Summary
Intradiscal oxygen-ozone (O2-O3) chemonucleolysis is a well-known effective treatment for pain caused by protruding disc disease and nerve root compression due to bulging or herniated disc.
The most widely used therapeutic combination is intradiscal injection of an O2-O3 mixture (chemonucleolysis), followed by periradicular injection of O2-O3, steroid and local anaesthetic to enhance the anti-inflammatory and analgesic effect. The treatment is designed to resolve pain and is administered to patients without motor weakness, whereas patients with acute paralysis caused by nerve root compression undergo surgery 24-48h after the onset of neurological deficit.
This paper reports on the efficacy of O2-O3 chemonucleolysis associated with anti-inflammatory foraminal injection in 13 patients with low back pain and cruralgia, low back pain and sciatica and subacute partial motor weakness caused by nerve root compression unresponsive to medical treatment. All patients were managed in conjunction with our colleagues in the Neurosurgery Unit of Bellaria Hospital and the IRCCS Institute of Neurological Sciences, Bologna.
The outcomes obtained are promising: 100% patients had a resolution of motor weakness, while 84.6% had complete pain relief. Our results demonstrate that O2-O3 therapy can be considered a valid treatment option for this category of patients.
Keywords: oxygen-ozone therapy, herniated lumbar disc, nerve root compression, motor weakness, low back pain
Introduction
Low back pain, defined as pain with or without functional limitation in the lumbar spine, affects around 80% of the population at least once in a lifetime, with a prevalence of 38.9% in any one year 3,5. It is one of the leading causes of GP visits and loss of working days, with a major economic and social impact on public health 3,5.
In most cases, the cause of low back pain remains unknown so that only 5-15% of cases can be attributed to a specific recognised cause 8. Among these, the largest percentage of patients present pain due to bulging disc accounting for around 40% in different series 5,23. Low back pain irradiating to the leg is known as lumbocruralgia or lumbosciatalgia depending on the nerve roots involved. Ninety per cent of these cases are caused by herniated and bulging disc.
Myriad therapeutic strategies have been developed in recent years to treat nerve root compression, ranging from conservative options like medical management (paracetamol, steroids, NSAIDs, muscle relaxants, etc.), mini-invasive interventional treatments like nucleolysis (mechanical, laser, heat) and oxygen-ozone (O2-O3) chemonucleolysis, to surgery. The choice of treatment is based on the patient's clinical characteristics: the two main parameters are the severity of the neurological deficit and pain intensity. Medical management is the first option for patients with pain but no major motor weakness. Should patients fail to benefit from conservative treatment, mini-invasive therapy is then prescribed 1,4,7,17,21.
O2-O3 chemonucleolysis is a well-known effective treatment for pain caused by low back pain with sciatica or cruralgia due to nerve root compression with bulging or herniated discs. The most widely used therapeutic combination is intradiscal injection of an O2-O3 mixture (chemonucleolysis), followed by periradicular injection of O2-O3, steroid and local anaesthetic to enhance the anti-inflammatory and analgesic effect 1,2-5,16,20.
Many studies have reported on the therapeutic effects of O2-O3 administration. In cases of nerve root compression, the treatment has led to dehydration of the bulging or herniated disc tissue with an attenuation or disappearance of nerve root compression, an anti-inflammatory effect, enhanced tissue oxygenation and oxidation of algogenic substances 2,3,4,6,9,13,16-18.
The associated periganglionic administration of corticosteroids enhances the anti-inflammatory effect of the ozone injection 2,3,6,22,23.
