Abstract
[Purpose] The purpose of this study was to investigate the psychometric properties of the lower extremity subscale of the Fugl-Meyer Assessment lower extremity (FMA-LE) for community-dwelling hemiplegic stroke patients. [Subjects] The participants were 140 community-dwelling hemiplegic stroke patients. [Methods] To determine the psychometric properties of the FMA-LE, we examined construct validity, response characteristics, item discrimination, and internal consistency. [Results] Factor analysis of the FMA-LE revealed that the first factor explained 61.73% of the variance and provided evidence of unidimensionality. The FMA-LE did not show ceiling or floor effects; Cronbach’s α was 0.935 (95% CI: 0.919–0.950). [Conclusion] Because the FMA-LE seems to be both valid and reliable, we conclude that it is appropriate for the measurement of the lower extremity motor impairment of community-dwelling hemiplegic stroke patients.
Key words: Fugl-Meyer Assessment, Hemiplegic stroke, Lower extremity
INTRODUCTION
Motor impairment is one of the most common stroke symptoms1). Evidence of relationships between motor impairment and disability, daily activities, and social participation following stroke has been reported. Motor impairment at the time of hospital admission has been reported to be a good predictor of physical disability after stroke rehabilitation. Chae et al.2) investigated motor impairment, assessed using the Fugl-Myer Assessment (FMA) Motor Impairment Scale, as a predictor of physical independence following inpatient stroke rehabilitation, and reported that dependency in physical activities of daily living was primarily determined by the degree of motor impairment. Independent walking has been correlated with lower extremity strength3). Therefore, stroke rehabilitation focuses on the recovery of impaired movement and its associated function4).
More attention has been paid to the evaluation of motor impairments in the upper extremities than in the lower extremities5, 6), despite lower-extremity motor functions being frequently impaired following stroke and functional mobility deterioration7). This tendency also appears in the FMA assessment, and the FMA, which is considered to be one of the most comprehensive quantitative measures of post-stroke motor impairment, suffers from this drawback. The psychometric properties of the FMA with regard to the upper extremities have been verified through various analyses, and it is widely used to assess upper extremity function8,9,10).
Although the FMA is commonly used in clinical trials to assess motor impairment and determine treatment efficacy, no study has yet verified the psychometric properties of the lower extremity subscales. Studies of FMA results for lower-extremities have not provided separate data for this subscale11, 12). The psychometric properties of the upper extremity subscale, however, have been thoroughly established. Woodbury et al.6) reported on the dimensionality and construct validity of the FMA upper extremity scale; we note that as a result, 3 reflex items were removed, based on factor loadings and item infit statistics and a modified 30-item assessment was recommended.
The existing research on the psychometric properties of the FMA has another limitation. To date, most studies have employed heterogeneous samples, and the FMA’s psychometric properties may differ among subjects. More sophisticated methodology is needed13). Therefore, recent research has investigated whether hierarchical properties of the FMA scale are the same in acute and chronic stroke patients14).
Choosing an appropriate measure is the foundation for planning an appropriate course of therapy and assessing the effects of an intervention. Lower extremity motor function of chronic stroke patients is important, and its improvement is a central aim of physical therapy. However, evidence supporting the use of the FMA for lower extremity motor impairment in chronic stroke patients is insufficient. Therefore, the purpose of this study was to investigate the psychometric properties of the FMA-LE subscale for community-dwelling hemiplegic stroke patients.
SUBJECTS AND METHODS
This study followed a cross-sectional design. The sample was chosen from a group of community-dwelling stroke patients visiting convalescence or rehabilitation centers for disabled individuals in South Korea. Patients scoring 18 or below on the Korean version of the Mini Mental State Examination (MMSE-K) were excluded from the study. Approval was received from the ethics review board of our affiliated university. Informed written consent was received from all the participants prior to their participation in the study. Questionnaire responses and measurements of the 140 participants were analyzed; none had missing data. Participants’ ages ranged from 42 to 86 years, with an average age of 57.07 years (SD = 9.88). Of the participants, 37.1% were female. The diagnoses included 66 hemorrhagic strokes and 74 ischemic strokes. The time since diagnosis of stroke ranged from 12 to 269 months, with an average of 50.48 months (SD = 47.06). The mean score on the MMSE-K was 26.63, and ranged from 18 to 30.
