Abstract
OBJECTIVES:
To compare the effects of two 9-month parent-implemented interventions within the Early Social Interaction (ESI) Project. Both individual-ESI, offered 2 or 3 times per week at home or in the community, and group-ESI, offered once per week in a clinic, taught parents how to embed strategies to support social communication throughout everyday activities.
METHODS:
Participants in the randomized controlled trial included 82 children diagnosed with autism spectrum disorder at 16 to 20 months. Children were matched on pretreatment nonverbal developmental level and pairs were randomly assigned to treatment condition. Child outcomes included measures of social communication, autism symptoms, adaptive behavior, and developmental level. Child outcomes are reported from baseline to the end of the 9-month interventions.
RESULTS:
Children in individual-ESI showed differential change on a standardized examiner-administered observational measure of social communication, as they improved at a faster rate than children in group-ESI. Individual-ESI also showed differential efficacy on a parent report measure of communication, daily living, and social skills, as they showed improvement or stability, whereas group-ESI led to worsening or no significant change on these skills. Finally, individual-ESI showed differential change on examiner-administered measures of receptive language skills, as children in individual-ESI improved significantly, whereas group-ESI showed no change.
CONCLUSIONS:
These findings support the efficacy of individual-ESI compared with group-ESI on child outcomes, suggesting the importance of individualized parent coaching in natural environments. The efficacy of a parent-implemented intervention using little professional time has potential for community viability, which is particularly important in light of the lack of main effects on child outcomes of most other parent-implemented interventions.
Keywords: autism, early intervention, toddlers, parent-implemented, outcomes
What’s Known on This Subject:
Randomized controlled trials (RCTs) of intensive clinician-implemented interventions have demonstrated significant improvements in outcomes of toddlers and preschool children with autism spectrum disorder. RCTs of parent-implemented interventions have demonstrated improvements in parent skills, but generally they have not demonstrated effects on children’s outcomes.
What This Study Adds:
This RCT found significantly greater improvements with individual home coaching on child outcome measures of social communication, adaptive behavior, and developmental level. These findings support the efficacy of a parent-implemented intervention using little professional time, which increases potential community viability.
Effective early intervention (EI) for children with autism spectrum disorder (ASD) has the potential to improve outcomes, which can reduce education costs.1–3 EI is a national priority, as evidenced by the Individuals With Disabilities Education Act (IDEA) Part C4 and the American Academy of Pediatrics5 recommendation for universal autism screening at age 18 to 24 months. Although a stable diagnosis is possible at 18 to 24 months,6–8 most children are not diagnosed with ASD until age 4, or later for lower-income, minority, and rural families,9–11 meaning the window of opportunity for EI is missed.
The National Research Council1 recommendation that children receive 25 hours per week of active engagement in systematically planned, developmentally appropriate educational activities is supported by recent systematic reviews.12,13 The recommended intensity of service and urgency of access4 reflects that early social attention deficits lead to cascading effects on learning and developmental outcomes.14–16
Randomized controlled trials (RCTs) with preschoolers with ASD demonstrated significant improvements on joint engagement17,18 and outcomes more distal to treatment targets, including IQ,19,20 and language,21,22 but only 1 study improved autism symptoms.23 RCTs with toddlers offer promise. In a clinician-delivered 2-year RCT of the Early Start Denver Model,20 significant effects were reported on child outcomes of developmental level and adaptive behavior but not on autism symptoms. In another 6-month RCT of an interpersonal synchrony supplement to classroom-based comprehensive intervention,24,25 short- and long-term effects were reported on social communication, developmental level, and adaptive functioning. Autism symptoms improved during treatment, but improvements were not sustained.
In contrast, large-scale RCTs of parent-implemented interventions have not reported main effects on child outcome measures but have found medium to large effects on increasing parent responsivity, synchronization, or interaction skills.26–28 The 2 RCTs of young toddlers did not find significant effects on child outcomes, but both had limited sessions (11–12).26,28 Parent-implemented interventions offering ≥18 sessions were more promising, with significant effects on targeted parent changes.22,23,27 The 1 treatment offered at home found differential effects on expressive language.29 Factors that may contribute to lack of effects of parent-implemented interventions on child outcomes include limited number of sessions (11–24), length (3–12 months), and clinic-based interventions, which may not support generalization.
Existing research has implications for treatments of toddlers with ASD. First, longitudinal and cross-sectional studies suggest that parental involvement is key to long-term change.30,31 Although intensive clinician-implemented treatments often include parents, the focus is on clinician–child curricula rather than parent implementation. Second, few interventions resulted in changes in core autism features unless specifically targeted. Third, current studies highlight potential limitations of existing parent education approaches, underscoring the need for innovative methods leading to stronger treatment effects. Finally, it is vital to improve earlier access to care. Intervention started before 24 months, when symptoms are generally less severe, may reduce the need for more intensive clinician-implemented intervention later. Limitations of existing approaches identify a critical need for evidence-based, community-viable interventions for toddlers with ASD that can be adopted and implemented by public systems.32–35
To address these needs, we developed the Early Social Interaction (ESI) Project36 by incorporating evidence-based active ingredients. Professional time is reduced through parent implementation in natural environments, integrating features consistent with IDEA Part C but also addressing the intensity needed for children with ASD: patient-centered approach, learning in natural environments, collaborative coaching to support parent learning and generalization, developmental framework to prioritize child outcomes, systematic instruction using evidence-based strategies, and intensity needed for children with ASD, achieved by embedding strategies in everyday activities intended for parent implementation ≥25 hours per week. The aim of this RCT was to compare the effects of 2 different ESI conditions, which vary in how (individual or group), how often, and where (home or clinic) parents of toddlers with ASD are taught, on child outcome measures of social communication, autism symptoms, adaptive behavior, and developmental level.
Methods
Study Procedures
Families of 82 toddlers with ASD were randomly assigned to one of two 9-month parent-implemented intervention conditions: individual or group. Child outcomes were measured at baseline and the end of the 9-month intervention.