The treatment offers numerous advantages in being fast, low cost and effective in 70-90% of cases in different series 3,4,5,11,14,16,17,20,22,24. Adverse effects or complications have been estimated at < 0.1% 15,19 and the procedure does not preclude subsequent surgery if required 12,20. For these reasons O2-O3 chemonucleolysis has become increasingly popular in recent years with surgery now confined to the treatment of large herniated discs or patients presenting acute or worsening lower limb weakness with or without neurogenic bladder or sphincter impairment in cauda equina syndrome. However, some patients are referred to interventional neuroradiological or neurosurgical consultation with intermediate clinical symptoms characterized by low back pain irradiating to the leg associated with subacute root nerve paresis but without paralysis or urinary or sphincter impairment. Medical management (cortisone, NSAIDs, vitamin B12 and supplements per os) have proved ineffective. Surgery is not indicated in the acute condition as the motor weakness is partial and subacute. In this study, these patients were assessed by both interventional neuroradiologists and neurosurgeons with a view to administering intradiscal chemonucleolysis associated with periradicular foraminal injection of O2-O3, steroid and local anaesthetic. The plan was to proceed to surgery in the case of treatment failure. This strategy was implemented in 13 patients with subacute partial nerve root motor weakness cause by herniated discs in L3-L4, L4-L5 and L5-S1 failing to respond to three months of conservative cortisone therapy.
Methods and Materials
Between March 2009 and August 2013, 13 patients were recruited: six women and seven men aged between 35 and 81 years, with an average age of 55 years. All patients underwent clinical and radiological assessment by an interventional neuroradiologist. Patients with partial motor weakness were referred for neurosurgical consultation to confirm the deficit. Patients were then placed on the waiting list for surgery awaiting the outcome of percutaneous interventional treatment. Patients underwent O2-O3 chemonucleolysis after the shortest possible time interval.
Selected cases were as follows:
− One patient with L3-L4 herniation (involving L4 territory): lumbocruralgia with paresis of the quadriceps femoris muscle;
− Nine patients with L4-L5 herniation (involving L5 territory): lumbosciatalgia with paresis of the tibialis anterior, extensor hallucis longus and extensor digitorum communis;
− 3 patients with L5-S1 herniation (involving S1 territory): lumbosciatalgia with weakness of the triceps surae.
All patients underwent blood tests and electrocardiogram before the procedure. Percutaneous O2-O3 chemonucleolysis treatment was administered under fluoroscopic guidance 10. Radiological equipment comprised GE Advantage 3D XR 2.0 and Philips Allura Xper FD biplane digital angiography systems. The radiology suite is fitted with equipment and material for anaesthesiological care. Peripheral venous access was obtained in each patient and the injection site was thoroughly disinfected and a sterile field set up before the start of the procedure.
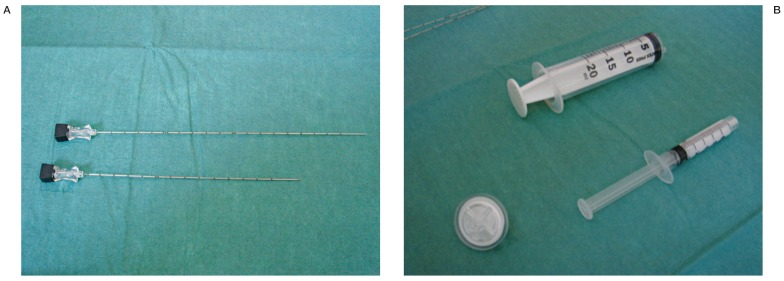
The following material was used during the procedure (Figure 1):
Figure 1.
Materials used: A) 22 G Chiba needles; above: 20 cm needle for puncture in the L5-S1 space; below: 15 cm needle for puncture in the higher spaces L3-L4 and L4-L5. B) 20 ml syringe for O2-O3 injection; filter to eliminate impurities and a 5 ml luer-lock syringe for injection of steroid and local anaesthetic.
1) 22 G chiba needles modified measuring 20 cm for puncture in the L5-S1 space (only one hole in the terminal portion), and 15 cm for puncture in the higher spaces L3-L4 and L4-L5 (three radial holes at 120° in the terminal portion) ;
2) 20 ml syringe for O2-O3 injection;
3) 5 ml luer-lock syringe for injection of steroid and local anaesthetic.
4) filter to eliminate impurities during O2-O3injection.
