Abstract
Alport syndrome is an inherited nephropathy associated with mutations in genes encoding type IV collagen chains present in the glomerular basement membrane. COL4A5 mutations are associated with the major X-linked form of the disease, and COL4A3 and COL4A4 mutations are associated with autosomal recessive and dominant forms (thought to be involved in 15% and 1%–5% of the families, respectively) and benign familial hematuria. Mutation screening of these three large genes is time-consuming and expensive. Here, we carried out a combination of multiplex PCR, amplicon quantification, and next generation sequencing (NGS) analysis of three genes in 101 unrelated patients. We identified 88 mutations and 6 variations of unknown significance on 116 alleles in 83 patients. Two additional indel mutations were found only by secondary Sanger sequencing, but they were easily identified retrospectively with the web-based sequence visualization tool Integrative Genomics Viewer. Altogether, 75 mutations were novel. Sequencing the three genes simultaneously was particularly advantageous as the mode of inheritance could not be determined with certainty in many instances. The proportion of mutations in COL4A3 and COL4A4 was notably high, and the autosomal dominant forms of Alport syndrome appear more frequently than reported previously. Finally, this approach allowed the identification of large COL4A3 and COL4A4 rearrangements not described previously. We conclude that NGS is efficient, reduces screening time and cost, and facilitates the provision of appropriate genetic counseling in Alport syndrome.
Keywords: Alport syndrome, genetic renal disease, molecular genetics
Alport syndrome (AS) is an inherited disorder characterized by progressive hematuric nephropathy with ultrastructural changes of the glomerular basement membrane (GBM). Affected patients often present with high-tone sensorineural hearing loss and specific ocular lesions.1 AS accounts for 0.6%–2% of patients starting RRT in Europe, with a frequency evaluated at 1 in 5000 people,2,3 although that number is probably overestimated.4 The disease is genetically heterogeneous and associated with mutations in one of three genes encoding the α3, α4, and α5 chains of type IV collagen that form a distinct network in the GBM that is essential for the long-term stability of the glomerular filtration barrier.5,6 Mutations in COL4A5, encoding the α5(IV) chain, are responsible for the X-linked form of the disease, which is usually much more severe in men than women. Mutations in COL4A3 and COL4A4, encoding the α3(IV) and α4(IV) chains, are associated with autosomal AS. In the autosomal recessive form, patients frequently reach end stage renal failure (ESRF) before the end of the second decade,7 and women are as severely affected as men. Heterozygous parents can present without any symptoms, with isolated microhematuria, which corresponds to what is observed in benign familial hematuria (BFH), or with a progressive renal disease, like in autosomal dominant AS. In this latter form of AS, women and men are equally affected and usually progress to ESRF later than in the autosomal recessive form.8–10 The frequency of each form of AS is estimated to be 80%–85% for X-linked AS, 15% for autosomal recessive AS, and 1%–5% for autosomal dominant AS.11 However, these numbers may be skewed, because most series with molecular analysis are limited to the sequencing of COL4A5. Identifying the mode of inheritance of AS is essential for providing genetic counseling in affected families. The study of the genealogy and the clinical and morphologic phenotypes does not always allow certain determination of the mode of transmission of the disease. Studying the expression of the type IV collagen chains in skin and/or kidney basement membranes can help.12 However, in about one third of the families, irrespective of the mutated gene, the expression of type IV collagen chains is normal, and thus, it does not rule out the diagnosis at all.13 In these cases as well as cases in which the expression of type IV collagen chains has not been studied, molecular testing might be required to make a definitive diagnosis and determine the mode of inheritance. Molecular testing is expensive and exhausting because of the broad size of the genes, comprising 48–53 exons each, and the lack of mutational hot spots.
High-throughput next generation sequencing (NGS) technologies that have recently been developed parallelize the sequencing process, producing millions of sequences at one time,14 and they can be used for limited genomic regions after targeted genome capture or multiplex PCR amplification. It has recently been shown to be efficient in diagnostic screening of human diseases,15 including renal diseases, such as autosomal dominant polycystic kidney disease16 and steroid-resistant nephrotic syndrome.17 Here, we used multiplex PCR, amplicon quantification, library barcoding, and sample pooling followed by NGS for mutation analysis of three type IV collagen genes in a large series of patients affected with AS or BFH.
Results
Patients’ Phenotypes and Mode of Inheritance
In total, 101 patients with hematuric nephropathy were included. Ninety patients were considered as possibly affected with AS. Ten patients were considered as likely affected with BFH (however, in families 57 and 79, only women were affected), because individuals in at least two generations presented with isolated hematuria (without proteinuria or renal failure). One woman (40) presented with sporadic isolated hematuria without proteinuria. Supplemental Table 1 shows the clinical, biologic, and morphologic information, modified Flinter scoring (Concise Methods), and suspected mode of inheritance for each proband. The mode of inheritance could be assessed with certainty in only 19 cases (shown in Supplemental Table 1): 12 X-linked cases displaying either a complete lack or a segmental distribution of α5(IV) expression in the skin basement membrane (BM), five autosomal recessive cases displaying a lack of α5(IV) in the GBM but normal α5(IV) expression in the skin and Bowman capsule BM, and two autosomal dominant cases with a father to son transmission.
NGS Results and Mapping Statistics
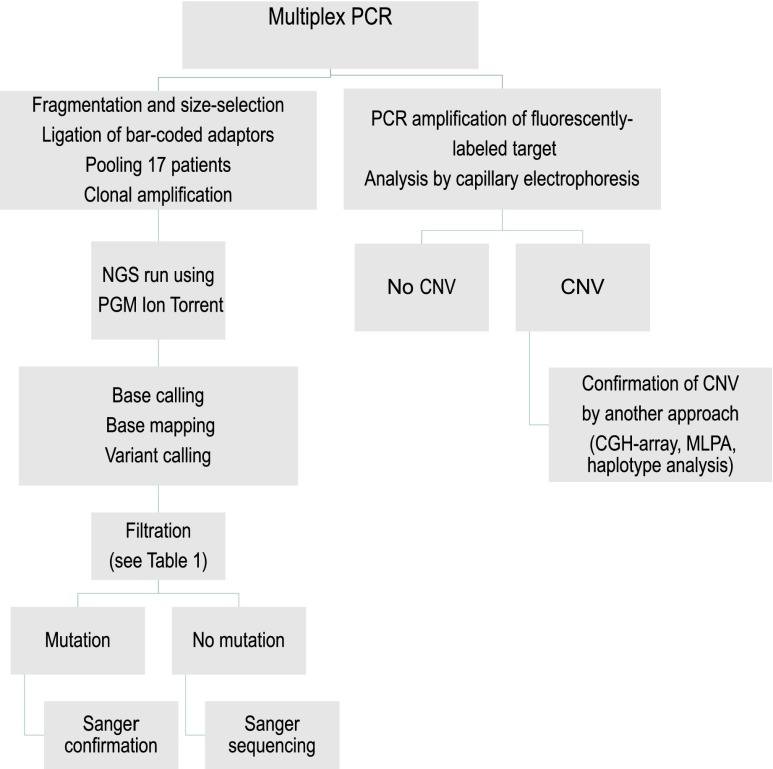
Schematic representation of the workflow used in this study is shown in Figure 1. All coding exons were amplified in a four-tube multiplex PCR reaction for each patient. PCR products were used to both prepare the library for NGS and perform capillary electrophoresis analysis of fluorescently labeled amplified targets to search for deletion or duplication. The barcoded library was sequenced using the nonoptical semiconductor (Ion Torrent Personal Genome Machine (PGM); Life Technologies) technology. For proof of principle, we tested 29 patients previously sequenced by Sanger analysis on one (15 patients), two (13 patients), or three (1 patient) COL4A3–COL4A4–COL4A5 genes; 310 variations had been identified by Sanger sequencing: 302 (68 being different) single nucleotide variants (SNVs), six different deletions (1–18 bases), and two different insertions (1 and 2 bases, respectively). All were detected by NGS. In addition, we detected a homozygous four-exon duplication in COL4A3 that had not been identified by Sanger analysis and two mutations in COL4A5 in individuals previously tested only on COL4A3 and COL4A4 based on clinical data.
Figure 1.
Mutation screening strategy. Schematic visualization of the workflow used for variation screening. CGH, comparative genomic hybridization; CNV, copy number variation; NGS, next generation sequencing; PGM, personal genome machine.
