ABSTRACT
OBJECTIVES
We conducted a review of the peer-reviewed literature since 2003 to catalogue reported methods of stakeholder engagement in comparative effectiveness research and patient-centered outcomes research.
METHODS AND RESULTS
We worked with stakeholders before, during and after the review was conducted to: define the primary and key research questions; conduct the literature search; screen titles, abstracts and articles; abstract data from the articles; and analyze the data. The literature search yielded 2,062 abstracts. The review was conducted on 70 articles that reported on stakeholder engagement in individual research projects or programs.
FINDINGS
Reports of stakeholder engagement are highly variable in content and quality. We found frequent engagement with patients, modestly frequent engagement with clinicians, and infrequent engagement with stakeholders in other key decision-making groups across the healthcare system. Stakeholder engagement was more common in earlier (prioritization) than in later (implementation and dissemination) stages of research. The roles and activities of stakeholders were highly variable across research and program reports.
RECOMMENDATIONS
To improve on the quality and content of reporting, we developed a 7-Item Stakeholder Engagement Reporting Questionnaire. We recommend three directions for future research: 1) descriptive research on stakeholder-engagement in research; 2) evaluative research on the impact of stakeholder engagement on the relevance, transparency and adoption of research; and 3) development and validation of tools that can be used to support stakeholder engagement in future work.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-2878-x) contains supplementary material, which is available to authorized users.
KEY WORDS: stakeholders, research, review
BACKGROUND
Better stakeholder engagement has been proposed to help realign healthcare research with the needs of clinicians, patients, policymakers, and payers. Advocates for comparative effectiveness research (CER) and patient-centered outcomes research (PCOR) have been especially strong proponents of this recommendation, on the basis that stakeholder engagement may improve the relevance of research questions, increase the transparency of research activities, and accelerate the adoption of evidence into practice.1–6 These entreaties could result in a new era of stakeholder-engaged research, and could lead to an important benchmark for patient-centered research: that it “is useful to clinicians and patients—and is used.”7
Because little is known about the methods that have been used for engaging stakeholders in the research process, we undertook a systematic review of the peer-reviewed literature to catalogue reported methods of engagement. In prior work,8 we defined stakeholder as an individual or group who is responsible for or affected by health-and healthcare-related decisions that can be informed by research evidence. We defined engagement as a bi-directional relationship between stakeholder and researcher that results in informed decision-making about the prioritization, conduct and use of research. We based our work on the 7Ps Framework for Stakeholder Engagement8 and the Six Stages Model for CER and PCOR. The 7Ps Framework, developed through use of a deductive-inductive method,10 suggests that stakeholders may be organized into seven types: patients and the public, providers, purchasers, payers, policy makers, product makers, and principal investigators. The Six Stages Model, developed by researchers affiliated with the Tufts Clinical and Translational Science Institute (CTSI), suggests that CER and PCOR may be organized conceptually into six types: evidence prioritization (identification of research priorities), evidence generation (trials and observational studies), evidence synthesis (systematic reviews and meta-analyses), evidence integration (simulation modeling, cost effectiveness analyses and other methods to address gaps left by trials, observational studies, meta-analyses and systematic reviews), evidence dissemination and application (dissemination and implementation research, and feedback and assessment (evaluation of the research program).
The 7Ps Framework and six Stages Model provided a structure by which we were able to review stakeholder engagement that was reported in the past 10 years of CER and PCOR.
METHODS
We used a five-step process to conduct the systematic review: definition of key questions; literature search; title, abstract and full text screening; data abstraction; and analysis. As described further below, we engaged stakeholders (Table 1) during each step.
Table 1.
Stakeholders Participating in this Review
| Category Subcategory |
Name | Affiliation |
|---|---|---|
| Patients and the public | ||
| Consumer | Grant P. Thompson | Consumer reports health ratings center |
| Consumer | Gerald Rasmussen | Consumer reports health ratings center |
| Providers | ||
| Provider organization | Judy Bradford | Fenway Institute/Fenway health |
| Payers and purchasers | ||
| Self-insured employer | Lawrence Becker | Xerox corporation |
| Policy Makers | ||
| Federal | JoAnne Grunbaum | Centers for disease control & prevention |
| Product makers | ||
| Pharmaceutical | Eleanor Perfetto | Pfizer, Inc. |
| Principal investigators | ||
| Health services | Julie Lynch | University of Massachusetts, Boston |
| Clinical | Radley (Chris) Sheldrick | Tufts Medical Center |
This table presents the 7P Framework category, a subcategory, name, and affiliation of stakeholders who participated in this systematic review. Stakeholders are also mentioned in the acknowledgements
Definition of Key Questions
Our primary question was: how have U.S. researchers reported engagement with stakeholders in the prioritization, conduct and use of comparative effectiveness and patient-centered outcomes research since 2003? Aside from this primary question, we set forth seven key questions for exploration (Text Box 1). In addition to these a priori research questions, we present findings about the impact of stakeholder engagement on research outcomes.
Text Box 1. Research Question and Key Questions
| Research Question How have U.S. researchers reported engagement with stakeholders in the prioritization, conduct and use of comparative effectiveness and patient-centered outcomes research since 2003? Key Questions 1. With which types of stakeholders have researchers reported engagement? 2. In what stages of research have researchers reported engagement with stakeholders? 3. How have researchers reported engagement with stakeholders? 4. What level of engagement have researchers used? 5. What modes of engagement have researchers reported? 6. What mechanisms of engagement have researchers reported? |
| 7. Was a special provision reported for the engagement of patients? |
This table presents the 7P Framework category, a subcategory, name, and affiliation of stakeholders who participated in this systematic review. Stakeholders are also mentioned in the acknowledgements
Literature Search
We searched peer-reviewed published literature that described stakeholder engagement in PCOR and CER since 2003, the year that the Medicare Prescription Drug Improvement and Modernization Act established the Effective Healthcare Program as part of the Agency for Healthcare Research and Quality. We first searched MEDLINE and Cochrane Central Trials Registry databases from 2003 to May 2012 for English-language studies that reported on stakeholder engagement in the prioritization, conduct or use of PCOR and CER. In addition, we searched the Cochrane Database of Systematic Reviews to identify relevant reviews on the topic. In this stage, we sought to capture publications that: 1) reported on health-related research and programs in any of the six stages of CER and PCOR; (2) reported engagement with stakeholders; and 3) were described as comparative or patient-centered. A wide scope of keywords and MESH terms was used. A preliminary search conducted in November of 2011 yielded several hundred abstracts that were used to inform the search strategy. Terms from these abstracts were added to the final search, followed by consultation with experts in automated search strategies, and with stakeholders who have expertise in making healthcare decisions. The final search strategy included 76 terms (Online Appendix A).
