Abstract
Objective
To review the literature evaluating the effect of practice guidelines and decision aids on use of surgery and regional variation.
Background
The use of surgical procedures varies widely across geographic regions. Although practice guidelines and decision aids have been promoted for reducing variation, their true effectiveness is uncertain.
Methods
Studies evaluating the influence of clinical practice guidelines or consensus statements, shared decision making and decision aids, or provider feedback of comparative utilization, on rates of surgical procedures were identified through literature searches of Ovid MEDLINE, EMBASE, and Web of Science.
Results
A total of 1946 studies were identified and 27 were included in the final review. Of the 12 studies evaluating implementation of guidelines, 6 reported a significant effect. Those examining overall population-based rates had mixed effects, but all studies evaluating procedure choice described at least a small increase in use of recommended therapy. Three of 5 studies examining the effect of guidelines on regional variation reported a significant reduction after dissemination. Of the 15 studies examining decision aids, 5 revealed significant effects. Many studies of decision aids reported decreases in population-based procedure rates. Nearly all studies evaluating the impact of decision aids on procedure choice reported increases in rates of less invasive procedures. Only one study of decision aids assessed changes in regional variation and found mixed results.
Conclusions
Both practice guidelines and decision aids have been proven effective in many clinical contexts. Expanding the clinical scope of these tools and eliminating barriers to implementation will be essential to further efforts directed toward reducing regional variation in the use of surgery.
Keywords: clinical practice guidelines and consensus statements, geographic variation, health services research, regional variation, shared decision making and decision aids
Studies of surgical variation have shown that a patient’s likelihood of operation often depends as much on where one lives as his or her clinical condition.1–4 According to data from the Dartmouth Atlas of Healthcare, a patient’s chance of undergoing cardiovascular, oncologic, orthopedic, and other procedures can vary 3- to 10-fold across geographic areas.5 Although determinants of regional variation in the use of surgery are debated and likely multifactorial, all agree that this issue is particularly relevant given the current national dialogue regarding health care reform and constraining health care costs.6 More importantly, the presence of wide regional variation in the use of surgery implies that many patients are being undertreated or overtreated.
The optimal strategies for reducing regional variation in the use of surgery remain unclear, however. Previous research suggests that the use of surgery varies in large part as a result of clinical uncertainty, which may in turn reflect gaps in current scientific knowledge or differences in how surgeons apply evidence.7–9 In this context, policymakers, professional organizations, and other stakeholders have pushed to disseminate more evidence-based practice guidelines and consensus statements to facilitate evidence-based clinical decision making.9–12 Even in the presence of sound clinical evidence, regional variation can occur as a result of inconsistent incorporation of individual patient preferences in surgical decisions.13–16 As a result, the use of decision aids and similar tools has been promoted to help patients make more informed decisions, and possibly reduce regional variation.17–20
Despite the conceptual appeal practice guidelines and decision aids may have for reducing surgical variation, their true effectiveness remains unclear. Studies evaluating these tools have been based on diverse patient populations, heterogeneous methods, and disparate measures of effectiveness. To better synthesize the literature in this area, we performed a systematic review of the effect of practice guidelines and decision aids on the use of surgery.
METHODS
Search Strategy
We performed a thorough and structured literature review of published and unpublished articles using the electronic databases MEDLINE (Ovid) (1946, November 2012), EMBASE (1946, November 2012), and Web of Science: Conference Proceedings Citation Index—Science (1990, November 2012). The search strategy was devised with the assistance of a research librarian specialized in the surgical literature. A broad literature search with explosion was conducted on the aforementioned databases using keywords and MeSH (Medical Subject Headings) terms from seminal articles. Results from this preliminary search were reviewed, and an iterative process was used to refine the search strategy over multiple subsequent searches.
The final search included 3 domains of MeSH terms and key words combined using “AND,” whereas each domain was created using “OR.” The first domain included terms to capture articles discussing surgery and surgical procedures, the second included terms to identify the specified strategies for intervention, and the third captured articles reporting surgery rates within a population or study cohort. Both experimental and observational studies were included, and the search was limited to English language and studies of humans. Letters and editorials were excluded (see Supplemental Digital Content Appendix 1, available at http://links.lww.com/SLA/A459, for the full search). Additional searches using Google Scholar and the Cochrane Database of Systematic Reviews were performed to enhance the results by including additional gray literature. Finally, comprehensive forward and backward bibliography searches were completed on all articles from the database search that were included in this review. The flow diagram of the search and systematic review protocol is shown in Figure 1.
FIGURE 1.
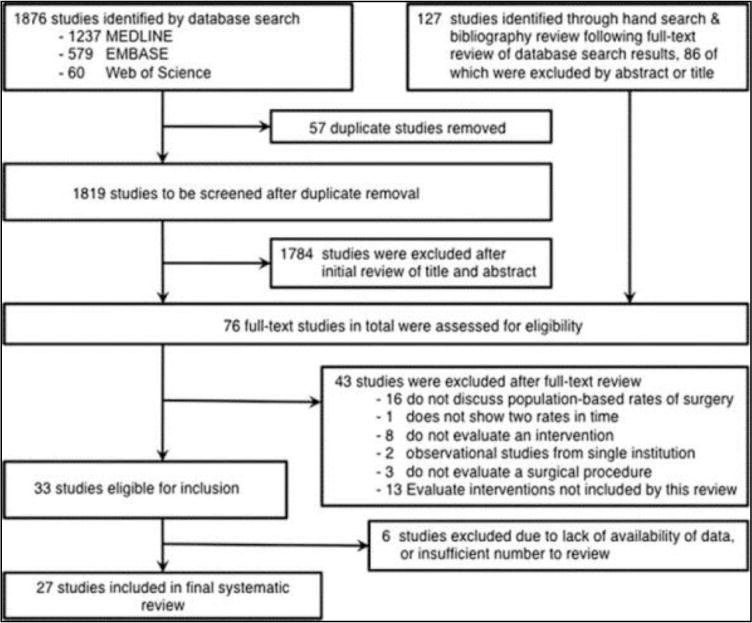
Flow diagram of selection process and systematic review protocol.
