Introduction
Hospital readmissions following surgical procedures are disruptive for patients and their families and correlates with poor outcomes including reoperation or death. Whereas readmissions following hospitalization for acute medical conditions have been the subject of ongoing research and policy initiatives for many years, readmissions have received less attention in the surgical specialties. This is remarkable given the frequency of surgery in this country, the overall cost of surgical care, and the perceived association between surgical readmission and quality of care.(1–3)
Moreover, the health care costs associated with readmissions are substantial. Unplanned readmissions have an economic impact estimated at $17.4 billion per year.(1) Although debatable, a significant portion of hospital readmissions may be preventable.(2,4) Consequently, in 2010, the Patient Protection and Affordable Care Act was passed which contained legislation mandating a national readmissions reduction program.(5) Shortly thereafter, the Centers for Medicare and Medicaid Services (CMS) developed and implemented policies to penalize readmission.(6) Specifically, these penalties reduce reimbursement to hospitals with higher-than-expected readmission rates. These penalties have been already implemented for three medical diagnoses: congestive heart failure, myocardial infarction, and pneumonia, and will be expanded to the surgical procedures including hip and knee arthroplasty beginning in 2015.(6)
Comprehensive reviews have addressed global aspects of readmission or readmission of patients following medical hospitalization. However, there are no systematic reviews that address surgical readmissions. In a review of interventions aimed to reduce medical readmissions, Hansen et al concluded that no single intervention was consistently associated with a reduced risk, but did note that certain components (e.g. post discharge telephone call) were common to successful bundled interventions.(7) Kansagara et al performed a systematic review of risk prediction models for readmission and determined that current models perform poorly, concluding that efforts are needed to improve their performance, including measures of patient’s social support and detailed clinical data.(8) These analyses help underscore the need for research in surgical readmissions since: (1) there is no synthesis of the current literature describing surgical readmission, (2) medical readmissions are fundamentally different from surgical readmissions, and (3) there are no proven models for predicting or preventing surgical readmissions.
In this review, recent studies of readmission within the surgical subspecialties of vascular, general, bariatric, and colorectal surgery are analyzed. Readmission rates and diagnoses as well as predictors of readmission are examined within these surgical fields to help create a foundation for future research that will ultimately improve the quality of surgical care.
Methods
Study Identification
We performed a search via PubMed using the search terms surgery AND intitle: readmission OR intitle: readmissions OR intitle: rehospitalization. The search was limited to January 1, 2009 through July 1, 2013. Two independent reviewers (JW, AG) examined all citations and abstracts, noting inclusion and exclusion criteria to determine study eligibility. Once articles were selected, the reference lists from these articles were reviewed to identify any additional qualifying studies.
Study Inclusion and Exclusion Criteria
For a study to be included we required that it contain at least one of the following analyses: (1) readmission diagnoses or (2) multivariable analysis of factors predicting readmission. Only English language articles were included. Articles were excluded if they evaluated (1) only planned readmissions or (2) readmissions to a facility other than a hospital (e.g. readmission to the intensive care unit). Meta-analyses were excluded if they contained a majority of articles that were selected for inclusion in this review.(9) In order to characterize procedures common to a general and vascular surgical practice, we selected articles pertaining to vascular, general, bariatric, and colorectal surgery. We defined general surgery as bariatric, colorectal, abdominal procedures involving the stomach, small bowel, appendix, and gallbladder as well as thyroid and hernia procedures. Articles that focused on other surgical specialties including cardiac, orthopedic/spine, plastic and reconstructive surgery, pediatric surgery, trauma and transplant were excluded. There is an extensive literature that addresses readmission following pancreaticoduodenectomy and complex pancreatic surgery; because of the focused and specialized nature of these procedures, we excluded these studies.
Data Review and Synthesis
We performed a systematic review because our initial analysis of eligible studies suggested a high degree of heterogeneity, making a meta-analysis impractical. Outcomes of interest were readmission rate, diagnoses upon readmission, predictors of readmission, and short and long term mortality of readmitted patients. Readmission rates are reported as percentages and, when possible, weighted averages were performed. Diagnoses that led to readmission were extracted from each article; we recorded the top 3 most frequent diagnoses for each. Predictors of readmission were reported as significant in multivariable regression modeling by having a p-value of < 0.05. Non-significant predictors of readmission were also reported. For each study we recorded the data source, sample size, study methodology, definition of the readmission window (e.g. 30-days, 60-days, following surgery, following discharge), procedural type, and any interventions attempted to reduce readmissions. Findings for vascular, general, bariatric, and colorectal surgery were summarized separately, followed by an analysis of overall trends and differences.
Results
Search Results
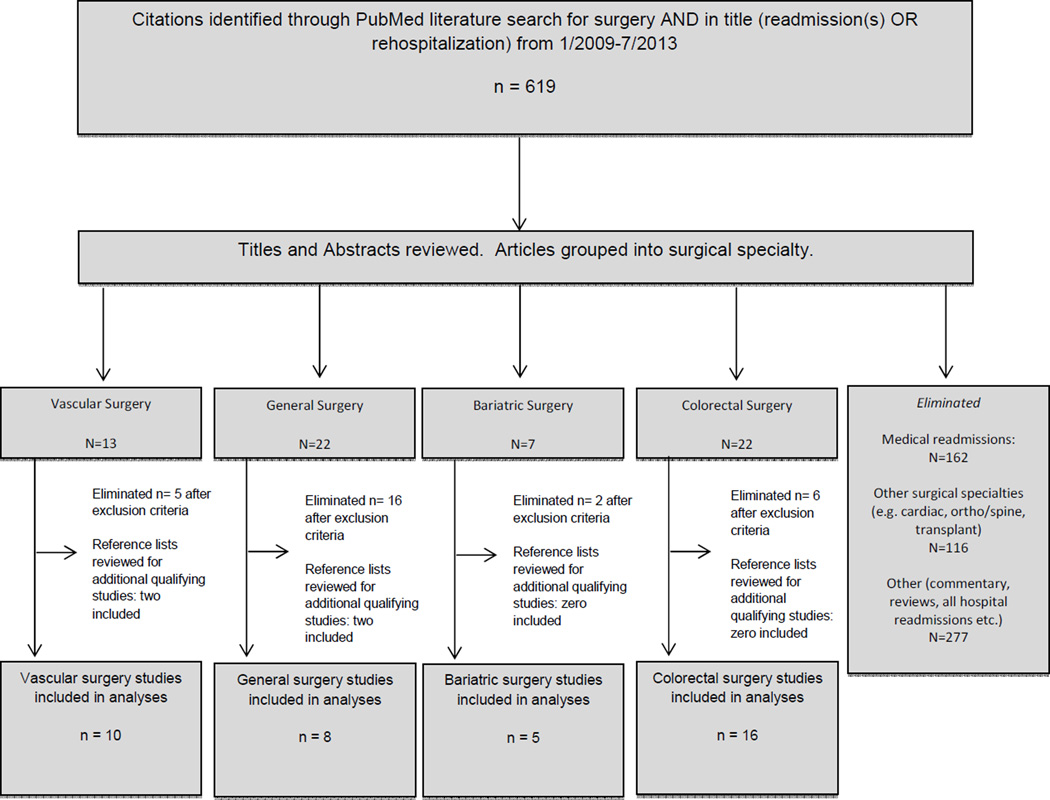
A total of 619 citations were identified using the described search criteria. The number of citations increased yearly. After reviewing all article titles and abstracts, 555 were excluded based on the aforementioned criteria, leaving a total of 64 articles for review (Figure 1). The full text of the remaining articles was then reviewed, followed by the elimination of an additional 29 articles using same criteria, with 35 remaining. The literature cited in these 35 articles was also reviewed searching for additional relevant articles resulting in the addition of 4 articles.(10–13) The final yield was a total of 39 articles included in this review.(10–48) The resulting articles were then categorized by surgical specialty: vascular surgery (n=10), (10,11,14–21) general surgery (n=8), (12,13,22–27) bariatric surgery (n=5) (28–32) and colorectal surgery (n=16). (33– 48)
Figure 1.
Study selection process from initial PubMed search results of January 2009 to July 2013.