Title, Abstract, and Full Text Screening
Following the search, we conducted a preliminary screen of article titles and abstracts, using double review by trained readers and adjudication of disagreements by the principal investigator. Explicit inclusion and exclusion criteria were developed prior to screening. To be included and advanced to full text screening, abstracts had to indicate that stakeholders were engaged in any one (or more) of the Six Stages of Research (prioritization, generation, synthesis, integration, dissemination & implementation, feedback & assessment) as investigators, staff, partners or consultants. Publications were also considered to be stakeholder-engaged if they reported collaboration with site-based staff who were practitioners in healthcare delivery, payment or policy organizations. Stakeholders had to plausibly belong to one of seven groups of individuals and organizations with an interest in the outcomes of research (patients and the public, providers, purchasers, payers, policy makers, product makers, and other principal investigators).9 Abstracts were excluded and did not proceed to full text screening if stakeholders and related terms were not mentioned, if the abstract was a report of planned research (we sought reports of completed research and programs), or if stakeholders were engaged as subjects of research only.
Full text screening involved a repetition of this process on the full text of the article. Our unit of analysis was the published research report. Thus, surveys of patients or clinicians as subjects of research, but not as fully-fledged stakeholders, did not qualify on their own for inclusion, and we did not try to infer if a survey led to further engagement with its respondents as stakeholders after the report was published. However, if a report described both a survey and use of respondents to inform priorities or conduct further research, it qualified for full text review.
Data Extraction
Data were extracted from full text articles into an electronic questionnaire and database built specifically for this project. Staff members conducting extractions used the electronic questionnaire (Online Appendix B) to populate an excel spreadsheet on which later analyses could be run. The electronic questionnaire and linked database were developed by the full team and used carefully crafted non-skip rules for required responses, skip patterns to follow question logic, drop down response options for uniform data gathering, free text fields to supplement uniform data gathering, and documentation to track progress on the reviews. The research question and seven key questions described in Table 1 formed the major sections of the electronic survey instrument and provide a framework for reporting our results. Randomly selected articles were re-reviewed by team members to check for accuracy. Free text fields were coded and reported after all extractions were completed.
Analysis
We adhered as closely as possible to address recommendations in the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA).9,10 Because our synthesis focused on what authors have reported about stakeholder engagement, no syntheses of any outcome measure were included in our analysis. This meant that formal tests of risk of bias in individual studies or across studies were not needed. Most data are reported categorically as a number or percent of publications.
Stakeholder Engagement
We engaged with stakeholders to assist in the design, conduct, and interpretation of our review (Table 1). During our planning stages, we engaged with two patients and one stakeholder from five of the remaining six categories described in the 7Ps framework. For this review, we combined payers and purchasers into a single category, since their standpoints on engagement in research are similar. The target numbers we identified for each stakeholder type assured that our panel was over-weighted with patients and was not dominated by individuals or organizations with a commercial interest, income, or organizational conflict of interest resulting from the sale of healthcare interventions or products. Stakeholders were identified through personal and professional networks prior to conducting the evidence synthesis, and all shared an interest in stakeholder engagement in research. All invited individuals agreed to participate.
We held two stakeholder meetings: the first to articulate relevant research and key questions and adapt the study design; the second to review preliminary results in the analysis. With respect to the study design, seven stakeholders and experts in the conduct of systematic review from Tufts Medical Center suggested data elements for inclusion in the electronic extraction form. Stakeholders also helped us identify effective ways to communicate the findings in tables and figures for this manuscript. All stakeholders were invited to participate by email and phone throughout the research, including a review of the manuscript. Stakeholders have been asked to assist in dissemination of the results. We did not conduct any formal evaluation of the impact of stakeholder engagement during the course of the review, but have included this project in a slate of stakeholder-engaged research that will be evaluated and whose results will be presented elsewhere.
RESULTS
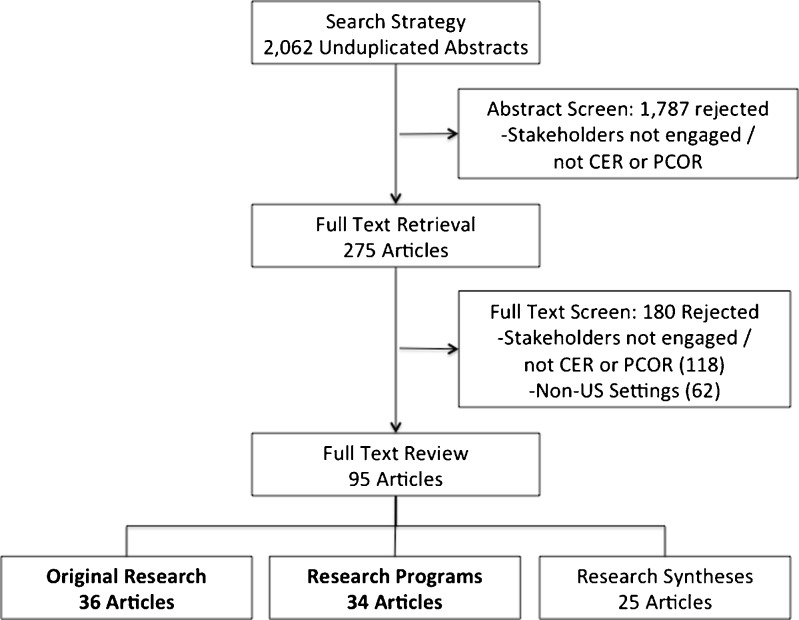
The search yielded 2,062 abstracts for initial screening. Abstract screening yielded 275 articles for full text screening. Full text screening yielded 157 articles, and of those, 62 reported on research or programs in non-U.S. settings and 95 reported on research or programs in U.S. settings. We further classified the 95 articles into reports of research (n = 36), reports on programs (n = 34), and syntheses of stakeholder engagement (n = 25). For the purposes of this project, reports of research describe and address a health question for which the answer is not already known, and reports of programs describe the implementation of a health-related intervention without addressing a related health question. A PRISMA diagram11,12 is depicted in Fig. 1. This review presents descriptive data on the reports of research projects or programs (n = 70) (Table 2),13–82 since it was not possible to extract from syntheses of multiple stakeholder engagement projects any detailed information on the individual projects.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) diagram. This diagram presents the number abstracts (n = 2,062) and articles (n = 275) retrieved for screening, the number of articles reporting on research or programs in U.S. settings (n = 95), and the number of articles included in the review (n = 70).
Table 2.
