.54 | 0.81 | (0.64–1.01) | 0.06 | 0.98 | (0.93–1.04) | 0.62 |
| Q9 | 1.12 | (0.92-1.37) | 0.23 | 1 | (0.95–1.04) | 0.97 | 0.72 | (056–0.93) | < 0.01 | 0.96 | (0.91–1.01) | 0.19 |
| Sexual Orientation | HIV Status | |||||||||||
| Uniform | Nonuniform | Uniform | Nonuniform | |||||||||
| OR | CI | p | OR | CI | p | OR | CI | p | OR | CI | p | |
| Q1 | 1.16 | (0.88–1.53) | 0.29 | 0.96 | (0.90–1.02) | 0.22 | 1.00 | (0.69–1.45) | 0.99 | 1.00 | (0.90–1.05) | 0.53 |
| Q2 | 1.11 | (0.84–1.46) | 0.46 | 1.00 | (0.94–1.08) | 0.84 | 1.00 | (0.69–1.46) | 0.96 | 1.01 | (0.92–1.10) | 0.81 |
| Q3 | 0.86 | (0.66–1.12) | 0.27 | 1.02 | (0.96–1.08) | 0.58 | 1.51 | (1.08–2.12) | 0.02 | 0.97 | (0.89–1.06) | 0.49 |
| Q4 | 0.81 | (0.62–1.04) | 0.1 | 0.96 | (0.90–1.02) | 0.16 | 1.02 | (0.71–1.48) | 0.89 | 0.97 | (0.89–1.05) | 0.49 |
| Q5 | 0.90 | (0.69–1.17) | 0.4 | 0.98 | (0.92–1.04) | 0.59 | 0.85 | (0.61–1.19) | 0.36 | 1.02 | (0.94–1.09) | 0.64 |
| Q6 | 0.85 | (0.65–1.11) | 0.24 | 0.99 | (0.93–1.05) | 0.75 | 1.07 | (0.76–1.52) | 0.69 | 0.98 | (0.90–1.67) | 0.68 |
| Q7 | 1.02 | (0.77–1.34) | 0.90 | 0.99 | (0.92–1.05) | 0.72 | 0.66 | (0.44–0.98) | 0.04 | 0.94 | (0.87–1.01) | 0.12 |
| Q8 | 1.08 | (0.81–1.44) | 0.61 | 0.96 | (0.90–1.03) | 0.31 | 0.98 | (0.69–1.40) | 0.93 | 1.04 | (0.95–1.14) | 0.41 |
| Q9 | 1.24 | (0.91–1.69) | 0.17 | 0.96 | (0.89–1.02) | 0.24 | 1.03 | (0.67–1.59) | 0.87 | 0.92 | (0.84–1.00) | 0.07 |
Uniform DIF results have 2° of freedom. Nonuniform DIF results have 3° of freedom
Construct Validity: Relationship Between PHQ-9, HIV Status and Sexual Orientation
Using ordinary least squares regression, results showed that the PHQ-9 depression score was significantly higher for participants testing positive for HIV (p = 0.002), and this remained significant in a multivariable model adjusting for age and educational attainment. The depression score was also noted to have an inverse relationship with education (p = 0.04), suggesting that participants with lower educational attainment have higher depression scores.
When combined categories for the PHQ-9 of moderately severe and severe symptoms are stratified across HIV status, the prevalence of depressive symptomatology is 6.2 % vs. 12.4 % for HIV-negative versus HIV-positive study participants (OR = 2.2, 95 % CI 1.3–3.7), respectively (Table 1). These findings suggests that HIV-positive Haitian MSM are twice as likely to screen for symptoms that are indicative of major depression, compared to their HIV-negative counterparts in this study population.
DISCUSSION
To our knowledge, this is the first study to investigate the prevalence of depressive symptoms amongst Haitian MSM and also the first study to examine the psychometric properties of the translated version of the Haitian-Creole Patient Health Questionnaire (PHQ-9) for use with Haitian populations. There are three major findings.