We administered the FMA-LE, which consists of 17 items, with a maximum possible score of 34 points. Each item was answered using a 3-point ordinal scale (0 = cannot perform, 1 = can partially perform, 2 = can fully perform). The assessment was completed by trained registered physical therapists.
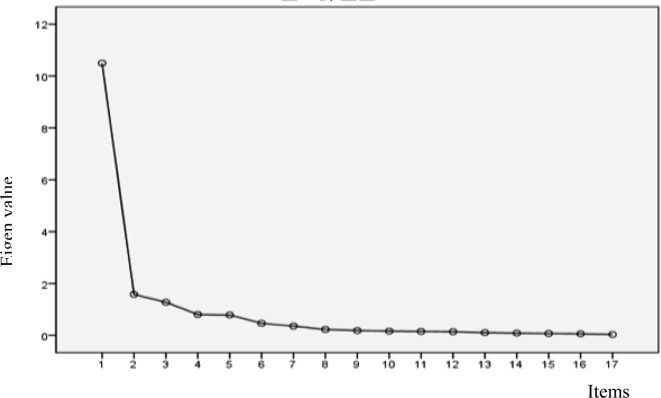
Construct validity, response characteristics, item discrimination and internal consistency were assessed. We employed factor analysis to identify unidimensionality. The suitability of the collected data for factor analysis was examined using Bartlett’s test of sphericity and the Kaiser-Meyer-Olkin (KMO) test. The KMO value was 0.918 and the χ2 of Barlett’s test was 2,841.56 (p < 0.001). The criteria for determining unidimensionality through factor analysis were as follows: 1) the scree plot shows one clear factor, 2) the eigenvalue of this factor is significantly larger than those of other factors, and 3) this factor explains over 20% of the total variance15).
We found that the collected data were appropriate for factor analysis. Item discrimination was analyzed by calculating the correlations between items and total scores. We employed the SPSS 20 for the analysis.
RESULTS
Factor analysis results are presented in Table 1 and Fig. 1.
Table 1. Results of factor analysis.
| Category | Factor 1 | Factor 2 | 1:2 Ratio |
|---|---|---|---|
| Eigenvalue | 10.494 | 1.580 | 6.642 |
| Explained variance (%) | 61.731 | 71.023 |
Fig. 1.
Scree plot
The first factor explained 61.73% of the variance meeting the > 20% criterion. The ratio between the eigenvalues of the first and second factors was 6.642 times the cutoff for unidimensionality reported previously16). The scree plot also showed the unidimensionality of the FMA-LE.
Response characteristics were examined through ceiling and floor effects. The lowest value (0) occurred in 2.9% of the responses, and the highest value (34) occurred in 7.9%.
Table 2 shows item discrimination results.
Table 2. Item discrimination.
| Items | Correlation | Items | Correlation |
|---|---|---|---|
| Hip flexion | 0.784** | Ankle dorsiflexion (sitting) | 0.850** |
| Hip extension | 0.789** | Ankle dorsiflexion (standing) | 0.784** |
| Hip adduction | 0.818** | Ankle plantar flexion | 0.806** |
| Knee flexion (supine) | 0.846** | Heel-shine speed | 0.746** |
| Knee flexion (sitting) | 0.840** | Heel-shin tremor | 0.800** |
| Knee flexion (standing) | 0.835** | Heel-sheen dysmetria | 0.679** |
| Knee extension | 0.859** | Knee reflex | 0.765** |
| Ankle dorsiflexion (supine) | 0.489** | Hamstring reflex | 0.703** |
| Ankle reflex | 0.850** |
**p < 0.01
Cronbach’s α of the FMA-LE was 0.935 (95% CI: 0.919–0.950).