Initial Review and Study Inclusion
Two investigators reviewed the titles and abstracts of all studies resulting from the initial database search. Articles were included in this review if they evaluated the rate of a surgical procedure before and after implementation or dissemination of clinical practice guidelines or consensus statements, shared decision-making tools and decision aids, or provider feedback detailing comparative rates of utilization. These were selected a priori, as they represent strategies directly related to clinical decision making and practice. Although other strategies of influence exist (eg, financial incentives, insurance models, and policy), adding these was felt to be beyond the scope of a single systematic review. Studies evaluating nonsurgical procedures such as diagnostic imaging or tests, medical (eg, endoscopy or cardiac catheterization), or dental (eg, wisdom tooth extraction) procedures were excluded. Studies focused on labor or cesarean section rates were also excluded, as this topic has been extensively studied and reviewed.21,22 Single-institution experimental trials were considered for inclusion, but single-institution observational studies were excluded.
To ensure all possibly relevant studies were considered for inclusion, every study with uncertain eligibility at title and abstract review was retained for further examination. Full-text documents were obtained for selected articles, and then 2 investigators independently reviewed the full text of each article to determine final inclusion in the systematic review. A simple kappa statistic (κ) was calculated to determine the level of agreement between investigators regarding final inclusion during the full-text review.23,24 Disagreements were resolved by the input of a third investigator.
Data Extraction, Summary Measures, and Analysis
Two investigators independently recorded data from included studies on a structured data extraction form. Extracted data included study year, location, design, size, type of procedure, intervention used, setting, results, and study conclusions. Study authors were contacted to obtain pertinent data if it was not reported in the full-text article. For observational studies, the reported rate of surgery before and after implementation of the intervention (and associated statistical significance) was used as the primary summary measure of this review. For randomized-controlled trials, the reported rate of surgery in experimental and control groups after the intervention was used as the primary summary measure. Measures of regional variation were recorded as secondary summary measures of this review. Given the extensive heterogeneity present between study designs (experimental and observational) and measures of effect (population-based rates, proportion of cohort, odds ratios, mean annual changes in rates), meta-analyses were not performed,25,26 and statistical evaluation of publication bias was limited to the subset of included randomized controlled trials.27 The Harbord test was applied to this subset to assess for small-study effects, and a funnel plot was visually inspected for asymmetry.28 To minimize risk of publication bias in the cohort of observational studies, a thorough search of the gray literature was conducted, and throughout the review protocol careful consideration for inclusion was given to both positive and negative observational studies.
Quality Assessment
Widely established quality assessment scales were used to assess for potential bias. Two investigators independently evaluated the quality of each included study using a standardized form, and any discrepancies were resolved by a third investigator. Randomized-controlled trials were assessed using the Cochrane Collaboration’s tool for assessing risk of bias to evaluate the quality of studies in the categories of random sequence generation, allocation concealment, blinding of participants, personnel, and outcomes, outcome reporting, and other risks of bias.29 Studies were considered low quality if they exhibited a high or unclear risk of bias in more than 3 major categories. Observational studies were assessed using the Newcastle-Ottawa Scale to evaluate methodological quality over the domains of selection, comparability, and outcome assessment.30 Studies were considered low quality if they did not meet criteria in 3 or more major categories.
Throughout the systematic review protocol, we carefully adhered to the Cochrane Handbook for Systematic Reviews.31 Both the PRISMA statement32 for systematic reviews and meta-analyses of randomized-controlled trials and the MOOSE guidelines33 for meta-analyses of observational studies were strictly followed.
RESULTS
Characteristics of Included Studies
The combined database and literature search identified 1946 studies, of which 76 qualified for full-text evaluation and 33 met inclusion criteria (Fig. 1). The k statistic revealed nearly excellent agreement between investigators after full-text review (87.8% agreement, κ = 0.733, P < 0.001). Seven of the included articles did not report specific rates of the procedure studied, and each corresponding author was contacted for additional information. Three articles were excluded because the authors confirmed the specific data of interest was not available,34–36 and 1 study was excluded after multiple failed attempts to contact the author.37
The majority of selected studies focused on clinical guidelines or decision aids. Only 2 of the selected studies evaluated the use of provider feedback detailing comparative utilization,38,39 and thus were excluded from formal systematic review. Characteristics of the included studies are detailed in Tables 1 and 2. Twelve studies evaluated the dissemination of practice guidelines or consensus statements, and 15 examined the use of decision aids and shared decision-making tools on rates of surgical procedures.
TABLE 1.
Summary of Studies Evaluating Dissemination of Practice Guidelines or Consensus Statements
| Author/s, Year | Study Design | Years Studied | Study Population | Location | Procedure | Quality | Practice Guideline or Consensus Statement | Summary of Findings | Statistically Signific ant Effect |
|---|---|---|---|---|---|---|---|---|---|
| Studies evaluating effects on population-based rates of surgery | |||||||||
| Black and Hutchings40 2002 | E | 1975–1998 | Children aged 10 or younger in 13 English health districts | United Kingdom | Myringotomy or tympanostomy tube insertion | Low | 1992 NHS Effective Health Care bulletin | The yearly decline in mean annual procedure rate increased from 1.6% to 10.1% in NHS hospitals during the study period. | Yes |
| Brownell42 2002 | E | 1994–1999 | Children aged 19 or younger in Manitoba | Canada | Tonsillectomy, adenoidectomy | High | 1995 Manitoba Clinical Guidelines and Analysis Program: Tonsillectomy Review Panel | Overall procedure rates decreased significantly after guideline release in all regions studied, but rates in some regions subsequently increased. | Mixed |
| Mason et al41 2001 | E | 1989–1996 | Children aged 15 or younger in England | United Kingdom | Tympanostomy tube insertion | Low | 1992 NHS Effective Health Care bulletin | In the 3 years before guideline distribution there was a small quarterly procedure rate increase. This increase subsequently decreased in the 4 years after implementation. Overall procedure rates decreased from 2.1 to 1.4 per 1000. | Yes |