First, there is strong evidence of psychometric adequacy for the translated measure. In our study, the properties of the PHQ-9 are similar to those reported for the PHQ-9 administered in western Kenya.47 The scree plot indicates one dominant dimension between first and second eigenvalues; low energy is the most highly endorsed item; factor loadings range from 0.45 to 0.60; internal consistency reliability is α = 0.78; and the instrument shows construct validity across HIV status. However, differences in floor and ceiling effects are negligible, which is similar to the findings in the study conducted in Kenya,47 but differs significantly from results reported by Crane, Gibbons, Willig et al., (2010) who found prominent floor effects.55 Also, there was no evidence of DIF across participant subgroups in the sample of Haitian MSM by age, education and sexual orientation. This also differs from the results reported by Crane, Gibbons, et al. (2010), whose findings suggested there are three individual items showing evidence of DIF with respect to race (African-American vs. White), sex and age.55
Second, HIV-positive Haitian MSM are twice as likely to screen positive for moderately severe and severe depressive symptoms compared to their HIV-negative counterparts, similar to the meta-analytical findings reported by Ciesla and Roberts (2001).9 Implications of these findings suggest that prioritization of funding to support psychological services for HIV-positive Haitian men is needed in this setting. To date, few tailored programs have been rigorously designed to address the special needs of MSM in Haiti.
Finally, the prevalence of moderately severe and severe depressive symptomatology is 7.1 % in this study population (Table 1), and this rate is remarkably similar to the 12-month prevalence (7.3 %) of any psychiatric disorder identified amongst Haitians living in the US, which was measured using the World Mental Health Composite International Diagnostic Interview (WMH-CIDI).71 These findings suggest that susceptibility to mental illness amongst Haitians in the homeland may be similar to that of Haitians in the Diaspora. Thus, results highlight the importance of future research to enhance our understanding and the variations within the respective larger social contexts of these populations.
LIMITATIONS
There are several study limitations. First, due to the highly selected nature of the sample (and the recruitment strategy using respondent-drive sampling), study results cannot be generalized to the larger Haitian population that would include women, older adults, individuals without HIV and/or who are heterosexual.
Second, criterion validity was not tested because this is the first translation of a Haitian-Creole instrument measuring depression. However, there is no translated version of a structured psychiatric interview for Haitian-Creole speakers. Given the dearth of research on the mental health of Haitians, future studies should identify the operating characteristics (optimal cutoff values, sensitivity and specificity) of the translated version of this instrument.
Third, construct validity was weakly tested against only one variable—HIV status—rather than comparing with constructs more robustly aligned with depression. To our knowledge, no other validated measures of depression exist in the Haitian-Creole language to assess convergence, and data on other domains aligned with depression, such as social/work/role functioning, were not captured in this study to assess correlations.
CONCLUDING REMARKS
This manuscript provides evidence supporting the PHQ-9 as a valid measure for assessing depressive symptomatology in a sample of Haitian MSM. Given the unique health risk factors and social vulnerabilities in this population, future research is necessary to examine the predictive validity of depression for subsequent health behaviors or clinical outcomes among Haitian MSM. For example, depressive symptomatology as assessed by the PHQ-9 might predict future engagement in sexual risk behaviors, HIV or sexually transmitted infections (STI) acquisition, substance use, or psychiatric outcomes in this population. This measure might thus be an appropriate tool for screening and targeting preventive interventions for members of this population. Furthermore, interventions to address and reduce depressive symptomatology among MSM in Haiti are warranted. In this sample, nearly one-quarter of MSM reported signs of moderate to severe depressive symptoms, and HIV-positive MSM had a twofold greater odds of reporting depressive symptoms compared with HIV-negative MSM. Therefore, validation of this measure provides a useful tool for future research, which is needed to screen, identify, and reduce depression in this highly vulnerable population. The study authors recommend that the measure be evaluated for its adequacy with the general population in Haiti, which is much needed for both research and clinical services.