Study Characteristics
Data included in these articles were derived prospectively and retrospectively from a variety of sources with the distribution as follows: Single institutional (n=20), Medicare (n=8), State registry (n=2), American College of Surgeons National Surgical Quality Improvement Program(49) (ACS-NSQIP; a clinically validated, multicenter data set) (n=2), a National Patient Registry (n=2), proprietary insurance-based claims (n=1), multi-institution registry (n=1), the Health Facts database (n=1), the Bariatrics Outcomes Longitudinal Database (n=1), and the Hospital Episodes Statistics Database (n=1).
Readmission rates
Overall, readmission rates were reported in 39 (100%) studies. Readmission rates were reported at 28-days,(39) 30-days,(11,13–24,27–38,40,42–47) 6-weeks,(26) 60-days,(30,48) 90-days,(12,18,25,30,34) 6-months,(10) 1-year,(18,33) 2-years(26) and >2-years.(26) In one article interval to readmission was not defined.(41) Readmissions were characterized in the majority of studies from the time of discharge (n=24, 62%). Alternatively, in a number of articles readmission was calculated from the time of procedure (n=12, 31%). In 3 articles (8%) the starting point for the readmission period was not defined. The reported overall 30-day readmission rates (for those studies that reported a 30-day period) ranged from 3.7 to 32.5%.
Subgroup analysis by specialty yielded varying medians and ranges of 30-day readmission rates. The median vascular surgery readmission rate was 18.5% (n=9, range: [8.9,24.4%]). Respective 30-day median readmission rates within vascular surgery varied with the procedure as follows: abdominal aneurysm repair 15.8% (n=4, range: [12.5,23.2%]);(15,17,18,21)and lower extremity revascularizations 23% (n=3, range: [14.5,24.4%]).(11,19,20) The general surgery median readmission rate was 9.7% (n=5, range: [5.3,12.1%]). Within general surgery, the readmission rates were variable, even for like procedures. For example, patients undergoing ventral hernia repair had rates of 5.3%,(13) 5.6%,(27) and 12.1%.(22). Patients undergoing laparoscopic cholecystectomy experienced readmission rates of 4.3% at 1-year in one study,(26) compared to 4.3% at 90-days in another.(12) The bariatric surgery median readmission rate was 6.8% (n=5, range [3.7 to 9.3%]). All patients within the bariatric surgery group were treated with roux-en-y gastric bypass (versus band or duodenal switch). The colorectal surgery median readmission rate was 12.8% (n=13, range: [8.3,32.5%]). In two studies, 30-day readmission rates were quite high; specifically in patients that underwent ileal-anal pouch anastomosis (30.3%)(44) or creation of an ileostomy (32.5%).(47) With these two studies removed, the median readmission rate for colorectal was 12.0%.
Mortality of readmitted patients
Although overall mortality was reported in 18 studies, amongst these, only 4 studies reported mortality rates for readmitted versus non-readmitted patients.(10,15,35,36) Greenblatt and colleagues demonstrated a significant association between readmission and one-year mortality in Medicare beneficiaries undergoing colectomy for cancer (the predicted probability of one-year mortality was 16.3% for readmitted patients, compared to 7.4% for those not readmitted). Greenblatt and colleagues also showed a similar disparity in a parallel study evaluating Medicare beneficiaries undergoing abdominal aortic aneurysm repair (the unadjusted one-year mortality rate in readmitted patients was 23.4%, compared to 4.5% in those who were not readmitted). The association of readmission and mortality was found by Schneider and colleagues to persist for as long as three years; patients with a diagnosis of primary colorectal cancer treated with colectomy and readmitted within 30 days of discharge had less favorable long-term survival (47.5% compared to 61.7% for patients who did not require readmission).
Readmission Diagnoses
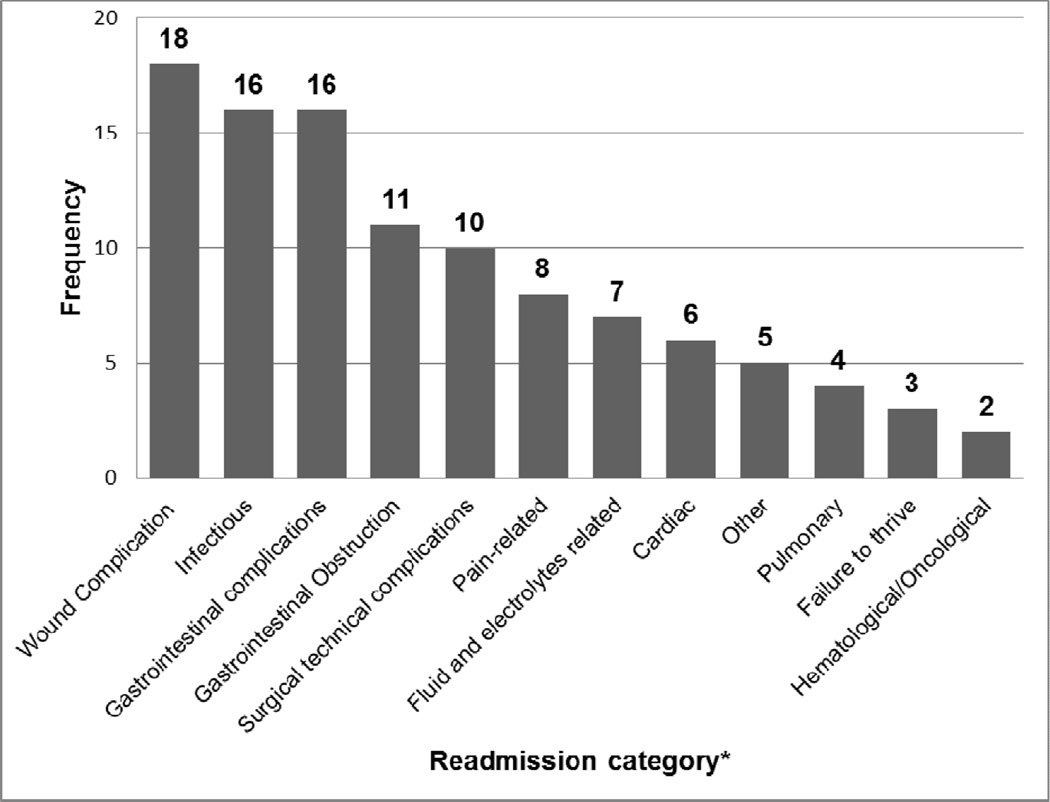
There were 31 studies where diagnoses leading to readmission along with their incidence were reported. Comparison of these findings was hindered by the considerable variability in the definition and categorization of these diagnoses (e.g. wound complication in one study versus wound infection in another). The three most frequent diagnoses were collected for each study and reported in Tables 1–4. These readmission diagnoses were then combined for all reported specialties and presented in Figure 2.
Table 1.