Sequencing the cohort of 101 patients generated a total of about 5 million reads with an average size of 149 bases. Because protocols for library preparation and sequencing and primary analysis software were regularly upgraded during the time of our study (Concise Methods), the mapping statistics are shown for the last two runs, including 33 patients. These two runs are representative of the data obtained with the last version of the variant caller (variant caller 3). Mean coverage was 508×, and 98% of each base (of all exons and 20 bases of padding around all targeted coding exons) was covered more than 15×. Because of the lack of PCR amplification of COL4A4 exon 43 (Supplemental Material) and low coverage of COL4A3 exon 1, these two exons were resequenced by Sanger analysis in all patients. In addition, COL4A4 exon 5 was resequenced by Sanger analysis in 11 patients. Supplemental Table 2 shows the average and minimum coverage of each of 150 coding exons (COL4A3, -4, and -5) across these 33 patients. SNV and indel calling resulted in the identification of 715 SNVs (76 being synonymous) and 44 indel calls for 33 patients, which represent 98 different SNVs (12 being synonymous) and 12 different indels. Variant filtering procedures, shown in Table 1, led to retention of 28 different variations that were tested by Sanger sequencing; 27 of them were confirmed. The single variation that was not confirmed by Sanger analysis was a 1-bp deletion. Thus, with the latest version of the software, our rate of false positive was 1/28.
Table 1.
Variant filtering procedure
| Filtration Criteria | Total | Different Variations | ||||
|---|---|---|---|---|---|---|
| Nonsynonymous SNV | Synonymous SNV | Indel | Nonsynonymous SNV | Synonymous SNV | Indel | |
| Variant caller | 639 | 76 | 44 | 86 | 12 | 12 |
| After frequency filteringa | 44 | 11 | 36 | 33 | 6 | 10 |
| After in-house rare variant filtering | 21 | — | 32 | 21 | — | 9 |
| After visual inspectionb | 21 | — | 9 | 21 | — | 7 |
| After Sanger confirmation | 21 | — | 6 | 21 | — | 6 |
SNV, single nucleotide variant.
Based on allele frequencies in dbSNP135, 1000 Genome, and EVS (ESP6500) databases (variants with minor allele frequency<0.01 are retained).
Visual inspection consists in analysis of the reads by using the Integrative Genomics Viewer software.
Mutation Analysis of Our Cohort
We identified 94 different variants considered as disease-causing (n=88) or of unknown significance (n=6) on 116 alleles in 83 unrelated patients. All small variations were confirmed by Sanger sequencing. To look for potential false negatives, 18 patients for whom no possibly disease-causing variation was identified as well as 1 patient (patient 9) presenting like autosomal recessive AS but found to carry a single heterozygous COL4A3 mutation were then tested by Sanger analysis. Two additional mutations were identified: the c.2621_2622delinsT (p.Gly874Valfs*9) in COL4A3 in patient 9 and the c.2322delT (p.Leu775Phefs*7) in COL4A4 in patient 87. Thus, if we add these 19 patients to the 29 patients in our proof-of-principle group, 636,360 bases have been sequenced by both NGS and Sanger, and the sensitivity of NGS is 99% (310/312), whereas the specificity is 99.99% (636,033/636,048). Importantly, we went back to the NGS reads for two patients carrying the two mutations not detected by NGS. The Integrative Genomics Viewer (IGV) software18 clearly displayed these two mutations (Supplemental Figure 1).
Results of the molecular analysis for all patients are shown in Supplemental Table 1. Mutations were identified in 80% (81/101) of patients; variants of unknown significance were identified in three additional patients. Seventy-five mutations were novel, confirming that most mutations identified in type IV collagen genes are private. Variations of unknown significance (detailed in Supplemental Table 3) were three missense variants not involving a glycine residue located at the X or Y position of the Gly-X-Y collagenous repetition, one COL4A4 silent variant possibly affecting splicing (c.114G>A), and two intronic variants in COL4A3. The silent COL4A4 change c.114G>A as well as the COL4A3 c.988–6C>T change only modestly modified the score of the acceptor splice sites of COL4A4 intron 2 and COL4A3 intron 17, respectively. The c.2981–76C>T variation was predicted to create a donor splice site with a very good score (87/100 with the Human Splicing Finder program19), which might be responsible for the inclusion of a novel exon in the COL4A3 transcript.
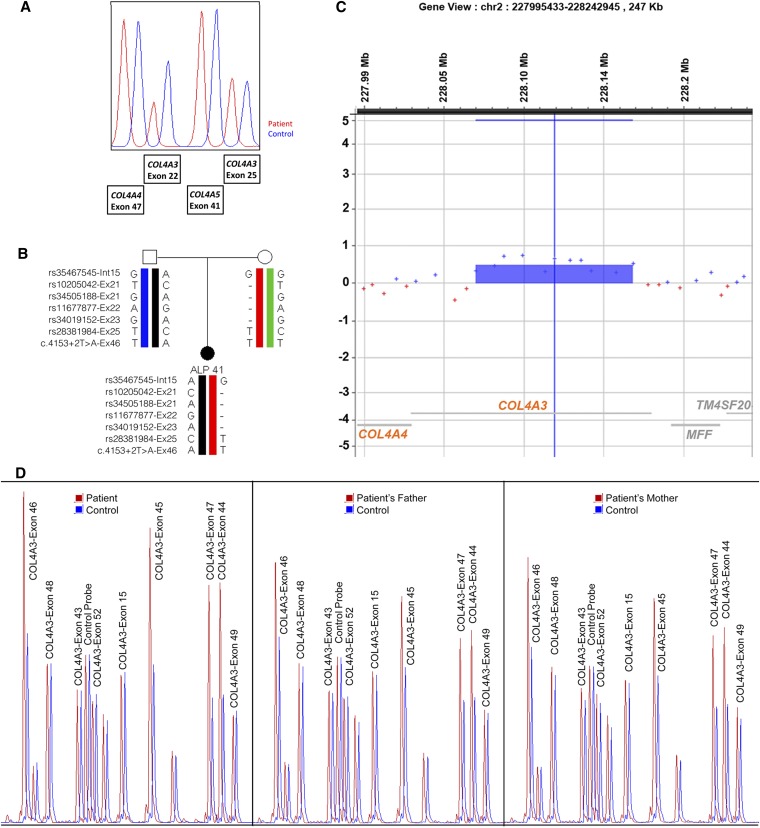
Only 30 mutations (and one variation of unknown significance) were identified in COL4A5; 28 mutations and three variations of unknown significance were found in COL4A3, and 22 mutations and two variations of unknown significance were found in COL4A4. Table 2 shows details regarding the different mutation types in each of the three genes. Novel mutations and variations of unknown significance in COL4A3, COL4A4, and COL4A5 are shown in Tables 3, 4 and 5, respectively. As previously reported by us20 and others,21 most variations were missense mutations affecting a glycine codon. Interestingly, we found two variants in the heterozygous state in two genes (one in each gene) in three patients (14, 37, and 67) and two different mutations (one glycine missense and one frameshift) in the homozygous state in the same gene (COL4A4) in one patient (patient 1). Importantly, analysis by capillary electrophoresis allowed the identification of large rearrangements in 10 patients, affecting COL4A5 in three patients, COL4A3 in six patients (a four-exon duplication in COL4A3 was present in two unrelated patients), and COL4A4 in one patient. The homozygous COL4A3 three-exon deletion in case 30 was confirmed by the lack of amplification of genomic DNA by simplex PCR. All other rearrangements were confirmed by a second method (haplotype analysis, comparative genomic hybridization array, or customized multiplex ligation-dependant probe amplification [MLPA] analysis) as illustrated in Figure 2. The deletion in patient 24 was shown by MLPA to involve COL4A4 exons 1–4 and COL4A3 exon 1. Thus, this patient was carrying both a heterozygous COL4A3 mutation and a heterozygous COL4A4 mutation on the same allele. In addition, mosaicism for a deletion of 21 exons in COL4A5 detected by capillary electrophoresis analysis of the amplicons was likely in one man (84), which fits with a discontinuous labeling of the dermoepidermic basement membrane with anti-α5(IV) antibodies. Parents’ DNAs could have been tested in 36 cases. Mutations were inherited in 33 patients and de novo in 3 patients (all 3 patients carried a COL4A5 mutation).
Table 2.