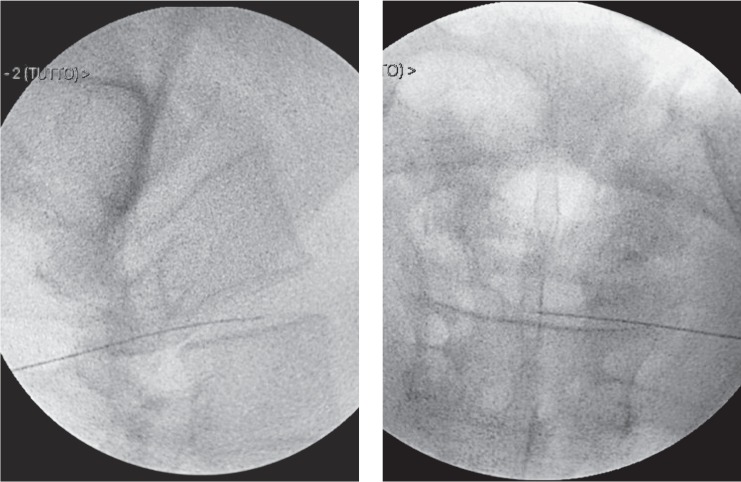
The patient is positioned on the radiology table in a lateral decubitus. The access site is ipsilateral to the site of pain while the access route to the disc is extra-articular postero-lateral. Two standard x-ray views are taken before the procedure to display to disc space to be treated. Then an oblique projection is taken of the facet joint in the direction of the posterior third of the intervertebral space. The skin is pierced making sure the needle tip is inserted slightly anterior to the facet joint (Figure 2). Once the needle is inserted in the muscle the lateral view is resumed and the needle inserted into the disc. Successive antero-posterior and lateral views allow the needle to be correctly positioned within the centre of the disc (Figure 3).
Figure 2.
Oblique view in L4-L5 with the facet joint in the direction of the posterior third of the intervertebral space. The skin is pierced making sure the needle tip is inserted within the virtual rectangle shown.
Figure 3.
Lumbo-sacral spine x-ray in two orthogonal views to display the needle in an intradiscal position.
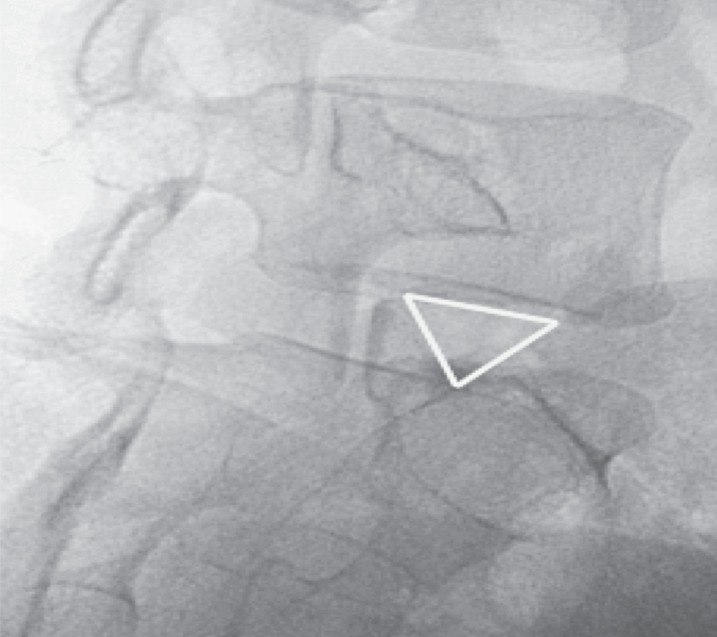
If the L5-S1 disc needs to be punctured, the oblique view differs due to the presence of the iliac wing. In this case, the facet joint is projected to the posterior third of the intervertebral space to obtain a virtual inverted triangle whose sides are composed of the anterior portion of the facet joint posteriorly, the profile of the iliac wing anteriorly and the inferior endplate of L5 superiorly (Figure 4). The needle tip is positioned within the triangle for skin puncture.
Figure 4.
Oblique view in L5-S1 showing the virtual triangle.
An intradiscal injection is made inserting 4 ml of an O2-O3 mixture at a concentration of 27 μg/ml. The needle is then extracted from the disc and positioned in the intervertebral foramen injecting 10 ml of the O2-O3 mixture at the same concentration into the periradicular site. After the gas injection, the needle is left in position for periganglionic injection of 40 mg cortisone associated with 5 mg bupivacaine.