Acknowledgments
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Contributors
The authors would like to thank the Republic of Haiti’s Programme National de Lutte contre le SIDA (Mme. Nirva Duval, Dr. Edieux Louissaint), Laboratoire National de Santé Publique (Dr. Jacques Boncy), SEROvie (Mr. Reginald Dupont), PSI LAC (Dr. Benjamin Nieto-Andrade), UNAIDS (Ms Kate Spring), FOSREF and POZ for their sustained support to the design and implementation of the study. We also thank Ms. Marie-Andre Pierre Victor (Social Worker, Codman Square Community Health Center, Dorchester, MA) and Mrs. Magalie Laraque (Translator, Port-au-Prince, Haiti) for their participation on the Bilingual/Bicultural Expert Panel; Dr. Charles Lewis (Department of Graduate Psychometrics, Fordham University, Bronx, NY), Dr. Janet St. Lawrence (Mississippi State University, Meridian), Dr. Don Operario (Brown University School of Public Health), Dr. David Williams (Harvard School of Public Health, Boston, MA) and Ms. Isabel Morgan (Mount Holyoke College) for reviewing the final draft of this manuscript.
Funders
The project was supported by funding from PEPFAR/USAID, KfW (Kreditanstalt für Wiederaufbau), the Global Fund to Fight AIDS, Malaria and Tuberculosis, the Elton John AIDS Foundation, PSI and Housing Works, Inc. Manuscript development was funded, in part, by a grant from the National Institutes of Health (L60 MD002421-02) and Fellowship (R25MH083620) awarded to the primary author, LGM.
Prior Presentations
Presented at the 19th International AIDS Conference in Washington, DC, July 26, 2012, ‘HIV in Haiti in the Time of Reconstruction, Epidemiology, Achievements, Challenges and Perspectives,’ Session THSA08.
REFERENCES
- 1.Malebranche R, Arnoux E, Guerin JM, Pierre GD, Laroche AC, Pean-Guichard C, et al. Acquired immunodeficiency syndrome with severe gastrointestinal manifestations in Haiti. Lancet. 1983;2(8355):873–8. doi: 10.1016/S0140-6736(83)90868-1. [DOI] [PubMed] [Google Scholar]
- 2.Haiti, Programme National de Lutte contre le SIDA (PNLS): Plan Strategique National Multisectoriel (2008–2012), in Date Accessed: September 26, 2012http://www.aidstar-one.com/sites/default/files/prevention/resources/national_strategic_plans/Haiti_2008-2012_French.pdf, Gourvernement de la Republique d'Haiti: Port-au-Prince, Haiti.
- 3.Marc LG, Patel-Larson A, Hall HI, Hughes D, Alegria M, Jeanty G, et al. HIV among Haitian-born persons in the United States, 1985–2007. AIDS. 2010;24(13):2089–2097. doi: 10.1097/QAD.0b013e32833bedff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.PSI Haiti, Understanding the needs of Haitian Men who have Sex with Men. Qualitative study. (unpublished). Port-au-Prince, Haiti, 2011, PSI Haiti.
