Abstract
In a previous trial, we found that combined 13-cis retinoic acid (13-cRA), interferon-α and α-tocopherol more effectively reversed advanced premalignant lesions of the larynx than of the oral cavity and that cyclin D1 (CD1)G/A870 single nucleotide polymorphism correlated with cancer risk. We conducted the present trial primarily to confirm the clinical activity of the combination in advanced laryngeal premalignancy and to confirm and extend our findings on CD1, both genotype and protein expression, in association with cancer risk in this setting. Twenty-seven moderate-to-severe laryngeal dysplasia patients underwent induction with combined 13-cRA daily, α-interferon twice weekly, and α-tocopherol daily for one year; 14 non-progressing patients then were randomized to maintenance fenretinide or placebo for two years. During induction, 2 patients had pathological complete responses, 6 had partial responses (30% overall response rate), and 5 developed laryngeal cancer. There were no significant differences between maintenance fenretinide and placebo in response or cancer rates. Ten patients developed cancer overall. Twenty-four patients were evaluated for the CD1 G/A870 genotype, and 23 for pre- and post-treatment CD1 protein expression. Consistent with our earlier report, shorter cancer-free survival was associated with the CD1 AA/AG genotype (p = 0.05). Extending our earlier work, high CD1 expression was associated with worse cancer-free survival overall (p= 0.04) and within each CD1 genotype group. These findings support CD1 genotype and protein expression as important risk markers for laryngeal cancer and suggest future trials targeting upstream regulators of CD1 transcription.
Keywords: Premalignant lesions, larynx, biochemoprevention, cyclin D1 genotype, cyclin D1 protein expression
Premalignant lesions of the head and neck (HN) are a useful model for evaluating strategies for chemoprevention of upper aerodigestive tract cancers (1). These lesions most often develop in association with exposure to tobacco and alcohol and frequently precede the development of invasive carcinoma (2). Although early premalignant HN lesions (hyperplasia and mild dysplasia) are commonly responsive to single-agent retinoid therapy (3, 4), advanced premalignant HN lesions (moderate-to-severe dysplasia) are resistant to retinoid monotherapy (3–5). The combination of retinoids and interferons (IFNs; biochemoprevention) enhances the induction of cell differentiation and suppression of cell proliferation (6–8) (9, 10). A clinical trial of combined 13-cis-retinoic acid (13-cRA), interferon-α (IFN-α), and α-tocopherol [on the basis of possible enhancement of activity and attenuation of retinoid toxicity (11, 12)], for 12 months in patients with oral and laryngeal premalignant lesions produced a high response rate of laryngeal lesions (13). In the original study, we also examined cyclin D1 (CD1) G/A870 single nucleotide polymorphism (SNP), gene amplification and protein expression. CD1 is key regulatory protein of the cell cycle and tissue homeostasis, and alterations of both its gene copy number and/or protein expression are frequently found in premalignancy and neoplasia. The CD1 G/A870 SNP is associated with two different splice variant transcripts, CD1a and CD1b. CD1a encodes for the full-length native form of the CD1 protein, which has a short nuclear half-life, tightly regulated by phosphorylation of residues in exon 5, followed by nuclear export and ubiquination (14). CD1b encodes for a truncated alternate CD1 protein, which lacks exon 5 and is a constitutively nuclear protein with enhanced oncogenic properties(14). The major translational findings were a correlation between CD1 AA or AG genotype and increased cancer risk (vs CD1 GG genotype) and a trend toward an association between modulation of CD1 protein expression and lesion response (15).
We designed the present randomized trial in two phases: induction with combined 13-cRA, IFN-α and αtocopherol to confirm the clinical/histologic activity of this regimen in patients with advanced premalignant lesions of the larynx, followed by maintenance with fenretinide (vs placebo) to prolong the chemopreventive effects. We chose the synthetic retinoid fenretinide for the maintenance phase because it has a different mechanism of action from that of the related compound 13-cRA, the potential to reverse persistent lesions (16–18), and a favorable toxicity profile (19). The major translational goal of this study was to prospectively confirm and extend the CD1 findings of our earlier trial.
Patients and Methods
Patient eligibility
All patients were required to provide signed informed consent prior to entering this randomized, double-blind, placebo-controlled, single-institution trial conducted at M. D. Anderson Cancer Center, where the trial protocol was approved by the Institutional Review Board. Eligibility included the following criteria: histologic evidence of moderate or severe dysplasia or carcinoma in situ of the larynx, no retinoid therapy within the 3 months prior to study entry, no prior history of invasive cancer for the 3 years preceding entry into the study, adequate bone marrow, hepatic, renal function and triglyceride level ≤2.5 the upper limit of normal. Patients with gastroesophageal or laryngopharyngeal reflux were treated with anti-reflux measures and esomeprazole or omeprazole for 2 months. Only patients that showed no signs of clinical improvement of their laryngeal lesion(s) along with symptomatic reflux improvement were eligible for inclusion in the study. Exclusion criteria included use of oral anticoagulants and severe intercurrent illness.