The steroid used in 11 patients was Methylprednisolone acetate, while the remaining two received Triamcinolone acetonide which replaced Methylprednisolone in October 2013. To avoid missing possible contact between needle and nerve root, no local anaesthetic was applied before the start of the procedure. At the end of the treatment patients remain in a lateral position for around 30 minutes, changing to supine decubitus for two to four hours. When no procedure-related problems arise and normal sensitivity has resumed in the anaesthetized nerve root, patients are discharged home in the afternoon of the day of treatment. Patients are instructed to rest in bed at home on the first day after treatment, only getting up for meals and to use the bathroom. On the second day, patients are instructed to rest and only go out for walks after the third day depending on individual clinical conditions. In the two weeks following treatment patients are told not to load the spine and to avoid physical work and public transport.
All patients were reassessed after the procedure at the end of convalescence, two weeks and one month later. Patients reporting only partial pain relief underwent a second treatment session under the same conditions followed by the same post-treatment control visits.
Results
Motor weakness: the following results were obtained after the first treatment (Table 1):
Table 1.
Motor weakness outcome two weeks and one month after O2-O3 treatment.
| 1st TREATMENT |
COMPLETE REMISSION OF MOTOR WEAKNESS |
PARTIAL REMISSION OF MOTOR WEAKNESS |
NO REMISSION OF MOTOR WEAKNESS |
| After 2 weeks | 12/13 | 1/13 | 0/13 |
| After 1 month | 13/13 | 0/13 | 0/13 |
− complete remission in 12 patients;
− partial remission at two-week follow-up and full remission after one month in one patient.
Pain: the following results were obtained after the first treatment (Table 2):
Table 2.
Pain outcome two weeks and one month after O2-O3 treatment.
| 1st TREATMENT |
COMPLETE REMISSION OF PAIN |
PARTIAL REMISSION OF PAIN |
NO REMISSION OF PAIN |
| After 2 weeks | 11/13 | 1/13 | 1/13 |
| After 1 month | 11/13 | 1/13 | 1/13 |
− moderate reduction in 11 patients;
− mild reduction in one patient;
− no significant reduction in one patient.
To achieve complete pain relief, a second treatment was performed between one and three months after the first procedure under the same conditions. Twelve of the 13 patients underwent a second treatment whereas one patient opted for surgery for intolerable pain. As for the first treatment, follow-up controls were carried out at the end of convalescence, two weeks and one month later.
Pain: the following results were obtained after the second treatment (Table 3):
Table 3.
Pain outcome two weeks and one month after O2-O3 treatment.
| 2nd TREATMENT |
COMPLETE REMISSION OF PAIN |
PARTIAL REMISSION OF PAIN |
NO REMISSION OF PAIN |
| After 2 weeks | 11/12 | 1/12 | 0/12 |
| After 1 month | 11/12 | 1/12 | 0/12 |
− complete resolution in 11 patients;
− mild reduction in one patient.
The patient who obtained only a mild attenuation of pain after the second treatment opted for surgery, subsequently gaining pain relief.
In conclusion, after the two O2-O3 treatment sessions all 13 patients had a complete remission of motor weakness, while 84.6% also had a complete remission of pain. Two patients (15.4%) opted for surgery as the reduction of pain after O2-O3 treatment was deemed inadequate (Table 4). No treatment-related complications occurred in our series. Table 5 shows a general summary of our results.
Table 4.
Overall outcome of O2-O3 treatment.
| TREATMENT SUCCESS | TREATMENT FAILURE | |
| Resolution of motor weakness | 100% | 0 |
| Resolution of pain | 84.6% | 15.4% (mild reduction) |
Table 5.