- 5.Mills TC, Paul J, Stall R, Pollack L, Canchola J, Chang Y, et al. Distress and depression in men who have sex with men: the urban men's health study. Am J Psychiatr. 2004;161(2):278–285. doi: 10.1176/appi.ajp.161.2.278. [DOI] [PubMed] [Google Scholar]
- 6.Sandfort TG, de Graaf R, Bijl RV, Schnabel P. Same-sex sexual behavior and psychiatric disorders: Findings from the Netherlands mental health survey and incidence study (NEMESIS) Arch Gen Psychiatr. 2001;58(1):85–91. doi: 10.1001/archpsyc.58.1.85. [DOI] [PubMed] [Google Scholar]
- 7.Sivasubramanian M, Mimiaga MJ, Mayer KH, Anand VR, Johnson CV, Prabhugate P, et al. Suicidality, clinical depression, and anxiety disorders are highly prevalent in men who have sex with men in Mumbai, India: Findings from a community-recruited sample. Psychol Health Med. 2011;16(4):450–462. doi: 10.1080/13548506.2011.554645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nurius PS. Mental health implications of sexual orientation. J Sex Res. 1983;19(2):119–136. doi: 10.1080/00224498309551174. [DOI] [Google Scholar]
- 9.Ciesla JAMA, Roberts JEPD. Meta-Analysis of the Relationship Between HIV Infection and Risk for Depressive Disorders. Am J Psychiatr. 2001;158(5):725–730. doi: 10.1176/appi.ajp.158.5.725. [DOI] [PubMed] [Google Scholar]
- 10.Marks G, Bingman CR, Duval T. Negative affect and unsafe sex in HIV-positive men. AIDS and Behavior. 1998;2(2):89–99. doi: 10.1023/A:1022138712044. [DOI] [Google Scholar]
- 11.Martin, J.I. and J. Knox, Loneliness and sexual risk behavior in gay men. Psychological Reports, 1997. 81 (3, Pt 1): p. 815–825. [DOI] [PubMed]
- 12.Perkins DO, Leserman J, Murphy C, Evans DL. Psychosocial predictors of high-risk sexual behavior among HIV-negative homosexual men. AIDS Educ Prev. 1993;5(2):141–152. [PubMed] [Google Scholar]
- 13.Strathdee SA, Hogg RS, Martindale SL, Cornelisse PG, Craib KJ, Montaner JS, et al. Determinants of sexual risk-taking among young HIV-negative gay and bisexual men. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;19(1):61–6. doi: 10.1097/00042560-199809010-00010. [DOI] [PubMed] [Google Scholar]
- 14.Thompson SC, Nanni C, Levine A. The stressors and stress of being HIV-positive. AIDS Care. 1996;8(1):5–14. doi: 10.1080/09540129650125957. [DOI] [PubMed] [Google Scholar]
- 15.Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychol. 2001;20(4):291–299. doi: 10.1037/0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- 16.Kalichman SC, Weinhardt L. Negative affect and sexual risk behavior: Comment on Crepaz and Marks (2001) Health Psychol. 2001;20(4):300–301. doi: 10.1037/0278-6133.20.4.300. [DOI] [PubMed] [Google Scholar]
- 17.Saint-Jean G, Metsch L, Gomez-Marin O, Pierre C, Jeanty Y, Rodriguez A, et al. Use of HIV primary care by HIV-positive Haitian immigrants in Miami. Florida. AIDS Care. 2011;23(4):486–493. doi: 10.1080/09540121.2010.516339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boarts, J.M., E.M. Sledjeski, L.M. Bogart, Delahanty DL.The Differential Impact of PTSD and Depression on HIV Disease Markers and Adherence to HAART in People Living with HIV. AIDS and Behavior Vol 10 (3) May 2006, 253–261, 2006. [DOI] [PubMed]
- 19.Sledjeski, E.M., D.L. Delahanty, and L.M. Bogart.Incidence and Impact of Posttraumatic Stress Disorder and Comorbid Depression on Adherence to HAART and CD4-super (+) Counts in People Living with HIV. AIDS Patient Care and STDs Vol 19 (11) Nov 2005, 728–736, 2005. [DOI] [PubMed]
- 20.Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzadegan H, Howard AA, et al. Impact of Active Drug Use on Antiretroviral Therapy Adherence and Viral Suppression in HIV-infected Drug Users. Journal of General Internal Medicine. 2002;17(5):377–381. doi: 10.1007/s11606-002-0044-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19(2):124–133. doi: 10.1037/0278-6133.19.2.124. [DOI] [PubMed] [Google Scholar]
- 22.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 23.Gordillo V, del Amo J, Soriano V, Gonzalez-Lahoz J. Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. AIDS. 1999;13(13):1763–1769. doi: 10.1097/00002030-199909100-00021. [DOI] [PubMed] [Google Scholar]