| Rob et al43 2004 | RC | 1981, 1983, 1986, 1988–1999 | Children aged 15 or younger in New South Wales | Australia | Myringotomy, tonsillectomy, adenoidectomy, or tonsillectomy and adenoidectomy | Low | 1993 NSW Health Department Working Party: Guidelines on the management of pediatric middle ear disease | Procedure rates decreased immediately after guideline introduction, but subsequently increased in the next few years. Overall rate of procedures increased by 21% during the study period. | No |
| Sherman et al44 1992 | RC | 1983–1989 | 56,406 patients SEER and Medicare databases | United States | Radical prostatectomy | High | 1987 NIH CDC on management of clinically localized prostate cancer | Preconference procedure rate was increasing at 2% per year and did not change after the consensus conference. | No |
| Studies evaluating effects on the choice of procedure | |||||||||
| Du et al45 2000 | RC | 1983–1995 | 169,466 patients SEER database | United States | Breast conservation therapy | High | 1990 NIH CDC on treatment of early stage breast cancer | Overall BCT rates increased from 27.5% to 42.6% after guideline release. The rate of BCT use increased by 2.37% in the initial period after the conference. | Yes |
| Fukada et al46 2009 | RC | 1996–2007 | 2199 patients 5 hospitals | Japan | Breast conservation therapy | High | 1999 Japanese Breast Cancer Society Practice Guideline: Breast Conserving Surgery | The proportion of patients undergoing BCT increased from 26.4% to 59.9% after guideline publication. | Yes |
| Kosecoff et al51 1987 | RC | 1977–1981 | 2770 patients 10 hospitals | United States | Total mastectomy with axillary dissection | Low | 1979 NIH CDC on treatment of primary breast cancer: management of local disease | The proportion of patients receiving total mastectomy with axillary dissection increased from 74% in 1977–1978 to 84% after guideline publication in 1980–1981. | No |
| Lazovich et al47 1997 | RC | 1983–1993 | 13,551 patients SEER database | United States | Breast conservation therapy | High | 1990 NIH CDC on treatment of early stage breast cancer | In this study, BCT rates increased from 36.9% in 1983–1985 to 54.9% in 1990–1993 for stage I patients and from 25.1% to 35.2% in stage II patients. | Yes |
| Lazovich et al48 1999 | RC | 1983–1995 | 109,880 patients SEER database | United States | Breast conservation therapy | High | 1990 NIH CDC on treatment of early stage breast cancer | In this study, BCT rates increased from 34.6% in 1985–1990 to 53.4% in 1990–1995. When compared to 1983–1985, the adjusted OR of BCT in 1990–1995 was 3.39 for stage I and 3.11 for stage II patients. | Yes |
| Nattinger et al49 2000 | RC | 1983–1995 | 145,490 Patients SEER database | United States | Breast conservation therapy | High | 1990 NIH CDC on treatment of early stage breast cancer | After guideline release, BCT rates increased between 1990 and 1995 from approximately 30% to 50%. | Not reported |
| Struikmans et al50 2011 | RC | 1997–2008 | 65,966 Patients 4 cancer centers | The Netherlands | Breast conservation surgery and radiotherapy | High | 2002 Working Group Treatment Breast Cancer: Guideline Treatment Breast Cancer | The proportion of patients receiving breast conservation surgery increased from 32% to 45% in 1997 to 41% to 57% in 2008, whereas use of mastectomy decreased from 50% to 61% to 36% to 53%. Use of postoperative radiotherapy increased in all regions. | Not reported |
| Studies evaluating effects on regional variation | |||||||||
| Brownell42 2002 | Regional variation was present in all study areas and changed over the study period. In 1998–1999, non-Winnipeg children were 30.5% more likely to undergo tonsillectomies than Winnipeg children and tonsillectomy rates varied from 2.3/1000 to 6.9/1000 across regions. | No | |||||||
| Lazovich et al47 1997 | After 1990, the rates of BCT rose from 41.6% to 50.8% in King County and from 19.4% to 35.8% in nearby areas. Overall, there was a decrease in regional variation over the study period. | Yes | |||||||
| Lazovich et al48 1999 | Rates of BCT and regional variation increased in all 9 SEER regions during the study period. Before 1990, rates of BCT was in the range from 12.6% to 33.9% and after 1990, from 26.7 to 55.6%. | No | |||||||
| Mason et al41 2001 | In 1992, regional and national per capita procedure rates varied by a factor of 2. This variation decreased by 30% after bulletin dissemination. | Yes | |||||||
| Struikmans et al50 2011 | Statistically significant differences in utilization of postoperative radiotherapy between centers existed in 1997, but not in 2008. | Yes | |||||||
TABLE 2.
Summary of Studies Evaluating Shared Decision Making and Decision Aids
| Author/s, Year | Study Design | Years Studied | Study Population | Location | Surgery Evaluated | Quality | Summary of Findings | Statistically Significant Effect |
|---|---|---|---|---|---|---|---|---|
| Studies evaluating effects on population-based rates of surgery | ||||||||
| Arterburn et al15 2012 | Prospective cohort | 2009–2010 | 1310 patients 27 surgeons 5 sites | United States | Total hip replacement, total knee replacement | High | The introduction of decision aids led to 26% fewer total hip replacements and 38% fewer total knee replacements. | Yes |
| Auvinen et al52 2004 | Randomized controlled trial | 1993–1994 | 210 patients 4 hospitals | Finland | Radical prostatectomy or orchiectomy | High | In this study, 58% of patients in the enhanced participation arm opted for radical prostatectomy or orchiectomy, whereas 86% of patients in the standard practice arm opted for surgical therapy. | Yes |
| Bernstein et al55 1998 | Randomized controlled trial | 1996–1997 | 217 patients 2 institutions | United States | CABG | High | In this study, 21% of patients using a decision aid chose CABG vs 38% of patients in the usual care group. | No |
| Deyo et al54 2000 | Randomized controlled trial | Not given | 393 patients 2 institutions | United States | Lumbar spine surgery | High | The overall surgery rate was 22% lower for patients receiving the videodisc. Patients with herniated disks underwent significantly less surgery, whereas spinal stenosis patients chose surgery more often. | Mixed |
| Kennedy et al53 2002 | Randomized controlled trial | 1996–1998 | 894 patients 6 hospitals | United Kingdom | Hysterectomy | High | In this study, 38.2% of patients receiving the decision aid and interview, 48% of those receiving standard practice, and 48% of those receiving the decision aid alone chose hysterectomy. | Yes |
| Protheroe et al58 2007 | Randomized controlled trial | 2003–2005 | 146 patients 200 group practices | United Kingdom | Hysterectomy or transcervical endometrial resection | High | In this study, 13% of patients receiving a decision aid and informational leaflet chose surgical treatment compared with 5% of patients receiving an informational leaflet alone. | No |
| Schwartz et al56 2009 | Randomized controlled trial | 2001–2005 | 214 patients 2 institutions | United States | Risk reducing mastectomy | Low | In this study, 18% of patients using a decision aid selected risk reducing mastectomy compared with 13% of patients receiving usual care. | No |
| Tiller et al57 2006 | Randomized controlled trial | Not reported | 131 patients 6 familial cancer clinics | Australia | Prophylactic oopherectomy | Low | In this study, 34% of women with a family history of breast cancer, ovarian cancer, or HNPCC chose prophylactic oophorectomy after viewing a decision aid compared with 30.3% of patients that received only the informational pamphlet. | No |
