Summary
We present a percutaneous modified technique to access large thoracic vertebral body lytic lesions, to increase the volume of tumor accessible to ablation, prior to cement augmentation.
Tumor ablation and cavity creation-assisted percutaneous vertebroplasty was considered a palliative measure for structural stabilization in plasmocytoma involvement of the entire T8 vertebral body. Given the extent of osteolysis bilateral combined transpedicular and extrapedicular access to the vertebral body was undertaken to maximize the volume of cavity creation within the tumor.
The combined transpedicular and extrapedicular access was feasible, uncomplicated, and successful in reaching all the quadrants of the anterior two thirds of the vertebral body. Slow, fluoroscopically monitored injection of high-viscosity cement resulted in a successful, desired cement distribution into the anterior two thirds of the vertebral body, spanning superior to inferior endplates, providing structural stability, in the absence of venous or epidural leakage.
The technical modification described in this case yielded positive results while overcoming some of the limitations of the existing coblation device. This approach may offer an option for cement augmentation of extensive vertebral body lytic lesions, at increased risk for tumor displacement and extra-vertebral cement leakage.
Keywords: vertebroplasty, coblation, tumor ablation, spine tumor, plasmocytoma, osteolytic lesion
Introduction
Percutaneous vertebroplasty (PV) is increasingly performed as an adjunct interventional therapy for the treatment of spinal malignancies, to relieve pain and stabilize vertebral bodies at risk of pathologic fracture 1-3. Several authors report positive results using coblation for tumor cavitation prior to cement injection, as this may reduce the risk of both tumor displacement and extra-vertebral cement leakage 4-6.
Coblation is a form of low-temperature radiofrequency, through which plasma ionization causes instantaneous tissue dissolution 7. The coblation device is a rigid electrode with a slightly bent active tip, which is inserted coaxially through a vertebroplasty needle. The controlled plasma field, active at the proximity of the electrode tip, is determined by the orientation of the entry needle. The limitations in reach of the plasma field, coupled with the rigid nature of the wand, determine the amount of tissue that can be ablated in a single setting.
Percutaneous needle access to the thoracic vertebral bodies utilizes either a transpedicular or an extrapedicular approach, allowing access to the superior and inferior aspects of the vertebral body respectively. In large vertebral lytic lesions, the choice of either access may limit the volume of tumor that can be ablated. We present a novel modification of the percutaneous access to the thoracic vertebral body, combining both the transpedicular and extrapedicular bilateral approaches. Using four access paths at a single level substantially increases the volume of tumor accessible to ablation.
Materials and Methods
A 63-year-old man in good health presented with slowly progressive onset of mild mid-thoracic back pain. An MRI revealed a large lesion involving the entire T8 vertebral body, with minimal epidural involvement (Figure 1A-C). CT showed the lesion to be purely lytic, with extensive cortical destruction involving the disc endplates and the posterior vertebral wall (Figure 1D-F). A percutaneous biopsy revealed a plasma-cell tumor. Due to the high risk of vertebral collapse, PV was considered a palliative measure for structural stabilization as an adjunct to radiation treatment. The extensive cortical disruption posed a high risk for tumor displacement and cement leakage, so coblation was planned as a cavity-creation measure prior to cement augmentation. Given the extent of osteolysis within the vertebral body, it was decided to combine bilateral transpedicular and extrapedicular approaches to maximize the volume of cavity creation within the tumor. Surgical back-up had been alerted and was available in the event of procedural complications.
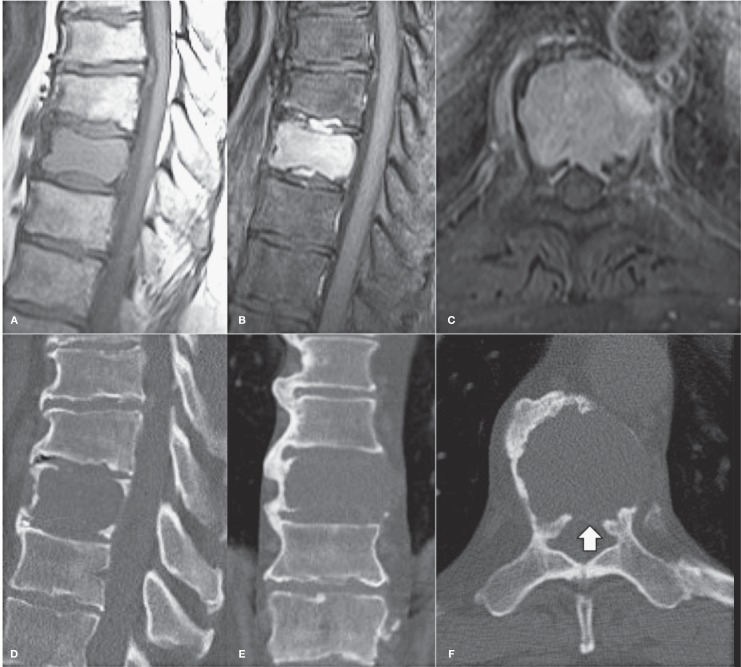
Figure 1.