Participants
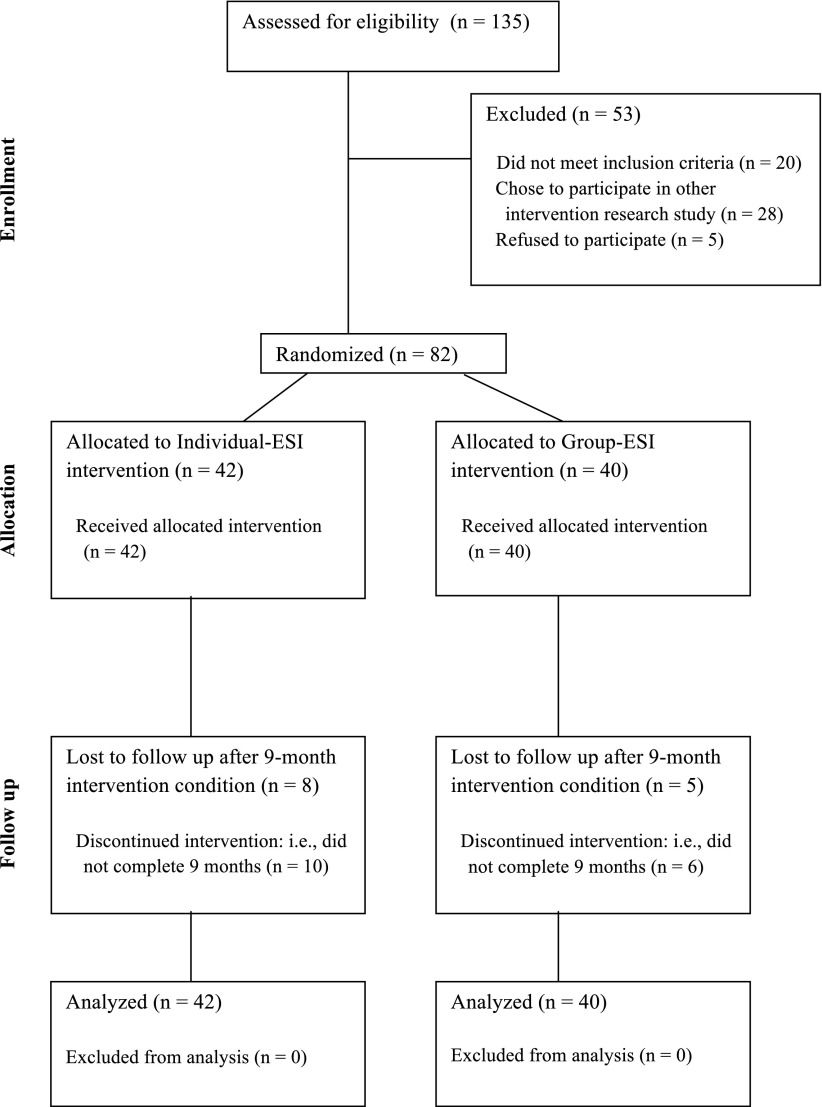
One hundred thirty-five children were assessed for eligibility from 2 sites: Florida State University (FSU) and University of Michigan (UM). FSU recruited children from primary care screening by using the Communication and Symbolic Behavior Scales (CSBS).8,16,37 UM children were referred because of parental or professional concern. Fifty-three were excluded: 20 did not meet inclusion criteria, 28 enrolled in other intervention research studies, and 5 refused to participate. Eighty-two children enrolled in this study. This study was approved by FSU and UM institutional review boards, and all families gave written informed consent for participation.
Children included in this study received an ASD diagnosis between ages 16 and 20 months and lived within 50 miles of either research site. Experienced diagnosticians administered the Autism Diagnostic Observation Schedule (ADOS),38–40 home observation, parent report measures, standardized measures, and developmental history. Clinical judgment was used to make a best estimate diagnosis, the gold standard41,42 shown to predict later diagnosis.6 See Table 1 for baseline characteristics.
TABLE 1.
Participant Demographics and Baseline Characteristics
| Individual-ESI (N = 42) | Group-ESI (N = 40) | p | Hedges’s g | |
|---|---|---|---|---|
| Demographics | ||||
| Age | 19.64 (1.93) | 19.58 (1.42) | .86 | 0.04 |
| Ethnicity | .58 | — | ||
| White, % | 73.8 | 72.5 | — | — |
| Black, % | 7.1 | 10.0 | — | — |
| Other, % | 14.3 | 15.0 | — | — |
| Gender, % male | 81.0 | 92.5 | .13 | — |
| Maternal age | 31.98 (5.74) | 31.71 (5.44) | .83 | 0.05 |
| Maternal education | 15.64 (2.07) | 15.51 (2.26) | .80 | 0.06 |
| Communication and Symbolic Behavior Scales | ||||
| Social Composite | 37.02 (17.25) | 39.49 (21.11) | .57 | 0.13 |
| Speech Composite | 8.61 (2.32) | 6.50 (10.03) | .42 | 0.18 |
| Symbolic Composite | 24.00 (16.60) | 21.54 (15.15) | .49 | 0.15 |
| Autism Diagnostic Observation Schedule | ||||
| Social Affect | 13.50 (4.28) | 14.43 (3.86) | .47 | 0.17 |
| Restricted, Repetitive Behavior | 3.05 (1.50) | 2.85 (1.55) | .66 | 0.10 |
| Vineland Adaptive Behavior Scales | ||||
| Communication | 78.83 (13.06) | 79.79 (13.51) | .98 | 0.01 |
| Daily Living | 86.60 (10.98) | 87.42 (11.97) | .97 | 0.01 |
| Socialization | 84.55 (8.77) | 87.21 (9.62) | .52 | 0.15 |
| Motor | 94.55 (8.85) | 95.34 (11.66) | .72 | 0.08 |
| Adaptive Behavior Composite | 83.98 (8.93) | 85.03 (11.37) | .65 | 0.07 |
| Mullen Scales of Early Learning | ||||
| Visual Reception | 42.07 (13.01) | 40.42 (10.44) | .45 | 0.17 |
| Fine Motor | 46.20 (11.59) | 42.48 (12.65) | .15 | 0.33 |
| Receptive Language | 29.27 (12.34) | 31.35 (12.61) | .39 | 0.19 |
| Expressive Language | 29.61 (11.22) | 28.68 (10.95) | .66 | 0.10 |
| Early Learning Composite | 75.56 (16.68) | 74.05 (16.86) | .69 | 0.17 |
P and Hedges’s g values refer to comparison of individual-ESI and group-ESI conditions. —, not applicable.