| Vuorma et al59 2004 | Randomized controlled trial and prospective cohort | 1997–1999 | 363 patients 14 hospitals | Finland | Hysterectomy, uterus saving surgery | High | In this study, 51% of patients receiving the decision aid, 48% of patients receiving usual care, and 53% of those in the pretrial group chose hysterectomy, whereas 10% of patients receiving the decision aid, 16% of patients receiving usual care, and 6% of those in the pretrial group chose uterus saving surgery | No |
| Wagner et al65 1995 | Retrospective cohort and ecological | 1989–1991 | 451 patients 2 KP regions | United States | Transurethral resection of the prostate | High | In Colorado patients receiving the shared decision-making program, rates of TURP decreased from 6 to 2.5 (per 1000) between 1988 and 1991. In Washington patients receiving the same program, rates fell from 4.9 to 2.3 between 1987 and 1990, but increased in 1991. | Mixed |
| Studies evaluating effects on the choice of procedure | ||||||||
| Molenaar et al60 2001 | Prospective cohort | 1996–1998 | 180 patients 3 hospitals | The Netherlands | Breast conservation therapy | Low | In this study, patients who used a decision aid chose BCT in 75% of cases as compared with 68% of those receiving standard care. | No |
| Street et al61 1995 | Randomized controlled trial | 1993–1994 | 60 patients 1 hospital | United States | Breast conservation therapy | Low | In this study, patients who used a decision aid chose BCT in 76% of cases as compared with 58% of those viewing a brochure only. | No |
| Vodermaier et al62 2009 | Randomized controlled trial | 2003–2004 | 152 patients 1 institution | Germany | Breast conservation therapy | High | In this study, patients who used a decision aid chose BCT in 94.9% of cases as compared with 87.8% of those receiving standard care. | No |
| Whelan et al65 1999 | Prospective cohort | 1996–1997 | 369 patients 7 surgeons | Canada | Breast conservation therapy | High | The rate of BCT was 88% before use of a decision board during surgical consultation and decreased to 73% after its introduction. | Yes |
| Whelan et al64 2004 | Randomized controlled trial | 1999–2002 | 201 patients 20 surgeons | Canada | Breast conservation therapy | High | Patients viewing a decision board during surgical consultation chose BCT 94% of the time as compared with 76% of women receiving usual care. | Yes |
| Studies evaluating effects on regional variation | ||||||||
| Wagner et al65 1995 | In 1991, the TURP rate in KP Colorado was 60% lower than other CO regions. The KP region in Washington performed 50% fewer TURPs in 1990 than other WA regions, but this reduction did not persist the following year. | Unclear | ||||||
CABG indicates coronary artery bypass graft; HNPCC, hereditary nonpolyposis colorectal cancer.
Most studies were published within the last 20 years. Twelve (44%) studies originated from the United States and 15 (56%) were international. The majority of articles examining guidelines were observational studies that utilized a retrospective cohort time-series design, whereas most studies of decision aids were randomized-controlled trials. Breast surgery was the most common surgery evaluated (48%), but the type of surgery examined varied significantly between studies. Most studies were considered of high quality (19 of 27, 70%). The Harbord test evaluating for possible small-study effects did not achieve significance, and funnel plot did not reveal significant asymmetry. Measures of the influence of practice guidelines or decision aids on the use of surgery can be characterized in 3 ways: effects on population-based rates of surgery, effects on the choice of procedure, and effects on regional variation in the use of surgery.
Practice Guidelines and Consensus Statements
The details of studies examining the influence of clinical practice guidelines or consensus statements on rates of surgery use are listed in Table 1. Of the 12 studies, 7 evaluate breast cancer surgery, 4 evaluate pediatric ear, nose, and throat surgery, and 1 study evaluates radical prostatectomy.
Population-Based Rates
Five studies evaluated population-based rates of procedures to examine the influence of practice guidelines on the decision to perform surgery. Although 4 of 5 studies found a measurable change in rates reflecting guideline recommendations, only 2 studies report a statistically significant impact. Both of these studies evaluate the 1992 NHS Effective Health Care bulletin’s influence on pediatric tympanostomy tube rates in NHS hospitals.40,41 Of the remaining 3 studies, 2 evaluating pediatric tonsillectomy found rates decreased immediately after guideline dissemination, but returned to baseline or higher levels in the following years.42,43 The single study of radical prostatectomy rates for prostate cancer found that annual rates steadily increased (1%–2% per year) during the study period, but determined this was not attributable to guideline release.44
Procedure Choice
Seven studies evaluated the particular choice of surgical procedure in the treatment of breast cancer. Most of these studies reported an increase in breast conservation therapy (BCT) after implementation of clinical practice guidelines that encouraged its use in certain populations. Four of these studies found the increase in BCT was statistically significant,45–48 whereas 2 studies reported sizable increases in rates (ranging from 10% to 20%) but did not comment on statistical significance.49,50 The only study that did not find a statistically significant effect examined the use of total mastectomy with axillary dissection after a National Institute of Health Consensus Development Conference on primary breast cancer in 1979.51 Despite not achieving significance, it reported an increase in rates of recommended therapy by 10% during the period.
Regional Variation
Five studies of guideline dissemination included an analysis of changes in regional variation. The study by Mason et al41 evaluating tympanostomy tube insertion in NHS hospitals found that regional variation decreased by 30% following the NHS bulletin. Although not evaluating surgery directly, Struikmans et al50 reported that the variation between Dutch centers in radiotherapy utilization after breast conserving surgery was significant before, but not after, the release of multidisciplinary breast cancer treatment guidelines in 2002. Lazovich et al47 found that the range of BCT rates in 3 counties in Washington state was narrowed after the 1990 NIH Consensus Development Conference (19.4%–41.6% before, 35.8%–50.8% after). However, a subsequent study of national data found that the range of BCT rates widened in 9 SEER (Surveillance, Epidemiology, and End Results) registry regions (12.6%–33.9% before, 26.7%–55.6% after).48 Brownell42 reported that substantial regional variation in the rate of tonsillectomies in Manitoba persisted throughout the period studied.
Decision Aids and Shared Decision-Making Tools
Studies evaluating the impact of decision aids and shared decision-making programs in clinical practice are listed in Table 2. The type of procedure examined varied substantially and included surgery for breast cancer, menorrhagia, familial cancer syndromes, benign prostatic hypertrophy, prostate cancer, back pain, ischemic heart disease, and osteoarthritis.