Details on variations’ types within each gene
| Mutation Features | COL4A3 | COL4A4 | COL4A5 |
|---|---|---|---|
| Number of variations (number of novel mutations) | 41 (36) | 24 (22) | 31 (23) |
| Number of mutated alleles | 53 | 34 | 31 |
| Number of patients | 33a | 20 (+2a+1b) | 31b |
| Number of patients with homozygous variation | 7 | 7 | 0 |
| Number of patients with two heterozygous variations | 13 | 4 | 0 |
| Number of patients with heterozygous variation | 13a | 9 (+2a+1b) | 8c |
| Number of splice variations | 7 | 4d | 6 |
| Number of nonsense variations | 3 | 1 | 3 |
| Number of frameshift variations | 6 | 7 | 2 |
| Number of missense variations (missense affecting glycine) | 19 (14) | 9 (7) | 15 (12) |
| Number of small deletions | 1 | 2 | 2 |
| Number of larger arrangements (type) | 5 (three deletions and two duplications) | 1e (one deletion) | 3f (three deletions) |
Cases 14 and 37 carry a heterozygous COL4A3 variation and a heterozygous COL4A4 variation.
Case 67 carries a heterozygous COL4A4 variation and a heterozygous COL4A5 variation.
Variation was heterozygous in eight women.
Effect on splicing of COL4A4 c.114G>A p.Gly38Gly is modest according to the Human Splicing Finder program.18
The COL4A4 deletion of exons 1–4 was shown by multiplex ligation-dependant probe amplification (MLPA) to also involve COL4A3 exon 1 in patient 24.
One 21-exon deletion was a probable mosaic in one man, and one 3-exon deletion was present in one woman; one deletion, removing COL4A5 exons 1 and 2 and all COL4A6 exons, was present in one man and thus, did not require capillary electrophoresis analysis to be detected.
Table 3.
Novel COL4A3 variations
| Exon (Intron) Number | Nucleotide Change | Amino Acid Substitution |
|---|---|---|
| 1 | c.[2T>G] | p.[Met1Arg] |
| 2–50 | c.[88- ?_4755+ ?dup] | |
| 3 | c.[145G>C] | p.[Gly49Arg] |
| 3 | c.[172G>A] | p.[Gly58Ser] |
| 6 | c.[345delG] | p.[Pro116Leufs*37] |
| 6 | c.[346C>A]a | p.[Pro116Thr] |
| 7 | c.[432_440delinsGATTA] | p.[Gly145Ilefs*7] |
| (9) | c.[546+1G>T] | |
| 14 | c.[805G>T] | p.[Glu269*] |
| 16–19 | c.[889- ?_1114+ ?del] | |
| 17 | c.[934G>C ] | p.[Gly312Arg] |
| (17) | c.[988–6C>T]a | |
| 22 | c.[1354G>A] | p.[Gly452Arg] |
| 22 | c.[1363G>T] | p.[Gly455Cys] |
| 21–23 | c.[1151-?_1504+?del] | |
| (23) | c.[1504+1G>A] | |
| 24 | c.[1558G>C] | p.[Gly520Arg] |
| 26 | c.[1855G>A] | p.[Gly619Arg] |
| (27) | c.[2020+2T>C] | |
| 28 | c.[2065G>A] | p.[Gly689Arg] |
| 29 | c.[2197G>A] | p.[Gly733Arg] |
| 30 | c.[2323_2340del] | p.[Leu775_Gly780del] |
| 31–32 | c.[ 2375-?_2656+?del] | |
| 33 | c.[2737G>A] | p.[Gly913Arg] |
| 34 | c.[2768_2778del] | p.[Val923Glufs*13] |
| (35) | c.[2981–76C>T]a | |
| 37 | c.[3115G>C] | p.[Gly1039Arg] |
| 38 | c.[3238G>A] | p.[Gly1080Arg] |
| 40 | c.[3454G>C] | p.[Gly1152Arg] |
| 42 | c.[3674G>T] | p.[Gly1225Val] |
| 44–47 | c.[3883- ?_4252+?dup]b | |
| (46) | c.[4153+2T>A] | |
| 48 | c.[4364delC] | p.[Thr1455Lysfs*74] |
| 49 | c.[4502C>A] | p.[Pro1501Gln] |
| 50 | c.[4708T>C] | p.[Cys1570Arg] |
| 50 | c.[4743T>G] | p.[Phe1581Leu] |
Variants of unknown significance.
Location of the duplications has not been checked.
Table 4.
Novel COL4A4 variations
| Exon (Intron) Number | Nucleotide Change | Amino Acid Substitution |
|---|---|---|
| 1–4 | c.[1-?_192+?del]a | |
| 3 | c.[114G>A]b | p.[Gly38Gly] |
| 3 | c.[81_86del] | p.[Ile29_Leu30del] |
| 5 | c.[313delG] | p.[Asp105Thrfs*16] |
| 7 | c.[455G>A] | p.[Gly152Glu] |
| 8 | c.[508G>A] | p.[Gly170Arg] |
| 9 | c.[560delG] | p.[Gly187Glufs*32] |
| (11) | c.[694–2A>T] | |
| 15 | c.[919C>T]b | p.[Pro307Ser] |
| 15 | c.[914_930+30del] | |
| 19 | c.[1118G>A] | p.[Gly373Glu] |
| 20 | c.[1351G>A] | p.[Gly451Ser] |
| 22 | c.[1460G>T] | p.[Gly487Val] |
| 27 | c.[2075G>T] | p.[Gly692Val] |
| 28 | c.[2322delT]c | p.[Leu775Phefs*7] |
| (30) | c.[2717–2A>G] | |
| 39 | c.[3684delG] | p.[Gly1230Valfs*58] |
| (40) | c.[3817+1G>T] | |
| 47 | [4646delT] | [Leu1549Profs*3]] |
| 47 | c.[4693C>T] | p.[Arg1565Cys] |
| 47 | [4698delT] | p.[Cys1566Trpfs*37] |
| 48 | c.[5013_5017del] | p.[Glu1672Profs*17] |
Deletion was shown by MLPA to also involve COL4A3 exon 1 in patient 24.
Variants of unknown significance; the c.[114G>A] variation may have some effect on splicing.
Variation was identified by Sanger analysis.
Table 5.
Novel COL4A5 variations
| Exon (Intron) Number | Nucleotide Change | Amino Acid Substitution |
|---|---|---|
| 1–2 | c.[1-?_141+?del]a | |
| 2–22 | c.[82-?_1516+?del] | |
| 5 | c.[321_321+1dup] | p.G108Wfs*48 |
| 17 | c.[947G>A] | p.[Gly316Asp] |
| 25 | c.[1826G>A] | p.[Gly609Asp] |
| 25 | c.[1846_1854del] | p.[Asn616_Gly618del] |
| 25 | c.[1894G>C] | p.[Gly632Arg] |
| 25 | c.[1913G>A] | p.[Gly638Asp] |
| 25 | c.[1931G>A] | p.[Gly644Asp] |
| 29 | c.[2264T>G] | p.[Leu755*] |
| 31 | c.[2589_2660del] | c.[Ser864_Gly887del] |
| 32 | c.[2765_2766delinsTT] | p.[Lys922Ile] |
| (33) | c.[2918–1G>A] | |
| 34 | c.[2918G>A] | p.[Gly973Asp] |
| 35 | c.[3071G>A] | p.[Gly1024Glu] |
| 36 | c.[3154C>T] | p.[Gln1052*] |
| 41 | c.[3685G>T] | p.[Gly1229Cys] |
| 44 | c.[3899delG] | p.[Gly1300Glufs*20] |
| 45–47 | c.[3925-?_4198+?] | |
| 46 | c.[4054C>A]b | p.[Leu1352Ile] |
| (48) | c.[4316–2A>G] | |
| 49 | c.[4352G>A] | p.[Gly1451Asp] |
| 53 | c.[5051G>A] | p.[Cys1684Tyr] |
Deletion was extending in COL4A6.
Variants of unknown significance.
Figure 2.
Large COL4A3-COL4A4 rearrangements. Characterization of rearrangements detected by NGS. (A) GeneScan analysis of part of one multiplex PCR amplification product in patient 41 (red) and control DNA (blue) showing a heterozygous deletion of COL4A3 exon 22, whereas the signal for COL4A3 exon 25 appears normal. (B) Haplotype analysis of single nucleotide variants (SNVs) localized in COL4A3 intron 15 and exons 21–23, 25, and 46 in patient 41 and her parents showing no maternal contribution for SNVs in exons 21–23 but a biparental contribution to the SNVs in intron 15, exon 25 (there is no SNV in COL4A3 exon 24), and exon 46. (C) Array CGH profile of chromosome 2 showing a duplication of most of the COL4A3 gene in case 35. Results are shown as log2 intensity ratios of patient 35 to reference. Size of the duplication, which includes 11 probes, is between 99 and 113 kb. (D) MLPA analysis of DNA of patient 42 (left panel), his father (center panel), and his mother (right panel). Probes for COL4A3 and COL4A4 exons are indicated above their respective peaks. Three control probes (not labeled) are used for normalization. MLPA shows a duplication of COL4A3 exons 44–47 in the homozygous state in the patient and the heterozygous state in his parents. The same customized MLPA approach confirmed the rearrangements in cases 24, 42, 54, and 68.