Intervention Procedures
Children were randomly assigned to individual-ESI or group-ESI that varied in how and where parents were taught. In both conditions, training focused on teaching parents the importance of intensive intervention and how to support active engagement in natural environments. The manualized Social Communication, Emotional Regulation, and Transactional Supports (SCERTS) curriculum was used for both conditions.43,44 Parents were encouraged to embed evidence-based strategies for child targets in everyday activities for ≥25 hours per week. See Supplemental Information about the ESI model and SCERTS curriculum.
Individual-ESI Condition
Interventionists met individually with parents for 3 sessions per week (2 home, 1 clinic) for 6 months and 2 sessions per week (1 home, 1 community, eg, playground, grocery store, restaurant) for 3 months for maintenance and generalization. Intervention sessions included reviewing and updates, practicing supports and strategies in 3 to 5 different activities, problem solving, and planning. A 4-step collaborative coaching model was used: (1) identify what works, with direct teaching if needed, (2) guided practice with parent in an active role and provide feedback, (3) caregiver-led practice and reflection with feedback, and (4) interventionist back-out for caregiver independence. Interventionists were trained to ≥80% fidelity on 20 items. Fidelity was monitored for 20% of sessions, with an average of 81% fidelity (95% confidence interval, 80% to 82%).
Group-ESI Condition
Interventionists met with groups of 4 or 5 families of children with ASD, communication delays, or typical development in a clinic for 1 session per week. The SCERTS curriculum was organized into 9 monthly topics. An educational meeting was held the first week of the month, where content was discussed without children. The remaining sessions were playgroups that provided opportunities to talk with interventionists and other parents, with practice using strategies. Interventionists were trained to ≥80% fidelity on 10 items. Fidelity was monitored for 20% of sessions with an average of 88% (95% confidence interval, 86%–90%).
Child Measures
Diagnosticians for all measures were blind to intervention condition. Child outcome measures of social communication, autism symptoms, adaptive behavior, and developmental level were collected at baseline and after 9 months of intervention.
Social Communication Skills
The CSBS Behavior Sample is a standardized, norm-referenced examiner-administered assessment using systematic naturalistic sampling procedures to encourage spontaneous social communication.37,45,46 Twenty items are summed to form Social, Speech, and Symbolic composites.
Autism Symptoms
The ADOS,38–40 the gold standard examiner-administered diagnostic measure of ASD, yields Social Affect (SA) and Restricted, Repetitive Behavior (RRB) domain totals by using the ADOS revised algorithms47 to measure autism symptom severity.
Adaptive Behavior
The Vineland Adaptive Behavior Scales, Second Edition (VABS-II48) parent report interview yields standard scores for Communication, Daily Living, Socialization, and Motor.
Developmental Level
The Mullen Scales of Early Learning (MSEL),49 administered by an examiner, measures developmental level with T scores for Visual Reception, Fine Motor, Receptive Language, and Expressive Language.
Intervention Hours
ESI Intervention Hours
Number of sessions per week attended was recorded for 9 months, with a total possible average of 3.33 hours/week of individual or 1 hour/week of group. Parents in individual-ESI attended 80% of scheduled sessions, averaging 2.46 (SD = 0.93) hours/week. Parents in group-ESI attended 82% of scheduled sessions, averaging 0.80 (SD = 0.42) hours/week.
Other Intervention Hours
Parents reported hours of psychosocial and educational intervention in addition to ESI at baseline and updated monthly. The weekly average calculated for individual-ESI was 1.26 (SD = 1.09) hours/week of other intervention, and group-ESI was 1.37 (SD = 1.31). No differences were observed between conditions (P = .66) or sites (P = .11).
Family Evaluation Survey
After the 9-month intervention, parents completed a 20-item survey designed for this study to measure parent perception of family-centered practice (12 items), intervention satisfaction (4 items), and sense of self-efficacy supporting their child’s development (4 items) by using a 4-point rating scale. Reliability was acceptable for each subscale (family-centered, α = 92; satisfaction, α = 0.85; self-efficacy, α = 0.79). Parents in both conditions rated family-centered practice (M = 3.56, SD = 0.55), satisfaction (M = 3.60, SD = 0.50), and self-efficacy (M = 3.45, SD = 0.73) high. Differences were not observed between conditions.
Randomization
Children were randomly assigned by a computer-generated list to either individual-ESI or group-ESI according to a matched random assignment process, which is preferred to stratifying.50 Children were matched on baseline nonverbal developmental level. The first member of each matched pair was randomly assigned to individual or group, and then the other member received the other condition. A trickle process was used as children were enrolled over time, with the matched pair filled when the second member matching that developmental level was determined eligible to allow immediate enrollment.50,51
Data Analysis
Repeated-measures analyses of variance with fixed between- and within-subjects factors were used to determine main effects of time (repeated measures) and interactions between time and treatment condition. Models were run through SPSS MIXED (IBM SPSS Statistics, IBM Corporation) to use maximum likelihood estimation in handling of missing data. Contrasts were performed on outcome measures with significant interaction effects. Consistent with an intent-to-treat approach, all participants were included in analyses regardless of dropout status, with maximum likelihood used to handle missing data from attrition. When available, follow-up data from children who dropped from treatment were include in analyses.
Results
Preliminary Analyses
Outcome variables were examined for nonnormality, with particular attention paid to MSEL and VABS standard scores, which may show floor effects in children with developmental delays. Indices of skewness and kurtosis indicated normality for the majority of outcome variables (ie, skew and kurtosis values <|2|). Nonnormality was observed for some language measures (ie, MSEL Receptive and Expressive Language and CSBS Speech Composite), so these variables were log transformed. Homogeneity of variance was violated for some outcome variables. However, the models used are robust to these violations, particularly when groups are nearly equal in size.52 Standard scores were used when available, rather than raw scores or age equivalents, given the superior psychometric properties of standard scores and the ordinal nature of age equivalent scores.53 When both age equivalents and standardized scores were available (ie, MSEL and VABS), findings were identical in models run with each type of score.