- 24.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 25.Singh N, Squier C, Sivek C, Wagener M, et al. Determinants of compliance with antiretroviral therapy in patients with human immunodeficiency virus: Prospective assessment with implicaions for enhancing commpliance. AIDS Care. 1996;8(3):261–269. doi: 10.1080/09540129650125696. [DOI] [PubMed] [Google Scholar]
- 26.Starace F, Ammassari A, Trotta MP, Murri R, De Longis P, Izzo C, et al. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;15(31):S136–9. doi: 10.1097/00126334-200212153-00010. [DOI] [PubMed] [Google Scholar]
- 27.Waldrop-Valverde D, Valverde E. Homelessness and Psychological Distress as Contributors to Antiretroviral Nonadherence in HIV-Positive Injecting Drug Users. AIDS Patient Care and STDs. 2005;19(5):326–334. doi: 10.1089/apc.2005.19.326. [DOI] [PubMed] [Google Scholar]
- 28.Reynolds NR, Testa MA, Marc LG, Chesney MA, Neidig JL, Smith SR, et al. Psychosocial influences of attitudes and beliefs toward medication adherence in HIV + persons naïve to antiretroviral therapy: A cross-sectional survey. Journal of AIDS and Behavior. 2004;8(2):141–150. doi: 10.1023/B:AIBE.0000030245.52406.bb. [DOI] [PubMed] [Google Scholar]
- 29.Marc LG, Testa MA, Walker AM, Robbins GK, Shafer RW, Anderson NB, et al. Educational attainment and response to HAART during initial therapy for HIV-1 infection. J Psychosom Res. 2007;63(2):207–16. doi: 10.1016/j.jpsychores.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Nicolas G, Desilva AM, Subrebost KL, Breland-Noble A, Gonzalez-Eastep D, Manning N, et al. Expression and treatment of depression among Haitian immigrant women in the United States: clinical observations. Am J Psychother. 2007;61(1):83–98. doi: 10.1176/appi.psychotherapy.2007.61.1.83. [DOI] [PubMed] [Google Scholar]
- 31.Desrosiers, A., L.G. Marc, S. Leff, R. Frank, S. St Fleurose, and M. Alegria.Clinical Characteristics and Demographics Profile of A Group of Haitians Admitted to an Acute Psychiatric Unit. in Annual Meeting of the American Public Health Association, Mental Health Posters V, November 4–8. 2006. Boston, Massachusetts.
- 32.Desrosiers, A. and S. St Fleurose, Treating Haitian patients: key cultural aspects. Am J Psychother, 2002. 56 (4): p. 508–21. [DOI] [PubMed]
- 33.Nicolas G, DeSilva AM, Grey KS, Gonzalez-Eastep D, Manning N. Using a Multicultural Lens to Understand Illnesses Among Haitians Living in America. Prof Psychol Res Pract. 2006;37(6):702–707. doi: 10.1037/0735-7028.37.6.702. [DOI] [Google Scholar]
- 34.Marc L, Honore JG, Nejuste P, Setaruddin M, Lamothe NN, Thimothe G, et al. Uptake to HIV Post-Exposure Prophylaxis in Haiti: Opportunities to Align Sexual Violence, HIV PEP and Mental Health. Am J Reprod Immunol. 2013;69(Suppl 1):132–41. doi: 10.1111/aji.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marc, L.G., Mental Health Literacy in the Context of Emergencies, in Annual Conference of the Haitian Mental Health Network, Trauma and Mental Illness in the Haitian Community. May 5 . Massachusetts School of Professional Psychology. MA: West Roxbury; 2012. [Google Scholar]
- 36.Marc, L.G., Desrosiers, A., Coicou, N., Brennan, R., Vallie, R.A., Henderson, W., Pierre-Victor, M., Dabao, J., Jean, M., Guillaume, A.J., Avramovsk, V., Resnick, H., St. Lawrence. J., Testa, M.A.Abstract #278652: Association of depressive symptoms and socioeconomic position amongst Haitian women living in post-earthquake camps., in Program Agenda: 141st Annual Meeting of the American Public Health Association, November 2–62013, APHA: Boston, MA
- 37.Stewart AL, Napoles-Springer A. Health-related quality-of-life assessments in diverse population groups in the United States. Med Care. 2000;38(9 Suppl):II102–24. [PubMed] [Google Scholar]
- 38.Nicolas, G. and C.L. Whitt.Conducting qualitative research with a Black immigrant sample: Understanding depression among Haitian immigrant women, in Qualitative strategies for ethnocultural research2012, American Psychological Association; US: Washington, DC. p. 199–217.