Thoracic spine MRI and CT. Unenhanced sagittal T1-W (A), enhanced fat suppressed sagittal (B) and axial (C) T1-W MR images, and multiplanar unenhanced CT images (D-F), showing a large enhancing osteolytic lesion involving the whole T8 vertebral body. There is extensive cortical destruction, with a large posterior wall defect (arrow).
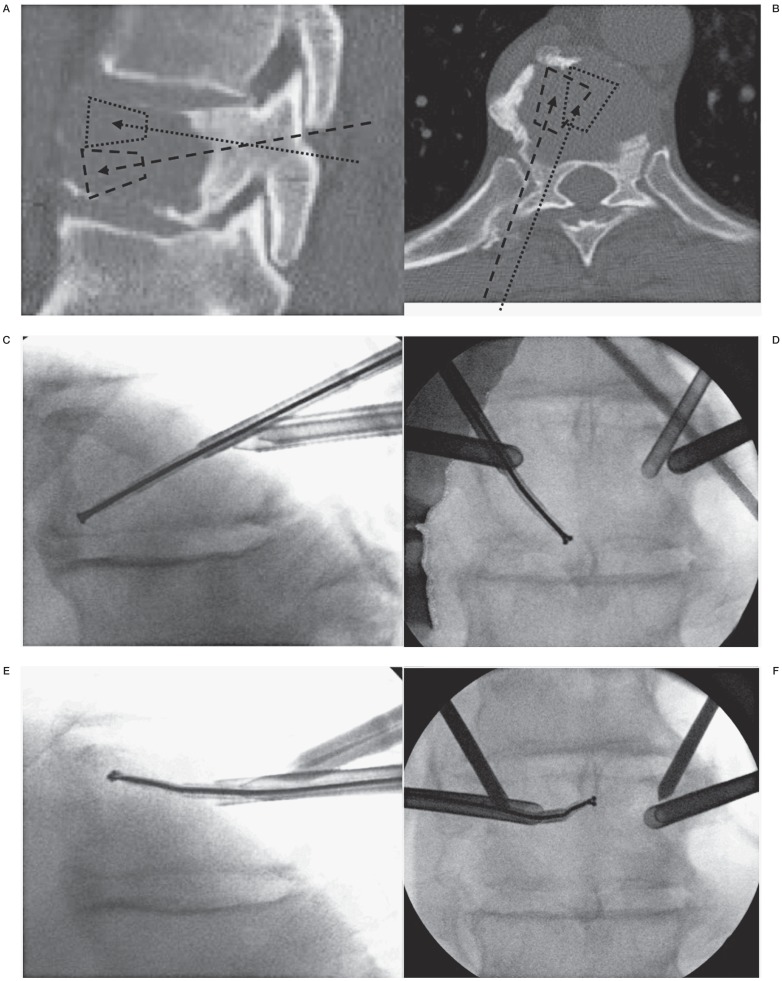
The patient was placed in the prone position under conscious intravenous sedation and local anesthesia. Using biplanar fluoroscopic guidance, two 8G transpedicular needles and two 11G extrapedicular needles were placed in the posterior third of the T8 vertebral body. The transpedicular needles were directed toward the supero-medial aspects of the vertebral body. The extrapedicular needles, advanced through the costo-pedicular joint, had a more cranio-caudal direction toward the inferior and medial aspects of the vertebral body (Figure 2A-E).
Figure 2.
Graphic model and intraoperative images of the combined trans- and extrapedicular approach. The projected transpedicular (dotted line) and extrapedicular (dashed line) accesses and expected volumes of ablation are shown on sagittal (A) and axial (B) CT images. The coblation wand is inserted through the 11G (C,D) and 8G (E,F) cannulas and placed, along midline in the anterior two-thirds of the T8 vertebral body, into the lytic lesion to create a cavity.
Under fluoroscopic control, a coblation wand (Cavity SpineWand, Arthrocare, Austin, TX, USA) was passed consecutively through each needle, to reach all portions of the anterior two thirds of the vertebral body and ablate the maximum volume of tumor (Figure 2F-I). Ablation was stopped when the operator experienced tactile absence of resistance in the advancement of the wand. Subsequently, a total of 7-8 cc of high-viscosity polymethylmethacrylate (PMMA) cement (Stryker VertaPlex HV, Kalamazoo, MI, USA) was slowly injected through the same needles into the cavity created.