Summary of Vascular Surgery Articles
| First author |
n | Data source |
Study characteristics | Readmission, % | Mortality of readmitted patients, % |
Top 3 readmission diagnoses |
Significant predictors of readmission on multivariate analysis |
|---|---|---|---|---|---|---|---|
| Gioia (10) | < 1000 | Institutional | Patients who underwent AAA repair at a tertiary care center between 1998 and 2000 |
21% @ 6 mo | 13.6% at 6 mo |
1. Cardiovascular 2. Neoplasms 3. Respiratory |
Diabetes Non-elective AAA repair |
| Brooke (14) |
1000– 10,000 |
Medicare | Patients who were discharged home after elective TEVAR and open repair for nonruptured TAA between 2000 and 2007 |
18% at 30 d for TEVAR 20.2% at 30 d for open TAA 19.7% at 30 d overall |
NR | NR | For TEVAR: Comorbidity score renal failure pulmonary failure Shorter length of stay* For open TAA: Age Comorbidity score Shorter length of stay* |
| Greenblatt (15) |
1000– 10,000 |
Medicare | Patients who underwent elective EVAR and open AAA repair between 2004 and 2006 |
13.3% at 30 d for EVAR 12.8% at 30 d for open AAA repair 13.1% at 30 d overall |
23.4% at 1-y for readmitted 4.5% at 1-y for not readmitted |
For EVAR: 1. Wound complication 2. Pneumonia and Respiratory 3. AAA or graft For open AAA repair: 1. Wound complication 2. GI obstruction 3. Pneumonia and respiratory |
Wound complication Discharge destination Age Renal/Urologic complication History of cancer Congestive Heart Failure Anemia |
| Vogel (11) | 1000– 10,000 |
Health Facts database |
Patients who underwent lower extremity procedures for peripheral arterial disease between 2008 and 2010 |
13.9% at 30 d for open procedures 15.3% at 30 d for endovascular procedures 14.5% at 30 d overall |
NR | NR | Aspartate- aminotransferase level >30 medications ordered and dispensed Length of stay |
| Jackson (16) |
<1000 | Institutional | Patients who were discharged from the vascular surgery service at a tertiary care center between 2008 and 2009 |
8.9% at 30 d overall | NR | 1. Reintervention for bleeding, thrombosis, pseudoaneurysm, nonhealing wound 2. Groin wound complication 3. Minor amputation/wound debridement 3. Infection (urinary tract infection, pneumonia, cellulitis) |
Diabetes |
| Vogel (17) | 1000– 10,000 |
State | Patients who underwent elective EVAR and open AAA repair between 2000 and 2005 |
11.6% at 30 d for EVAR 13.1% at 30 d for open AAA repair 12.5% at 30 d overall |
NR | For EVAR: 1. Cardiac complications 2. Mechanical complications of vascular device 3. Postoperative infection For open AAA repair: 1. Rehabilitation services 2. Cardiac complications 3. Digestive system complications |
NR |
| Casey (18) |
>10,000 | State | Patients who underwent elective EVAR and open AAA repair between 2003 and 2008 |
17.4% at 30 d for EVAR 20.0% at 30 d for open AAA repair 18.5% at 30 d overall 29.7% at 90 d for EVAR 31.3% at 90 d for open AAA repair 55.4% at 1 y for EVAR 52.1% at 1 y for open AAA repair |
NR | For EVAR: 1. Cardiac 2. Infection 3. Device/aneurysm For open AAA repair: 1. Failure to thrive 2. Cardiac 3. Infection |
Sex Age Comorbidity score Insurance type Length of stay Congestive heart failure Hypertension Peripheral vascular disease* Open AAA repair* |
| McPhee (19) |
1000– 10,000 | Multicenter | Patients who underwent lower extremity vein graft bypass for critical limb ischemia between 2001–2003 |
24.4% at 30 d | NR | 1. Wound infection in index leg 2. Additional procedure in index leg 3. Nonvascular reasons |
Sex Smoking Dialysis dependence In-hospital graft event Tissue loss |
| McPhee (20) |
1000– 10,000 |
Institutional | Patients who underwent lower extremity bypasses for occlusive disease between 1995 and 2011 |
23% at 30 d | NR | 1. Wound infection 2. Unrelated medical/surgical 3. Graft related |
Postoperative surgical site infection Postoperative graft failure Postoperative myocardial infarction Current dialysis Tissue loss Congestive heart failure Distal inflow source |
| Vogel (21) | >10,000 | Medicare | Patients who underwent elective aortic, iliac, or visceral vascular procedures between 2005 and 2007 |
21.5% at 30 d for patients who did not development a postoperative infection during index hospitalization 33.7% at 30 d for patients who did develop a postoperative infection during index hospitalization 23.2% at 30 d overall |
NR | NR | Infection Race Sex |
Protective against readmission on multivariate analysis.
EVAR, endovascular abdominal aortic aneurysm repair; NR, not reported; TAA, thoracic aortic aneurysms; TEVAR, thoracic endovascular aneurysm repair.
Table 4.
Summary of Colorectal Surgery Articles
| First author |
n | Data source | Study characteristics | Readmission, % | Mortality of readmitted patients, % |
Top 3 readmission diagnoses |
Significant predictors of readmission on multivariate analysis |
|---|---|---|---|---|---|---|---|
| White (33) | <1000 | Institutional | Patients with Crohn's disease who underwent abdominal surgery between 2002 and 2006 |
8.3% at 30 d | NR | 1. Intra-abdominal abscess 2. Small bowel obstruction 3. Enterocutaneous fistula |
NR |
| Wick (34) | >10,000 | Insurance administrative claims database |
Patient who underwent colon and/or rectal resection between 2002 and 2008 |
11.4% at 30 d 23.3% at 90 d |
NR | 1. Gastrointestinal complication 2. Surgical-site infection related 3. Reoperation |
Surgical-site infection during index admission Proctectomy or colectomy Ostomy created index operation Discharge disposition to nonhome setting Length of stay Severity of illness Admission diagnosis of diverticulitis (vs. colon cancer)* |
| Greenblatt (35) |
>10,000 | SEER Medicare | Patients >65 y old with colon cancer who underwent colectomy between 1992 and 2002 |
11% at 30 d | 7.4% at 1 y for non- readmitted patients 16.3% at 1 y for readmitted patients |
1. Ileus, obstruction, and other gastrointestinal complications 2. Surgical-site infection 3. Pneumonia and other respiratory complications |
Sex Race SEER registry state Hospitalized in year before surgery Hierarchical Condition Categories score Tumor grade Emergent admission Year of surgery Length of stay Blood transfusion Stoma creation In-hospital complication Discharge destination Hospital procedure volume* |
| Schneider (36) |
>10,000 | SEER Medicare | Patients >65 y old with colorectal cancer who underwent colorectal surgery between 1986 and 2005 |
11.2% at 30 d | 52.5% at 3- years for readmitted patients 38.3% at 3- years for non- readmitted patients |
1. Operative complications 2. Dehydration 3. Postoperative infections |
Age Discharge year Length of stay Comorbidity score Postoperative complication Transfusion during index admission Primary rectal procedure Sex* |
| Toneva (37) |
1000– 10,000 |
National Veterans Affairs Surgical Quality Improvement Program |
Patients who underwent elective colorectal resections between 2005 and 2009 |
14.2% at 30 d | NR | NR | Procedure: total colectomy, rectal resection (vs. partial colectomy) Ostomy supplies American Society of Anesthesiologists class Oral antibiotic preparation (vs. no preparation)* |
| Abarca (38) |
<1000 | Institutional | Patients who underwent laparoscopic colectomy between 2004 and 2009 |
12.8% at 30 d | NR | 1. Nausea/vomiting 2. Wound infection 3. Pain (abdominal/rectal) |
NR |
| Faiz (39) | >10,000 | Hospital Episode Statistics database |
Patients who underwent elective colorectal resections for malignancy between 1996 and 2006 |
8.5% at 28 d | NR | NR | Procedure: colorectal resection beyond proximal colonic resection Benign diagnosis Sex Carstairs deprivation score Hospital volume Age* |
| Gu (40) | <1000 | Institutional | Patients who underwent laparoscopic total abdominal colectomy with end ileostomy for severe ulcerative colitis or indeterminate colitis between 1998 and 2010 |
17.2% at 30 d | NR | 1. Small bowel obstruction 1. Distal stump leak 3. Wound infection |
NR |
| Gash (41) | <1000 | Institutional | Patients who underwent laparoscopic colorectal resection with primary anastomosis discharged within 3-days of surgery between 2004 and 2009 |
4% | NR | 1. Anastomotic leak 1. Abscess 1. Ileus |
NR |
| Lidor (42) | >10,000 | Medicare | Patients >65 y old with diverticulitis that underwent left colon resection, colostomy, or ileostomy between 2004 and 2007 |
21.4% at 30 d for initial emergent/urgent surgery 11.9% at 30 d for initial elective surgery 17.2% at 30 d overall |
NR | NR | Emergent/Urgent surgery (vs. elective) Age Comorbidity scale Race |
| Hendren (43) |
>10,000 | Medicare | Patients >65 y old with colon cancer who underwent colectomy between 2003 and 2008 |
15.8% at 30 d | NR | NR | Late discharge Age Gender Race Emergent admission Peptic ulcer disease Paralysis Renal failure Psychoses Congestive heart failure Coagulopathy Diabetes with chronic complications Lymphoma Liver disease Rheumatoid arthritis/collagen vascular disease Myocardial infarction complication Renal failure complication Pulmonary failure complication Thromboembolic event complication Surgical site infection Hemorrhage complication Pneumonia complication Gastrointestinal hemorrhage complication Early discharge* High socioeconomic status* Laparoscopic surgery (vs. open)* |
| Datta (44) | <10000 | Institutional | Patients who underwent ileal pouch-anal anastomosis between 2000 and 2005 |
30.3% at 30 d | NR | 1. Small bowel obstruction 2. Pelvic sepsis / anastomotic leak 3. Dehydration |
Perioperative steroid use |
| Ozturk (45) |
1000– 10,000 |
Institutional | Patients who underwent ileal pouch-anal anastomosis between 1984 and 2008 |
12.0% at 30 d | NR | 1. Ileus, obstruction 2. Dyselectrolytemia 3. Surgical site infection |
Comorbid conditions Laparoscopic technique (vs. open) Synchronous proctocolectomy and ileal pouch–anal anastomosis Postoperative blood transfusion |
| Krpata (46) |
<1000 | Institutional | Patients who underwent laparoscopic or open abdominal colorectal surgery between 2007 and 2011 |
10.4% at 30 d | NR | 1. Ileus/obstruction 2. Anastomotic leak/pelvic collection 2. Surgical site infection 2. intra-abdominal abscess |
NR |
| Nagle (47) | < 1000 | Institutional | Patients who underwent creation of a new permanent or temporary ileostomy in 2011 |
35.4% at 30 d prepathway 21.4% at 30 d postpathway 32.5% at 30 d overall |
NR | 1. Dehydration 2. Infection 3. Small bowel obstruction/ileus |
|
| Messaris (48) |
< 1000 | Institutional | Patients who underwent a colon and/or rectal resection with a diverting ileostomy between 1990 and 2010 |
16.9% at 60 d | NR | 1. Dehydration 2. Infection 3. Gastrointestinal / small bowel obstruction |
Use of perioperative diuretics |
Protective against readmission on multivariate analysis.