General summary of outcomes for each patient.
| Patients |
Level of herniation |
Nerve root involved |
Remission of neurologic deficit |
Remission of pain |
No. of O2-O3 treatment sessions |
| ♂ | L4-L5 | L5 | + | - | 2 |
| ♀ | L4-L5 | L5 | + | + | 2 |
| ♂ | L5-S1 | L5 | + | + | 2 |
| ♂ | L5-S1 | S1 | + | + | 3 |
| ♂ | L3-L4 | L4 | + | + | 2 |
| ♀ | L4-L5 | L5 | + | + | 2 |
| ♂ | L5-S1 | S1 | + | + | 2 |
| ♀ | L4-L5 | L5 | + | + | 2 |
| ♀ | L4-L5 | L5 | + | + | 2 |
| ♀ | L4-L5 | L5 | + | - | 1 |
| ♀ | L5-S1 | S1 | + | + | 2 |
| ♂ | L4-L5 | L5 | + | + | 2 |
| ♂ | L4-L5 | L5 | + | + | 2 |
Discussion
Percutaneous O2-O3 chemonucleolysis treatment is usually reserved for patients presenting low back pain with or without cruralgia and/or sciatica resistant to conservative management (drugs, physiotherapy or other), persisting for at least three months but without acute neurological motor deficit compatible with documented disc disease 2,3,4,5,12,16. However, in clinical practice patients are commonly encountered with intermediate symptoms characterized by partial motor weakness and severe pain but without paralysis or urinary or sphincter impairment. These patients are difficult to manage as emergency surgery is deemed too invasive for a subacute partial neurologic deficit. At the same time, pain and motor weakness can be extremely invalidating for the patient and often fail to respond to medical management.
The present study aimed to test O2-O3 treatment in this category of patients with herniated disc to establish whether a mini-invasive approach could lead to an improvement in motor weakness and/or pain. This strategy was designed as a first choice antalgic and anti-inflammatory therapy with surgery planned in case of treatment failure. All patients had an excellent outcome with a complete resolution of motor weakness after the first O2-O3 treatment session: remission was complete in 12 patients two weeks after the first procedure, while one patient had a complete remission at the one-month follow-up.
In terms of pain relief, one patient opted for surgery after the first treatment due to intolerable pain. The remaining 12 patients had moderate pain relief and underwent a second session of O2-O3 treatment. After the second treatment 11 patients (84.6%) had an excellent outcome with a complete resolution of pain, whereas one deemed the outcome inadequate and opted for surgery subsequently gaining pain relief.
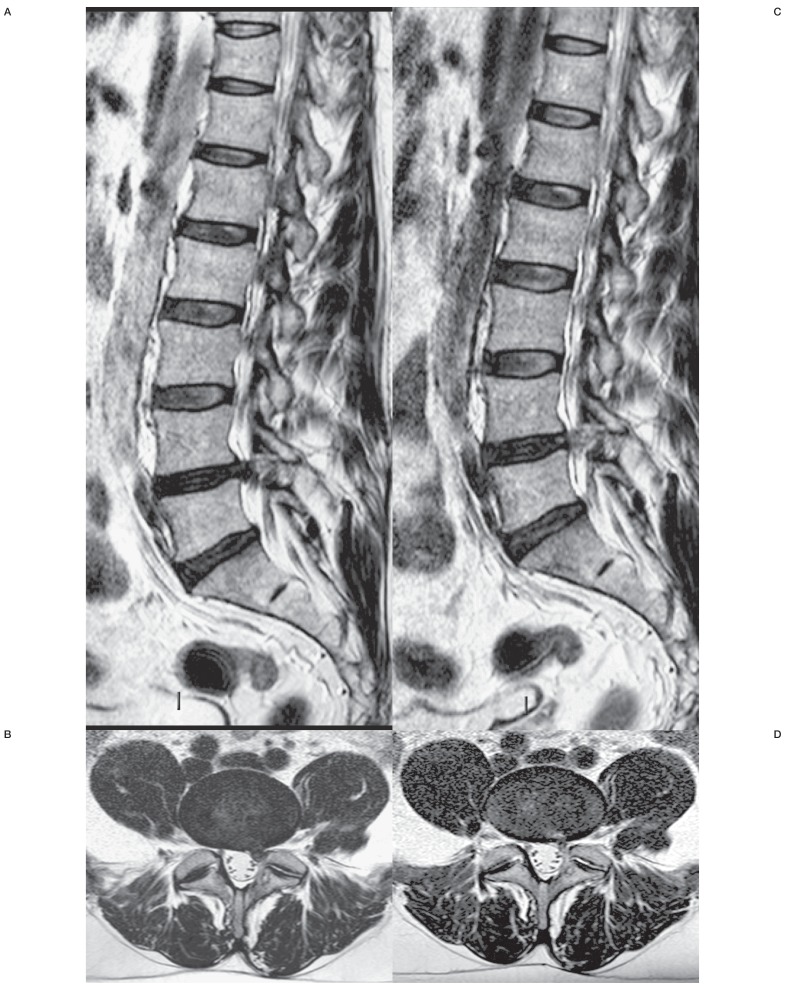
We think the resolution of motor weakness in all our patients was due to the potent anti-inflammatory action of concomitant periganglionic administration of both cortisone and the O2-O3 gas mixture. The anti-inflammatory effect of the treatment is even more apparent considering that all selected patients had previously undergone prolonged medical management with no clinical benefit. Pain relief was accompanied by a shrinkage or disappearance of the bulging herniated disc responsible for nerve root compression (Figure 5).