Article Characteristics
| n | % | |
|---|---|---|
| Article setting (n = 157) | ||
| U.S. | 95 | 61 |
| Non-U.S. | 62 | 39 |
| Type of article (U.S. only, n = 95) | ||
| Research | 36 | 38 |
| Programmatic | 34 | 36 |
| Synthesis of research | 25 | 26 |
| Selected characteristics (Research only, n = 36) | ||
| Research stage | ||
| Evidence prioritization | 6 | 17 |
| Evidence generation | 26 | 72 |
| Evidence synthesis | 0 | 0 |
| Evidence interpretation and integration | 0 | 0 |
| Dissemination and Application | 3 | 8 |
| Feedback and Assessment | 1 | 3 |
| Type of methodology used | ||
| Qualitative | 11 | 31 |
| Quantitative | 4 | 11 |
| Mixed methods | 14 | 39 |
| ND* | 7 | 19 |
| Study setting | ||
| Community | 28 | 78 |
| Health care setting | 6 | 17 |
| NA* | 2 | 6 |
| Unit of analysis | ||
| Current patients | 7 | 19 |
| Population (Public health), including community individuals | 19 | 53 |
| Providers and provider organizations (hospitals, health centers…) | 5 | 14 |
| Other** | 5 | 14 |
This table presents characteristics of 157 U.S. and non-U.S. research articles, program reports, and syntheses of research and programs that were included in the full text review. *NA and ND responses include articles in Stages 1 and 6, where a formal research may have not been presented. **Other includes miscellaneous responses, such as members of a collaborative, geographic/administrative boundaries, etc.
Of the 70 articles included in this review, topics included health behaviors (diet, sexual health), mental health, disparities, violence prevention, chronic diseases, health insurance enrollment, and others. Articles addressed the needs of current patients (commonly patients with HIV, diabetes, or depression), minority populations (including African Americans, Hispanics, Native Americans, and Asians) and service providers (commonly clinicians or nurses).
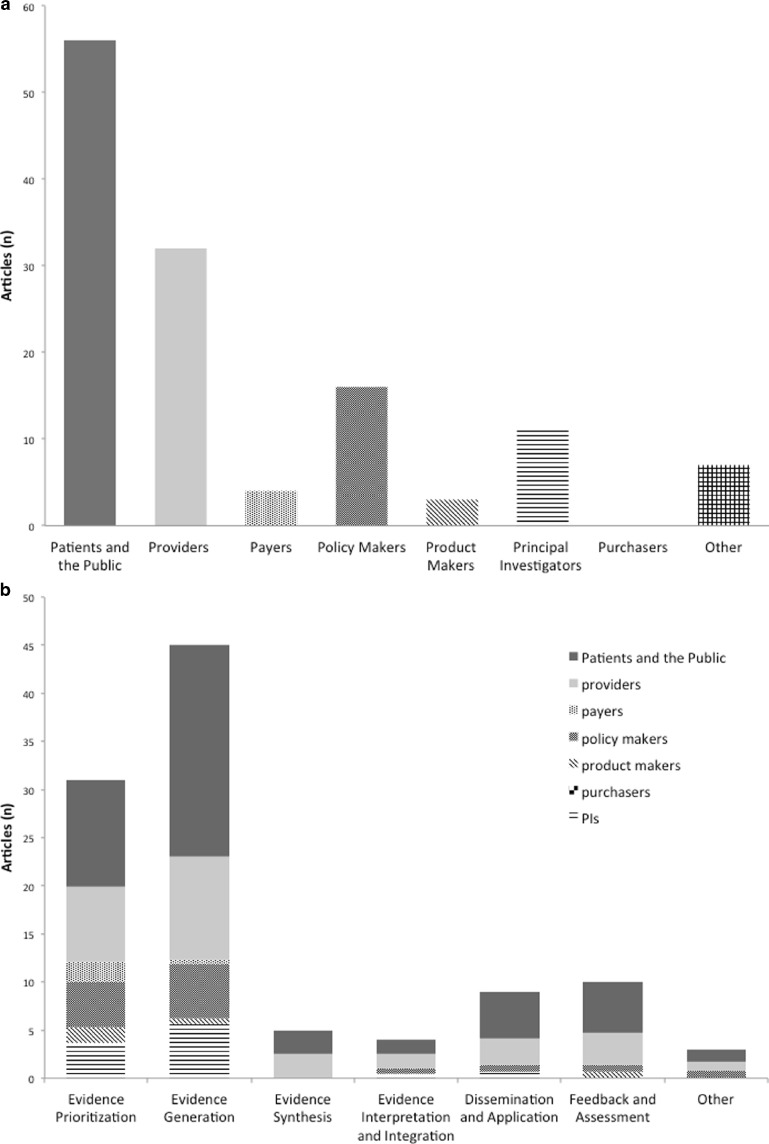
Stakeholder Categories
Of the seven stakeholder categories in the 7Ps Framework, patients and the public were most frequently engaged in peer reviewed research and program reports (Fig. 2a). Eighty percent of articles (n = 56) reported engagement with this group. Providers were the next most frequently cited group (n = 32); policy makers (n = 16) and principal investigators (n = 11) were next. Payers (n = 6), product makers (n = 4), and purchasers (n = 0) were rarely or never mentioned. Only 9 % of research and program reports described strategies to balance views of stakeholders with competing viewpoints. Stakeholders were typically recruited through personal and professional networks (61 %). About a quarter of the articles did not report on the method of recruitment, and there were no articles reporting use of sampling methods to recruit stakeholders from a specific population.
Figure 2.
Who are the stakeholders and in what stages of research are they engaged? Panel A presents the frequencies of articles mentioning engagement with each of the seven stakeholder categories in the 7Ps Framework. Because articles might report engagement with multiple stakeholder groups, the denominator for each bar in this histogram equals 70. In Panel B, the share of each bar presenting engagement with a stakeholder group represents the probability of engagement with that group within the stage of research. Because an article could span multiple stages of research, the total reports of engagement in the six research stages equals more than 70 (n = 107).
Stage of Research
Stakeholder engagement was more common in earlier than in later stages of research (Fig. 2b). The first two stages in the Tufts CTSI six-stage model of CER, the prioritization (n = 31) and generation (n = 45) of evidence, were by far the most common type of research or program activity for which stakeholder engagement was reported. Engagement was less common in the process of dissemination and application of evidence (n = 9) and in evaluating research activities (n = 10), and it was rare in research projects that involved the synthesis, integration, or interpretation of evidence.
Much of the engagement occurred before the research or program was underway, either by helping to define a research question (34 %) or by defining some key aspect of the population, intervention(s), or comparators (44 %). Engagement to monitor and oversee a project after it was up and running was also fairly common (36 %). Slightly less frequent were engagement activities that involved interpreting, disseminating and applying the results of a project (9–10 %), echoing the relative lack of engagement in research projects that focused on these activities.