The randomized matching procedure created baseline equivalency between conditions, as P values for all group comparisons on baseline measures were >.10 (range, .15–.98; see Table 1). Condition groups did not differ on demographic variables or hours of other intervention. Differences by site were not observed on demographic variables, CSBS, ADOS, or VABS (P > .10, range, .10–.95). However, as expected given differences in recruitment strategies, FSU children had significantly higher scores on MSEL Visual Reception (P = .05) and Fine Motor (P = .01), but not Receptive or Expressive Language. Site × time × condition effects were calculated and reported to examine potential differential efficacy of treatment by site.
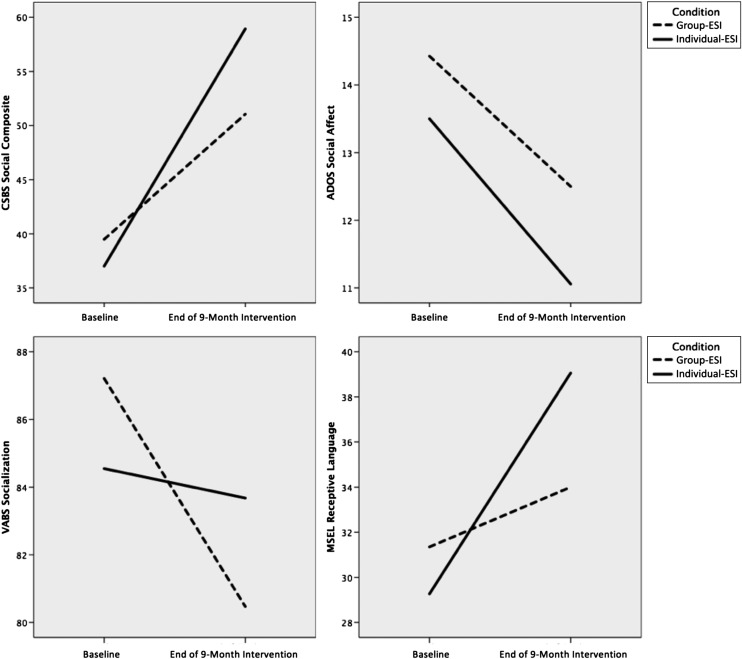
Attrition, defined as failure to return for follow-up assessment (regardless of treatment completion), was 16% (13/82) overall, 19% (8/42) in individual-ESI, and 13% (5/40) in group-ESI. Attrition was comparable between conditions (P = .42) and sites (P = .91). Data from 2 children in individual-ESI and 1 child in group-ESI who dropped treatment during the study were included in analyses. Thus, 33 of the 42 children who were enrolled in individual-ESI and 34 of the 40 who were enrolled in group-ESI completed intervention. Figure 1 shows the participant flowchart. Table 2 reports statistics for child outcomes after the first intervention condition and results of the linear mixed model analyses. Figure 2 illustrates significant effects from baseline to the end of intervention.
FIGURE 1.
Participant Flowchart.
TABLE 2.
Child Outcome Measures and Linear Mixed Model Results
| Child Outcome Measures | Linear Mixed Model Results | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Individual-ESI | Group-ESI | Time (Across Condition) | Time × Condition | ||||||||||||
| M | SE | Δ | 95% CI | M | SE | Δ | 95% CI | p | Hedges’s g | CLES | p | Hedges’s g | CLES | ||
| Communication and Symbolic Behavior Scales | |||||||||||||||
| Social Composite | 59.4 | 3.8 | 22.3 | 15.5 to 29.1 | 51.9 | 3.9 | 12.4 | 5.5 to 19.3 | <.001 | 0.76 | 0.70 | .04 | 0.48 | 0.63 | |
| Speech Compositea | 1.4 | 0.1 | 0.7 | 0.5 to 0.9 | 1.3 | 0.1 | 0.8 | 0.6 to 1.0 | <.001 | 1.27 | 0.82 | .81 | 0.05 | 0.51 | |
| Speech Compositeb | 42.1 | 3.8 | 33.7 | 24.9 to 42.6 | 34.0 | 4.1 | 27.5 | 18.4 to 36.6 | — | — | — | — | — | — | |
| Symbolic Composite | 52.6 | 3.6 | 28.9 | 21.5 to 36.3 | 48.6 | 3.8 | 27.0 | 19.4 to 34.6 | <.001 | 1.28 | 0.82 | .72 | 0.13 | 0.54 | |
| Autism Diagnostic Observation Schedule | |||||||||||||||
| Social Affect | 10.9 | 0.7 | −2.6 | −3.8 to −1.4 | 12.3 | 0.7 | −2.1 | −3.4 to −0.9 | <.001 | −0.51 | 0.36 | .61 | 0.15 | 0.54 | |
| Restricted, Repetitive Behavior | 3.4 | 0.3 | 0.4 | −0.2 to 1.0 | 3.6 | 0.3 | 0.7 | 0.1 to 1.4 | .01 | 0.38 | 0.61 | .43 | 0.17 | 0.55 | |
| Vineland Adaptive Behavior Scales | |||||||||||||||
| Communication | 90.2 | 2.2 | 11.8 | 7.7 to 15.9 | 82.9 | 2.3 | 3.1 | −1.0 to 7.3 | <.001 | 0.50 | 0.64 | .004 | 0.69 | 0.69 | |
| Daily Living | 91.0 | 1.7 | 4.2 | 0.2 to 8.1 | 85.0 | 1.8 | −2.5 | −6.5 to 1.5 | .56 | 0.07 | 0.52 | .02 | 0.58 | 0.66 | |
| Socialization | 84.1 | 1.5 | −0.9 | −4.1 to 2.5 | 81.2 | 1.5 | −5.6 | −9.0 to −2.3 | .008 | −0.31 | 0.41 | .04 | 0.66 | 0.68 | |
| Motor | 88.8 | 1.6 | −5.5 | −8.8 to −2.2 | 87.6 | 1.6 | −8.4 | −11.8 to −5.0 | <.001 | −0.69 | 0.31 | .22 | 0.34 | 0.59 | |
| Adaptive Behavior Composite | 86.2 | 1.6 | 2.2 | −1.0 to 5.5 | 81.7 | 1.6 | −3.3 | −6.7 to 0.0 | .65 | −0.14 | 0.46 | .02 | 0.72 | 0.69 | |
| Mullen Scales of Early Learning | |||||||||||||||
| Visual Reception | 42.1 | 2.2 | −0.1 | −4.2 to 4.0 | 39.2 | 2.2 | −1.2 | −5.4 to 2.9 | .65 | −0.04 | 0.49 | .70 | 0.03 | 0.51 | |
| Fine Motor | 37.2 | 2.0 | −9.0 | −13.1 to −5.0 | 37.7 | 2.1 | −4.7 | −8.8 to −0.7 | <.001 | −0.57 | 0.34 | .14 | 0.41 | 0.61 | |
| Receptive Languagea | 1.6 | 0.0 | 0.1 | 0.1 to 0.2 | 1.5 | 0.0 | 0.0 | 0.0 to 0.1 | <.001 | 0.41 | 0.61 | .008 | 0.58 | 0.66 | |
| Receptive Languageb | 39.5 | 2.2 | 10.1 | 6.2 to 14.1 | 34.1 | 2.3 | 2.8 | −1.2 to 6.8 | — | — | — | — | — | — | |
| Expressive Languagea | 1.6 | 0.0 | 0.1 | 0.1 to 0.2 | 1.5 | 0.0 | 0.1 | 0.0 to 0.1 | <.001 | 0.54 | 0.65 | .61 | 0.18 | 0.55 | |
| Expressive Languageb | 39.0 | 2.2 | 9.0 | 4.7 to 13.3 | 36.2 | 2.2 | 7.5 | 3.3 to 11.8 | — | — | — | — | — | — | |
| Early Learning Composite | 81.7 | 3.3 | 5.9 | 0.2 to 11.6 | 76.2 | 3.4 | 2.1 | −3.7 to −7.9 | .06 | 0.20 | 0.56 | .36 | 0.13 | 0.54 | |
F values for linear mixed model results can be found in the Supplemental Table 3. Estimated marginal means are presented. CI, confidence interval; CLES, Common Language Effect Size; Δ, mean change from baseline to end of intervention; CLES, which is derived from the g effect, represents the likelihood that a randomly selected child from individual-ESI will show greater improvement than a randomly selected child from group-ESI. —, not applicable.
Estimated marginal means, SEs, and linear mixed model results using log transformed variables.