Figure 5.
MR scans in patients after O2-O3 treatment for recurrent herniated disc. T2-weighted FSE sagittal (A) and axial (B) acquisitions before treatment showing a left L4-L5 postero-lateral herniated disc compressing and displacing the ipsilateral nerve root of L5. T2-weighted FSE sagittal (C) and axial (D) acquisitions 6 months after treatment showing a marked shrinkage of the herniated disc with a disappearance of L5 root compression.
It is important to emphasize that recourse to O2-O3 chemonucleolysis had no impact on subsequent surgical treatment. Close collaboration with the neurosurgery team is therefore essential to optimize the therapeutic regimen of each individual patient.
Conclusions
Intradiscal O2-O3 chemonucleolysis associated with periradicular injection of O2-O3, corticosteroid and local anaesthetic is a consolidated and effective treatment for pain and nerve root compression in patients without motor weakness. Our study showed that O2-O3 chemonucleolysis is equally valid in patients with intermediate symptoms characterized by severe pain associated with subacute partial motor weakness unresponsive to medical management. All patients in our study obtained a resolution of motor weakness, while 84.6% had complete pain relief. Our preliminary findings suggest that O2-O3 chemonucleolysis may be an additional therapeutic option in this category of patients. These promising results await confirmation in future studies on larger patient cohorts.
References
- 1.Andreula C. Percutaneous disc treatments. Neuroradiol J. 2009;22(1):141–143. [Google Scholar]
- 2.Andreula C, Simonetti L, De Santis F, et al. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. Am J Neuroradiol. 2003;24:996–1000. [PMC free article] [PubMed] [Google Scholar]
- 3.Bonetti M, Fontana A, Cotticeli B, et al. Intraforaminal O2-O3 versus periradicular steroidal infiltrations in lower back pain: randomized controlled study. Am J Neuroradiol. 2005;26:996–1000. [PMC free article] [PubMed] [Google Scholar]
- 4.Das G, Ray S, Ishwarari S, et al. Ozone nucleolysis for management of pain and disability in prolapsed lumber intervertebral disc. Interv Neuroradiol. 2009;15:330–334. doi: 10.1177/159101990901500311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Oliveira Magalhaes F, Dotta L, Sasse A, et al. Ozone therapy as a treatment for low back pain secondary to herniated disc: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2012;15:E115–129. [PubMed] [Google Scholar]
- 6.De Santis F, Leonardi M, Simonetti L, et al. Ossigeno-Ozonoterapia: la tecnica intradiscale. International Journal of Ozone Therapy. 2009;8:138–146. [Google Scholar]
- 7.Guarnieri G, Vassallo P, Pezzullo MG, et al. A comparison of minimally invasive techniques in percutaneous treatment of lumbar herniated discs a review. Neuroradiol J. 2009;22(1):108–121. doi: 10.1177/197140090902200116. [DOI] [PubMed] [Google Scholar]
- 8.Hoy D, Brooks P, Blyth F, et al. The epidemiology of low back pain. Best Practice & Research Clinical Rheumatology. 2010;24:769–781. doi: 10.1016/j.berh.2010.10.002. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Iliakis E, Valadakis V. Rationalization of the activity of medical ozone on intervertebral disc: a histological and biochemical study. Rivista di Neuroradiologia. 2001;14(1):23–30. [Google Scholar]