- 39.Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–15. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 40.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. . J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coyne JC, Thombs BJ, Mitchell AJ. PHQ-9 and PHQ-2 in Western Kenya. J Gen Intern Med. 2009;24(7):890. doi: 10.1007/s11606-009-0985-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22(11):1596–602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gilbody S, Sheldon T, House A. Screening and case-finding instruments for depression: a meta-analysis. CMAJ. 2008;178(8):997–1003. doi: 10.1503/cmaj.070281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gilbody S, Sheldon T, Wessely S. Should we screen for depression? BMJ. 2006;332(7548):1027–30. doi: 10.1136/bmj.332.7548.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pignone MP, Gaynes BN, Rushton JL, Burchell CM, Orleans CT, Mulrow CD, et al. Screening for depression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;136(10):765–76. doi: 10.7326/0003-4819-136-10-200205210-00013. [DOI] [PubMed] [Google Scholar]
- 46.Williams JW., Jr M. Pignone, G. Ramirez, and C. Perez Stellato, Identifying depression in primary care: a literature synthesis of case-finding instruments. Gen Hosp Psychiatry. 2002;24(4):225–37. doi: 10.1016/S0163-8343(02)00195-0. [DOI] [PubMed] [Google Scholar]
- 47.Monahan PO, Shacham E, Reece M, Kroenke K, Ong WO. Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in Western Kenya. J Gen Intern Med. 2009;24(2):189–197. doi: 10.1007/s11606-008-0846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21(6):547–52. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martin A, Rief W, Klaiberg A, Braehler E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen Hosp Psychiatr. 2006;28(1):71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 50.Becker S, Zaid KA, Faris EA. Screening for somatization and depression in Saudi Arabia: A validation study of the PHQ in primary care. Int J Psychiatr Med. 2002;32(3):271–283. doi: 10.2190/XTDD-8L18-P9E0-JYRV. [DOI] [PubMed] [Google Scholar]
- 51.Wulsin L, Somoza E, Heck J. The Feasibility of Using the Spanish PHQ-9 to Screen for Depression in Primary Care in Honduras. Primary care companion to the Journal of clinical psychiatry. 2002;4(5):191–195. doi: 10.4088/PCC.v04n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Omoro S, Fann J, Weymuller E, Macharia I, Yueh B. Swahili translation and validation of the Patient Health Questionnaire-9 depression scale in the Kenyan head and neck cancer patient population. Int J Psychiatr Med. 2006;36(3):367–381. doi: 10.2190/8W7Y-0TPM-JVGV-QW6M. [DOI] [PubMed] [Google Scholar]
- 53.Adewuya AO, Ola BA, Afolabi OO. Validity of the patient health questionnaire (PHQ-9) as a screening tool for depression amongst Nigerian university students. J Affect Disord. 2006;96(1–2):89–93. doi: 10.1016/j.jad.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 54.Okulate G, Olayinka M, Jones O. Somatic symptoms in depression: Evaluation of their diagnostic weight in an African setting. Br J Psychiatr. 2004;184(5):422–427. doi: 10.1192/bjp.184.5.422. [DOI] [PubMed] [Google Scholar]