Estimated marginal means and SEs presented using nontransformed variables.
FIGURE 2.
Mean Scores for Individual-ESI and Group-ESI from Baseline to End of 9-Month Intervention Condition.
Social Communication Skills: CSBS
Analyses revealed a significant time × condition interaction effect for the Social Composite with a small effect size. Contrasts indicated that both conditions showed significant improvement, but children in individual-ESI showed significantly greater improvement. Significant main effects of time without significant interaction effects were found for Speech and Symbolic Composites, indicating that both conditions showed similar rates of improvement. However, the current study cannot determine whether improvements in speech and symbolic skills resulted from treatment effects or maturation.
Autism Symptoms: ADOS
Analyses revealed significant main effects of time without significant interaction effects for SA and RRB domain scores. Children in both conditions showed improvement in SA and worsening on RRB.
Adaptive Behavior: VABS
A significant interaction effect was found on Communication with a medium effect size. Contrasts revealed that children in individual-ESI demonstrated significant improvement, whereas group-ESI showed no change. A significant interaction effect was also found on Daily Living with a medium effect size. Contrasts revealed significant improvement in individual-ESI and no change in group-ESI. A significant interaction effect was also found on Socialization with a medium effect size. Contrasts revealed stability in individual-ESI and a significant decrease in group-ESI. Finally, a significant main effect of time without a significant interaction effect was observed for Motor Skills, as both groups showed decreases in standard scores after intervention compared with baseline. Analyses using raw scores revealed significant increases, indicating that decreases in standard scores were not caused by loss of skills during intervention but by failure to progress, comparable to VABS norms.
Developmental Skills: MSEL
Nonverbal Skills
Analyses revealed no significant main effect of time or interaction effect for Visual Reception, as children in both groups did not gain T scores but did maintain their scores and keep up with normative progress (9-month gain in 9 months) compared with MSEL norms. A significant main time effect without a significant interaction effect was also found for Fine Motor. However, children in both groups demonstrated lower T scores after intervention compared with baseline. Analyses using age equivalents revealed that children showed an increase in age equivalents during intervention. Thus, the observed decrease in Fine Motor T scores was caused by failure to make normative progress rather than loss of skills during intervention.
Verbal Skills
A significant interaction effect was found for Receptive Language with a medium effect size. Contrasts revealed that children in individual-ESI demonstrated significant improvement, whereas group-ESI showed no change during intervention. A significant main effect of time without a significant interaction effect was found for Expressive Language, as children in both conditions demonstrated improvement.
Site and Other Intervention Effects
Given differences between sites on baseline MSEL Visual Reception and Fine Motor, site was examined as a potential threat to validity of treatment effects. However, site was not found to interact with any significant time × condition effects, indicating that the differential effect of individual-ESI did not differ by site for any measures. Children’s participation in other interventions outside ESI was also examined in relation to significant findings and not found to interact with any significant time × condition effects, indicating that other intervention hours did not explain differential efficacy of individual-ESI.
Discussion
This study is the first large RCT to compare two 9-month parent-implemented interventions for toddlers with ASD resulting in significant effects on child outcomes. Group-ESI is similar to other group parent interventions held once per week in a clinic26–28 and contrasts with individual-ESI, which was offered in individual sessions 2 or 3 times per week, with 2 at home. Taken together, these findings support the differential efficacy of individual-ESI on some child outcomes compared with group-ESI. Individual-ESI led to significantly greater improvement on social components of communication and receptive language compared with group-ESI. Individual-ESI also resulted in stability or slight improvements on Daily Living and Socialization, in contrast to the worsening seen in the group-ESI condition. These findings are particularly important given limited main effects of other parent education and parent-implemented interventions on child outcomes for toddlers with ASD. Comparing 2 ESI conditions is a conservative approach to test efficacy, and yet individual-ESI was superior on 6 child outcomes. The young age of these toddlers at baseline may contribute to these novel treatment effects.