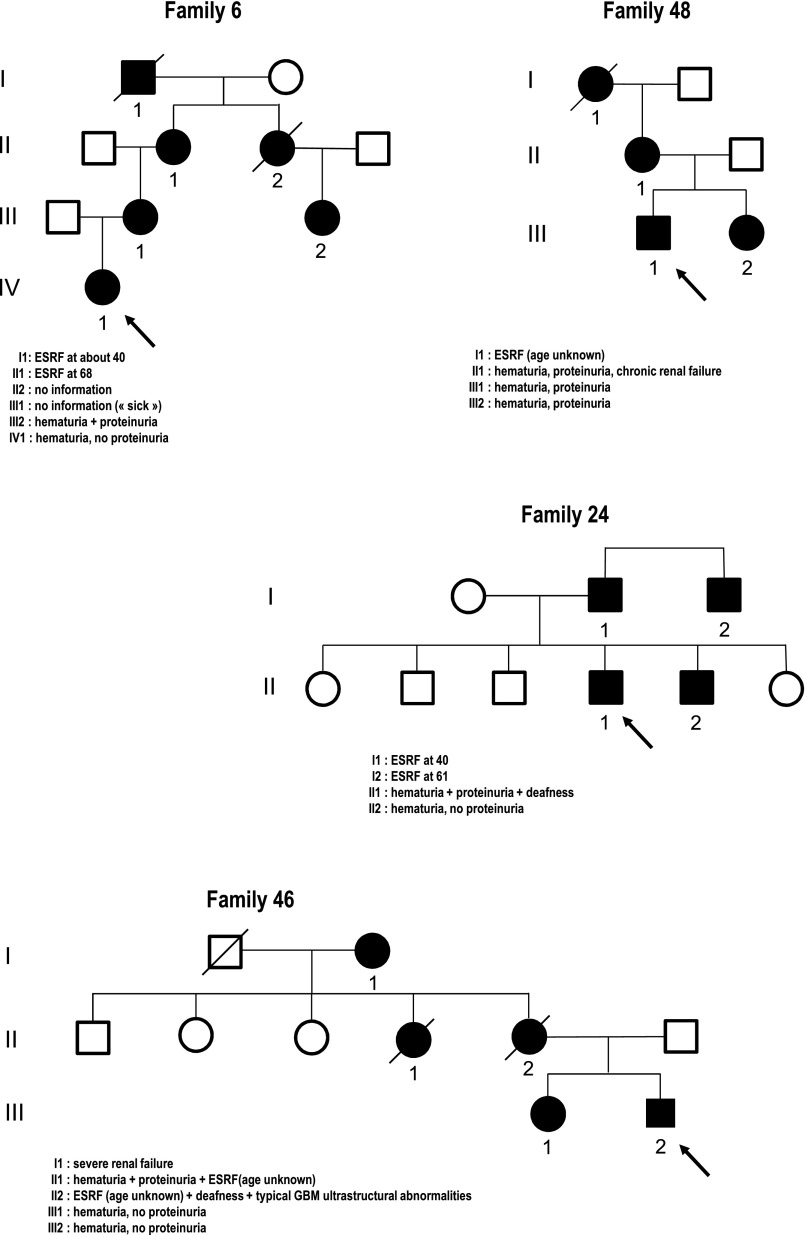
Interestingly, a high proportion of probands of our cohort (n=22) was found to carry a heterozygous mutation in COL4A3 (12 cases plus 1 case with a variant of unknown significance) or COL4A4 (eight cases plus one case with a variant of unknown significance). For all of them, the clinical, familial, and morphologic data were compatible with an autosomal dominant mode of inheritance of the disease. Six probands seemed to belong to families affected with BFH, which was suggested by the presence of isolated hematuria without any proteinuria or progression to renal failure in several generations. The 16 other probands belonged to families affected with a progressive hematuric nephropathy. Six had deafness, nine were known to have developed proteinuria, and three had ultrastructural examination of their GBMs, which were thin two times and thick and thin one time. None of them had developed ESRF yet (at an average age of 34.6 years), but older family members had developed ESRD between 40 and 76 years in 10 families, chronic renal failure in 4 families, and nephrotic range proteinuria in 1 family as well as deafness in six families and typical ultrastructural alteration of the GBM in two families. Figure 3 shows examples of four families with autosomal dominant AS (three of them initially were considered as either X-linked or autosomal dominant). The unexpectedly high rate of autosomal dominant inheritance that we observed in our series is also illustrated by the fact that, among 16 patients presenting with either X-linked or autosomal dominant inheritance, only five patients were shown to carry a COL4A5 mutation, seven patients were shown to carry a heterozygous COL4A3 or COL4A4 mutation, and one patient was compound heterozygous for two COL4A3 variations, including one of unknown significance.
Figure 3.
Autosomal dominant forms of AS appear more frequently than reported previously. Pedigrees of four families with autosomal dominant Alport syndrome. The mode of inheritance was certain in family 24 because of father to son transmission of the disease, but it may have been either autosomal dominant or X-linked in the three other families. In all cases, probands (shown by arrows) present without renal failure, but their parents and/or grandparents have developed renal failure with or without deafness.
Twenty-nine probands were shown to carry two COL4A3 or two COL4A4 mutations, and two probands were shown to carry one COL4A3 mutation and one variation of unknown significance. For nine of 29 probands, autosomal recessive inheritance was proven by the testing of the two parents, who were shown to carry one mutation each. For four cases, only one parent was tested and shown to carry one mutation in the heterozygous state; one of these 29 probands had been considered as affected with X-linked AS because of false-negative expression of α5(IV) in skin basement membrane associated with important melanic pigmentation. Thirteen of the patients with autosomal recessive inheritance had reached ESRF at an average age of 19.5 years (15–27 years).
We searched for genotype–phenotype correlations in patients carrying COL4A3 or COL4A4 mutations. We observed no obvious difference in the severity of the disease between probands (or affected relative) carrying a heterozygous mutation in COL4A3 versus COL4A4 or between probands carrying two COL4A3 mutations (five patients having reached ESRF at 20.5 years on average) and probands carrying two COL4A4 mutations (eight patients having reached ESRF at 19.6 years on average). Also, the position (regarding the 5′-3′ orientation of the genes) of the heterozygous variants in COL4A3 or COL4A4 was not different (P=0.64) between the 6 families presenting as BFH (nucleotide 1639 on average) and the 16 families presenting as AS (nucleotide 1866).
In 17 cases (Table 6), we did not identify any variation thought to be possibly disease-causing. In seven patients (patients 16, 21, 39, 43, 52, 56, and 59), the diagnosis of AS was based on abnormality in the expression of type IV collagen chains or typical ultrastructural changes of the GBM. One man (43) was likely mosaic for a COL4A5 mutation (possibly absent of blood cell DNA), because he presented with sporadic hematuria, deafness, and discontinuous labeling of the skin BM with anti-α5(IV) antibodies. In 10 other cases, the diagnosis was not certain, especially in 3 cases: one patient (49) had normal GBM at electron microscopy examination, one patient (33) had proteinuria that spontaneously disappeared, and one patient (44) had severe deafness but had not developed proteinuria or renal failure.
Table 6.