NR, not reported.
Figure 2.
Frequency of the top three readmission diagnosis categories across all specialties (n=31 studies). See supplemental digital content in online-only Appendix Table 1 for full definitions of variables.
There was significant commonality amongst surgical readmission diagnoses regardless of specialty. Overall, the top five most frequent readmissions diagnosis groups were: (1) wound-related complication, (2) Infection (not wound), (2) gastrointestinal complication, (4) gastrointestinal obstruction, and (5) surgical technical complications.
Frequently shared readmission diagnoses amongst general, bariatric, and colorectal surgery were gastrointestinal complications. Infections were a common readmission diagnosis for vascular, general, and colorectal surgery. Pain symptoms were frequently reported in the general and bariatric populations. Additionally, subsets of readmission diagnoses were unique to certain surgical specialties. For example, frequently reported readmission diagnoses that clustered in vascular surgery included graft-related complications and cardiac-related complications / exacerbations; a readmission diagnosis of anastomotic leak was frequently reported in colorectal surgery.
Further emphasizing the differences between readmission of surgical and medical patients, by far the most frequent diagnoses leading to readmission of surgical patients were issues related primarily to surgery (wound complications, gastrointestinal obstruction, etc.), rather than medical complications of operation (cardiac, pulmonary, hematological, etc.).
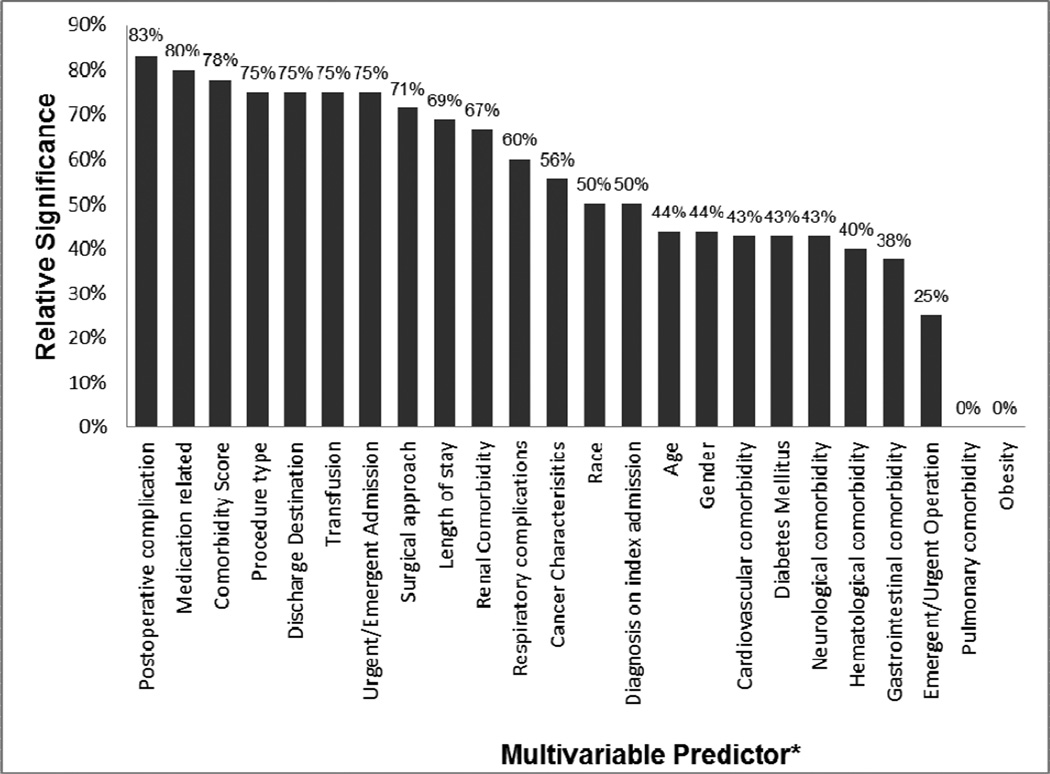
Predictors of Readmission
There were 24 studies (62%) where a multivariable analysis of factors predicting readmission was performed. Comparison of these findings was hindered by the considerable variability in the definition and categorization of readmission predictors. To address this variability, we grouped similar variables into like categories (e.g. open versus laparoscopic and open versus endovascular surgery were grouped into “surgical approach”). Although many variables were evaluated in the majority of studies, some variables were analyzed infrequently. Thus when combining data, we considered only variables that were evaluated in four or more studies. We then calculated the frequency at which a variable was found to be a predictor of readmission using the following formula (the number of studies in which the variable was significant within a multivariable model divided by the number of studies where the variable was evaluated).
Based on the aforementioned approach, the top three predictors of readmission across all studies were: (1) postoperative complication, (2) medication-related (i.e. total number of medications, >30 medications ordered and dispensed, etc.) and (3) comorbidity score (i.e. Charlson index, Hierarchical conditions category score, etc.). Additional frequent predictors of readmission are summarized in Figure 3.
Figure 3.
Multivariable predictors that were included in at least 4 of the 24 articles that reported a multivariable model predicting hospital readmission. The relative significance percentage reflects the number of times the variable was significant within a multivariable model (numerator) divided by the frequency that variable was included in a multivariable model regardless of significance (denominator). See supplemental digital content in online-only Appendix Table 2 for full definitions of variables.
In a separate analysis, we stratified predictors of readmission by patient demographics, patient comorbidities, postoperative complications and perioperative factors. Across specialties, the most frequently reported predictors of readmission amongst patient demographics were age and gender (female gender compare to male being a predictor in 57%). The most frequently reported predictor of readmission amongst patient comorbidities was comorbidity score and the most frequently reported predictor of readmission amongst complications was “any postoperative complication”. The most frequently reported predictor of readmission amongst perioperative factors was length of stay.
Additionally, comorbid conditions that predicted readmission were different between specialties. Congestive heart failure and diabetes predicted readmission among vascular patients, hernia defect size or presence of a fistula predicted readmission in general surgery, the number of medications and depression were predictors for bariatric surgical patients, and comorbidity scores were found to be a significant predictor for readmission of colorectal surgical patients.
Outcomes for cancer patients
Articles focusing on patients with cancer were limited to general and colorectal surgery, with the majority of articles in the latter group.(23,24,34–39,43,45–48) There appeared to be a general trend towards an increased risk of readmission for cancer patients with more progressive disease, but this relationship was not always consistent. Kassin and colleagues evaluated patients with and without cancer undergoing a variety of general surgery procedures and demonstrated that patients with disseminated cancer were at a more than double the risk for readmission compared to those without (p=0.015).(23) Tuggle and colleagues studied thyroid cancer patients and showed that patients with distant cancer stage were at an increased risk for readmission compared to patients with localized cancer (p=<0.001).(24) In contrast, Greenblatt and colleagues showed that there was not a significant difference in odds of readmission for Medicare beneficiaries undergoing colectomy for cancer across cancer stages.(35)
Furthermore, readmission rates for cancer patients were not always higher than their non-cancer cohorts. For example, Wick and colleagues showed significantly higher readmission rates for patients undergoing colorectal surgery for colon cancer compared to diverticulitis, but did not find a difference when compared to inflammatory bowel disease.(34) Also, Toneva and colleagues found a lower readmission rate for cancer patients undergoing colorectal surgery compared to patients with irritable bowel disease, diverticulitis, and other colorectal diagnoses.(37)
Studies exploring risk prediction models or interventions
Out of 39 studies, only one evaluation explicitly generated a risk prediction tool based upon a multivariate analysis of a multi-institution registry data.(19) The authors found a very modest ability (C statistic of 0.60) to discriminate between patients who were and were not readmitted. (For a review of models predicting readmission, see Kansagara, et al.(8)) There was one institutional study by Nagle and colleagues that prospectively instituted an “ileostomy pathway” in order to reduce readmissions and facilitate patient education and well-being.(47) Their group was able to demonstrate a significant decrease in dehydration-related readmissions and a decreasing trend in overall readmissions after implementation of the pathway.