- 55.Crane P, Gibbons L, Willig J, Mugavero M, Lawrence S, Schumacher J, et al. Measuring depression levels in HIV-infected patients as part of routine clinical care using the nine-item Patient Health Questionnaire (PHQ-9) AIDS Care. 2010;22(7):874–885. doi: 10.1080/09540120903483034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Justice, A.C., K.A. McGinnis, J. Atkinson, R.K. Heaton, C. Young, J. Sadek, et al.Psychiatric and neurocognitive disorders among HIV-positive and negative veterans in care: Veterans Aging Cohort Five-Site Study. AIDS, 2004. 18 (Suppl1): p. S49-S59. [PubMed]
- 57.Malekinejad M, Johnston LG, Kendall C, Kerr LR, Rifkin MR, Rutherford GW. Using respondent-driven sampling methodology for HIV biological and behavioral surveillance in international settings: a systematic review. AIDS Behav. 2008;12(4 Suppl):S105–30. doi: 10.1007/s10461-008-9421-1. [DOI] [PubMed] [Google Scholar]
- 58.Testa MA, Nackley JF. Methods for quality-of-life studies. Annu Rev Public Health. 1994;15:535–59. doi: 10.1146/annurev.pu.15.050194.002535. [DOI] [PubMed] [Google Scholar]
- 59.Marc LG, Wang MM, Testa MA.Psychometric evaluation of the HIV symptom distress scale. AIDS Care. 2012;24(11):1432–1441. [DOI] [PMC free article] [PubMed]
- 60.DeVellis, R.F.Scale development : theory and applications. 2nd ed. Applied social research methods series; v. 262003, Thousand Oaks, Calif.: SAGE Publications. viii, 171.
- 61.StataCorp LP.Stata user's guide. Release 122011, College Station, Tex.: StataCorp LP. x, 389 p.
- 62.Microsoft Corporation.Microsoft Excel [computer program] 2010: Microsoft Corp. xvi, 344.
- 63.Streiner, D.L. and G.R. Norman.Health measurement scales : a practical guide to their development. Oxford medical publications1989, Oxford; New York: Oxford University Press. vii, 175 p.
- 64.Nunnally, J.C.Psychometric theory. 2nd ed1978, New York: McGraw-Hill. xv, 701 p.
- 65.Coste J, Bouee S, Ecosse E, Leplege A, Pouchot J. Methodological issues in determining the dimensionality of composite health measures using principal component analysis: case illustration and suggestions for practice. Quality of Life Research. 2005;14(3):641–54. doi: 10.1007/s11136-004-1260-6. [DOI] [PubMed] [Google Scholar]
- 66.Zwick WR, Velicer WF. Comparison of five rules for determining the number of components to retain. Psychol Bull. 1986;99(3):432–442. doi: 10.1037/0033-2909.99.3.432. [DOI] [Google Scholar]
- 67.Howard KI, Forehand GA. A method for correcting item-total correlations for the effect of relevant item inclusion. Educ Psychol Meas. 1962;22(4):731–735. doi: 10.1177/001316446202200407. [DOI] [Google Scholar]
- 68.Cole SR. Assessment of differential item functioning in the Perceived Stress Scale-10. J Epidemiol Community Health. 1999;53(5):319–20. doi: 10.1136/jech.53.5.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cole SR, Kawachi I, Maller SJ, Berkman LF. Test of item-response bias in the CES-D scale. experience from the New Haven EPESE study. J Clin Epidemiol. 2000;53(3):285–9. doi: 10.1016/S0895-4356(99)00151-1. [DOI] [PubMed] [Google Scholar]
- 70.Marc LG, Raue PJ, Bruce ML. Screening performance of the 15-item geriatric depression scale in a diverse elderly home care population. Am J Geriatr Psychiatry. 2008;16(11):914–21. doi: 10.1097/JGP.0b013e318186bd67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Williams DR, Haile R, Gonzalez HM, Neighbors H, Baser R, Jackson JS. The mental health of Black Caribbean immigrants: results from the National Survey of American Life. Am J Public Health. 2007;97(1):52–9. doi: 10.2105/AJPH.2006.088211. [DOI] [PMC free article] [PubMed] [Google Scholar]