Results
The combined transpedicular and extrapedicular approach was performed uneventfully, and allowed coaxial access of the coblation wand to the superior and inferior two thirds anterior aspects of the vertebral body, along the midline. The subsequently injected cement reached the superior and inferior disc endplates, bilaterally and across the midline, and approached the posterior wall with no epidural or vascular leaks (Figure 3A,B). No complications were encountered during the two-hour procedure.
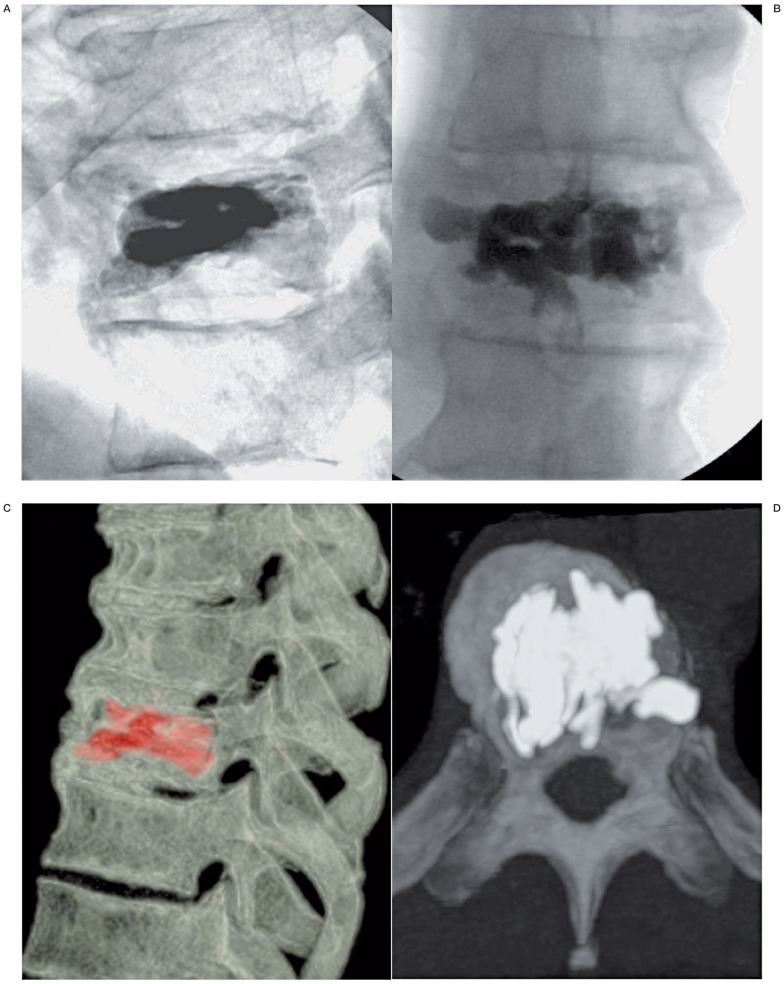
Figure 3.
Post-operative antero-posterior (A) and lateral (B) fluoroscopic images demonstrating bone cement distribution within the T8 vertebral body. Post-operative CT scan, with sagittal volume rendering view (C) and axial MIP (D) images shows with further precision the distribution of PMMA cement in the vertebral body, spanning superior to inferior disc endplates, restoring structural stability, without evidence of intracanalar leakage.
Post-operative CT images confirmed good cement filling and a well-distributed spread involving the entire vertebral body. The cement was completely confined, with no venous or epidural leakage. The patient subsequently underwent radiation treatment at the index level. A follow-up CT at three months post surgery showed the cement in an unchanged, solid bolus pattern, and no subsequent compression fractures (Figure 3C,D).
Discussion
Percutaneous vertebroplasty (PV) stabilizes weight-bearing bones through the injection of bone cement into the vertebral body. Cement leakage is one of the primary risks for this procedure, which may compromise the spinal cord or nerve roots. Risk of cement extravasation may be high in cases where malignant lesions cause cortical destruction 1,4,8,9. Tumor displacement, especially toward the epidural space, is another potential risk in cases of posterior wall breach. Cavity creation through the dissolution of the neoplastic tissue, prior to cement injection, seems a reasonable method to reduce these risks.
Several studies propose that the cavity created by coblation helps to direct the flow of cement away from the compromised posterior wall of the vertebra. Precise tissue removal facilitates a focused cavity formation, reducing pressure and potentially decreasing the risk of cement leakage 7. The limited radius of ablation at the electrode tip ensures optimal control, which is valuable in proximity of neural structures. However, because of the rigid wand the volume of ablation is limited, especially in large lesions. Other methods of tumor ablation, such as thermal radiofrequency and cryotherapy, have the potential for ablation of larger areas, but lack the ability of instantaneous dissolution of tissue.