Methods and Modes of Engagement
The activities of stakeholders were highly variable across research and program reports. Approximately half of the articles reported engaging with stakeholders as consultants to their projects, while one-third reported engagement at the level of co-principal investigator and one-third reported engaging stakeholders as staff on the project (more than one response per project was possible). One in five reports indicated that stakeholders were engaged as the subjects of the research or program. Stakeholders were engaged through surveys and key informant interviews about 15–20 % of the time and in focus groups and panels 20–30 % of the time.
Analysis and Impact of Stakeholder Engagement
Nearly half (44 %) of the articles did not report how the views of stakeholders were synthesized and used in the project. About one-quarter (26 %) reported qualitative synthesis of written notes or transcripts and more than one-third (36 %) reported that stakeholders and investigators engaged with each other in joint-decision making.
Although it was not possible to validate claims of the benefits and challenges related to stakeholder engagement, several common themes were reported. About one in five articles reported that stakeholder engagement improved the relevance of research, increased stakeholder trust in research and researchers, enhanced mutual learning by stakeholders and researchers about each other, or improved research adoption. A smaller number reported that engagement improved the transparency of research (6 %) and increased understanding of the research process (9 %). The most common challenge reported was that stakeholder engagement is time consuming (19 %). Other challenges were reported by between 3 and 6 % of articles, including that stakeholder engagement requires researcher flexibility, trust among researchers and stakeholders, commitment from both the researchers and stakeholders to maintain contact and participation, difficulty establishing stakeholder representativeness throughout the course of the research program, increased ethical concerns in some institutional review boards (IRB), stakeholder distress while participating (particularly with patients and family members), and difficulty overcoming cultural differences between stakeholders and researchers.
DISCUSSION
Reports on CER and PCOR are highly variable in the types of stakeholders who are engaged. We found frequent engagement with patients, modestly frequent engagement with clinicians, and infrequent engagement with stakeholders representing other key decision-makers across the healthcare system. The frequency of engagement with patients is encouraging, as it reflects a growing opinion that this ultimate decision-maker is the most salient stakeholder in research. This view was emphasized by the stakeholder panel, is reflected in the call for patient-centered medicine in initiatives across the Federal government,83–87 and is explicitly emphasized in guidance on Patient-Centered Outcomes Research Institute (PCORI)-funded research.88,89
The relatively modest frequency of engagement with clinicians and infrequency of engagement with payers, purchasers, policy-makers, product-makers and other principal investigators is discouraging. These groups, though not salient for every research project or program evaluation, represent a broad range of critical decision-makers in the healthcare system. Many high profile cases have demonstrated that ignoring these groups during research activities can lead to unwarranted challenges: the research can result in policy and other decisions that are ill-fitted to the interests, opinions, and needs of these groups, and can result in fierce opposition that derails well-intentioned decision-making. One of the best known of such cases recently was the U.S. Preventive Services Task Force (USPSTF) guideline on mammography screening, in which patients, patient advocates, radiologists, oncologists, and others lined up to oppose the guideline after it was issued for public comment.88 Inclusion of clinicians and other stakeholders has been embraced by PCORI,89,90 and has been identified as a priority for dissemination and implementation of CER and PCOR findings.91
The inclusion of a broad range of stakeholders in research is not without its challenges. These may range from logistical (e.g., scheduling and funding) to process-oriented (e.g., balancing competing interests, addressing implicit power differentials, and managing conflict). Indeed, the main reported barriers to engaging stakeholders in CER and PCOR were time and the need for logistical support and funding flexibility. We did not, however, see reports of difficulties in managing the decision-making process. Stakeholders may have conflicts with each other and perceived or direct conflicts of interest, but well-developed mechanisms for managing these conflicts exist, including public disclosure, non-voting participation, and recusal. Where conflicts of interest cannot be managed, intentional exclusion may be the right choice, but this decision should be made explicitly and transparently before the research begins.
We also saw variable reporting on engagement by stage of research. Engagement is most common during evidence prioritization and generation, and is infrequent or rare in latter stages: synthesis, integration, dissemination and evaluation. The infrequency of engagement in these latter stages could reflect just an omission in reporting, but we suspect it reflects actual lack of engagement. In order to maintain bi-directional relationships between researchers and stakeholders, we believe that uninterrupted engagement over the lifecycle of research is necessary. To accomplish full and uninterrupted engagement, researchers and stakeholders may need to invest time and resources for training and support. Furthermore, one potential benefit of engagement during methodologically challenging stages of synthesis and integration would be to improve the transparency of research activities. If stakeholders understand and can articulate how findings were established, they are far more likely to become effective ambassadors during dissemination and implementation efforts.
To improve on the quality and content of reporting, we developed a 7-Item questionnaire for reporting on stakeholder engagement in research (Text Box 2). The questionnaire includes items on the types of stakeholders engaged, whether target numbers were established for each type of stakeholder before recruitment began, how a balance of stakeholder perspectives was considered and achieved, and the methods used to identify, recruit and enroll stakeholders in engagement activities. We also recommend reporting on whether engagement occurred: 1) before research, in priority setting, topic development, question development, and research design; 2) during research, including enrollment of patients, conduct of data collection, analysis, and interpretation of findings; and 3) after research, including dissemination and implementation of findings, and evaluation of the research itself. Finally, we suggest reporting on the modes and methods of engagement, and we recommend an assessment of the impact of engagement on the relevance, transparency, and adoption of research.
Text Box 2. A 7-Item Questionnaire for Reporting on Stakeholder Engagement in Research
| 1. What types of stakeholders were engaged? 2. What were the a priori target number(s) for each type of stakeholder? Were targets met? 3. How was balance of stakeholder perspectives considered and achieved? 4. What methods were used to identify, recruit and enroll stakeholders in research activities? 5. Did engagement occur: a. before research began, during priority setting, topic development, question development, and research design; b. during research activities, including enrollment of patients, conduct of data collection, analysis, and interpretation of findings; and c. after research was concluded, including dissemination and implementation of findings, and evaluation of the research itself? 6. What were the intensity, methods and modes of engagement? |
| 7. What, if any, was the impact of stakeholder engagement on: a. the relevance of research questions; b. the transparency of the research process; and c. the adoption of research evidence into practice settings? |
This figure presents a list of questions that may be used by researchers to guide future reporting on stakeholder-engaged research. These questions were co-developed with a stakeholder panel
We recommend three directions for future research: 1) descriptive research on stakeholder-engagement in research; 2) evaluative research on the impact of stakeholder engagement on the relevance, transparency and adoption of research; and 3) development and validation of tools that can be used to support stakeholder engagement in future work. First, future research is needed to describe the nature and extent of stakeholder engagement. For example, to understand in more detail how extensively stakeholders have been engaged in clinical trial research or evidence syntheses, a review team might draw a random sample of peer reviewed articles from a limited set of top-ranked journals within a limited time frame, and contact corresponding author(s) for structured interviews aimed at learning whether, to what extent and how stakeholders were engaged in the project. Second, future lines of inquiry could evaluate the benefits of different approaches for engaging stakeholders with respect to the relevance of research questions, transparency of research activities, and adoption of evidence into practice. Third, future research should be organized to develop training materials, methods and tools for advancing stakeholder engagement in healthcare research. Hands-on training opportunities and user-friendly tools and methods for stakeholder identification and recruitment, engagement, and evaluation are needed to help investigators embrace stakeholder engagement in their research projects. Prior work in the field of Community-Based Participatory research (CBPR) has addressed some of these needs.92
This review of stakeholder engagement faced a key limitation. First, though our search strategy cast a wide net by deploying a comprehensive set of terms in multiple databases, we recognize that many research programs and projects may engage with stakeholders without reporting on engagement in the published article. This limitation, however, also underscores the primary finding: that reporting on stakeholder engagement activities is highly variable in quality and content.