Discussion
Although once controversial, it is now reasonably well accepted that surgical readmission is a marker of quality of hospital care. Emphasizing this point, Tsai and colleagues demonstrated a relationship between surgical readmission rates and adherence to surgical process measures, procedural volume, and procedure-specific 30-day risk-adjusted surgical mortality rates, three established measures of hospital surgical quality.(2) Thus, decreasing the rate of surgical readmission represents an opportunity to improve patient care. Original research on this topic is required to provide surgeons, hospitals, and policymakers with the necessary tools to accomplish this goal. To characterize the body of current literature on surgical readmissions, we reviewed the findings of recent studies within the surgical subspecialties of general, bariatric, colorectal and vascular surgery.
Our review of 39 studies confirms a high rate of hospital readmission within the surgical population.(1,50) In 2009, Jencks et al found 23.9% and 16.6% respective 30-day readmission rates among Medicare beneficiaries for vascular and major bowel surgical procedures. Our summative analysis reveals numbers that are somewhat lower for vascular and colorectal surgery. The slightly higher readmission rates reported by Jencks and colleagues are likely reflective of sampling from an exclusively Medicare population, representing older patients with a greater frequency of comorbidities, and also Medicare’s ability to track readmissions to non- index hospitals. Nevertheless, our review suggests that readmission rates are high across surgical populations and are not isolated to older patient cohorts.
Our findings revealed two themes with regard to readmission diagnoses: (1) several diagnoses were common across all surgical specialties (e.g. wound and gastrointestinal complications) (2) Other diagnoses were common to their respective surgical specialties (e.g. graft related complications in vascular and anastomotic leak in colorectal). The former may benefit from system-wide changes that address all surgical patients. For example, outpatient monitoring of wounds prior to the traditional 2 to 3-week follow up appointment might be generalizable and reduce the rate of readmission for wound complications for all surgical specialties. However, diagnoses that are specific to individual surgical specialties may require focused strategies or protocols that are service specific. For example, a vascular service may institute a graft monitoring protocol where bypass grafts are scanned before hospital discharge to identify potential issues that might lead to early occlusion. Continuing to define the frequency of specific readmission diagnoses will help focus efforts to reduce their incidence.
One of the issues that we encountered was the tremendous variability in defining and categorizing readmission diagnoses. For example, in some studies a category was created for wound infections whereas in others, the category was wound complications and in still others there was a more general category for infections (including pneumonia and urinary tract infection). This observation emphasizes the importance of creating standard groupings of readmission diagnoses so that studies can be compared and more importantly the data derived from these studies can be used to inform targeted interventions that might prevent specific complications.
Better understanding the predictors of readmission is also a key component in efforts to stem preventable readmissions. We found that reliable predictors of readmission included postoperative complications, medication-related issues, comorbidity, and postoperative length of stay. Identification of the predictors of readmission can reveal which patients are vulnerable and inform strategies to reduce readmission. For example, patients that have prolonged length of stay might be targeted with interventions at the time of discharge that address the issues that lead to readmission (e.g. more rapid follow-up, better outpatient management of hospital derived complications, etc.). Patient comorbidities that predict rehospitalization (which are known prior to the initial hospitalization) can be used to develop targeted strategies that can be employed in this patient cohort prior to elective surgery.
Nonetheless, the relationship between post-operative length of stay and readmission is complex. One might predict that shorter length of stay would be associated with a higher rate of readmission with the presumption that patients are being discharged too early before their care is complete, resulting in a return to the hospital. However, we found just the opposite. Increased postoperative length of stay in multivariate analysis was a predictor of readmission in 69% of reporting studies. The likely reason for this finding is that prolonged length of stay is associated in many cases with the development of a postoperative complication. This then selects a group of patients that are prone to complications and likely to develop additional post-discharge issues. Or alternatively these patients are discharged before their complication has completely resolved. Or another possibility is that discharge efforts designed to care for the complication are not adequate, leading to readmission.(15,34,35) Conversely, if surgery and the postoperative course are uneventful, one might anticipate a relatively short length of stay and no readmission.
The relationship between length of stay and readmission does appear to be specific to the type of surgery. Baker and colleagues compared laparoscopic to open distal pancreatectomy with a focus on readmission, and found that the laparoscopic approach was associated with a shorter initial length of stay, but a higher rate of readmission compared to the open approach.(51) Baker’s findings underscore the complicated relationship between the occurrence of complications and readmission. For procedures that have very short lengths of stay, the patient may be discharged before the complication can occur. Thus, for minimally invasive operations with short lengths of stay, there is the need for readmission for almost any postoperative complication. In any event, minimally invasive procedures are the exception and the data are overwhelmingly conclusive that increased length of stay is associated with an increased rate of readmission.
An important finding of the reported studies was the association between readmission and mortality. The mortality difference between readmitted and non-readmitted patients was evident at one year in vascular and colorectal patients(15,35) and up to three years in colorectal patients.(36)There are two possible explanations for this finding. The association between mortality and readmission could potentially arise from the fact that readmission has “selected” a cohort of patients who are inherently more likely to die; readmission is a marker of those with poor longevity. This theory suggests that readmission in these patients is not preventable and likely the consequence of predetermined disease.(35) An alternative hypothesis is that readmissions, as well as the complications that lead to readmission, are preventable. Moreover, if these complications are prevented, the enhanced mortality in the readmitted cohort could be markedly diminished. The latter hypothesis presents a more optimistic view of these patients and suggests that interventions to prevent readmission might have a substantial impact on overall patient mortality. Thus, the truth likely lies somewhere in between. Our assessment after review of these multiple studies is that overall mortality in surgical patients can be favorably affected by interventions to reduce readmission; this of course remains to be proven.
Patients undergoing surgery for cancer may have inferior outcomes than matched non-cancer patients, particularly if undergoing chemotherapy (adjuvant or neoadjuvant). However, contrary to this notion, Greenblatt and colleagues showed no association between receiving chemotherapy within 30-days of discharge and increased risk of readmission.(35) The risk of having cancer may commonly be manifested in an increased risk of mortality as opposed to readmission, but we are unable to make firm conclusions to support this given the mixed results within the respective articles. Further studies identifying the impact of cancer and the effects of adjuvant and neoadjuvant therapies on readmissions are warranted.
In attempting to synthesize studies of surgical readmissions we have become readily cognizant of the lack of uniformity and standardization of the data. Unfortunately, the current literature contains a significant amount of heterogeneity across studies with regard to reporting standards. The major sources of this heterogeneity are (1) the utilization of varying data sources (e.g. Medicare versus institutional records, versus multicenter registries), (2) substantial differences in the definition of readmission (e.g. 30-day versus 60- or 90-day), and lastly, (3) differing definitions of important variables (e.g. wound infections versus all infections, congestive heart failure versus all cardiovascular complications). This heterogeneity is problematic when attempting to glean patterns and trends in surgical readmissions.
More important than variability in the data sets, is the fact that the working definition for readmission varies significantly, as do definitions of the important variables. Time-to-readmission is typically reported either from the date of hospital discharge or the surgical procedure. This variability is likely data driven. In ACS NSQIP readmission was prospectively defined as within 30 days of the primary procedure; it is impossible with NSQIP to determine readmission from the date of discharge. Alternatively CMS has made the decision to calculate readmission from the date of hospital discharge. This lack of standardization makes comparison of results problematic. There is currently no initiative underway to create research reporting standards around readmission, although uniform definitions would significantly improve consensus and cross-study comparisons.