Strengths of this study are the use of random assignment with a large 2-site sample using gold standard measures of child outcomes, blind diagnosticians, and standardized observational measures, which are less susceptible to expectation of change than parent report. Comparison of 2 active teaching conditions provides information on differential effects; however, this study cannot rule out alternative explanations such as maturation for improvements found in both conditions. Child improvements in core social deficits and expressive language were observed for parent groups held once a week for 9 months, findings that are in contrast to other briefer interventions that may not have been sufficiently intensive to affect these child outcomes. Teaching parents in individual-ESI at home for an additional 2 sessions per week led to significant effects on early social skills and receptive language and lessened the worsening of adaptive behaviors. Improvements in core social deficits have been demonstrated in only a few other treatment studies.23,24 Although both groups worsened on motor standard scores, it is important to note that motor skills were high at baseline, with the average score within normal limits.
It is possible that the significant effects observed on adaptive behavior, which is a parent report measure, are confounded by parent expectations in that parents participating in individual-ESI were more likely to rate their child’s adaptive behavior highly than parents in group-ESI. However, this limitation is tempered by the significant findings on related constructs assessed by blinded examiner-administered measures (eg, significant effect on VABS Socialization and CSBS Social Composite; VABS Communication and MSEL Receptive Language).
A limitation of this study is that follow-up measures are not available after the 9-month intervention to examine maintenance of effects. Another limitation is that children in both conditions received an active treatment; therefore, maturation cannot be easily separated from intervention effects. However, comparing these outcomes with studies that report longitudinal trajectories for toddlers with ASD and other treatment studies suggests that the expected developmental trajectory is a worsening of standard scores, as seen on motor composites for both MSEL and VABS.30,54–58 Our findings contribute by demonstrating the efficacy of a 9-month low-intensity treatment, which led to increases in social and language skills and some reduction of the expected worsening in developmental trajectory, which may prevent the secondary impact of autism symptoms on intellectual ability.
Important future research directions include performing mediation analysis of the effect of parent change in transactional supports on child outcomes, along with examining characteristics of children who show substantial response to treatment, now that we have demonstrated effects on child outcomes. Additional research is needed to replicate these findings, to examine the effect of the ESI model with younger children and with different combinations or dosage of the 2 conditions, and to document the time needed by Part C service providers to learn the ESI model and effectiveness of community implementation.
Conclusions
Current health care and education systems are challenged to provide intervention of adequate intensity that is shown to be effective for toddlers with ASD. Services delivered by professionals within IDEA Part C average 2 to 3 hours/week.59 ESI incorporates evidence-based active ingredients implemented by parents in natural environments while maintaining professional time comparable to that of current Part C systems, increasing the potential for community viability. The efficacy of individual-ESI compared with group-ESI on many child outcomes is particularly important in light of the lack of main effects on child outcomes of most other parent-implemented interventions with toddlers with ASD. Although there may be a narrow window of time for effectiveness of this approach, the potential to identify children with ASD by 18 to 24 months is within our reach.6,8,60 Availability of community-viable treatments for toddlers with ASD makes the recommendations of the Council on Children with Disabilities3 for collaboration of primary care and Part C systems possible and offers promise for addressing existing health disparities in access to EI.
Supplementary Material
Glossary
- ADOS
Autism Diagnostic Observation Schedule
- ASD
autism spectrum disorder
- CSBS
Communication and Symbolic Behavior Scales
- EI
early intervention
- ESI
Early Social Interaction
- FSU
Florida State University
- IDEA
Individuals With Disabilities Education Act
- MSEL
Mullen Scales of Early Learning
- RCT
randomized controlled trial
- RRB
Restricted, Repetitive Behavior
- SA
Social Affect
- SCERTS
Social Communication, Emotional Regulation, and Transactional Supports
- UM
University of Michigan
- VABS
Vineland Adaptive Behavior Scales
Footnotes
Dr Wetherby conceptualized and designed the study, oversaw implementation at Florida State University, and drafted the manuscript; Ms Guthrie supervised data collection of child measures and conducted statistical analyses; Dr Woods helped conceptualize and implement the intervention model; Dr Schatschneider contributed to the design and oversaw statistical analyses; Ms Holland coordinated training of interventionists across both sites; Dr Morgan supervised data collection of intervention measures; Dr Lord helped conceptualize the study and oversaw implementation at the University of Michigan; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00760812).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by the National Institute of Mental Health grant R01MH077730/R01MH078165 (A.M.W., C.L.) and funding from Autism Speaks (A.M.W., C.L.) and the Simons Foundation (C.L.). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Lord is author of the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2). Dr Lord and Ms Guthrie are authors of the ADOS Toddler Module (ADOS-T). They receive royalties from use of the ADOS-2 and ADOS-T but not from this study. Dr Wetherby receives royalties from use of the Communication and Symbolic Behavior Scales and Social Communication, Emotional Regulation, and Transactional Supports but not from this study. Dr Woods, Dr Schatschneider, Ms Holland, and Dr Morgan have indicated they have no potential conflicts of interest to disclose.