In summary, we found substantial variation in the quality and content of reporting about stakeholder engagement in research. To address some of these shortfalls, we developed a 7-item questionnaire for reporting on stakeholder engagement in research (Text Box 2). Finally, we recommend new descriptive research on stakeholder engagement; new evaluation studies to establish whether engagement influences the relevance, transparency and adoption of research; and new training, method and tool development to support best practices in future stakeholder-engaged research activities.
Electronic Supplementary Material
(PDF 61 kb)
(PDF 118 kb)
Acknowledgements
Contributors
Ushahsi Basu, Ridita Nizam, and Madeleine Streit screened abstracts, retrieved and reviewed full text articles, and recorded data on the articles that were included in the review. Samuel Hirshman and Shawna Beck-Sullivan assisted in preparation of the manuscript.
The authors also wish to thank Grant P. Thompson and Gerald Rasmussen of the Consumer Reports Panel, Judith Bradford of Fenway Institute & Fenway Health, Lawrence Becker of Xerox, JoAnne Grunbaum of the Centers for Disease Control & Prevention, Eleanor Perfetto of Pfizer Inc., Julie Lynch of the University of Massachusetts-Boston, and Radley (Chris) Sheldrick of Tufts Medical Center, who participated as stakeholders on this research project. Further information on these individuals and their roles on the project is presented in the Methods section and in Table 1.
Funders
The authors were support by grants from the Agency for Healthcare Research and Quality (AHRQ) (K01 HS017726 and HHSA 290 2007 10055 I) and the National Center for Advancing Translational Science (NCATS), NIH (UL1 RR025752).
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Agency for Healthcare Research and Quality or the National Institutes of Health.
Prior Presentations
The data presented in this article have not been presented at any conference or in any other peer reviewed publication.
Conflict of Interest
The authors have no competing interests that bear on the content of this manuscript.
Author Contributions
Dr. Concannon took primary responsibility for conceiving and writing the manuscript, obtaining contributions from co-authors and managing stakeholder reviews and government clearances. All co-authors made intellectual contributions during the research design and analysis stages.
REFERENCES
- 1.Institute of Medicine . Initial Priorities for Comparative Effectiveness Research. Washington: National Academies Press; 2009. [Google Scholar]
- 2.Federal Coordinating Council for Comparative Effectiveness Research . Report to the President and Congress. Washington: US Department of Health and Human Services; 2009. [Google Scholar]
- 3.Sox HC, Greenfield S. Comparative effectiveness research: a report from the institute of medicine. Ann Intern Med. 2009;151:203–205. doi: 10.7326/0003-4819-151-3-200908040-00125. [DOI] [PubMed] [Google Scholar]
- 4.Patient Centered Outcomes Research Institute. http://www.pcori.org. Accessed March 21, 2014.
- 5.McClellan M, Benner J, Garber AM, Meltzer DO, Tunis SR, Pearson S. Comparative Effectiveness Research: Will it bend the Health Care Cost Curve and Improve Quality? The Brookings Institute: Washington; 2009. [Google Scholar]
- 6.Roehr B. More stakeholder engagement is needed to improve quality of research, say US experts. BMJ. 2010;341:c4193. doi: 10.1136/bmj.c4193. [DOI] [Google Scholar]
- 7.Conway PH, Clancy C. Charting a path from comparative effectiveness funding to improved patient-centered health care. JAMA. 2010;303:985–6. doi: 10.1001/jama.2010.259. [DOI] [PubMed] [Google Scholar]
- 8.Concannon TW, Meissner P, Grunbaum JA, McElwee N, Guise JM, Santa J, Conway PH, Daudelin D, Morrato EH, Leslie LK. A new taxonomy for stakeholder engagement in patient centered outcomes research. J Gen Intern Med. 2012;27:985–991. doi: 10.1007/s11606-012-2037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Selker HP, Leslie LK, Wasser JS, Plaut AG, Wilson IB, Griffith JL, Tufts CTSI. Tufts CTSI. Clin Transl Sci. 2010;3:56–8. doi: 10.1111/j.1752-8062.2010.00184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;424:1758–72. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA group preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA). http://www.prisma-statement.org. Accessed March 21, 2014.