Patients without identified variations
| Patient | Suspected Mode of Inheritance | Sex | Proteinuria (Age [yr]) | Renal Failure (Age [yr] at ESRF) | Deafness | Eye | EM | Immunofluorescence | Modified Flinter Score |
|---|---|---|---|---|---|---|---|---|---|
| 16 | AR | W | Y (NA) | Y (ESRF at 25) | Y | NA | Y (thick and thin) | NA | 2 |
| 21 | X or AR | W | N | N | Y | NA | Y (thick and thin) | GBM, normal; skin, normal | 2 |
| 23 | AD | M | NA | Y | NA | NA | N | NA | 1 |
| 33 | X or AD | M | Y | Y | NA | NA | N | NA | 1 |
| 39 | X | M | NA | Y | N | NA | NA | Skin, negative | 2 |
| 40 | X, AD, or AR | W | N | N | N | N | Y (thin) | NA | 0 |
| 43 | X or AR | M | NA | NA | Y | Y | NA | Skin, discontinuous | 2 |
| 44 | X, AD, or AR | W | NA | N | Y | NA | N | NA | 1 |
| 49 | BFH | W | Y (15) | N | N | N | Y (normal) | NA | 1 (BFH) |
| 52 | X | M | Y (26) | Y | Y | Y | N | Skin, negative | 4 |
| 56 | X or AD | W | Y (64) | N | N | NA | Y (thick and thin) | GBM, normal | 2 |
| 59 | X | W | Y (4) | N | N | NA | N | GBM, discontinuous | 1 |
| 69 | BFH | M | N (29) | N | N | NA | N | NA | 1 (BFH) |
| 71 | BFH | W | N (3) | N | N | N | N | NA | 1 (BFH) |
| 74 | X | M | NA | Y (ESRF at 21) | Y | N | N | NA | 2 |
| 80 | X or AR | M | N (7) | N | N | N | N | NA | 1 |
| 81 | X | W | NA | NA | Y | N | N | NA | 2 |
EM, electron microscopy; AR, autosomal recessive; W, woman; Y, yes; NA, not applicable; X, X-linked; N, no; AD, autosomal dominant; M, man; BFH, benign familial hematuria.
The difference for the modified Flinter score between 84 patients with a variation thought to be possibly disease-causing (average=1.7) and 17 patients without (average=1.5) was not significant (P=0.25). Conversely, the proportion of patients with an identified mutation was not significantly higher in patients with a high (3 or 4) score compared with patients with a low (0–2) score (P=0.29). Also, the proportion of patients with an identified mutation was not statistically different between patients presenting as BFH (6 patients with a mutation and 1 patient with a variation of unknown significance of 10 patients) and patients presenting as AS (75 patients with at least one mutation and 2 patients with a single variant of unknown significance of 90 patients; P=0.57).
Discussion
Mutations in COL4A3, COL4A4, or COL4A5 result in a spectrum of phenotypes from BFH to AS,22 including X-linked AS, autosomal recessive AS, or autosomal dominant AS. Accurate genetic counseling and reasonable estimation of prognosis in patients and families with persistent hematuria require precise diagnosis, which is especially important, because early therapeutic intervention has recently been shown to be effective in AS.23 Comprehensive clinical evaluation and pedigree analysis (including testing of relatives for hematuria) combined with histopathology and study of type IV collagen expression in skin and kidney BM are sometimes sufficient to firmly establish a diagnosis and determine the risk of transmission. However, in many cases, molecular analysis is necessary to achieve the desired level of diagnostic accuracy. Screening for mutations in these three very large (about 50 exons each) genes by conventional (Sanger) sequencing is exhausting, time-consuming, and expensive, which is why molecular analysis is usually performed in a step-by-step process based on familial, clinical, and morphologic data. In families for which these data do not point to a particular mode of inheritance as well as sporadic cases, the traditional work flow usually leads to the analysis of COL4A5 in the first instance based on the estimated frequency of the X-linked form of the disease, although familial and clinical data do not allow for exclusion of autosomal transmission with certainty. In some molecular diagnosis centers, COL4A5 is the only one of the three genes routinely sequenced. More than 800 COL4A5 mutations have been reported to date in the literature (https://grenada.lumc.nl/LOVD2/COL4A/home.php?select_db=COL4A5 and https://portal.biobaseinternational.com/hgmd/pro/all.php), and genotype–phenotype correlations have been clearly established in X-linked AS.20,21 By comparison, only 91 mutations have been reported in COL4A3 and 63 mutations have been reported in COL4A4 in the HGMD database. Very little has been reported on genotype–phenotype correlations in autosomal AS,10 which are considered to be much rarer than the X-linked form.
NGS, by producing millions of DNA sequence reads in a single run, has made easily available whole-exome and whole-genome sequences analyses, and it can also be used for resequencing targeted small genomic regions. NGS has been shown to be successful for identifying type IV collagen mutations in three AS patients.24 Here, we used the Ion PGM (Life Technologies) 316 chips, which allow at least 10 Mb to be read in one run through about 200-bp-long reads at the end of our study. We used a strategy that uses multiplex PCR and sample pooling after library barcoding to sequence in each run 150 exons from 16 or 17 patients. COL4A3 exon 1, which contains 77% of CG and was frequently not amplified during the multiplex PCR process, was tested by Sanger sequencing in all patients. COL4A4 exon 5 (63% CG) was also sometimes not amplified. Although the GC content of that exon is only moderately high, a 20-bp window with 85% GC could be the cause of this bad amplification. COL4A5 exons 41a and 41b have not been included in the design of our study, because no mutation had ever been identified in these alternatively spliced exons (in our department, more than 80 X-linked unrelated AS patients have been tested for these two exons). However, they will be included in the next version of the ALPORT MASTR mix.
In our cohort, we identified 96 different variations: 90 variations are considered as disease-causing and six variations are of unknown significance. Altogether, at least one mutation was identified in 80% (81/101) of the patients, representing a high rate of mutation compared with previously published series of patients tested by conventional approaches.22,25–28 The sensitivity of our NGS screen was 99%, because among 312 variations identified by Sanger sequencing in patients tested by both Sanger and NGS, two variations (one 1-bp insertion–deletion in COL4A3 as well as one 1-bp deletion in COL4A4) were missed by NGS. It is known that NGS-based methods are less accurate to detect indel mutations than point mutations.17 Importantly, simple visual inspection of the NGS reads using IGV very clearly showed these two mutations, suggesting that, even if a few indels are missed by the variant caller, they will be caught by simple careful visual analysis of the reads by using IGV, which thus, must be performed for all patients with no identified mutation. Another problem thought to be unique to certain NGS methods is contiguous runs of the same base pair called homopolymer repeats. However, they should not be a major issue for type IV collagen gene sequencing in AS patients, because sequence analysis of 149 amplicons tested shows only five homopolymer of 6 bp.
In addition, our strategy allowed the detection of large COL4A3 or COL4A4 rearrangements (in seven patients of the cohort and one patient among 29 patients tested in our proof-of-principle experiment) that would not have been detected by Sanger analysis. Because the technology used does not allow for gaining insight into quantification of the PCR products, we performed capillary electrophoresis analysis of the multiplex PCR products (Concise Methods) and detected, in either COL4A3 or COL4A4, heterozygous deletions in four patients, homozygous duplications in two patients, and heterozygous duplications in one patient. It is possible that we missed additional deletions or duplications in the few exons with poor amplification, such as COL4A4 exon 5. Deletions or duplications involving one or more exons have been frequently reported in COL4A529,30 (also see the HGMD database at https://portal.biobase-international.com/hgmd/pro/all.php and the LOVD database at https://grenada.lumc.nl/LOVD2/COL4A/home.php?select_db=COL4A5) but only one time in COL4A331 and never in COL4A4, because they are not easily detectable by conventional Sanger sequencing. Capillary electrophoresis analysis will not even be required in the future, when the 400-bp biochemistry will be available for Ion Torrent, because heterozygous deletions will be easily visible.32 These results should incite laboratories performing COL4A3 and COL4A4 mutation screening by conventional sequencing to complete their screen with a quantitative amplification method to detect heterozygous large rearrangements.
The proportion of variations considered as possibly disease-causing identified in COL4A3 and COL4A4 in our cohort (41 and 24, respectively, of a total of 96) is more important than in previously reported series of AS.33 Our study strongly suggests that the frequency of autosomal AS and in particular, autosomal dominant AS is more important than previously thought in the literature.11 Not taking into account 10 families presenting with BFH and the case of sporadic hematuria, we observed a likely autosomal dominant inheritance in 18.9% (17/90) of the tested AS families in this cohort. It is interesting to note that our traditional diagnostic workflow would have led to the analysis of COL4A5 at first for 29 patients presenting as AS inherited as either an X-linked or an autosomal trait, for whom we identified COL4A5 mutations only 10 times and COL4A3 or COL4A4 mutations 13 times. In the same way, three families with autosomal dominant AS and six families with autosomal recessive AS reported here had been previously tested (by single-strand conformation polymorphism or Sanger sequencing) only on the COL4A5 gene. These results illustrate one of the great benefits of this NGS technology, which allows the sequencing of three type IV collagen genes at one time and led us to reconsider the mode of transmission of the disease and provide adequate genetic counseling in several families. In addition, the finding of patients carrying disease-causing mutations on two different genes (COL4A3 and COL4A4 for cases 14 and 24 and COL4A4 and COL4A5 for case 67) also illustrates the interest of the sequencing in one of three genes and suggests possible digenic inheritance.