Readmissions can be planned and these patients need to be excluded from both analysis and penalty. Depending on the data source utilized, classification of a “planned readmission” can be a difficult task. This is reflected in the existing literature. Jencks and colleagues estimate that 10% of readmissions for both medical and surgical Medicare beneficiaries are planned whereas Jackson and colleagues estimated a 25% planned readmission rate in vascular surgery patients.(1,16) Attempts have been made to address this issue; an algorithm has been developed that uses pre- procedural codes and discharge diagnoses categories to identify planned readmissions.(52) Removing planned readmissions from these analyses will enhance the findings of studies focused on identifying factors that can prevent readmission.
Of the 39 studies we examined, we found only one that produced and validated a risk prediction model for surgical readmissions.(19) The development of an accurate readmission risk prediction algorithm has the potential to improve surgical quality by serving two purposes: (1) to identify patients that are at “high risk” and would likely benefit from an intervention, such as a transitional-care program, and (2) to facilitate the calculation of risk-adjusted readmission rates that allow inter-hospital comparisons. To the former, interventions designed to prevent readmission are often costly and thus cannot be broadly applied to all patients. Optimally, these resources should be devoted to a smaller subset of patients where the impact might be most significant. Out of the 39 articles we reviewed, in only one was a pathway instituted prevent readmission.(47) The majority of trialed models have only been tested or employed for medical or combined medical/surgical patients.(7,53,54) Transitional care models with demonstrated effectiveness in medical patients will need to be adapted for the surgical population.
We excluded patients undergoing pancreaticoduodenectomy because these patients present unique challenges both pre- and postoperatively owing to the indications for surgery and the complexity of the operation. Patients undergoing pancreaticoduodenectomy have high 30-day readmission rates ranging from approximately 10 to 20%.(55–61) The driver of these high rates is likely the incidence of complications, with published ranges from 30 to 60%.(62,63) These readmission rates are comparatively higher than our reported general surgery readmission rates and are more similar to our colorectal surgery readmission rates. Given the greater development of this literature and distinct patient population, separate summative analysis of this distinctive cohort is warranted.
There are important limitations to our study. The majority of articles we summarized were published in 2009 or later to ensure that our review is relevant to the previous 10 years of practice. This seemed appropriate considering that the emphasis on readmission is relatively recent; for prior years the focus was on early discharge, not readmission. This research summary does not include other common surgical specialties including cardiac, thoracic, or orthopedic surgery. Therefore, any expansion of our conclusions to the entire surgical population should be guarded. Predictors of readmission were sampled from individual multivariable analyses; each which was controlled for a different set of confounding variables limiting our ability to blend predictors across specialties. Mortality of readmitted patients is only reported in a small sample of studies, which may limit the validity of our conclusions. Finally, the study was retrospective and summarizes aggregated findings, which may introduce bias.
Overall, hospital readmissions following surgery are disruptive for patients and their families, are a significant cost to the payers of healthcare, and represent lesser quality of patient care. Thus, there are multiple reasons for improving our understanding of surgical readmissions. This review represents the growing body of surgical readmission literature cultivated by an ever-increasing interest in this field by surgeons. A great deal of knowledge regarding surgical readmissions already exists, which we have summarized within. However, future efforts should focus on standardizing definitions for readmission and reporting criteria, designing prediction models for surgical patients and ultimately the important task of creating interventions that reduce the morbidity and mortality of these patients and further improve the quality of surgical care.
Supplementary Material
Table 2.
Summary of General Surgery Articles
| First author |
n | Data source | Study characteristics | Readmission % |
Mortality of readmitted patients, % |
Top 3 readmission diagnoses |
Significant predictors of readmission on multivariate analysis |
|---|---|---|---|---|---|---|---|
| Blatnik (22) | < 1000 | Institutional | Patients who underwent open or laparoscopic ventral hernia repair between 2005 and 2010 |
12.1% at 30 d | NR | 1. Wound infection 2. Gastrointestinal 3. Hematologic 3. Cardiac |
Open repair (vs. laparoscopic) Active abdominal infection Hernia defect size Presence of a fistula |
| Kassin (23) | 1000– 10,000 |
NSQIP single hospital |
Patients who underwent many different inpatient general surgery procedures between 2009 and 2011 |
11.3% at 30 d | NR | 1. Gastrointestinal complication 2. Surgical Infection 3. Failure to thrive / malnutrition |
Postoperative complication Procedure performed |
| Tuggle (24) | 1000– 10,000 |
SEER- Medicare |
Patients older than 65 with thyroid cancer who underwent thyroidectomy between 1997 and 2002 |
8% at 30 d | NR | NR | Comorbidity scale Stage: distant Length of stay Complication during index stay Hospital size: large* Post discharge physician visit* |
| Martin (25) | < 1000 | Institutional | Patients who underwent a variety of open or laparoscopic abdominal general surgery procedures between 2009 and 2010 |
27.1% at 90 d | NR | 1. Dehydration 2. Obstruction / Ileus 3. Abdominal abscess |
NR |
| Down (12) | < 1000 | Institutional | Patients who underwent elective or emergent laparoscopic cholecystectomy between 2006 and 2007 |
4.3% at 90 d | NR | 1. Abdominal pain 2. Wound infection 2. Retained common bile duct stone |
NR |
| Bisgaard (13) |
1000– 10,000 |
National Patient Registry |
Patients older than 18 who underwent umbilical or epigastric hernia repair between 2005 and 2006 |
5.3% at 30 d | NR | 1. Wound related problems / complications 2. Seroma 3. Pain with negative clinical finding |
NR |
| Sanjay (26) | 1000– 10,000 |
Institutional | Patients who underwent elective laparoscopic cholecystectomy without intraoperative cholangiogram between 2002 and 2007 |
2.8% at 6 wk 4.3% at 1 y 5.7% at 2 y 6.4% at >2 y |
NR | 1. Non-specific abdominal pain 2. Obstructive jaundice 3. Peptic ulcer disease |
NR |
| Helgstrand (27) |
1,000– 10,000 |
National Patient Registry |
Patients older than 18 who underwent elective ventral hernia repair in 2008 |
5.6% at 30 d | NR | 1. Wound dehiscence or deep wound infection 2. Miscellaneous 3. Pain |
NR |
Protective against readmission on multivariate analysis.
NR, not reported.
Table 3.
Summary of Bariatric Surgery Articles
| First author |
n | Data source | Study characteristics | Readmission % |
Mortality of readmitted patients, % |
Top 3 readmission diagnoses | Significant predictors of readmission on multivariate analysis |
|---|---|---|---|---|---|---|---|
| Moon (28) |
<1000 | Institutional | Patients who underwent roux-en-y gastric bypass with gastrostomy tube placement between 2008 and 2010 |
3.7% at 30 d | NR | 1. Abdominal pain 2. Nausea/vomiting 3. Gastrostomy tube related complications |
NR |
| Dorman (29) |
>10,000 | Bariatric Outcomes Longitudinal Database |
Patients who underwent roux-en-y gastric bypass between 2007 and 2009 |
5.8% at 30 d | NR | 1. Nausea/Vomiting 2. Dehydration 3. Gastrointestinal bleeding |
Race No. of medications Open surgical approach (vs. laparoscopic) Length of stay Cholelithiasis Depression Psychosocial impairment Pseudotumor cerebri Alcohol use* |
| Kellogg (30) |
1000– 10,000 |
Institutional | Patients who underwent roux-en-y gastric bypass between 2004 and 2007 |
6.8% at 30 d 10.9% at 60 d 13.4% at 90 d |
NR | 1. Nausea/vomiting/dehydration 2. Abdominal pain 3. Wound issues |
NR |
| Hong (31) |
<1000 | Institutional | Patients who underwent roux-en-y gastric bypass between 2002 and 2008 |
9.3% at 30 d | NR | 1. Technical complications 1. Malaise 3. Benign abdominal pain 3. Nausea/Vomiting/dehydration |
NR |
| Dallal (32) |
1000– 10,000 |
Institutional | Patients who underwent roux-en-y gastric bypass between 2006 and 2010 |
7.5% at 30 d | NR | 1. Abdominal pain and/or vomiting 2. Other causes 3. Gastrointestinal bleeding |
Length of stay |
Protective against readmission on multivariate analysis
NR, not reported.