DISCUSSION
The purpose of the present study was to evaluate the reliability and validity of the FMA’s lower extremity subscale. Although the FMA is widely used to measure motor impairment and recovery of stroke patients, the psychometric properties of the lower extremity subscale have not been separately examined until now.
The 50-item FMA motor scale is a widely used assessment of motor function of both the upper and lower extremities following stroke, and has been recommended as an outcome measure for stroke rehabilitation17). Nevertheless, although the construct validity of the FMA has been reported in previous studies, confirmation of unidimensionality of the FMA has only been reported for the upper extremity subscale6). Our results verified the unidemensionality of the FMA-LE, which suggests that the scale has a utility similar to that of the upper extremity subscale.
The acceptable level of ceiling and floor effects is below 30%18). We found no ceiling or floor effects, with the lowest score percentage being 2.9% and the highest score percentage being 7.9%. Concern about the FMA’s ceiling effect was raised in a previous review13); however, this effect has not been examined objectively. In the present study, the FMA-LE showed no ceiling or floor effects in community-dwelling hemiplegic stroke patients.
Although there is no absolute standard for judging item discrimination, correlations above 0.40, between 0.30–0.40, and below 0.30 have been deemed to have high, moderate, and low discriminant ability, respectively19). If items scored below 0.20, they were considered for removal in a previous study20). We found that the FMA-LE item-total correlations were all above 0.40.
The FMA-LE demonstrated high internal consistency. According to Nunnally and Bernstein21), the classifications for the strength of Cronbach’s α coefficients are: poor = below 0.50, moderate from 0.50 to 0.75, good = 0.75 to 0.90, and high above 0.90. Our result for internal consistency was similar to the value of 0.96 found in the study by Duncan et al22). Methodological shortcomings related to a small number of subjects being tested have been raised in previous research examining the reliability of the FMA13). Our participants were 140 hemiplegic community-dwelling patients. The present results suggest that the FMA-LE is a reliable assessment tool for this group.
The FMA has been deemed to have appropriate validity and reliability; however, physical therapists should bear its limitations in mind. Our results suggest that the FMA-LE can be used as a separate assessment for measuring the motor impairment of community-dwelling stroke patients with hemiplegia. Further studies should explore the various psychometric properties among homogenous subjects.
REFERENCES
- 1.Sullivan KJ, Tilson JK, Cen SY, et al. : Fugl-Meyer assessment of sensorimotor function after stroke: standardized training procedure for clinical practice and clinical trials. Stroke, 2011, 42: 427–432. [DOI] [PubMed] [Google Scholar]
- 2.Chae J, Johnston M, Kim H, et al. : Admission motor impairment as a predictor of physical disability after stroke rehabilitation. Am J Phys Med Rehabil, 1995, 74: 218–223. [DOI] [PubMed] [Google Scholar]
- 3.Jørgensen HS, Nakayama H, Raaschou HO, et al. : Recovery of walking function in stroke patients: the Copenhagen Stroke Study. Arch Phys Med Rehabil, 1995, 76: 27–32. [DOI] [PubMed] [Google Scholar]
- 4.Langhorne P, Coupar F, Pollock A: Motor recovery after stroke: a systematic review. Lancet Neurol, 2009, 8: 741–754. [DOI] [PubMed] [Google Scholar]