We did not find any genotype–phenotype correlations in patients carrying a heterozygous COL4A3 or COL4A4 variant; 17 of 22 patients carried a variant expected to have a dominant effect (15 missense mutations affecting a glycine 13 times, one synonymous mutation possibly affecting splicing, and one splice site mutation predicted not to alter the reading frame). The five other patients (24, 28, 32, 34, and 87) were found to carry a COL4A4 frameshift mutation three times, a COL4A4 deletion removing the initiation ATG codon one time, and a COL4A4 deletion in the signal peptide one time. Heterozygous COL4A4 frameshift mutations have already been reported in autosomal dominant AS.10 Although we cannot exclude the hypothesis that the frameshift mutations and the deletion of the initiation codon eventually lead to the production of an abnormal α4(IV) chain, it is possible that these five mutations lead to AS or BFH because of haploinsufficiency.
It is interesting to note that the proportion of patients with an identified mutation was not statistically different between patients presenting as BFH and patients presenting as AS. Although the number of cases of BFH is limited in our series, this finding suggests that there is no genetic heterogeneity in BFH and that families that have been described with hematuria that does not segregate with the COL4A3/COL4A4 locus34,35 can be explained by coincidental hematuria in family members rather than a novel locus for BFH.
The rate of patients without any identified variation thought to be possibly disease-causing in our series is low (16.8%). We may have missed some deep intronic mutations or mutations affecting regulatory elements, especially in seven cases in which the diagnosis was certain. In others, whole-exome sequencing might be helpful to decipher the cause of the disease in these families. Anyway, our results emphasize the fact that patients with a low Flinter score also must be tested, because we observed no significant difference for that score between patients with and without an identified mutation.
The last but not the least benefit of this strategy regards spared money and time. Barcoding strategies allow us to mix several patients in the same run and thus, reduce costs of the NGS, which itself is constantly decreasing in cost. Currently, taking into account costs of the consumables, sequencing all COL4A3–COL4A4–COL4A5 exons and searching for copy number variation are the same cost as sequencing 25 exons of one gene by Sanger methods. Thus, conventional sequencing of a single gene (when the mode of inheritance is certain, for example) is more expensive than testing three genes by multiplex amplicon quantification and NGS. In terms of time, the different steps of our protocol for a run (17 patients) are currently completed in our laboratory two times more rapidly than Sanger sequencing of three genes.
In conclusion, our study shows that the frequency of autosomal AS and particularly, autosomal dominant AS has been underestimated. We show that the combined approach of multiplex PCR amplification, amplicon quantification, and NGS greatly facilitates the molecular diagnosis of AS, improves appropriate genetic counseling, reduces time and cost of the screening, provides rapid sequencing of three large COL4A3, COL4A4, and COL4A5 genes, and allows the detection of heterozygous rearrangements in COL4A3 and COL4A4.
Concise Methods
Patients
DNA or blood samples from 101 patients were received for molecular screening in the laboratory of the Genetic Department at Necker Hospital in Paris, France with written informed consent and clinical information. They were sent from Nephrology, Pediatric Nephrology, and Genetics Departments in France, Sweden, and Tunisia between June of 2011 and October of 2012. The 101 patients presented hematuria. Sex ratio of the patients was 1.4 (59 men and 42 women). Average age at molecular diagnosis was 26 years (3–54 years). Average age at first symptom (usually hematuria) was 11 years (<1–54 years). Albuminuria (>30 mg/mmol creatininuria) was present in 61 of 77 cases and absent in 16 of 77 cases at the time of molecular diagnosis. Twenty-six patients (seven women and nineteen men) had reached ESRF between 15 and 34 years of age. Sixteen patients (five women and eleven men) had chronic renal failure; 52 patients (28 women and 24 men) had normal renal function.
Patients, all presenting hematuria, were classified according to the Flinter diagnosis criteria,36 which were slightly modified to take into account the expression of type IV collagen chains, when studied: (1) positive family history of hematuria, chronic renal failure, or both, (2) characteristic ophthalmic signs (that is, anterior lenticonus, white macular flecks, or both), (3) high-tone sensorineural deafness, and (4) typical electron microscopic evidence of AS on renal biopsy (that is, irregularly thick GBM or the association of thick and thin segments) and/or abnormal expression of type IV collagen chains within the GBM and/or the dermoepidermal basement membrane. Uniformly thin GBM at electron microscopy examination was not considered as typical of AS, because it can also be observed in BFH as well as other glomerular nephropathies.37 Analysis of our cohort for those criteria is shown Table 7, and the score of each patient is shown in Supplemental Table 1. Altogether, 4 index cases fulfilled four criteria, 14 index cases fulfilled three criteria, 38 index cases fulfilled two criteria, 43 index cases fulfilled one criterion (including 10 patients considered as BFH), and 2 index cases had zero criteria (one women [40] with sporadic hematuria and thin basement membrane and one man [42] with hematuria and proteinuria without hearing or eye defect and without known family history of renal disease). Surprisingly, two men had a discontinuous expression of the α5(IV) in the skin BM.
Table 7.
Analysis of our cohort of patients for diagnosis criteria
| Criteria | Yes/Positive | No/Absent (Discontinuous) | Unknown |
|---|---|---|---|
| Positive family history | 77 | 19 | 5 |
| Characteristic ocular signs | 12 | 40 | 49 |
| High tone sensorineural deafness | 47 | 47 | 7 |
| Typical defect of the GBM on EM | 21 | 5a | 75 |
| α5(IV) labeling in GBM | 8 | 15b (4) | 78 |
| α5(IV) labeling in skin BM | 25 | 12 (3c) | 64 |
BM, basement membrane.
Includes four cases of thin GBM and one case of normal GBM.
Among these 15 cases, 7 cases had skin biopsies: 6 cases showed normal α5(IV) labeling, and 1 case showed negative α5(IV) labeling.
Includes two men and one woman.
The mode of inheritance was suspected according to the study of the genealogy (including the search for hematuria in parents and relatives as often as possible), the severity of the disease in men and women when patients of both sex were affected in a same family, and the study of the expression of α5(IV) chain in skin and/or kidney.
Nineteen patients had been previously tested on at least one type IV collagen gene (fourteen patients on COL4A5) by single-strand conformation polymorphism (twelve patients) or Sanger sequencing (seven patients).
Sample Preparation
Genomic DNA specimens were isolated from peripheral blood using standard procedures.
We used the commercially available, ready-to-use massive parallel sequencing assay for detection of COL4A3, COL4A4, and COL4A5 mutations (ALPORT MASTR; Multiplicom N.V., Niel, Belgium) to amplify all coding exons of the three genes in a four-tube multiplex PCR reaction starting with 4×50 ng genomic DNA; 149 amplicons (representing 150 coding exons) were amplified for each of the 101 patients. COL4A5 exons 41a and 41b were not amplified. Amplification products were diluted and then reamplified with the universal primers included in the ALPORT MASTR kit. Part (50%) of the amplification product was used for five-cycle PCR amplification with fluorescent primers, then checked by capillary electrophoresis, and analyzed using the GeneScan analysis software (Applied Biosystems) to verify the proper amplification of each amplicon. Size of the amplicons ranged from 195 to 445 bp after the last PCR step. For each patient, the remaining four multiplex PCR products were pooled with predefined proportions according to the manufacturer’s instructions, and this pool was used to prepare a barcoded library compatible with the Ion Torrent PGM sequencer (Life Technologies). Libraries construction, NGS procedures, and variants’ filtration are detailed in Supplemental Material. All filtered variations were visualized using the IGV software and then checked by conventional Sanger sequencing after PCR amplification of the exons using flanking intronic primers like in refs. 27, 28, and 38. Variations confirmed by Sanger analysis were checked by the Alamut software (Interactive Biosoftware, Rouen, France) (Supplemental Material).
The cDNAs NM_000091, NM_000092, and NM_0000495 for COL4A3, COL4A4, and COL4A5, respectively, were used for numbering, with nucleotide+1 corresponding to the A of the ATG translation initiation codon.
MLPA
Probes were designed for 17 and 10 exons of the COL4A3 and COL4A4 genes, respectively, using the AlleleID software (Premier Biosoft, Palo Alto, CA). Customized MLPA was performed as described by White et al.39 in a four-probemix assay. We used the SALSA MLPA probemix P300-A2 Human DNA Reference-2 (MRC-Holland, Amsterdam, The Netherlands) as reference.
Statistical Analyses
Data were analyzed using Fisher exact and t tests. All tests were two-sided. P values<0.05 were considered significant.