References
- 1.National Research Council Educating Children With Autism. Washington, DC: National Academy Press, Committee on Educational Interventions for Children with Autism, Division of Behavioral and Social Sciences and Education; 2001 [Google Scholar]
- 2.US Government Accountability Office. Special Education: Children With Autism. Report to the Chairman and Ranking Minority Member, Subcommittee on Human Rights and Wellness, Committee on Government Reform, House of Representatives. Washington, DC: US Government Accountability Office
- 3.Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States [published online ahead of print June 9, 2014]. JAMA Pediatr. 2014;168(8):721–728. 10.1001/jamapediatrics.2014.210 [DOI] [PubMed] [Google Scholar]
- 4.Adams R, Tapia C, The Council on Children With Disabilities. Early intervention, IDEA Part C services, and the medical home: collaboration with best practice and best outcome. Pediatrics. 2013;132(4). Available at: www.pediatrics.org/cgi/content/full/132/4/e1073 [DOI] [PubMed] [Google Scholar]
- 5.Johnson CP, Myers SM, American Academy of Pediatrics Council on Children With Disabilities . Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183–1215 [DOI] [PubMed] [Google Scholar]
- 6.Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age. Arch Gen Psychiatry. 2006;63(6):694–701 [DOI] [PubMed] [Google Scholar]
- 7.Guthrie W, Swineford LB, Nottke C, Wetherby AM. Early diagnosis of autism spectrum disorder: stability and change in clinical diagnosis and symptom presentation. J Child Psychol Psychiatry. 2013;54(5):582–590. 10.1111/jcpp.12008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wetherby AM, Brosnan-Maddox S, Peace V, Newton L. Validation of the Infant–Toddler Checklist as a broadband screener for autism spectrum disorders from 9 to 24 months of age. Autism. 2008;12(5):487–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baio J, Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators, Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders - Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012:6(3):1–19 [PubMed] [Google Scholar]
- 10.Mandell DS, Novak MM, Zubritsky CD. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics. 2005;116(6):1480–1486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mandell DS, Listerud J, Levy SE, Pinto-Martin JA. Race differences in the age at diagnosis among Medicaid-eligible children with autism. J Am Acad Child Adolesc Psychiatry. 2002;41(12):1447–1453 [DOI] [PubMed] [Google Scholar]
- 12.Maglione MA, Gans D, Das L, Timbie J, Kasari C, Technical Expert Panel. HRSA Autism Intervention Research–Behavioral (AIR-B) Network . Nonmedical interventions for children with ASD: recommended guidelines and further research needs. Pediatrics. 2012;130(suppl 2):S169–S178 [DOI] [PubMed] [Google Scholar]
- 13.Warren Z, McPheeters ML, Sathe N, Foss-Feig JH, Glasser A, Veenstra-Vanderweele J. A systematic review of early intensive intervention for autism spectrum disorders. Pediatrics. 2011;127(5). Available at: www.pediatrics.org/cgi/content/full/127/5/e1303 [DOI] [PubMed] [Google Scholar]
- 14.Mundy P, Burnette C. Joint attention and neurodevelopmental models of autism. In: Volkmar FR, Paul R, Klin AJ, Cohen D, eds. Handbook of Autism and Pervasive Developmental Disorders. 3rd ed. New York, NY: Wiley; 2005:650–681 [Google Scholar]
- 15.Dawson G, Bernier R, Ring RH. Social attention: a possible early indicator of efficacy in autism clinical trials. J Neurodev Disord. 2012;4(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wetherby AM, Watt N, Morgan L, Shumway S. Social communication profiles of children with autism spectrum disorders late in the second year of life. J Autism Dev Disord. 2007;37(5):960–975 [DOI] [PubMed] [Google Scholar]
- 17.Yoder P, Stone WL. Randomized comparison of two communication interventions for preschoolers with autism spectrum disorders. J Consult Clin Psychol. 2006;74(3):426–435 [DOI] [PubMed] [Google Scholar]
- 18.Kasari C, Freeman S, Paparella T. Joint attention and symbolic play in young children with autism: a randomized controlled intervention study. J Child Psychol Psychiatry. 2006;47(6):611–620 [DOI] [PubMed] [Google Scholar]
- 19.Smith T, Groen AD, Wynn JW. Randomized trial of intensive early intervention for children with pervasive developmental disorder. Am J Ment Retard. 2000;105(4):269–285 [DOI] [PubMed] [Google Scholar]
- 20.Dawson G, Rogers S, Munson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125(1). Available at: www.pediatrics.org/cgi/content/full/125/1/e17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kasari C, Paparella T, Freeman S, Jahromi LB. Language outcome in autism: randomized comparison of joint attention and play interventions. J Consult Clin Psychol. 2008;76(1):125–137 [DOI] [PubMed] [Google Scholar]
- 22.Kasari C, Gulsrud AC, Wong C, Kwon S, Locke J. Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. J Autism Dev Disord. 2010;40(9):1045–1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aldred C, Green J, Adams C. A new social communication intervention for children with autism: pilot randomised controlled treatment study suggesting effectiveness. J Child Psychol Psychiatry. 2004;45(8):1420–1430 [DOI] [PubMed] [Google Scholar]
- 24.Landa RJ, Kalb LG. Long-term outcomes of toddlers with autism spectrum disorders exposed to short-term intervention. Pediatrics. 2012;130(suppl 2):S186–S190 [DOI] [PubMed] [Google Scholar]
- 25.Landa RJ, Holman KC, O’Neill AH, Stuart EA. Intervention targeting development of socially synchronous engagement in toddlers with autism spectrum disorder: a randomized controlled trial. J Child Psychol Psychiatry. 2011;52(1):13–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carter AS, Messinger DS, Stone WL, Celimli S, Nahmias AS, Yoder P. A randomized controlled trial of Hanen’s “More Than Words” in toddlers with early autism symptoms. J Child Psychol Psychiatry. 2011;52(7):741–752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Green J, Charman T, McConachie H, et al. PACT Consortium . Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet. 2010;375(9732):2152–2160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rogers SJ, Estes A, Lord C, et al. Effects of a brief Early Start Denver model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2012;51(10):1052–1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siller M, Hutman T, Sigman M. A parent-mediated intervention to increase responsive parental behaviors and child communication in children with ASD: a randomized clinical trial. J Autism Dev Disord. 2013;43(3):540–555. 10.1007/s10803-012-1584-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lord C, Luyster R, Guthrie W, Pickles A. Patterns of developmental trajectories in toddlers with autism spectrum disorder. J Consult Clin Psychol. 2012;80(3):477–489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson DK, Oti RS, Lord C, Welch K. Patterns of growth in adaptive social abilities among children with autism spectrum disorders. J Abnorm Child Psychol. 2009;37(7):1019–1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boyd BA, Odom SL, Humphreys BP, Sam AM. Infants and toddlers with autism spectrum disorder: early identification and early intervention. J Early Interv. 2010;32(2):75–98 [Google Scholar]