Population-Based Rates
Ten of the included studies examined the influence of decision aids on population-based rates of surgery. Although 3 of these studies reported a statistically significant effect, the direction of influence varied according to the specific operation and clinical context. The strongest impact of decision aids was reported by Arterburn et al15 in a prospective study of osteoarthritis patients who viewed a multimedia decision aid before surgical consultation. In this group of patients, rates of total knee replacement decreased by 38%, and rates of total hip replacement decreased by 26% during the 6-month period. Auvinen et al52 reported a similar decrease in a study evaluating the impact of an enhanced participation program on rates of surgery for prostate cancer. The authors found that only 58% of enhanced participation patients chose surgical therapy, compared with 86% of standard practice patients. A third trial reporting a significant effect compared standard practice, a decision aid, and a decision aid with a preference elicitation interview in women with menorrhagia. This study found that addition of the interview decreased the rate of hysterectomies performed by 10%.53
The study by Deyo et al54 found that although the relative difference of 22% in overall rates of lumbar spine surgery was not significant, the subgroup of patients with herniated discs underwent significantly less surgery throughout the year (32% vs 47% in the booklet group). No significant effects were found after use of decision aids for coronary revascularization,55 risk reducing mastectomy,56 prophylactic oophorectomy,57 or gynecologic procedures for menorrhagia.58,59
Procedure Choice
Five studies investigated the rate of a particular procedure chosen after the need for surgery was established in breast cancer treatment. Three of these did not report a statistically significant change in the rate of a specific procedure after decision aid administration.60–62 The 2 studies that demonstrated significant effects were both performed by Whelan and colleagues and evaluated the rate of BCT. While the study from 1999 found that rates of BCT use decreased from 88% to 73% following administration of a decision board by surgeons,63 the 2004 study reported an increase in BCT rates from 76% to 94%.64
Regional Variation
Wagner et al65 performed the only study to evaluate the influence of decision aids on regional variation. This retrospective study evaluated the impact of a videodisc-based shared decision-making program for Kaiser-Permanente (KP) patients with benign prostatic hypertrophy. The authors compared KP regions in Washington and Colorado that utilized the decision aid with surrounding nonstudy KP regions. After implementation of the decision aid, the investigators found that the 1990 rate of transurethral resection of the prostate (TURP) in the Washington KP region was 50% that of other Washington regions (95% confidence interval, 33%–77%), and the 1991 TURP rate in KP Colorado was 60% lower than other Colorado regions (95% confidence interval, 47–74). However, although this decrease persisted in Colorado, it did not persist in Washington at the conclusion of the study.
DISCUSSION
This is the first systematic review to focus on the impact of clinical practice guidelines and decision aids on population-based rates of surgery, patient procedure choice, and regional variation. Despite heterogeneous patient populations, study designs, and measures of effect among the examined studies, this review highlights the potential of both strategies to influence use of surgery and regional variation.
Half of the studies evaluating the influence of practice guidelines on use of surgery reported statistically significant effects. All studies examining the effect of guidelines on procedure choice (ie, the selection of one procedure over another) found a measurable increase in use of the recommended procedure. Furthermore, of the studies that examined impact on regional variation, 3 of 5 described a significant reduction after guideline implementation. On the contrary, studies that described the impact of guidelines on overall population-based rates were mixed. Although procedure rates in most studies showed some impact, this effect was often transient. In many cases, population-based rates later returned to the prestudy rate, negating the effects of the initial intervention.
To a large degree, our findings mirror the conclusions of previous work examining the influence of guidelines. Grimshaw and colleagues66,67 found that explicit guidelines can be highly effective in improving patient care when supported by rigorous evaluations. A more recent Cochrane review concluded that clinical practice guidelines and other printed materials may have a beneficial effect on practice, but the review was unable to estimate the effect on outcomes or the observed effect size.68 Given that guidelines are heavily dependent on many factors like clinical context and methods of development, dissemination, and implementation,69–71 it comes as no surprise that the impact of individual guidelines on clinical practice may vary widely, as suggested by our results. However, in many clinical contexts, our findings confirm that guidelines have the potential to influence use of surgery and reduce the wide variation observed across geographic areas.
We found similar results in our analysis of studies evaluating the impact of decision aids. Although only one study evaluated their effects on regional variation, with mixed results, statistically significant effects were observed in one third of the included studies. The introduction of decision aids led to reductions in population-based procedure rates in many studies examined. However, 1 study of menorrhagia patients, and 2 studies of prophylactic surgery for patients at high-risk for cancer, reported small but nonsignificant increases in procedure rates. Almost all studies evaluating a patient’s choice of procedure found that decision aids increased use of the less invasive option. Although these findings highlight the potential of decision aids to influence use of procedures and possibly reduce variation, these results also illustrate that the direction of influence is highly dependent on the specific circumstance and clinical context.
Although this is the first review to specifically evaluate the influence of decision aids on population-based rates of surgery, multiple recent reviews corroborate these findings. A 2011 review from the Cochrane Collaboration confirmed that the use of decision aids enhances patient decision making across multiple other important domains.20 The authors found that decision aids increase knowledge scores, improve patient perceptions of risk, lessen decisional conflict, decrease the proportion of patients who assume a passive role and who remain undecided, and increase consistency between patients’ informed values and the treatment chosen. Although not a primary outcome of their analysis, they also reported decreases in the utilization of major surgery with use of some decision aids. A more recent review by Knops and colleagues72 also reported that patients using decision aids chose less invasive treatments more frequently.
This systematic review has several limitations. First, because there was no single term within the controlled vocabularies (eg, Medical Subject Headings, EMTREE) to reflect the rate of surgery concept, broad statistical subheadings, and controlled terms were used in combination with title and abstract keywords. Although such an approach is sufficiently sensitive for this review, it could have resulted in a failure to identify some articles that meet inclusion criteria. To ensure this risk was minimized, the keyword search was kept broad and articles with uncertain eligibility were included for further review at each stage. In addition, the database search was supported by multiple searches of common search engines and a comprehensive backward and forward bibliography search of included studies. A second limitation is the substantial heterogeneity of published studies with regards to study design, patient populations, and outcome measures, which led to considerable variability within the results of individual studies and precluded formal meta-analysis.
Third, most of the studies evaluating guidelines utilized a retrospective time-series observational study design. Although replicate measures may help identify regression to the mean, this design cannot separate effects of the intervention in question from secular trends. And fourth, many of the included studies report on a small population size and are likely inadequately powered to detect a statistically significant effect. Despite this potential bias toward the null hypothesis, this review was able to identify evidence to support the use of practice guidelines and decision aids to reduce the regional variation observed in use of surgery.