- 5.Page SJ, Levine P, Hade E: Psychometric properties and administration of the wrist/hand subscales of the Fugl-Meyer Assessment in minimally impaired upper extremity hemiparesis in stroke. Arch Phys Med Rehabil, 2012, 93: 2373–2376, e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woodbury ML, Velozo CA, Richards LG, et al. : Dimensionality and construct validity of the Fugl-Meyer Assessment of the upper extremity. Arch Phys Med Rehabil, 2007, 88: 715–723. [DOI] [PubMed] [Google Scholar]
- 7.Perry J, Garrett M, Gronley JK, et al. : Classification of walking handicap in the stroke population. Stroke, 1995, 26: 982–989. [DOI] [PubMed] [Google Scholar]
- 8.Malouin F, Pichard L, Bonneau C, et al. : Evaluating motor recovery early after stroke: comparison of the Fugl-Meyer Assessment and the Motor Assessment Scale. Arch Phys Med Rehabil, 1994, 75: 1206–1212. [DOI] [PubMed] [Google Scholar]
- 9.van der Lee JH, Beckerman H, Lankhorst GJ, et al. : The responsiveness of the Action Research Arm test and the Fugl-Meyer Assessment scale in chronic stroke patients. J Rehabil Med, 2001, 33: 110–113. [DOI] [PubMed] [Google Scholar]
- 10.Rabadi MH, Rabadi FM: Comparison of the action research arm test and the Fugl-Meyer assessment as measures of upper-extremity motor weakness after stroke. Arch Phys Med Rehabil, 2006, 87: 962–966. [DOI] [PubMed] [Google Scholar]
- 11.Kim H, Her J, Ko J, et al. : Reliability, concurrent validity, and responsiveness of the Fugl-Meyer Assessment (FMA) for hemiplegic patients. J Phys Ther Sci, 2012, 24: 893–899. [Google Scholar]
- 12.Crow JL, Harmeling-van der Wel BC: Hierarchical properties of the motor function sections of the Fugl-Meyer assessment scale for people after stroke: a retrospective study. Phys Ther, 2008, 88: 1554–1567. [DOI] [PubMed] [Google Scholar]
- 13.Gladstone DJ, Danells CJ, Black SE: The fugl-meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil Neural Repair, 2002, 16: 232–240. [DOI] [PubMed] [Google Scholar]
- 14.Crow JL, Kwakkel G, Bussmann JB, et al. : Are hierarchical properties of the Fugl-Meyer Assessment Scale (FM Motor Scale) the same in acute and chronic stroke? Phys Ther, 2014, Advance online publication. [DOI] [PubMed] [Google Scholar]
- 15.Hambleton RK, Swaminatha H, Rogers HJ: Fundamentals of Item Response Theory. Newbury Park: Sage, 1991, pp 50–160. [Google Scholar]
- 16.Waller NG, Kojetin BA, Bouchard TJ, et al. : Genetic and environmental influences on religious interests, attitudes, and values: a study of twins reared apart and together. Psychol Sci, 1990, 1: 138–142. [Google Scholar]
- 17.Chen KL, Chen CT, Chou YT, et al. : Is the long form of the Fugl-Meyer Motor Scale more responsive than the short form in patients with wtroke? Arch Phys Med Rehabil, 2014, Advance online publication. [DOI] [PubMed] [Google Scholar]
- 18.Kane RL: Understanding Health Care Outcomes Research, 2nd ed. Massachusetts: Jones and Bartlett, 2006, pp 60–193. [Google Scholar]
- 19.Ebel RL: Measuring Educational Acheivement. NJ: Prentice-Hall, 1972, p 399. [Google Scholar]
- 20.Sung TJ: The Theory and Practice of Item Development and Analysis. Seoul: Hakjisa, 2004, pp 193–218. [Google Scholar]
- 21.Nunnally JS, Bernstein IH: Psychometric Theory, 3rd ed. USA: McGraw-Hill, 1994, pp 264–265. [Google Scholar]
- 22.Duncan PW, Propst M, Nelson SG: Reliability of the Fugl-Meyer assessment of sensorimotor recovery following cerebrovascular accident. Phys Ther, 1983, 63: 1606–1610. [DOI] [PubMed] [Google Scholar]