Abstract
Objective
Individuals with borderline personality disorder (BPD) often engage in dysregulated eating behaviors, such as binge-eating and purging. Rejection sensitivity, or the tendency to worry about and expect rejection in most situations, may be involved in this relationship by increasing the intensity and frequency of emotion dysregulation.
Method
Using a sample which included individuals diagnosed with BPD, a structural equation model was constructed using BPD symptoms and measures of rejection sensitivity, emotion dysregulation, and dysregulated eating behaviors.
Results
The hypothesized model was supported in which BPD symptoms predicted high levels of rejection sensitivity, which then led to increased problems with emotion dysregulation and subsequent dysregulated eating behaviors. A significant indirect effect for rejection sensitivity on dysregulated eating behaviors, through emotion dysregulation, was found. This model also provided better fit than alternative models.
Conclusion
The results of this study indicate that those with BPD may be more sensitive to rejection, and these fears of rejection may result in increased emotion dysregulation and subsequent dysregulated eating behaviors. Appearance-relevant rejection sensitivity may be an important factor to explore in future research.
Keywords: borderline personality disorder, binge-eating, purging, rejection sensitivity, emotion dysregulation
The relationship between borderline personality disorder (BPD) and dysregulated eating behaviors is quite strong, with binge-eating and purging frequently found in individuals with BPD both with1, and without2, diagnoses of anorexia nervosa and bulimia nervosa. Yet, the mechanisms linking these two phenomena are less well known. One potential mechanism is the dysregulation of negative affect, which has been linked to both BPD3 and dysregulated eating4,5. These findings indicate that dysregulated eating behaviors may arise from fluctuations in negative affect, as well as difficulty tolerating negative emotions6-8. There is also evidence indicating that dysregulated eating behaviors may reduce negative affect9.
One factor that may contribute to emotion dysregulation in both BPD and dysregulated eating behaviors is rejection sensitivity. Rejection sensitivity refers to the disposition to defensively or anxiously expect, readily perceive, and intensely react to situations where rejection is possible10. Essentially, a person with high rejection sensitivity is constantly anticipating rejection, and he or she likely has a low threshold for identifying what are perceived as legitimate signs of rejection. Research on those with high levels of rejection sensitivity has indicated that they are more ready to perceive intentional hurt by significant others, even if the behavior of that significant other is ambiguous or innocuous11.
Importantly, no studies to our knowledge have linked rejection sensitivity to dysregulated eating behaviors, although rejection sensitivity has been linked to BPD12. Rejection sensitivity may induce emotion dysregulation and be particularly relevant to dysregulated eating behaviors in BPD. Appearance-related rejection sensitivity, for example, may contribute to purging behaviors in BPD as a method of simultaneously attempting to change appearance and regulate emotion. The purpose of this study is to test the roles of rejection sensitivity and emotion dysregulation in the relationship between BPD and dysregulated eating behaviors.
Methods
Participants
Participants were 94 college students (20 male and 74 female participants); 26 participants in the present sample (approximately 27%) met diagnostic criteria for BPD. The large percentage of individuals diagnosed with BPD in the sample was the result of an intensive screening process that covered over 5,000 students in order to identify those with high levels of BPD symptomatology. All participants were interviewed with the BPD module of the Structured Clinical Interview for Axis II Personality Disorders13. More detailed information about the sample and diagnostic assessment procedures can be found in Selby et al.5. Individuals were assigned a diagnosis of BPD if they met five or more criteria for BPD, but in this study a dimensional measure of BPD symptoms was created by summing the threshold rating for each symptom. Age of participants ranged from 18-24 with the average age of participants being 18.75 (SD=1.05). The ethnic composition of the sample was 69% Caucasian, 14.1% Hispanic, 10.6% African-American, 2.8% Asian, 2.1% Native American, and 1.4% other ethnicity.
Measures
The Eating Disorder Inventory (EDI)14. In this study only the Bulimia subscale (EDI-BUL) was used, a scale which determines the degree to which individuals engaged in dysregulated eating behaviors such as binge-eating and purging, with higher scores indicative of more severe eating pathology. The alpha for the EDI-BUL in the present sample was α = .84.