- 13.Amico KL, Wieland ML, Weis JA, Sullivan SM, Nigon JA, Sia IG. Capacity building through focus group training in community-based participatory research. Educ Health (Abingdon) 2011;24:638. [PMC free article] [PubMed] [Google Scholar]
- 14.Ammerman A, Corbie-Smith G, St George DM, Washington C, Weathers B, Jackson-Christian B. Research expectations among African American church leaders in the PRAISE! project: a randomized trial guided by community-based participatory research. Am J Publ Health. 2003;93:1720–1727. doi: 10.2105/AJPH.93.10.1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amtmann D, Cook KF, Johnson KL, Cella D. The PROMIS initiative: involvement of rehabilitation stakeholders in development and examples of applications in rehabilitation research. Arch Phys Med Rehabil. 2011;92:S12–19. doi: 10.1016/j.apmr.2011.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Angstman KB, Bender RO, Bruce SM. Patient advisory groups in practice improvement: sample case presentation with a discussion of best practices. J Amb Care Mgmt. 2009;32:328–332. doi: 10.1097/JAC.0b013e3181ba6e90. [DOI] [PubMed] [Google Scholar]
- 17.Austin SA, Claiborne N. Faith wellness collaboration: a community-based approach to address type II diabetes disparities in an African-American community. Soc Work Health Care. 2011;50:360–375. doi: 10.1080/00981389.2011.567128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boutain DM. Collective knowledge sharing as a social justice strategy: the difference it made in a service project about preterm birth disparity. ANS Adv Nurs Sci. 2009;32:E68–80. doi: 10.1097/ANS.0b013e3181a3b54e. [DOI] [PubMed] [Google Scholar]
- 19.Boyer BB, Mohatt GV, Pasker RL, Drew EM, McGlone KK. Sharing results from complex disease genetics studies: a community based participatory research approach. Int J Circumpolar Health. 2007;66:19–30. doi: 10.3402/ijch.v66i1.18221. [DOI] [PubMed] [Google Scholar]
- 20.Breslin M, Mullan RJ, Montori VM. The design of a decision aid about diabetes medications for use during the consultation with patients with type 2 diabetes. Pat Educ Couns. 2008;73:465–472. doi: 10.1016/j.pec.2008.07.024. [DOI] [PubMed] [Google Scholar]
- 21.Buckler AJ, Bresolin L, Dunnick NR, Sullivan DC. A collaborative enterprise for multi-stakeholder participation in the advancement of quantitative imaging. Radiology. 2011;258:906–914. doi: 10.1148/radiol.10100799. [DOI] [PubMed] [Google Scholar]
- 22.Chang DI, Burton A, O’Brien J, Hurley RE. Honesty as good policy: evaluating Maryland’s medicaid managed care program. Milbank. 2003;81:389–414. doi: 10.1111/1468-0009.t01-1-00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chung B, Corbett CE, Boulet B, et al. Talking wellness: a description of a community-academic partnered project to engage an African-American community around depression through the use of poetry, film, and photography. Ethn Dis. 2006;16:S67–78. [PubMed] [Google Scholar]
- 24.Chung B, Jones L, Dixon EL, Miranda J, Wells K. Using a community partnered participatory research approach to implement a randomized controlled trial: planning community partners in care. J Health Care Poor Underserved. 2010;21:780–795. doi: 10.1353/hpu.0.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cooley WC, McAllister JW, Sherrieb K, Clark RE. The Medical Home Index: development and validation of a new practice-level measure of implementation of the Medical Home model. Ambul Pediatr. 2003;3:173–180. doi: 10.1367/1539-4409(2003)003<0173:TMHIDA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Corona R, Gonzalez T, Cohen R, Edwards C, Edmonds T. Richmond Latino needs assessment: a community-university partnership to identify health concerns and service needs for Latino youth. J Commun Health. 2009;34:195–201. doi: 10.1007/s10900-008-9140-6. [DOI] [PubMed] [Google Scholar]
- 27.Crowe JL, Keifer MC, Salazar MK. Striving to provide opportunities for farm worker community participation in research. J Agric Saf Health. 2008;14:205–219. doi: 10.13031/2013.24351. [DOI] [PubMed] [Google Scholar]
- 28.Curran GM, Pyne J, Fortney JC, et al. Development and implementation of collaborative care for depression in HIV clinics. AIDS Care. 2011;23:1626–1636. doi: 10.1080/09540121.2011.579943. [DOI] [PubMed] [Google Scholar]
- 29.Davis RM, Hitch AD, Nichols M, Rizvi A, Salaam M, Mayer-Davis EJ. A collaborative approach to the recruitment and retention of minority patients with diabetes in rural community health centers. Contemp Clin Trials. 2009;30:63–70. doi: 10.1016/j.cct.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 30.Egede LE, Ellis C. Development and testing of the multidimensional trust in health care systems scale. J Gen Intern Med. 2008;23:808–815. doi: 10.1007/s11606-008-0613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fredericks JE, Bunting RF., Jr Implementation of a patient-friendly medication schedule to improve patient safety within a healthcare system. J Healthc Risk Mgmt. 2010;29:22–27. doi: 10.1002/jhrm.20030. [DOI] [PubMed] [Google Scholar]
- 32.Freysteinson WM. The ethical community consultation model as preparation for nursing research: a case study. Nurs Ethics. 2010;17:749–758. doi: 10.1177/0969733010379176. [DOI] [PubMed] [Google Scholar]
- 33.Gallagher LP, Truglio-Londrigan M, Levin R. Partnership for healthy living: an action research project. Nurs Res. 2009;16:7–29. doi: 10.7748/nr2009.01.16.2.7.c6759. [DOI] [PubMed] [Google Scholar]
- 34.Garretson M, Walline V, Heisler J, Townsend J. New medical school engages rural communities to conduct regional health assessment. Fam Med. 2010;42:693–701. [PubMed] [Google Scholar]
- 35.Goins RT, Garroutte EM, Fox SL, Dee Geiger S, Manson SM. Theory and practice in participatory research: lessons from the native elder care study. Gerontology. 2011;51:285–294. doi: 10.1093/geront/gnq130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hitchcock K, Appelt K. Sustainable collaboration for community outreach: lessons from the Spanish Access to Literature/Uso Directo (SALUD) project. J Med Libr Assoc. 2008;96:58–60. doi: 10.3163/1536-5050.96.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.James S, Arniella G, Bickell NA, et al. Community ACTION boards: an innovative model for effective community-academic research partnerships. Prog Commun Health Part. 2011;5:399–404. [PMC free article] [PubMed] [Google Scholar]
- 38.Kaplan SA, Calman NS, Golub M, Ruddock C, Billings J. The role of faith-based institutions in addressing health disparities: a case study of an initiative in the southwest Bronx. J Health Care Poor Underserved. 2006;17:9–19. doi: 10.1353/hpu.2006.0088. [DOI] [PubMed] [Google Scholar]