Note that, during the review process of this manuscript, another group has independently shown, by an NGS approach, that autosomal dominant transmission of AS accounts for a relevant proportion of families.40
Disclosures
None.
Supplementary Material
Acknowledgments
We thank the patients and families for their participation in the study. We thank Mohammed Zarhrate for technical help with NGS and Valerie Malan for comparative genomic hybridization array analysis. We also thank Olivier Gribouval for help in editing the manuscript.
This program has received a state subsidy managed by the National Research Agency under “Investments for the Future” Program ANR-10-IAHU-01.
Part of this material was presented in poster format at the 2013 Annual Meeting of the European Society of Human Genetics (June 8–11, 2013) in Paris, France.
We thank the following physicians for contributions of material and clinical data: Dr. B. Amara (Centre de Néphrologie, Bourgoins), Dr. B. Barrou (APHP), Dr. P. Bataille (Centre Hospitalier de Boulogne sur mer), Dr. S. Bataille (APHM), Dr. S. Beneteau (CHU Nancy), Dr. S. Benoit (CHU Tours), Dr. L. Bessenay (CHU Clermont Ferrand), Dr. N. Biebuyck (APHP), Dr. K. Brochard (CHU Toulouse), Dr. F. Broux (CHU Rouen), Dr. M.C. Camoin-Schweitzer (CHU Nancy), Dr. M. Charbit (APHP), Dr. M.P. Cordier-Alex (Hospices civils de Lyon), Dr. C. Combe (CHU Bordeaux), Dr. B. Demeer (CHU Amiens), Dr. M. Dehnnault (CHU Lille), Dr. G. Deschênes (APHP), Dr. O. Dunan (CHU de la Réunion), Dr. A. Durrbach (APHP), Dr. S. Faguer (CHU Toulouse), Dr. E. Flori (CHU Strasbourg), Dr. A. Garnier (CHU Toulouse), Dr. L. Ghedira (CHU Monastir, Tunisia), Dr. S. Gié (CHU Rennes), Dr. A. Goldestein (CH du Mans), Dr. J.P. Grunfeld (APHP), Dr. F. Guiliano (CHU Nice), Dr. M. Holder (CHU Lille), Dr. A. Hummel (APHP), Dr. B. Isidor (CHU Nantes), Dr. M.L. Jacquemont (CHU La Réunion), Dr. P. Krug (APHP), Dr. M.P. Lavocat (CH Saint Etienne), Dr. V. Layet (CH Le Havre), Dr. D. Le Chapois (CH Bourges), Dr. V. Leroy (APHP), Dr. P. Lesavre (APHP), Dr. S. Manouvrier (CHU Lille), Dr. F. Martinez (APHP), Dr. K. Megri (CH Thonon les bains), Dr. J. Melki (APHP), Dr. E. Merieau (CHU Tours), Dr. B. Morel (CH Chambery), Dr. N. Noel (CHU Lille), Dr. S. Odent (CHU Rennes), Dr. V. Planquois (CH Dieppe), Dr. G. Plessis (CH Caen), Dr. C. Pouteil Noble (Hospices civils de Lyon), Dr. C. Rigothier (CHU Bordeaux), Dr. R. Salomon (APHP), Dr. S. Sigaudy (APHM), Dr. P. Simon (CH Saint Brieuc), Dr. A. Simon (CH Angers), Dr. N. Vittoz (CH Corbeil essones), Dr. M.A. Voelckel (APHM), and Dr. H. Weclawiak (CHU Clermont Ferrand).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2013080912/-/DCSupplemental.
References
- 1.Kashtan CE, Michael AF: Alport syndrome. Kidney Int 50: 1445–1463, 1996 [DOI] [PubMed] [Google Scholar]
- 2.Gretz N, Broyer M, Brunner FP, Brynger H, Donckerwolcke RA, Jacobs C, Kramer P, Selwood NH, Wing AJ: Alport’s syndrome as a cause of renal failure in Europe. Pediatr Nephrol 1: 411–415, 1987 [DOI] [PubMed] [Google Scholar]
- 3.Atkin CL, Gregory MC, Border WA: Alport syndrome. In: Diseases of the Kidney, edited by Schrier RW, Gottschalk CW, Boston, Little and Brown, 1988, pp 617–641 [Google Scholar]
- 4.Levy M, Feingold J: Estimating prevalence in single-gene kidney diseases progressing to renal failure. Kidney Int 58: 925–943, 2000 [DOI] [PubMed] [Google Scholar]
- 5.Kalluri R, Shield CF, Todd P, Hudson BG, Neilson EG: Isoform switching of type IV collagen is developmentally arrested in X-linked Alport syndrome leading to increased susceptibility of renal basement membranes to endoproteolysis. J Clin Invest 99: 2470–2478, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gunwar S, Ballester F, Noelken ME, Sado Y, Ninomiya Y, Hudson BG: Glomerular basement membrane. Identification of a novel disulfide-cross-linked network of alpha3, alpha4, and alpha5 chains of type IV collagen and its implications for the pathogenesis of Alport syndrome. J Biol Chem 273: 8767–8775, 1998 [DOI] [PubMed] [Google Scholar]
- 7.Longo I, Scala E, Mari F, Caselli R, Pescucci C, Mencarelli MA, Speciale C, Giani M, Bresin E, Caringella DA, Borochowitz ZU, Siriwardena K, Winship I, Renieri A, Meloni I: Autosomal recessive Alport syndrome: An in-depth clinical and molecular analysis of five families. Nephrol Dial Transplant 21: 665–671, 2006 [DOI] [PubMed] [Google Scholar]
- 8.van der Loop FT, Heidet L, Timmer ED, van den Bosch BJ, Leinonen A, Antignac C, Jefferson JA, Maxwell AP, Monnens LA, Schröder CH, Smeets HJ: Autosomal dominant Alport syndrome caused by a COL4A3 splice site mutation. Kidney Int 58: 1870–1875, 2000 [DOI] [PubMed] [Google Scholar]
- 9.Pescucci C, Mari F, Longo I, Vogiatzi P, Caselli R, Scala E, Abaterusso C, Gusmano R, Seri M, Miglietti N, Bresin E, Renieri A: Autosomal-dominant Alport syndrome: Natural history of a disease due to COL4A3 or COL4A4 gene. Kidney Int 65: 1598–1603, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Marcocci E, Uliana V, Bruttini M, Artuso R, Silengo MC, Zerial M, Bergesio F, Amoroso A, Savoldi S, Pennesi M, Giachino D, Rombolà G, Fogazzi GB, Rosatelli C, Martinhago CD, Carmellini M, Mancini R, Di Costanzo G, Longo I, Renieri A, Mari F: Autosomal dominant Alport syndrome: Molecular analysis of the COL4A4 gene and clinical outcome. Nephrol Dial Transplant 24: 1464–1471, 2009 [DOI] [PubMed] [Google Scholar]
- 11.Kashtan CE, Segal Y: Genetic disorders of glomerular basement membranes. Nephron Clin Pract 118: c9–c18, 2011 [DOI] [PubMed] [Google Scholar]
- 12.Gubler MC, Knebelmann B, Beziau A, Broyer M, Pirson Y, Haddoum F, Kleppel MM, Antignac C: Autosomal recessive Alport syndrome: Immunohistochemical study of type IV collagen chain distribution. Kidney Int 47: 1142–1147, 1995 [DOI] [PubMed] [Google Scholar]
- 13.Patey-Mariaud de Serre N, Garfa M, Bessiéres B, Noël LH, Knebelmann B: Collagen alpha5 and alpha2(IV) chain coexpression: Analysis of skin biopsies of Alport patients. Kidney Int 72: 512–516, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Tucker T, Marra M, Friedman JM: Massively parallel sequencing: The next big thing in genetic medicine. Am J Hum Genet 85: 142–154, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wei X, Ju X, Yi X, Zhu Q, Qu N, Liu T, Chen Y, Jiang H, Yang G, Zhen R, Lan Z, Qi M, Wang J, Yang Y, Chu Y, Li X, Guang Y, Huang J: Identification of sequence variants in genetic disease-causing genes using targeted next-generation sequencing. PLoS ONE 6: e29500, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rossetti S, Hopp K, Sikkink RA, Sundsbak JL, Lee YK, Kubly V, Eckloff BW, Ward CJ, Winearls CG, Torres VE, Harris PC: Identification of gene mutations in autosomal dominant polycystic kidney disease through targeted resequencing. J Am Soc Nephrol 23: 915–933, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCarthy HJ, Bierzynska A, Wherlock M, Ognjanovic M, Kerecuk L, Hegde S, Feather S, Gilbert RD, Krischock L, Jones C, Sinha