Acknowledgments
Source of Funding: Dr Wiseman is supported by the National Institutes of Health T32 University of Wisconsin Research Training in Vascular Surgery grant HL110853. Dr Saunders is supported by the National Institutes of Health T32 University of Wisconsin Research Training in Vascular Surgery grant HL110853.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N. Engl. J. Med. 2009 Apr 2;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Tsai TC, Joynt KE, Orav EJ, et al. Variation in surgical-readmission rates and quality of hospital care. N. Engl. J. Med. 2013 Sep 19;369(12):1134–1142. doi: 10.1056/NEJMsa1303118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. [cited 2013 Sep 1];FastStats - Inpatient Surgery [Internet] 2013 Available from: http://www.cdc.gov/nchs/fastats/insurg.htm.
- 4.Frankl SE, Breeling JL, Goldman L. Preventability of Emergent Hospital Readmission. Am. J. Med. 1991 Jun;90(6):667–674. [PubMed] [Google Scholar]
- 5.Patient Protection and Affordable Care Act. Public Law 111 – 148 111th Congress. 2010:1–906. [Google Scholar]
- 6. [cited 2013 Sep 15];Centers for Medicare & Medicaid Services Readmissions Reduction Program [Internet] 2013 Available from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- 7.Hansen L, Young R. Interventions to Reduce 30-Day Rehospitalization: A Systematic Review. Ann. Intern. Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 8.Kansagara D, Englander H, Salanitro A, Kagen D, et al. Risk Prediction Models for Hospital Readmission: A Systematic Review. J. Am. Med. Assoc. 2011;306(15):1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li LT, Mills WL, White DL, et al. Causes and Prevalence of Unplanned Readmissions After Colorectal Surgery: a Systematic Review and Meta-Analysis. J. Am. Geriatr. Soc. 2013 Jul;61(7):1175–1181. doi: 10.1111/jgs.12307. [DOI] [PubMed] [Google Scholar]
- 10.Gioia LC, Filion KB, Haider S, et al. Hospital Readmissions Following Abdominal Aortic Aneurysm Repair. Ann. Vasc. Surg. 2005 Jan;19(1):35–41. doi: 10.1007/s10016-004-0132-4. [DOI] [PubMed] [Google Scholar]
- 11.Vogel TR, Kruse RL. Risk Factors for Readmission after Lower Extremity Procedures for Peripheral Artery Disease. J. Vasc. Surg. Society for Vascular Surgery. 2013 Jul;58(1):90–97. doi: 10.1016/j.jvs.2012.12.031. e4. [DOI] [PubMed] [Google Scholar]
- 12.Down SK, Nicolic M, Abdulkarim H, et al. Low ninety-day re-admission rates after emergency and elective laparoscopic cholecystectomy in a district general hospital. Ann. R. Coll. Surg. Engl. 2010 May;92(4):307–310. doi: 10.1308/003588410X12664192075053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bisgaard T, Kehlet H, Bay-Nielsen M, et al. A nationwide study on readmission, morbidity, and mortality after umbilical and epigastric hernia repair. Hernia. 2011;15:541–546. doi: 10.1007/s10029-011-0823-z. [DOI] [PubMed] [Google Scholar]
- 14.Brooke BS, Goodney PP, Powell RJ, et al. Early discharge does not increase readmission or mortality after high-risk vascular surgery. J. Vasc. Surg. 2013 Mar;57(3):734–740. doi: 10.1016/j.jvs.2012.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greenblatt DY, Greenberg CC, Kind AJH, et al. Causes and implications of readmission after abdominal aortic aneurysm repair. Ann. Surg. 2012;256(4):595–605. doi: 10.1097/SLA.0b013e31826b4bfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jackson BM, Nathan DP, Doctor L, et al. Low rehospitalization rate for vascular surgery patients. J. Vasc. Surg. 2011 Sep;54(3):767–772. doi: 10.1016/j.jvs.2011.03.255. [DOI] [PubMed] [Google Scholar]
- 17.Vogel T, Symons R, Flum D. Longitudinal outcomes after endovascular repair of abdominal aortic aneurysms. Vasc. Endovascular Surg. 2008;42(5):412–419. doi: 10.1177/1538574408316143. [DOI] [PubMed] [Google Scholar]
- 18.Casey K, Hernandez-Boussard T, Mell MW, Lee JT. Differences in readmissions after open repair versus endovascular aneurysm repair. J. Vasc. Surg. 2013 Jan;57(1):89–95. doi: 10.1016/j.jvs.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McPhee JT, Nguyen LL, Ho KJ, et al. Risk prediction of 30-day readmission after infrainguinal bypass for critical limb ischemia. J. Vasc. Surg. Society for Vascular Surgery. 2013 Jun;57(6):1481–1488. doi: 10.1016/j.jvs.2012.11.074. [DOI] [PubMed] [Google Scholar]
- 20.McPhee JT, Barshes NR, Ho KJ, et al. Predictive factors of 30-day unplanned readmission after lower extremity bypass. J. Vasc. Surg. Society for Vascular Surgery. 2013 Apr;57(4):955–962. doi: 10.1016/j.jvs.2012.09.077. [DOI] [PubMed] [Google Scholar]
- 21.Vogel TR, Dombrovskiy VY, Lowry SF. Impact of Infectious Complications After Elective Surgery on Hospital Readmission and Late Deaths in the U.S Medicare Population. Surg. Infect. 2012 Oct;13(5):307–311. doi: 10.1089/sur.2012.116. [DOI] [PubMed] [Google Scholar]
- 22.Blatnik JA, Harth KC, Aeder MI, Rosen MJ. Thirty-day readmission after ventral hernia repair: predictable or preventable? Surg. Endosc. 2011 May;25(5):1446–1451. doi: 10.1007/s00464-010-1412-4. [DOI] [PubMed] [Google Scholar]
- 23.Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. J. Am. Coll. Surg. 2012 Sep;215(3):322–330. doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tuggle CT, Park LS, Roman S, et al. Rehospitalization among elderly patients with thyroid cancer after thyroidectomy are prevalent and costly. Ann. Surg. Oncol. 2010 Nov;17(11):2816–2823. doi: 10.1245/s10434-010-1144-7. [DOI] [PubMed] [Google Scholar]
- 25.Martin RCG, Brown R, Puffer L, et al. Readmission Rates After Abdominal Surgery. Ann. Surg. 2011 Oct;254(4):591–597. doi: 10.1097/sla.0b013e3182300a38. [DOI] [PubMed] [Google Scholar]
- 26.Sanjay P, Weerakoon R, Shaikh IA, et al. A 5-year analysis of readmissions following elective laparoscopic cholecystectomy - cohort study. Int. J. Surg. 2011 Jan;9(1):52–54. doi: 10.1016/j.ijsu.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 27.Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T. Nationwide analysis of prolonged hospital stay and readmission after elective ventral hernia repair. Dan. Med. Bull. 2011 Oct;58(10):A4322. [PubMed] [Google Scholar]
- 28.Moon R, Teixeira A, Potenza K, Jawad MA. Routine gastrostomy tube placement in gastric bypass patients: impact on length of stay and 30-day readmission rate. Obes. Surg. 2013 Feb;23(2):216–221. doi: 10.1007/s11695-012-0835-5. [DOI] [PubMed] [Google Scholar]
- 29.Dorman RB, Miller CJ, Leslie DB, et al. Risk for hospital readmission following bariatric surgery. PLoS One. 2012 Jan;7(3):e32506. doi: 10.1371/journal.pone.0032506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kellogg TA, Swan T, Leslie DA, et al. Patterns of readmission and reoperation within 90 days after Roux-en-Y gastric bypass. Surg. Obes. Relat. Dis. American Society for Metabolic and Bariatric Surgery. 2009;5(4):416–423. doi: 10.1016/j.soard.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 31.Hong B, Stanley E, Reinhardt S, Panther K, et al. Factors associated with readmission after laparoscopic gastric bypass surgery. Surg. Obes. Relat. Dis. 2012;8(6):691–695. doi: 10.1016/j.soard.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 32.Dallal RM, Trang A. Analysis of perioperative outcomes, length of hospital stay, and readmission rate after gastric bypass. Surg. Endosc. 2012 Mar;26(3):754–758. doi: 10.1007/s00464-011-1947-z. [DOI] [PubMed] [Google Scholar]