The Difficulties in Emotion Regulation Scale (DERS)15 is a 36-item measure that assesses problems with non-acceptance of negative emotions (NONACCEPTANCE), an inability to engage in goal-directed behaviors when experiencing negative emotions (GOALS), difficulties controlling impulsive behaviors when experiencing negative emotions (IMPULSE), limited access to emotion regulation strategies perceived as effective (STRATEGIES), lack of emotional awareness (AWARENESS), and lack of emotional clarity (CLARITY). The AWARENESS and IMPULSE subscales were not used in this study due to poor fit in the measurement model and potential behavioral overlap, respectively. All subscales were scored such that higher scores reflected greater difficulties with emotion dysregulation. Internal consistency for the DERS subscales within this sample ranged from .85 to .91.
The Rejection Sensitivity Questionnaire (RSQ)10 assesses an individual's concern about, and anticipation of, rejection through self-report. It consists of 18 hypothetical interpersonal situations in which rejection by a significant other is possible. For each situation, people were first asked to indicate their degree of anxiety about the outcome of each situation and the likelihood that the other person would respond favorably. The outcome expectation ratings were reverse-coded, then they were multiplied with anxiety ratings; finally they were averaged across scenarios for an overall rejection sensitivity score. The RSQ has demonstrated an alpha of .83.
Data Analytic Strategy
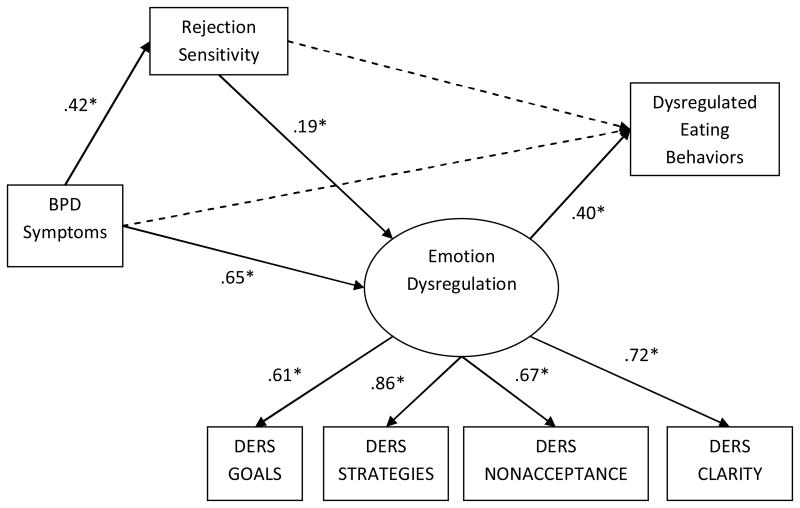
Structural equation modeling with AMOS16 was used to test the model displayed in Figure 1. The latent variable in this model was named Emotion Dysregulation, and it was created from the DERS subscales. We hypothesized that the flow of the model would be such that high BPD symptoms would lead to high levels of rejection sensitivity, which would then lead to high levels of emotion dysregulation and subsequently high levels of dysregulated eating behaviors. Sex was used as a covariate in the model. The fit of the model was evaluated with standard criteria: non-significant chi-square statistic (χ2), comparative fit index (CFI > .95), and root-mean-square error of approximation (RMSEA<.08)17. Akaike Information Criterion (AIC) values with lower AIC values of 10 or more units were used to indicate significantly better fitting models18.
Figure 1.
Note: * indicates path significant at p<.05; dashed lines indicate non-significant paths; DERS refers to the Difficulties with Emotion Regulation Scale.