The current literature evaluating the impact of guidelines and decision aids on use of surgery and regional variation is deep but limited in clinical scope. Of the 27 studies included in this review, 75% focus on 4 surgical conditions: breast cancer, prostatic disease, tonsillitis, and recurrent ear infection. As a result, the generalizability of these studies toward other clinical contexts remains uncertain, and suggests the need for further research. This gap in knowledge presents a significant opportunity for health care researchers. Professional and specialty organizations, in turn, should continue to encourage, develop, and disseminate new guidelines and decision tools using the highest-quality evidence available, to maximize the potential effectiveness of these strategies.
Although the primary focus of this review was to assess the comparative effectiveness of guideline dissemination and decision aids in reducing variation, the broader dissemination of these tools into real world clinical practice will depend on additional factors. Incentives for physicians to use them would no doubt accelerate adoption. Accountable care organizations, shared savings programs, and risk-based reimbursement (including capitation) may better establish the “business case” for reducing regional variation in the use of surgery.6 Payers could create additional incentives through pay-for-performance programs.18
In addition to financial incentives, the use of practice guidelines and decision aids could be enhanced by reducing practical barriers to their implementation in everyday clinical practice. As laid out in the PARIHS framework, for example, successful implementation of clinical interventions depends on not only high-quality evidence, but also a receptive environment, facilitation, and support.73,74 Buy-in from surgeons will be essential in establishing that environment. Rather than view guidelines and decision aids as threats to their professional autonomy, surgeons could be proactive and take the lead in the development of these tools and the processes by which they are incorporated into day-to-day clinical decision making. Advances in electronic health record systems and information technology may also help minimize clinical workflow disruptions and accelerate adoption.
CONCLUSIONS
Although current implementation barriers should not be underestimated, findings from this review suggest that practice guidelines and decision aids could help surgeons improve clinical decision making for individual patients and populations with many clinical conditions.
Supplementary Material
Acknowledgments
The authors thank Mark P. MacEachern for his assistance in constructing and refining the literature search.
Disclosure: Supported by the National Cancer Institute grant (5-T32-CA-009672-22) (Dr Reames) and the National Institute on Aging grant (5-P01-AG-019783-10) (Dr Birkmeyer). These funding sources had no involvement in the manuscript herein. Dr Reames and Dr Shubeck have no conflicts of interest or disclosures related to the content of the manuscript. Dr Birkmeyer is Chief Scientific Officer and has an equity interest in ArborMetrix, Inc, which provides software and analytics for measuring hospital quality and efficiency. The company had no role in this study.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
References
- 1.Wennberg J, Gittelsohn J. Small area variations in health care delivery. Science. 1973;182:1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- 2.McPherson K, Wennberg JE, Hovind OB, et al. Small-area variations in the use of common surgical procedures: an international comparison of New England, England, and Norway. N Engl J Med. 1982;307:1310–1314. doi: 10.1056/NEJM198211183072104. [DOI] [PubMed] [Google Scholar]
- 3.Nattinger AB, Gottlieb MS, Veum J, et al. Geographic variation in the use of breast-conserving treatment for breast cancer. N Engl J Med. 1992;326:1102–1107. doi: 10.1056/NEJM199204233261702. [DOI] [PubMed] [Google Scholar]
- 4.Widmer M, Matter P, Staub L, et al. Regional variation in orthopedic surgery in Switzerland. Health Place. 2009;15:791–798. doi: 10.1016/j.healthplace.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 5.Dartmouth Atlas Project Database [database online] The Dartmouth Institute or Health Policy and Clinical Practice. 1996–2010 Available at: http://www.dartmouthatlas.org. Accessed September 24, 2013.
- 6.Wennberg JE, Brownlee S, Fisher ES, et al. Improving quality and curbing health care spending: opportunities for the Congress and the Obama Administration. A Dartmouth Atlas White Paper. 2008:1–18. [PubMed] [Google Scholar]
- 7.Wennberg JE, Fowler FJ., Jr A test of consumer contribution to small area variations in health care delivery. J Maine Med Assoc. 1977;68:275–279. [PubMed] [Google Scholar]
- 8.Wennberg JE. Dealing with medical practice variations: a proposal for action. Health Aff (Millwood) 1984;3:6–32. doi: 10.1377/hlthaff.3.2.6. [DOI] [PubMed] [Google Scholar]
- 9.Ray-Coquard I, Philip T, Lehmann M, et al. Impact of a clinical guidelines program for breast and colon cancer in a French cancer center. JAMA. 1997;278:1591–1595. [PubMed] [Google Scholar]
- 10.Vayda E. A comparison of surgical rates in Canada and in England and Wales. N Engl J Med. 1973;289:1224–1229. doi: 10.1056/NEJM197312062892305. [DOI] [PubMed] [Google Scholar]
- 11.Eddy DM. Variations in physician practice: the role of uncertainty. Health Aff (Millwood) 1984;3:74–89. doi: 10.1377/hlthaff.3.2.74. [DOI] [PubMed] [Google Scholar]
- 12.Park RE, Fink A, Brook RH, et al. Physician ratings of appropriate indications for six medical and surgical procedures. Am J Public Health. 1986;76:766–772. doi: 10.2105/ajph.76.7.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farrow DC, Hunt WC, Samet JM. Geographic variation in the treatment of localized breast cancer. N Engl J Med. 1992;326:1097–101. doi: 10.1056/NEJM199204233261701. [DOI] [PubMed] [Google Scholar]
- 14.Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health Aff (Millwood) 2002:W96–W114. doi: 10.1377/hlthaff.w2.96. Suppl Web Exclusives: [DOI] [PubMed] [Google Scholar]
- 15.Arterburn D, Wellman R, Westbrook E, et al. Introducing decision aids at Group Health was linked to sharply lower hip and knee surgery rates and costs. Health Aff (Millwood) 2012;31:2094–2104. doi: 10.1377/hlthaff.2011.0686. [DOI] [PubMed] [Google Scholar]
- 16.A Dartmouth Atlas Project Topic Brief: Preference Sensitive Care. The Dartmouth Atlas of Health Care. 2007 Available at: http://www.dartmouthatlas.org/downloads/reports/preference_sensitive.pdf. Accessed September 24, 2013. [PubMed]
- 17.Weinstein JN, Clay K, Morgan TS. Informed patient choice: patient-centered valuing of surgical risks and benefits. Health Aff. 2007;26:726–730. doi: 10.1377/hlthaff.26.3.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Connor AM, Wennberg JE, Legare F, et al. Toward the “tipping point”: decision aids and informed patient choice. Health Aff. 2007;26:716–725. doi: 10.1377/hlthaff.26.3.716. [DOI] [PubMed] [Google Scholar]
- 19.Elwyn G, Laitner S, Coulter A, et al. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146. doi: 10.1136/bmj.c5146. [DOI] [PubMed] [Google Scholar]
- 20.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;(10):CD001431. doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- 21.Korst LM, Gregory KD, Fridman M, et al. Nonclinical factors affecting women’s access to trial of labor after cesarean delivery. Clin Perinatol. 2011;38:193–216. doi: 10.1016/j.clp.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Khunpradit S, Tavender E, Lumbiganon P, et al. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst Rev. 2011;(6):CD005528. doi: 10.1002/14651858.CD005528.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 24.Banerjee M, Capozzoli M, Sweeney ML, et al. Beyond kappa: a review of interrater agreement measures. Can J Stat. 1999;27:3–23. [Google Scholar]
- 25.Higgins JPT, Green S, editors. Chapter 9: Analysing data and undertaking meta-analyses: Introduction – When not to use meta-analyses in a review [Cochrane Handbook for Systematic Reviews of Interventions web site] 2011 Available at: http://handbook.cochrane.org./ Accessed December 28, 2012.