- 39.Kaplan SA, Ruddock C, Golub M, et al. Stirring up the mud: using a community-based participatory approach to address health disparities through a faith-based initiative. J Health Care Poor Underserved. 2009;20:1111–1123. doi: 10.1353/hpu.0.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kataoka SH, Fuentes S, O’Donoghue VP, et al. A community participatory research partnership: the development of a faith-based intervention for children exposed to violence. Ethnic Dis. 2006;16:S89–97. [PubMed] [Google Scholar]
- 41.Katz JR, Martinez T, Paul R. Community-based participatory research and American Indian/Alaska Native nurse practitioners: a partnership to promote adolescent health. J Amer Acad Nurs Pract. 2011;23:298–304. doi: 10.1111/j.1745-7599.2011.00613.x. [DOI] [PubMed] [Google Scholar]
- 42.Kelly PJ, Lesser J, Cheng AL, et al. A prospective randomized controlled trial of an interpersonal violence prevention program with a Mexican American community. Fam Commun Health. 2010;33:207–215. doi: 10.1097/FCH.0b013e3181e4bc34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim S, Flaskerud JH, Koniak-Griffin D, Dixon EL. Using community-partnered participatory research to address health disparities in a Latino community. J Prof Nurs. 2005;21:199–209. doi: 10.1016/j.profnurs.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 44.Kogan JN, Bauer MS, Dennehy EB, et al. Increasing minority research participation through collaboration with community outpatient clinics: the STEP-BD community partners experience. Clin Trials. 2009;6:344–354. doi: 10.1177/1740774509338427. [DOI] [PubMed] [Google Scholar]
- 45.Laditka JN, Beard RL, Bryant LL, et al. Promoting cognitive health: a formative research collaboration of the healthy aging research network. Gerontology. 2009;49:S12–17. doi: 10.1093/geront/gnp085. [DOI] [PubMed] [Google Scholar]
- 46.Leape LL, Rogers G, Hanna D, et al. Developing and implementing new safe practices: voluntary adoption through statewide collaboratives. Q Saf Health Care. 2006;15:289–295. doi: 10.1136/qshc.2005.017632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Legaspi A, Orr E. Disseminating research on community health and well-being: a collaboration between Alaska Native villages and the academe. Am Indian Alsk Native Ment Health Res. 2007;14:24. doi: 10.5820/aian.1401.2007.28. [DOI] [PubMed] [Google Scholar]
- 48.Lopez ED, Lichtenstein R, Lewis A, et al. Drawing from Freirian empowerment methods to develop and use innovative learning maps: increasing enrollment of uninsured children on Detroit’s eastside. Health Prom Pract. 2007;8:181–191. doi: 10.1177/1524839906286617. [DOI] [PubMed] [Google Scholar]
- 49.McAllister CL, Green BL, Terry MA, Herman V, Mulvey L. Parents, practitioners, and researchers: community-based participatory research with early head start. Am J Pub Health. 2003;93:1672–1679. doi: 10.2105/AJPH.93.10.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McGhan WF, Al M, Doshi JA, Kamae I, Marx SE, Rindress D. The ISPOR good practices for quality improvement of cost-effectiveness research task force report. Value Health. 2009;12:1086–1099. doi: 10.1111/j.1524-4733.2009.00605.x. [DOI] [PubMed] [Google Scholar]
- 51.McKeithen T, Robertson S, Speight M. Developing clinical competencies to assess learning needs and outcomes: the experience of the CS2day initiative. J Cont Educ Health Prof. 2011;31:S21–27. doi: 10.1002/chp.20145. [DOI] [PubMed] [Google Scholar]
- 52.Meredith LS, Branstrom RB, Azocar F, Fikes R, Ettner SL. A collaborative approach to identifying effective incentives for mental health clinicians to improve depression care in a large managed behavioral healthcare organization. Adm Pol Ment Health. 2011;38:193–202. doi: 10.1007/s10488-010-0313-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Noe TD, Manson SM, Croy C, McGough H, Henderson JA, Buchwald DS. The influence of community-based participatory research principles on the likelihood of participation in health research in American Indian communities. Ethnic Dis. 2007;17:S6–14. [PubMed] [Google Scholar]
- 54.Peterson TH, Dolan T, Hanft S. Partnering with youth organizers to prevent violence: an analysis of relationships, power, and change. Prog Commun Health Part. 2010;4:235–242. doi: 10.1353/cpr.2010.0011. [DOI] [PubMed] [Google Scholar]
- 55.Pfefferle SG, Cooper B, Layton D, Rohrbach S. Early collaboration for adaptation: addressing depression in low-income new mothers. J Health Care Poor Underserved. 2009;20:539–544. doi: 10.1353/hpu.0.0134. [DOI] [PubMed] [Google Scholar]
- 56.Pickard AS, Lee TA, Solem CT, Joo MJ, Schumock GT, Krishnan JA. Prioritizing comparative-effectiveness research topics via stakeholder involvement: an application in COPD. Clin Pharm Ther. 2011;90:888–892. doi: 10.1038/clpt.2011.237. [DOI] [PubMed] [Google Scholar]
- 57.Raja S, Ball M, Booth J, Haberstro P, Veith K. Leveraging neighborhood-scale change for policy and program reform in Buffalo. N Y Am J Prev Med. 2009;37:S352–360. doi: 10.1016/j.amepre.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 58.Ray J, White M, Cannon P, Bowen C, O’Rourke K. Implementing the Florida KidCare open enrollment communications campaign: a framework for mobilizing community partners to reduce the number of uninsured children. Int Q Comm Health Educ. 2006;26:365–377. doi: 10.2190/IQ.26.4.e. [DOI] [PubMed] [Google Scholar]
- 59.Redwood D, Lanier A, Kemberling M, Klejka J, Sylvester I, Lundgren K. Community-based participatory research in a large cohort study of chronic diseases among Alaska native adults. Prog Commun Health Part. 2010;4:325–330. doi: 10.1353/cpr.2010.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Redwood Y, Schulz AJ, Israel BA, Yoshihama M, Wang CC, Kreuter M. Social, economic, and political processes that create built environment inequities: perspectives from urban African Americans in Atlanta. Fam Commun Health. 2010;33:53–67. doi: 10.1097/FCH.0b013e3181c4e2d4. [DOI] [PubMed] [Google Scholar]
- 61.Rhodes SD, Hergenrather KC, Montano J, et al. Using community-based participatory research to develop an intervention to reduce HIV and STD infections among Latino men. AIDS Educ Prev. 2006;18:375–389. doi: 10.1521/aeap.2006.18.5.375. [DOI] [PubMed] [Google Scholar]
- 62.Rhodes SD, Hergenrather KC, Vissman AT, et al. Boys must be men, and men must have sex with women: a qualitative CBPR study to explore sexual risk among African American, Latino, and White gay men and MSM. Am J Men’s Health. Mar 2011;5:140–151. [DOI] [PMC free article] [PubMed]
- 63.Sanchez RJ, Mardekian J, Cziraky MJ, Mullins CD. Developing a collaborative study protocol for combining payer-specific data and clinical trials for CER. J Man Care Pharm. 2011;17:S34–37. doi: 10.18553/jmcp.2011.17.s9-a.S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Savage CL, Xu Y, Lee R, Rose BL, Kappesser M, Anthony JS. A case study in the use of community-based participatory research in public health nursing. Publ Health Nurs. 2006;23:472–478. doi: 10.1111/j.1525-1446.2006.00585.x. [DOI] [PubMed] [Google Scholar]