Results
Structural Equation Model
The inter-correlations, means, and standard deviations of all variables used in the SEM model are displayed in Table 1. The final measurement model provided adequate fit to the data (χ2=4.46, df=2, p=.10, CFI=.98, RMSEA=.10), and all indicators loaded significantly onto the latent variable (NONACCEPTANCE=.70, STRATEGIES=.86, GOALS=.63, and CLARITY=.70; all p's<.01). The structural model (displayed in Figure 1) fit the data well (χ2=21.08, df=16, p=.18, CFI=.98, RMSEA=.06, AIC=77.08). A model with direct paths from both BPD and rejection sensitivity to dysregulated eating behaviors did not significantly improve the fit of the model (χ2=20.24, df=14, p=.12, CFI=.97, RMSEA=.07, χ2diff =.84, df=2, p=ns). As expected, there was a significant correlation between BPD and sex (r=.37, p<.05), but sex did not significantly predict any of the other variables in the model. The path from BPD symptoms to rejection sensitivity was significant (β=.42, p<.01), as was the path from BPD symptoms to emotion dysregulation (β=.65, p<.01). Furthermore, the path from rejection sensitivity to emotion dysregulation was significant (β=.19, p<.05). Finally, the path from emotion dysregulation to dysregulated eating behaviors was significant (β=.40, p<.01).
Table 1. Means, Standard Deviations, Range, and Intercorrelations Between All Variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. BPD Symptoms | -- | |||||||
| 2. Binge-Purge | .35** | -- | ||||||
| 3. Rej-Sensitivity | .44** | .29** | -- | |||||
| 4. NONACCEPT | .49** | .26* | .25* | -- | ||||
| 5. GOALS | .41** | .34** | .28** | .36** | -- | |||
| 6. CLARITY | .60** | .34* | .35** | .56** | .41** | -- | ||
| 7. STRATEGIES | .67** | .35** | .46** | .60* | .58** | .58** | -- | |
| 8. Sex | .37** | .26* | .20 | .26* | .32** | .38* | .24* | -- |
|
| ||||||||
| Mean | 14.37 | 15.26 | 8.39 | 10.57 | 15.54 | 11.27 | 18.48 | 23.2ˆ |
| St. Dev. | 4.88 | 6.98 | 3.28 | 4.81 | 4.90 | 4.24 | 7.74 | N/A |
Note. N=94.
indicates correlation is significant at p<.05;
indicates percent of male participants;
Binge-Purge refers to the bulimia subscale of the EDI; Rej-Sensitivity refers to rejection sensitivity; NONACCEPT refers to the NONACCEPTANCE scale of the DERS.
The Role of Rejection Sensitivity
There was a significant indirect effect of rejection sensitivity on dysregulated eating behaviors (β=.08, z=1.85, p<.05, one-tailed Sobel test). Furthermore, the indirect effect of BPD on emotion dysregulation, flowing through rejection sensitivity, was significant (β=.08, z=1.93, p<.05, one-tailed). Thus, rejection sensitivity may initiate emotion dysregulation in those with BPD, and then contribute to subsequent dysregulated eating behaviors.
Comparisons to Alternative Models
Alternative models in which BPD symptoms lead to emotion dysregulation, followed by dysregulated eating and then resulting in rejection sensitivity (χ2=33.97, df=16, p>.01, CFI=.92, RMSEA=.11, AIC=89.97, AICdiff=12.89) and in which BPD lead to rejection sensitivity, then dysregulated eating, and finally resulted in emotion dysregulation (χ2=69.21, df=16, p<.01, CFI=.78, RMSEA=.19, AIC=125.21, AICdiff=48.13) provided significantly worse fit to the data.
Conclusion
The findings of this study highlight the roles of rejection sensitivity and emotion dysregulation in the relationship between BPD and dysregulated eating behaviors. Importantly, this study replicates the finding that BPD is associated with rejection sensitivity12, and furthermore it provided novel evidence that rejection sensitivity may play a role in dysregulated eating through emotion dysregulation. An important direction for future research may be to determine what specific forms of rejection individuals with BPD are most sensitive to, and which may have the most influence on dysregulated eating behaviors. Further evaluation of differences in the emotional coping effects of binging versus purging is also warranted.