- 26.Higgins JPT. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008;37:1158–1160. doi: 10.1093/ije/dyn204. [DOI] [PubMed] [Google Scholar]
- 27.Terrin N, Schmid CH, Lau J, et al. Adjusting for publication bias in the presence of heterogeneity. Stat Med. 2003;22:2113–2126. doi: 10.1002/sim.1461. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JPT, Green S, editors. Chapter 10: Addressing reporting biases: Recommendations on testing for funnel plot asymmetry [Cochrane Handbook for Systematic Reviews of Interventions web site] 2011 Available at: http://handbook.cochrane.org./ Accessed July 22, 2013.
- 29.Higgins JPT, Green S, editors. Chapter 8: Assessing risk of bias in included studies [Cochrane Handbook for Systematic Reviews of Interventions web site] 2011 Available at: http://handbook.cochrane.org./ Accessed March 1, 2013.
- 30.Wells GA, D O’Connell BS, Peterson J, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2011 Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed December 28, 2012.
- 31.Higgins JPT, G S. Cochrane Handbook for Systematic Reviews of Interventions. 2011 Available at: http://handbook.cochrane.org./ Accessed December 28, 2012.
- 32.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535–b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 34.Morgan MW, Deber RB, Llewellyn-Thomas HA, et al. Randomized, controlled trial of an interactive videodisc decision aid for patients with ischemic heart disease. J Gen Intern Med. 2000;15:685–693. doi: 10.1046/j.1525-1497.2000.91139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murray E, Davis H, Tai SS, et al. Randomised controlled trial of an interactive multimedia decision aid on benign prostatic hypertrophy in primary care. BMJ. 2001;323:493–496. doi: 10.1136/bmj.323.7311.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Phelan EA, Deyo RA, Cherkin DC, et al. Helping patients decide about back surgery: a randomized trial of an interactive video program. Spine (Phila Pa 1976) 2001;26:206–211. doi: 10.1097/00007632-200101150-00016. discussion 212. [DOI] [PubMed] [Google Scholar]
- 37.Tataru D, Robinson D, Moller H, et al. Trends in the treatment of breast cancer in Southeast England following the introduction of national guidelines. J Public Health (Oxf) 2006;28:215–217. doi: 10.1093/pubmed/fdl011. [DOI] [PubMed] [Google Scholar]
- 38.Wennberg JE, Blowers L, Parker R, et al. Changes in tonsillectomy rates associated with feedback and review. Pediatrics. 1977;59:821–826. [PubMed] [Google Scholar]
- 39.Keller RB, Soule DN, Wennberg JE, et al. Dealing with geographic variations in the use of hospitals. The experience of the Maine Medical Assessment Foundation Orthopaedic Study Group. J Bone Joint Surg Am. 1990;72:1286–1293. [PubMed] [Google Scholar]
- 40.Black N, Hutchings A. Reduction in the use of surgery for glue ear: did national guidelines have an impact? Qual Saf Health Care. 2002;11:121–124. doi: 10.1136/qhc.11.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mason J, Freemantle N, Browning G. Impact of effective health care bulletin on treatment of persistent glue ear in children: time series analysis. BMJ. 2001;323:1096–1097. doi: 10.1136/bmj.323.7321.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brownell M. Tonsillectomy rates for Manitoba children: temporal and spatial variations. Healthc Manage Forum. 2002;(Suppl):21–26. doi: 10.1016/s0840-4704(10)60178-0. [DOI] [PubMed] [Google Scholar]
- 43.Rob MI, Westbrook JI, Taylor R, et al. Increased rates of ENT surgery among young children: have clinical guidelines made a difference? J Paediatr Child Health. 2004;40:627–632. doi: 10.1111/j.1440-1754.2004.00488.x. [DOI] [PubMed] [Google Scholar]
- 44.Sherman CR, Potosky AL, Weis KA, et al. The Consensus Development Program. Detecting changes in medical practice following a consensus conference on the treatment of prostate cancer. Int J Technol Assess Health Care. 1992;8:683–693. doi: 10.1017/s0266462300002373. [DOI] [PubMed] [Google Scholar]
- 45.Du X, Freeman DH, Jr, Syblik DA. What drove changes in the use of breast conserving surgery since the early 1980s? The role of the clinical trial, celebrity action and an NIH consensus statement. Breast Cancer Res Treat. 2000;62:71–79. doi: 10.1023/a:1006414122201. [DOI] [PubMed] [Google Scholar]
- 46.Fukuda H, Imanaka Y, Ishizaki T, et al. Change in clinical practice after publication of guidelines on breast cancer treatment. Int J Qual Health Care. 2009;21:372–378. doi: 10.1093/intqhc/mzp037. [DOI] [PubMed] [Google Scholar]
- 47.Lazovich D, White E, Thomas DB, et al. Change in the use of breast-conserving surgery in western Washington after the 1990 NIH Consensus Development Conference. Arch Surg. 1997;132:418–423. doi: 10.1001/archsurg.1997.01430280092014. [DOI] [PubMed] [Google Scholar]
- 48.Lazovich D, Solomon CC, Thomas DB, et al. Breast conservation therapy in the United States following the 1990 National Institutes of Health Consensus Development Conference on the treatment of patients with early stage invasive breast carcinoma. Cancer. 1999;86:628–637. [PubMed] [Google Scholar]
- 49.Nattinger AB, Hoffmann RG, Kneusel RT, et al. Relation between appropriateness of primary therapy for early-stage breast carcinoma and increased use of breast-conserving surgery. Lancet. 2000;356:1148–1153. doi: 10.1016/S0140-6736(00)02757-4. [DOI] [PubMed] [Google Scholar]
- 50.Struikmans H, Aarts MJ, Jobsen JJ, et al. An increased utilisation rate and better compliance to guidelines for primary radiotherapy for breast cancer from 1997 till 2008: a population-based study in the Netherlands. Radiother Oncol. 2011;100:320–325. doi: 10.1016/j.radonc.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 51.Kosecoff J, Kanouse DE, Brook RH. Changing practice patterns in the management of primary breast cancer: Consensus Development Program. Health Serv Res. 1990;25:809–823. [PMC free article] [PubMed] [Google Scholar]