- 33.Dingfelder HE, Mandell DS. Bridging the research-to-practice gap in autism intervention: an application of diffusion of innovation theory. J Autism Dev Disord. 2011;41(5):597–609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schertz HH, Baker C, Hurwitz S, Benner L. Principles of early intervention reflected in toddler research in autism spectrum disorders. Top Early Child Spec Educ. 2010;31(1):4–21 [Google Scholar]
- 35.Schwartz IS, Sandall SR. Is autism the disability that breaks Part C? A commentary on “Infants and toddlers with autism spectrum disorder: Early identification and early intervention,” by Boyd, Odom, Humphreys, and Sam. J Early Interv. 2010;32(2):105–109 [Google Scholar]
- 36.Wetherby AM, Woods JJ. Early Social Interaction Project for children beginning in the second year of life: a preliminary study. Top Early Child Spec Educ. 2006;26(2):67–83 [Google Scholar]
- 37.Wetherby AM, Prizant BM. Communication and Symbolic Behavior Scales: Developmental Profile: Normed Edition. Baltimore, MD: Paul H. Brooks Publishing; 2002 [Google Scholar]
- 38.Lord C, Rutter ML, DiLavore PS, Risi S. Autism Diagnostic Observation Schedule–Generic. Los Angeles, CA: Western Psychological Services; 1999 [Google Scholar]
- 39.Luyster R, Gotham K, Guthrie W, et al. The Autism Diagnostic Observation Schedule–Toddler Module: a new module of a standardized diagnostic measure for autism spectrum disorders. J Autism Dev Disord. 2009;39(9):1305–1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lord C, Luyster R, Gotham K, Guthrie W. Autism Diagnostic Observation Schedule–Toddler Module. Los Angeles, CA: Western Psychological Services; 2012 [Google Scholar]
- 41.Charman T, Baird G. Practitioner review: diagnosis of autism spectrum disorder in 2- and 3-year-old children. J Child Psychol Psychiatry. 2002;43(3):289–305 [DOI] [PubMed] [Google Scholar]
- 42.Volkmar F, Chawarska K, Klin A. Autism in infancy and early childhood. Annu Rev Psychol. 2005;56:315–336 [DOI] [PubMed] [Google Scholar]
- 43.Prizant BM, Wetherby AM, Rubin E, Laurent AC. The SCERTS Model: A transactional, family-centered approach to enhancing communication and socioemotional abilities of children with autism spectrum disorder. Infants Young Child. 2003;16(4):296–316 [Google Scholar]
- 44.Prizant BM, Wetherby AM, Rubin E, Laurent AC, Rydell PJ. The SCERTS Model: A Comprehensive Educational Approach for Children With Autism Spectrum Disorders. Baltimore, MD: Brookes Publishing; 2006 [Google Scholar]
- 45.Wetherby A, Goldstein H, Cleary J, Allen L, Kublin K. Early identification of children with communication disorders: concurrent and predictive validity of the CSBS Developmental Profile. Infants Young Child. 2003;16(2):161–174 [Google Scholar]
- 46.Wetherby AM, Allen L, Cleary J, Kublin K, Goldstein H. Validity and reliability of the communication and symbolic behavior scales developmental profile with very young children. J Speech Lang Hear Res. 2002;45(6):1202–1218 [DOI] [PubMed] [Google Scholar]
- 47.Gotham K, Risi S, Pickles A, Lord C. The Autism Diagnostic Observation Schedule: revised algorithms for improved diagnostic validity. J Autism Dev Disord. 2007;37(4):613–627 [DOI] [PubMed] [Google Scholar]
- 48.Sparrow S, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. 2nd ed. Circle Pines, MN: American Guidance Services; 2005 [Google Scholar]
- 49.Mullen EM. Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Services; 1995 [Google Scholar]
- 50.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin; 2002 [Google Scholar]
- 51.Braucht GN, Reichardt CS. A computerized approach to trickle-process, random assignment. Eval Rev. 1993;17(1):79–90 [Google Scholar]
- 52.Maxwell SE, Delaney HD. Designing Experiments and Analyzing Data: A Model Comparison Perspective. New York, NY: Psychology Press; 2004 [Google Scholar]
- 53.Sullivan JR, Winter SM, Sass DA, Svenkerud N. Assessing growth in young children: A comparison of raw, age-equivalent, and standard scores using the Peabody Picture Vocabulary Test. J Res Child Educ. 2014;28(2):277–291 [Google Scholar]
- 54.Lloyd M, MacDonald M, Lord C. Motor skills of toddlers with autism spectrum disorders. Autism. 2013;17(2):133–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Venker CE, Ray-Subramanian CE, Bolt DM, Ellis Weismer S. Trajectories of autism severity in early childhood. J Autism Dev Disord. 2014;44(3):546–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ozonoff S, Iosif AM, Baguio F, et al. A prospective study of the emergence of early behavioral signs of autism. J Am Acad Child Adolesc Psychiatry. 2010;49(3):256–266, e1–e2 [PMC free article] [PubMed] [Google Scholar]
- 57.Bryson SE, Zwaigenbaum L, Brian J, et al. A prospective case series of high-risk infants who developed autism. J Autism Dev Disord. 2007;37(1):12–24 [DOI] [PubMed] [Google Scholar]
- 58.Landa RJ, Holman KC, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Arch Gen Psychiatry. 2007;64(7):853–864 [DOI] [PubMed] [Google Scholar]
- 59.Hebbeler K, Spiker D, Bailey D, et al. Early Intervention for Infants and Toddlers With Disabilities and Their Families: Participants, Services, and Outcomes. Menlo Park, CA: SRI International; 2007 [Google Scholar]
- 60.Chlebowski C, Robins DL, Barton ML, Fein D. Large-scale use of the modified checklist for autism in low-risk toddlers. Pediatrics. 2013;131(4). Available at: www.pediatrics.org/cgi/content/full/131/4/e1121 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.