- 10.Leonardi M. La puntura discale sotto fluoroscopia. Rivista Italiana di Ossigeno-Ozonoterapia. 2002;1:73–78. [Google Scholar]
- 11.Leonardi M, Barbara C, Agati R, et al. Percutaneous treatment of herniated lumbar disc by intradiscal injection of ozone mixture. Rivista di Neuroradiologia. 2001;14(1):51–53. [Google Scholar]
- 12.Leonardi M, Albini Riccioli L, Battaglia S, et al. Oxygen-ozone chemonucleolysis for herniated disc with sciatica. A comparison of treatments in patients with subacute and chronic symptoms. Rivista Italiana di Ossigeno-Ozonoterapia. 2006;5:33–36. [Google Scholar]
- 13.Leonardi M, Simonetti L, Barbara C. The effects of ozone on the nucleus pulposus: pathological data on one surgical specimen. Rivista di Neuroradiologia. 2001;14(1):57–59. [Google Scholar]
- 14.Magalhaes FN, Dotta L, Sasse A, et al. Ozone therapy as a treatment for low back pain secondary to herniated disc: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2012;15(2):E115–129. [PubMed] [Google Scholar]
- 15.Muto M, Ambrosanio G, Guarnieri G. Low back pain and sciatica: treatment with intradiscal-intraforaminal O2-O3 injection. Our experience. Radiol Med. 2008;113:695–706. doi: 10.1007/s11547-008-0302-5. doi: 10.1007/s11547-008-0302-5. [DOI] [PubMed] [Google Scholar]
- 16.Muto M, Andreula C, Leonardi M. Treatment of herniated lumbar disc by intradiscal and intraforaminal oxygen-ozone (O2-O3 injection) Journal de Neuroradiologie. 2004;31:183–189. doi: 10.1016/s0150-9861(04)96989-1. doi: 10.1016/S0150-9861(04)96989-1. [DOI] [PubMed] [Google Scholar]
- 17.Muto M, Avella F. Percutaneous treatment of herniated lumbar disc by intradiscal oxygen- ozone injection. Interv Neuroradiol. 1998;4(4):279–286. doi: 10.1177/159101999800400403. [DOI] [PubMed] [Google Scholar]
- 18.Muto M, Steppan J. A meta-analysis of the effectiveness and safety of ozone treatments for herniated lumbar discs. J Vasc Interv Radiol. 2010;21:534–548. doi: 10.1016/j.jvir.2009.12.393. doi: 10.1016/j.jvir.2009.12.393. [DOI] [PubMed] [Google Scholar]
- 19.Pellicanò G, Bonetti M, Muto M, et al. Oxygen-Ozone therapy for herniated disc: analysys of complicances. Neuroradiol J. 2010;23(1):224. [Google Scholar]
- 20.Pellicanò F, Martinetti F, Tavanti V, et al. The Italian Oxygen-Ozone Therapy Federation (FIO) study on oxygen-ozone treatment of herniated disc. International Journal of Ozone Therapy. 2007;6:7–15. [Google Scholar]
- 21.Stagni S, De Santis F, Cirillo L, et al. A Minimally Invasive Treatment for lumbar disc herniation: discoGel Chemonucleolysis in patients unresponsive to Chemonucleolysis with oxygen-ozone. Interv Neuroradiol. 2012;18:97–104. doi: 10.1177/159101991201800113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu L, Li ZL, He XF, et al. Evaluation of the clinical curative effect of an O2-O3 mixture to treat lumbar disc herniation with different treatment sessions. Interv Neuroradiol. 2009;15:159–163. doi: 10.1177/159101990901500204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zennaro H, Dousset V, Viaud B, et al. Periganglionic foraminal steroid injections performed under CT control. Am J Neuroradiol. 1997;19:349–352. [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang Y, Ma Y, Jiang J, et al. Treatment of the lumbar disc herniation with intradiscal and intraforaminal injection of oxygen-ozone. J Back Musculoskelet Rehabil. 2013;26(3):317–322. doi: 10.3233/BMR-130386. [DOI] [PubMed] [Google Scholar]