- 65.Schensul JJ, Robison J, Reyes C, Radda K, Gaztambide S, Disch W. Building interdisciplinary/intersectoral research partnerships for community-based mental health research with older minority adults. Am J Commun Psychol. 2006;38:79–93. doi: 10.1007/s10464-006-9059-y. [DOI] [PubMed] [Google Scholar]
- 66.Shah ND, Mullan RJ, Breslin M, Yawn BP, Ting HH, Montori VM. Translating comparative effectiveness into practice: the case of diabetes medications. Med Care. 2010;48:S153–158. doi: 10.1097/MLR.0b013e3181d5956c. [DOI] [PubMed] [Google Scholar]
- 67.Spatz ES, Phipps MS, Wang OJ, et al. Expanding the safety net of specialty care for the uninsured: a case study. Health Serv Res. 2012;47:344–362. doi: 10.1111/j.1475-6773.2011.01330.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Spoth R, Redmond C, Clair S, Shin C, Greenberg M, Feinberg M. Preventing substance misuse through community-university partnerships: randomized controlled trial outcomes 4(1/2) years past baseline. Am J Prev Med. 2011;40:440–447. doi: 10.1016/j.amepre.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Steinman KJ, Wright V, Cooksey E, Myers LJ, Price-Spratlen T, Ryles R. Collaborative research in a faith-based setting: Columbus congregations for healthy youth. Publ Health Rep. 2005;120:213–216. doi: 10.1177/003335490512000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stewart AL, Napoles-Springer AM, Gregorich SE, Santoyo-Olsson J. Interpersonal processes of care survey: patient-reported measures for diverse groups. Health Serv Res. 2007;42:1235–1256. doi: 10.1111/j.1475-6773.2006.00637.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stewart MK, Colley D, Huff A, et al. Participatory development and implementation of a community research workshop: experiences from a community-based participatory research partnership. Prog Commun Health Part. 2009;3:165–178. doi: 10.1353/cpr.0.0068. [DOI] [PubMed] [Google Scholar]
- 72.Stiffman AR, Freedenthal S, Brown E, Ostmann E, Hibbeler P. Field research with underserved minorities: the ideal and the real. J Urban Health. 2005;82:56–66. doi: 10.1093/jurban/jti064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stockdale SE, Mendel P, Jones L, Arroyo W, Gilmore J. Assessing organizational readiness and change in community intervention research: framework for participatory evaluation. Ethnic Dis. 2006;16:S136–145. [PubMed] [Google Scholar]
- 74.Sullivan M, Bhuyan R, Senturia K, Shiu-Thornton S, Ciske S. Participatory action research in practice: a case study in addressing domestic violence in nine cultural communities. J Interpers Violence. 2005;20:977–995. doi: 10.1177/0886260505277680. [DOI] [PubMed] [Google Scholar]
- 75.Tanjasiri S, Tran J, Palmer P, et al. Developing a community-based collaboration to reduce cancer health disparities among Pacific Islanders in California. Pac Health Dialogues. 2007;14:119. [PubMed] [Google Scholar]
- 76.Tanjasiri SP, Tran JH, Palmer PH, Valente TW. Network analysis of an organizational collaboration for Pacific Islander cancer control. J Health Care Poor Underserved. 2007;18:184–196. doi: 10.1353/hpu.2007.0116. [DOI] [PubMed] [Google Scholar]
- 77.Taylor-Piliae RE, Froelicher ES. Methods to optimize recruitment and retention to an exercise study in Chinese immigrants. Nurs Res. 2007;56:132–136. doi: 10.1097/01.NNR.0000263971.46996.14. [DOI] [PubMed] [Google Scholar]
- 78.Weiner J, Aguirre A, Ravenell K, et al. Designing an illustrated patient satisfaction instrument for low-literacy populations. Am J Man Care. 2004;10:853–860. [PubMed] [Google Scholar]
- 79.Wennerstrom A, Vannoy SD, 3rd, Allen CE. Community-based participatory development of a community health worker mental health outreach role to extend collaborative care in post-Katrina New Orleans. Ethnic Dis. 2011;21(S1):45–51. [PMC free article] [PubMed] [Google Scholar]
- 80.Wong C, Mouanoutoua V, Chen MJ. Engaging community in the quality of hypertension care project with Hmong Americans. J Cult Divers. 2008;15:30–36. [PubMed] [Google Scholar]
- 81.Wong FY, Crisostomo VA, Bao D, et al. Development and implementation of a collaborative, multistakeholder research and practice model on HIV prevention targeting Asian/Pacific Islander men in the United States who have sex with men. Am J Pub Health. 2011;101:623–631. doi: 10.2105/AJPH.2008.154245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zoellner J, Connell CL, Santell R, et al. Fit for life steps: results of a community walking intervention in the rural Mississippi delta. Prog Commun Health Part. 2007;1:49–60. doi: 10.1353/cpr.0.0009. [DOI] [PubMed] [Google Scholar]
- 83.NIH. Health Care Systems (HCS) Research Collaboratory. http://grants.nih.gov/grants/guide/rfa-files/RFA-RM-12-002.html. Accessed March 21, 2013.
- 84.Lieu TA, Au D, Krishnan JA, Moss M, Selker H, Harabin A, Taggart V, Connors A. Comparative effectiveness research in lung diseases and sleep disorders: recommendations from the National Heart, Lung, and Blood Institute workshop. Am J Resp Crit Care Med. 2011;184:848–856. doi: 10.1164/rccm.201104-0634WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Agency for Healthcare Research & Quality. Comparative Effectiveness Research Portfolio. http://www.ahrq.gov/cpi/portfolios/comparative-effectiveness/index.html. Accessed March 21, 2014.
- 86.Hartung DMGJ, Fagnan LJ, Davis MM, Stange KC. The role of practice-based research networks in comparative effectiveness research. J Comp Eff Res. 2012;1:45–55. doi: 10.2217/cer.11.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Community-Based Participatory Research [Web page] http://obssr.od.nih.gov/scientific_areas/methodology/community_based_participatory_research/index.aspx. Accessed March 21, 2014.
- 88.Woolf SH. The 2009 breast cancer screening recommendations of the US Preventive Services Task Force. JAMA. 2010;303:162–3. doi: 10.1001/jama.2009.1989. [DOI] [PubMed] [Google Scholar]
- 89.Patient Centered Outcomes Research Institute. Funding Center. http://www.pcori.org/funding-opportunities/funding-announcements/funding-center/, Accessed March 21, 2014.
- 90.Patient Centered Outcomes Research Institute. Research We Support. http://www.pcori.org/research-we-support/. Accessed March 21, 2014.
- 91.Morrato EH, Concannon TW, Meissner P, Shah ND, Turner BJ. Dissemination and implementation of comparative effectiveness evidence: key informant interviews with clinical and translational science award institutions. J Comp Eff Res. 2013;2:185–194. doi: 10.2217/cer.13.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Burke JG, Jones J, Yonas M, Guizzetti L, Virata MC, Costlow M, Morton SC, Elizabeth M. PCOR, CER, and CBPR: alphabet soup or complementary fields of health research? Clin Trans Sci. 2013;6:493–496. doi: 10.1111/cts.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 61 kb)
(PDF 118 kb)