- 33.White EC, Melmed GY, Vasiliauskas E, et al. Does preoperative immunosuppression influence unplanned hospital readmission after surgery in patients with Crohn’s disease? Dis. Colon Rectum. 2012 May;55(5):563–568. doi: 10.1097/DCR.0b013e3182468961. [DOI] [PubMed] [Google Scholar]
- 34.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis. Colon Rectum. 2011 Dec;54(12):1475–1479. doi: 10.1097/DCR.0b013e31822ff8f0. [DOI] [PubMed] [Google Scholar]
- 35.Greenblatt DY, Weber SM, O’Connor ES, et al. Readmission after colectomy for cancer predicts one-year mortality. Ann. Surg. 2010;251(4):659–669. doi: 10.1097/SLA.0b013e3181d3d27c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schneider EB, Hyder O, Brooke BS, et al. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J. Am. Coll. Surg. 2012 Apr;214(4):390–398. doi: 10.1016/j.jamcollsurg.2011.12.025. discussion 398–9. [DOI] [PubMed] [Google Scholar]
- 37.Toneva GD, Deierhoi RJ, Morris M, et al. Oral antibiotic bowel preparation reduces length of stay and readmissions after colorectal surgery. J. Am. Coll. Surg. American College of Surgeons. 2013 Apr;216(4):756–762. doi: 10.1016/j.jamcollsurg.2012.12.039. discussion 762–3. [DOI] [PubMed] [Google Scholar]
- 38.Abarca F, Saclarides TJ, Brand MI. Laparoscopic colectomy: complications causing reoperation or emergency room/hospital readmissions. Am. Surg. 2011 Jan;77(1):65–69. [PubMed] [Google Scholar]
- 39.Faiz O, Haji A, Burns E, et al. Hospital stay amongst patients undergoing major elective colorectal surgery: predicting prolonged stay and readmissions in NHS hospitals. Colorectal Dis. 2011 Jul;13(7):816–822. doi: 10.1111/j.1463-1318.2010.02277.x. [DOI] [PubMed] [Google Scholar]
- 40.Gu J, Stocchi L, Remzi F, Kiran RP. Factors associated with postoperative morbidity, reoperation and readmission rates after laparoscopic total abdominal colectomy for ulcerative colitis. Colorectal Dis. 2013 Sep;15(9):1123–1129. doi: 10.1111/codi.12267. [DOI] [PubMed] [Google Scholar]
- 41.Gash K, Greenslade G, Dixon A. Enhanced recovery after laparoscopic colorectal resection with primary anastomosis: accelerated discharge is safe and does not give rise to increased readmission rates. Colorectal Dis. 2012 Oct;14(10):1287–1290. doi: 10.1111/j.1463-1318.2012.02969.x. [DOI] [PubMed] [Google Scholar]
- 42.Lidor AO, Schneider E, Segal J, et al. Elective surgery for diverticulitis is associated with high risk of intestinal diversion and hospital readmission in older adults. J. Gastrointest. Surg. 2010 Dec;14(12):1867–1873. doi: 10.1007/s11605-010-1344-2. discussion 1873–4. [DOI] [PubMed] [Google Scholar]
- 43.Hendren S, Morris AM, Zhang W, Dimick J. Early discharge and hospital readmission after colectomy for cancer. Dis. Colon Rectum. 2011 Nov;54(11):1362–1367. doi: 10.1097/DCR.0b013e31822b72d3. [DOI] [PubMed] [Google Scholar]
- 44.Datta I, Buie WD, Maclean AR, Heine JA. Hospital readmission rates after ileal pouch-anal anastomosis. Dis. Colon Rectum. 2009 Jan;52(1):55–58. doi: 10.1007/DCR.0b013e31819724a3. [DOI] [PubMed] [Google Scholar]
- 45.Ozturk E, Kiran RP, Remzi F, Fazio VW. Early readmission after ileoanal pouch surgery. Dis. Colon Rectum. 2009 Nov;52(11):1848–1853. doi: 10.1007/DCR.0b013e3181b15610. [DOI] [PubMed] [Google Scholar]
- 46.Krpata DM, Keller DS, Samia H, Lawrence J, et al. Evaluation of inflammatory markers as predictors of hospital stay and unplanned readmission after colorectal surgery. Pol. Przegl. Chir. 2013 Apr 1;85(4):198–203. doi: 10.2478/pjs-2013-0030. [DOI] [PubMed] [Google Scholar]
- 47.Nagle D, Pare T, Keenan E, et al. Ileostomy pathway virtually eliminates readmissions for dehydration in new ostomates. Dis. Colon Rectum. 2012 Dec;55(12):1266–1272. doi: 10.1097/DCR.0b013e31827080c1. [DOI] [PubMed] [Google Scholar]
- 48.Messaris E, Sehgal R, Deiling S, et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis. Colon Rectum. 2012 Feb;55(2):175–180. doi: 10.1097/DCR.0b013e31823d0ec5. [DOI] [PubMed] [Google Scholar]
- 49. [cited 2014 Apr 4];American College of Surgeons - National Surgical Quality Improvement Program [Internet] Available from: http://site.acsnsqip.org/
- 50.Lawson EH, Hall BL, Louie R, et al. Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann. Surg. 2013 Jul;258(1):10–18. doi: 10.1097/SLA.0b013e31828e3ac3. [DOI] [PubMed] [Google Scholar]
- 51.Baker MS, Bentrem DJ, Ujiki MB, et al. Adding days spent in readmission to the initial postoperative length of stay limits the perceived benefit of laparoscopic distal pancreatectomy when compared with open distal pancreatectomy. Am. J. Surg. 2011 Mar;201(3):295–299. doi: 10.1016/j.amjsurg.2010.09.014. discussion 299–300. [DOI] [PubMed] [Google Scholar]
- 52.Horwitz L, Partovian C, Lin Z, Herrin J. Hospital-Wide (All-Condition) 30-day Risk-Standardized Readmission Measure. 2011:1–59. [Google Scholar]
- 53.Kind AJH, Jensen L, Barczi S, et al. Low-cost transitional care with nurse managers making mostly phone contact with patients cut rehospitalization at a VA hospital. Health Aff. 2012 Dec;31(12):2659–2668. doi: 10.1377/hlthaff.2012.0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coleman EA, Parry C, Chalmers S, Min S. The Care Transitions Intervention Results of a Randomized Controlled Trial. Arch. Intern. Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 55.Grewal SS, McClaine RJ, Schmulewitz N, Alzahrani MA, et al. Factors associated with recidivism following pancreaticoduodenectomy. HPB. 2011 Dec;13(12):869–875. doi: 10.1111/j.1477-2574.2011.00377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Balcom JH, Rattner DW, Warshaw AL, et al. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch. Surg. 2001;136(4):391–398. doi: 10.1001/archsurg.136.4.391. [DOI] [PubMed] [Google Scholar]
- 57.Zhu Z, He J, Wang Y, et al. Multivariable analysis of factors associated with hospital readmission following pancreaticoduodenectomy for malignant diseases. Chin. Med. J. (Engl) 2007;124:1022–1025. [PubMed] [Google Scholar]
- 58.Ahmad SA, Edwards MJ, Sutton JM, et al. Factors influencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1302 patients. Ann. Surg. 2012 Sep;256(3):529–537. doi: 10.1097/SLA.0b013e318265ef0b. [DOI] [PubMed] [Google Scholar]
- 59.Yermilov I, Bentrem D, Sekeris EJ, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann. Surg. Oncol. 2009 Mar;16(3):554–561. doi: 10.1245/s10434-008-0178-6. [DOI] [PubMed] [Google Scholar]
- 60.Kastenberg ZJ, Morton JM, Visser BC, et al. Hospital readmission after a pancreaticoduodenectomy: an emerging quality metric? HPB. 2013 Feb;15(2):142–148. doi: 10.1111/j.1477-2574.2012.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hyder O, Dodson RM, Nathan H, et al. Influence of patient, physician, and hospital factors on 30-day readmission following pancreatoduodenectomy in the United States. JAMA Surg. 2013 Dec;148:1095–1102. doi: 10.1001/jamasurg.2013.2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lin J, Cameron J, Yeo C, et al. Risk factors and outcomes in postpancreaticoduodenectomy pancreaticocutaneous fistula. J. Gastrointest. Surg. 2004;8:951–959. doi: 10.1016/j.gassur.2004.09.044. [DOI] [PubMed] [Google Scholar]
- 63.Emick D, Riall T, Cameron J, et al. Hospital readmission after pancreaticoduodenectomy. J Gastrointes. Surg. 2006;10:1243–1253. doi: 10.1016/j.gassur.2006.08.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.