In the case presented, structural stabilization was necessary to prevent impending collapse of the vertebral body, which could potentially lead to spinal cord compression. Radiation treatment is the treatment of choice in plasmacytomas, with curative purposes, but in such large lytic lesions provides only partial and recuperation of structural stability after a two to four month delay.
The use of coblation and vertebroplasty has previously been described as a treatment for spinal tumors, but this case differed due to the extensive lytic destruction of the vertebral body. Ablating only a small portion of the tumor would not have mitigated the risk of cement leakage and/or tumor displacement. Furthermore and probably more relevant, in the absence of residual osseous supporting structures, was the need to create a supporting pillar of cement in the anterior weight-bearing portion of the vertebral body, spanning superior to inferior disc endplates. In this case, a standard transpedicular or extrapedicular approach would only eliminate a minor portion of the tumor, leaving a substantial soft tissue mass inside the vertebral body. A combination of four entry sites, transpedicular and extrapedicular, were used to maximize the volume of tissue removed. After placing the four needle tips in the posterior third of the vertebral body, the coblation wand was coaxially inserted one needle at a time, allowing the operator to ablate overlapping cone-shaped areas of tissue, involving superior and inferior, lateral and medial quadrants of the anterior two thirds of the vertebral body. The slow, fluoroscopically monitored injection of high-viscosity cement resulted in a successful, desired cement distribution into the anterior two thirds of the vertebral body, spanning superior to inferior endplates.
Although coblation and vertebroplasty are not curative therapies in the treatment of spinal malignancies, and combined treatment increases the cost of the procedure, they are employed to restore structural stability to the vertebrae while assisting in the management of pain and mobility. The volumetric removal of tumor tissue with the use of coblation prior to vertebroplasty may reduce the risk of tumor displacement and cement leakage.
Conclusions
The technical modification described in this case yielded positive results while overcoming some of the limitations of the existing coblation device. This approach may offer an option for cement-augmentation of extensive vertebral body lytic lesions, at increased risk for tumor displacement and extra-vertebral cement leakage, until a more adequate device design can be developed.
References
- 1.Chiras J, Depriester C, Weill A, et al. Percutaneous vertebral surgery. Technics and Indications. J Neuroradiol. 1977;24(1):45–59. [PubMed] [Google Scholar]
- 2.Krishnaney AA, Steinmetz MP, Benzel EC. Biomechanics of metastatic spine cancer. Neurosurg Clin N Am. 2004;15(4):375–380. doi: 10.1016/j.nec.2004.04.001. doi: 10.1016/j.nec.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Carrafiello G, Laganà D, Ianniello A, et al. Plasma-mediated radiofrequency ablation followed by percutaneous cementoplasty under fluro-CT guidance: a case report. Cases J. 2009;2(1):8548. doi: 10.4076/1757-1626-2-8548. doi: 10.4076/1757-1626-2-8548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Georgy BA, Wong W. Plasma-mediated radiofrequency ablation assisted percutaneous cement injection for treating advanced malignant vertebral compression fractures. Am J Neuroradiol. 2007;28(4):700–705. [PMC free article] [PubMed] [Google Scholar]
- 5.Schaefer O, Lohrmann C, Markmiller M, et al. Technical innovation Combined radiofrequency thermal ablation and percutaneous cementoplasty treatment of a pathologic fracture. J Vasc Interv Radiol. 2002;13(10):1047–1450. doi: 10.1016/s1051-0443(07)61872-7. doi: 10.1016/S1051-0443(07)61872-7. [DOI] [PubMed] [Google Scholar]
- 6.Georgy BA. Bone cement deposition patterns with plasma-mediated radio-frequency ablation and cement augmentation for advanced metastatic spine lesions. Am J Neuroradiol. 2009;30(6):1197–1202. doi: 10.3174/ajnr.A1548. doi: 10.3174/ajnr.A1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hong K, Georgiades C. Radiofrequency ablation: mechanism of action and devices. J Vasc Interv Radiol. 2010;21(Suppl. 8):S179–186. doi: 10.1016/j.jvir.2010.04.008. doi: 10.1016/j.jvir.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Klimo P, Jr, Schmidt MH. Surgical management of spinal metastases. Oncologist. 2004;9(2):188–196. doi: 10.1634/theoncologist.9-2-188. doi: 10.1634/theoncologist.9-2-188. [DOI] [PubMed] [Google Scholar]
- 9.Harrington KD. The use of methylmethacrylate for vertebral-body replacement and anterior stabilization of pathological fracture-dislocations of the spine due to metastatic malignant disease. J Bone Joint Surg Am. 1981;63(1):36–46. [PubMed] [Google Scholar]