MD, Webb NJ, Christian M, Williams MM, Marks S, Koziell A, Welsh GI, Saleem MA, RADAR the UK SRNS Study Group : Simultaneous sequencing of 24 genes associated with steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol 8: 637–648, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robinson JT, Thorvaldsdóttir H, Winckler W, Guttman M, Lander ES, Getz G, Mesirov JP: Integrative genomics viewer. Nat Biotechnol 29: 24–26, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Desmet FO, Hamroun D, Lalande M, Collod-Béroud G, Claustres M, Béroud C: Human Splicing Finder: An online bioinformatics tool to predict splicing signals. Nucleic Acids Res 37: e67, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jais JP, Knebelmann B, Giatras I, De Marchi M, Rizzoni G, Renieri A, Weber M, Gross O, Netzer KO, Flinter F, Pirson Y, Verellen C, Wieslander J, Persson U, Tryggvason K, Martin P, Hertz JM, Schröder C, Sanak M, Krejcova S, Carvalho MF, Saus J, Antignac C, Smeets H, Gubler MC: X-linked Alport syndrome: Natural history in 195 families and genotype- phenotype correlations in males. J Am Soc Nephrol 11: 649–657, 2000 [DOI] [PubMed] [Google Scholar]
- 21.Bekheirnia MR, Reed B, Gregory MC, McFann K, Shamshirsaz AA, Masoumi A, Schrier RW: Genotype-phenotype correlation in X-linked Alport syndrome. J Am Soc Nephrol 21: 876–883, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Longo I, Porcedda P, Mari F, Giachino D, Meloni I, Deplano C, Brusco A, Bosio M, Massella L, Lavoratti G, Roccatello D, Frascá G, Mazzucco G, Muda AO, Conti M, Fasciolo F, Arrondel C, Heidet L, Renieri A, De Marchi M: COL4A3/COL4A4 mutations: From familial hematuria to autosomal-dominant or recessive Alport syndrome. Kidney Int 61: 1947–1956, 2002 [DOI] [PubMed] [Google Scholar]
- 23.Gross O, Licht C, Anders HJ, Hoppe B, Beck B, Tönshoff B, Höcker B, Wygoda S, Ehrich JH, Pape L, Konrad M, Rascher W, Dötsch J, Müller-Wiefel DE, Hoyer P, Knebelmann B, Pirson Y, Grunfeld JP, Niaudet P, Cochat P, Heidet L, Lebbah S, Torra R, Friede T, Lange K, Müller GA, Weber M, Study Group Members of the Gesellschaft für Pädiatrische Nephrologie : Early angiotensin-converting enzyme inhibition in Alport syndrome delays renal failure and improves life expectancy. Kidney Int 81: 494–501, 2012 [DOI] [PubMed] [Google Scholar]
- 24.Artuso R, Fallerini C, Dosa L, Scionti F, Clementi M, Garosi G, Massella L, Epistolato MC, Mancini R, Mari F, Longo I, Ariani F, Renieri A, Bruttini M: Advances in Alport syndrome diagnosis using next-generation sequencing. Eur J Hum Genet 20: 50–57, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanson H, Storey H, Pagan J, Flinter F: The value of clinical criteria in identifying patients with X-linked Alport syndrome. Clin J Am Soc Nephrol 6: 198–203, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin P, Heiskari N, Zhou J, Leinonen A, Tumelius T, Hertz JM, Barker D, Gregory M, Atkin C, Styrkarsdottir U, Neumann H, Springate J, Shows T, Pettersson E, Tryggvason K: High mutation detection rate in the COL4A5 collagen gene in suspected Alport syndrome using PCR and direct DNA sequencing. J Am Soc Nephrol 9: 2291–2301, 1998 [DOI] [PubMed] [Google Scholar]
- 27.Boye E, Mollet G, Forestier L, Cohen-Solal L, Heidet L, Cochat P, Grünfeld JP, Palcoux JB, Gubler MC, Antignac C: Determination of the genomic structure of the COL4A4 gene and of novel mutations causing autosomal recessive Alport syndrome. Am J Hum Genet 63: 1329–1340, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heidet L, Arrondel C, Forestier L, Cohen-Solal L, Mollet G, Gutierrez B, Stavrou C, Gubler MC, Antignac C: Structure of the human type IV collagen gene COL4A3 and mutations in autosomal Alport syndrome. J Am Soc Nephrol 12: 97–106, 2001 [DOI] [PubMed] [Google Scholar]
- 29.Boye E, Vetrie D, Flinter F, Buckle B, Pihlajaniemi T, Hamalainen ER, Myers JC, Bobrow M, Harris A: Major rearrangements in the alpha 5(IV) collagen gene in three patients with Alport syndrome. Genomics 11: 1125–1132, 1991 [DOI] [PubMed] [Google Scholar]
- 30.Heidet L, Dahan K, Zhou J, Xu Z, Cochat P, Gould JD, Leppig KA, Proesmans W, Guyot C, Guillot M, Antignac C: Deletions of both alpha 5(IV) and alpha 6(IV) collagen genes in Alport syndrome and in Alport syndrome associated with smooth muscle tumours. Hum Mol Genet 4: 99–108, 1995 [DOI] [PubMed] [Google Scholar]
- 31.Boone PM, Soens ZT, Campbell IM, Stankiewicz P, Cheung SW, Patel A, Beaudet AL, Plon SE, Shaw CA, McGuire AL, Lupski JR: Incidental copy-number variants identified by routine genome testing in a clinical population. Genet Med 15: 45–54, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goossens D, Moens LN, Nelis E, Lenaerts AS, Glassee W, Kalbe A, Frey B, Kopal G, De Jonghe P, De Rijk P, Del-Favero J: Simultaneous mutation and copy number variation (CNV) detection by multiplex PCR-based GS-FLX sequencing. Hum Mutat 30: 472–476, 2009 [DOI] [PubMed] [Google Scholar]
- 33.Nagel M, Nagorka S, Gross O: Novel COL4A5, COL4A4, and COL4A3 mutations in Alport syndrome. Hum Mutat 26: 60–64, 2005 [DOI] [PubMed] [Google Scholar]
- 34.Yamazaki H, Nakagawa Y, Saito A, Nishi S, Sakatsume S, Takeda T, Maruyama Y, Ogino S, Maruyama S, Mochizuki T, Reeders ST, Arakawa M: No linkage to the COL4A3 gene locus in Japanese thin basement membrane disease families. Nephrology (Carlton) 1: 315–321, 1995 [Google Scholar]
- 35.Piccini M, Casari G, Zhou J, Bruttini M, Volti SL, Ballabio A, Renieri A: Evidence for genetic heterogeneity in benign familial hematuria. Am J Nephrol 19: 464–467, 1999 [DOI] [PubMed] [Google Scholar]
- 36.Flinter F: Alport’s syndrome. J Med Genet 34: 326–330, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gubler MC: Inherited diseases of the glomerular basement membrane. Nat Clin Pract Nephrol 4: 24–37, 2008 [DOI] [PubMed] [Google Scholar]
- 38.Arrondel C, Deschênes G, Le Meur Y, Viau A, Cordonnier C, Fournier A, Amadeo S, Gubler MC, Antignac C, Heidet L: A large tandem duplication within the COL4A5 gene is responsible for the high prevalence of Alport syndrome in French Polynesia. Kidney Int 65: 2030–2040, 2004 [DOI] [PubMed] [Google Scholar]
- 39.White SJ, Vink GR, Kriek M, Wuyts W, Schouten J, Bakker B, Breuning MH, den Dunnen JT: Two-color multiplex ligation-dependent probe amplification: Detecting genomic rearrangements in hereditary multiple exostoses. Hum Mutat 24: 86–92, 2004 [DOI] [PubMed] [Google Scholar]
- 40.Fallerini C, Dosa L, Tita R, Del Prete D, Feriozzi S, Gai G, Clementi M, La Manna A, Miglietti N, Mancini R, Mandrile G, Ghiggeri G, Piaggio G, Brancati F, Diano L, Frate E, Pinciaroli A, Giani M, Castorina P, Bresin E, Giachino D, De Marchi M, Mari F, Bruttini M, Renieri A, Ariani F: Unbiased next generation sequencing analysis confirms the existence of autosomal dominant Alport syndrome in a relevant fraction of cases [published online ahead of print September 4, 2013]. Clin Genet 10.1111/cge.122 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.