- 52.Auvinen A, Hakama M, Ala-Opas M, et al. A randomized trial of choice of treatment in prostate cancer: the effect of intervention on the treatment chosen. BJU Int. 2004;93:52–56. doi: 10.1111/j.1464-410x.2004.04554.x. ; discussion 56. [DOI] [PubMed] [Google Scholar]
- 53.Kennedy AD, Sculpher MJ, Coulter A, et al. Effects of decision aids for menorrhagia on treatment choices, health outcomes, and costs: a randomized controlled trial. JAMA. 2002;288:2701–2708. doi: 10.1001/jama.288.21.2701. [DOI] [PubMed] [Google Scholar]
- 54.Deyo RA, Cherkin DC, Weinstein J, et al. Involving patients in clinical decisions: impact of an interactive video program on use of back surgery. Med Care. 2000;38:959–969. doi: 10.1097/00005650-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 55.Bernstein SJ, Skarupski KA, Grayson CE, et al. A randomized controlled trial of information-giving to patients referred for coronary angiography: effects on outcomes of care. Health Expect. 1998;1:50–61. doi: 10.1046/j.1369-6513.1998.00007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schwartz MD, Valdimarsdottir HB, DeMarco TA, et al. Randomized trial of a decision aid for BRCA1/BRCA2 mutation carriers: impact on measures of decision making and satisfaction. Health Psychol. 2009;28:11–19. doi: 10.1037/a0013147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tiller K, Meiser B, Gaff C, et al. A randomized controlled trial of a decision aid for women at increased risk of ovarian cancer. Med Decis Making. 2006;26:360–372. doi: 10.1177/0272989X06290486. [DOI] [PubMed] [Google Scholar]
- 58.Protheroe J, Bower P, Chew-Graham C, et al. Effectiveness of a computerized decision aid in primary care on decision making and quality of life in menorrhagia: results of the MENTIP randomized controlled trial. Med Decis Making. 2007;27:575–584. doi: 10.1177/0272989X07306785. [DOI] [PubMed] [Google Scholar]
- 59.Vuorma S, Teperi J, Aalto AM, et al. A randomized trial among women with heavy menstruation – impact of a decision aid on treatment outcomes and costs. Health Expect. 2004;7:327–337. doi: 10.1111/j.1369-7625.2004.00297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Molenaar S, Sprangers MA, Rutgers EJ, et al. Decision support for patients with early-stage breast cancer: effects of an interactive breast cancer CDROM on treatment decision, satisfaction, and quality of life. J Clin Oncol. 2001;19:1676–1687. doi: 10.1200/JCO.2001.19.6.1676. [DOI] [PubMed] [Google Scholar]
- 61.Street RL, Jr, Voigt B, Geyer C, Jr, et al. Increasing patient involvement in choosing treatment for early breast cancer. Cancer. 1995;76:2275–2285. doi: 10.1002/1097-0142(19951201)76:11<2275::aid-cncr2820761115>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 62.Vodermaier A, Caspari C, Koehm J, et al. Contextual factors in shared decision making: a randomised controlled trial in women with a strong suspicion of breast cancer. Br J Cancer. 2009;100:590–597. doi: 10.1038/sj.bjc.6604916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Whelan T, Levine M, Gafni A, et al. Mastectomy or lumpectomy? Helping women make informed choices. J Clin Oncol. 1999;17:1727–1735. doi: 10.1200/JCO.1999.17.6.1727. [DOI] [PubMed] [Google Scholar]
- 64.Whelan T, Levine M, Willan A, et al. Effect of a decision aid on knowledge and treatment decision making for breast cancer surgery: a randomized trial. JAMA. 2004;292:435–441. doi: 10.1001/jama.292.4.435. [DOI] [PubMed] [Google Scholar]
- 65.Wagner EH, Barrett P, Barry MJ, et al. The effect of a shared decision making program on rates of surgery for benign prostatic hyperplasia. Pilot results. Med Care. 1995;33:765–770. doi: 10.1097/00005650-199508000-00002. [DOI] [PubMed] [Google Scholar]
- 66.Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342:1317–1322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- 67.Grimshaw JM, Russell IT. Achieving health gain through clinical guidelines II: ensuring guidelines change medical practice. Qual Health Care. 1994;3:45–52. doi: 10.1136/qshc.3.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Giguere A, Legare F, Grimshaw J, et al. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(10):CD004398. doi: 10.1002/14651858.CD004398.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Russell IT, G J. The effectiveness of referral guidelines: a review of the methods and findings of published evaluations. In: Roland MCA, editor. Hospital Referrals. Oxford: Oxford University Press; 1992. pp. 179–211. [Google Scholar]
- 70.Andrews EJ, Redmond HP. A review of clinical guidelines. Br J Surg. 2004;91:956–964. doi: 10.1002/bjs.4630. [DOI] [PubMed] [Google Scholar]
- 71.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8:iii–iv. 1–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 72.Knops AM, Legemate DA, Goossens A, et al. Decision aids for patients facing a surgical treatment decision: a systematic review and meta-analysis. Ann Surg. 2013;257:860–866. doi: 10.1097/SLA.0b013e3182864fd6. [DOI] [PubMed] [Google Scholar]
- 73.Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care. 1998;7:149–158. doi: 10.1136/qshc.7.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Helfrich CD, Damschroder LJ, Hagedorn HJ, et al. A critical synthesis of literature on the promoting action on research implementation in health services (PARIHS) framework. Implement Sci. 2010;5:82. doi: 10.1186/1748-5908-5-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