There are some limitations that must be taken into account when evaluating the findings of this study: 1) this was not a clinical sample, 2) the measure of dysregulated eating behaviors may not have been representative of clinically impairing levels of dysregulated eating, and 3) use of a cross-sectional design. Regarding clinical implications, therapeutic interventions may benefit from identifying and correcting rejection based maladaptive thoughts and beliefs in those with BPD and/or dysregulated eating behaviors. Doing so may decrease emotion dysregulation and therefore subsequent dysregulated eating.
Acknowledgments
This study was funded, in part, by National Institute of Mental Health grant F31MH081396 to Edward A. Selby, under the sponsorship of Thomas E. Joiner, Jr. This study was also supported by a Florida State University Bess Ward Honors Thesis Award to Anne C. Ward.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
References
- 1.Cassin SE, von Ranson KM. Personality and eating disorders: A decade in review. Clin Psychol Rev. 2005;25:895–916. doi: 10.1016/j.cpr.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 2.Marino MF, Zanarini MC. Relationship between EDNOS and its subtypes and borderline personality disorder. International Journal of Eating Disorders. 2001;29:349–353. doi: 10.1002/eat.1029. [DOI] [PubMed] [Google Scholar]
- 3.Selby EA, Joiner TE., Jr Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Review of General Psychiatry. doi: 10.1037/a0015687. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Selby EA, Anestis MD, Joiner TE. Understanding the relationship between emotional and behavioral dysregulation: Emotional cascades. Behav Res Ther. 2008;46(5):593–611. doi: 10.1016/j.brat.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Selby EA, Anestis MD, Bender TW, Joiner TE., Jr An exploration of the emotional cascade model in borderline personality disorder. J Abnorm Psychol. 2009;118(2):375–387. doi: 10.1037/a0015711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anestis MD, Selby EA, Fink E, Joiner TE. The multifaceted role of distress tolerance in dysregulated eating behaviors. International Journal of Eating Disorders. 2007;40:718–726. doi: 10.1002/eat.20471. [DOI] [PubMed] [Google Scholar]
- 7.Anestis MD, Peterson CB, Bardone-Cone AM, Klein MH, Mitchell JE, Crosby RD, et al. Affective lability and impulsivity in a clinical sample of women with bulimia nervosa: The role of affect in severely dysregulated behavior. International Journal of Eating Disorders. 2008;42:259–266. doi: 10.1002/eat.20606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whiteside U, Chen E, Neighbors C, Hunter D, Lo T, Larimer M. Difficulties regulating emotions: Do binge eaters have fewer strategies to modulate and tolerate negative affect? Eating Behaviors. 2007;8:162–169. doi: 10.1016/j.eatbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol. 2007;75(4):629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- 10.Downy G, Feldman S. Implications of rejection sensitivity for intimate relationships. J Pers Soc Psychol. 1996;70:1327–1343. doi: 10.1037//0022-3514.70.6.1327. [DOI] [PubMed] [Google Scholar]
- 11.Pietrzak J, Downey G, Ayduk O. Rejection sensitivity as an interpersonal vulnerability. In: Baldwin MW, editor. Interpersonal Cognition. New York: Guildford Press; 2005. pp. 62–84. [Google Scholar]
- 12.Ayduk O, Zayas V, Downey G, Blum Cole A, Shoda Y, Mischel W. Rejection sensitivity and executive control: Joint predictors of borderline personality features. Journal of Research in Personality. 2008;42:151–168. doi: 10.1016/j.jrp.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin L. Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II) Washington, DC: American Psychiatric Publishing; 1997. [Google Scholar]
- 14.Garner DM, Olmstead MP, Polivy J. Development and Validation of a Multidimensional Eating Disorder Inventory for Anorexia Nervosa and Bulimia. International Journal of Eating Disorders. 1983;2:15–19. [Google Scholar]
- 15.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- 16.Arbuckle JL, Wothke W. AMOS 4.0. Chicago, IL: SPSS Inc; 1999. [Google Scholar]
- 17.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 18.Burnham KP, Anderson DR. Multimodel inference: Understanding AIC and BIC in model selection. Sociological Methods and Research. 2004;33(2):261–304. [Google Scholar]