Evaluation and treatment plan
Pretreatment evaluation consisted of complete history and physical examination and detailed information on history of gastroesophageal reflux disease and a dietary questionnaire. Detailed alcohol and tobacco consumption information was obtained at baseline, and at months 6, 12, 24, and 36. All patients were counseled regarding smoking cessation and a proactive smoking cessation program was offered. Suspension laryngoscopy with videographic recording evaluation and biopsy was performed at baseline, months 12 and 36 and at any time patients developed symptoms (hoarseness) or clinical evidence of progression on laryngeal examination. The post-biopsy appearance of the vocal folds was recorded and stored such that the precise localization of the biopsy sites could be determined. Complete history and physical examination was performed every 3 months during the active intervention.
All patients received induction therapy consisting of IFN-α 2 million units (MU)/m2 subcutaneously twice a week (biw), daily 13-cRA (80mg/m2 orally) and daily α-tocopherol (1200 IU orally). Patients unable to tolerate the starting dose (toxicity grade ≥ 3) had the dose reduced to level minus 1 (IFN-α 1.5 MU/ m2 biw, 13-cRA 60 mg/ m2/day). Two additional dose reductions were implemented for recurrent toxicity grade ≥ 3: level minus 2 (IFN-α 1 MU/ m2 biw, 13-cRA 40 mg/ m2) and level minus 3 (IFN-α 0.75 MU/ m2 biw, 13-cRA 20 mg/ m2). After 12 months of induction therapy, responders and patients with stable disease were randomized (1:1) to daily fenretinide 200 mg orally or placebo for 24 months (maintenance phase). In case of ≥ grade-3 toxicity, drug would be stopped and the patient permanently taken off treatment; no dose reductions were implemented during the maintenance therapy phase. Patients were followed every 6 months for a minimum of 2 years after study completion.
Criteria for response and toxicity
Histological response definitions
Complete Response (CR) was defined as complete disappearance of dysplastic features with no clinically evident lesion, partial response (PR) as downgrading of dysplastic features from severe to moderate or from moderate to mild, stable disease (SD) as persistence of the same level of dysplasia after treatment and progressive disease (PD) as worsening of the degree of dysplasia from moderate to severe or from mild to moderate, or progression to invasive laryngeal cancer.
Clinical response definitions
CR was defined as disappearance of all measurable and evaluable lesions for at least one cycle of therapy or four weeks. PR was defined as 50% or greater decrease in the sum of the products of diameters of all measured lesions for at least 4 weeks; SD, stabilization of all existing lesions with no new lesions developing, no PD or less than partial response; PD, any increase of >25% in the sum of the products of diameters of any measurable lesion or in estimated size of non-measurable lesions or the appearance of an unequivocal new lesion or progression to invasive carcinoma. Clinical response was assessed by a speech pathologist (JL) performing the videostroboscopy, in conjunction with a medical oncologist (VP) and head and neck surgeon (JM) in a joint review of the videographic recording (Figure 1) resulting in a consensus decision on response.
Figure 1.
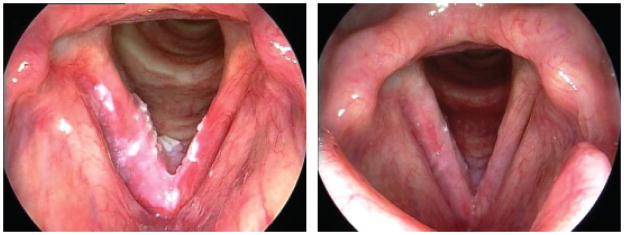
Left panel, Baseline laryngeal dysplasia involving both true vocal folds and immediate subglottis. Right panel, Near-complete resolution of laryngeal dysplasia post-treatment.
Toxicity was graded according to the NCI Common Toxicity Criteria (CTC) version 2.0, as well as previously published definitions of toxicities associated with treatment with retinoids (20).
Histopathologic evaluation
All biopsies (baseline, months 12 and 36) were evaluated for pathologic diagnosis from hematoxylin–eosin-stained slides. Unstained slides were prepared from formalin-fixed paraffin-embedded (FFPE) blocks were cut into 4-μm-thick sections and used for CD1 assessment. Histopathologic changes in tissue in response to the therapy were evaluated by a pathologist (AE-N) according to previously described criteria (13, 21).
CD1 genotype and protein assessments
Genomic DNA samples and target tissue lesions, including baseline and 12-month biopsies, were available for CD1 evaluation in 24 patients.
CD1 genotyping was performed using genomic DNA derived from peripheral blood lymphocytes using proteinase K, followed by isopropanol extraction and ethanol precipitation. The 870A genotype was assessed using the TaqMan SNP assay. The probes were labeled fluorescently with either 6-FAM or VIC on the 5′ end and a non-fluorescent minor grove binder (MGB) quencher on the 3′ end (Applied Biosystems). Primers and amplification conditions were previously described (22). The reactions were read using the ABI Prism 7900HT Sequence Detection system, and the analyzed fluorescence results were further called into genotypes (i.e. AA, AG, GG) using the built-in-software.
CD1 protein expression was evaluated using immunohistochemistry (IHC) on FFPE sections with a mouse monoclonal antibody (clone P2D11F11; Novocastra, Newcastle, United Kingdom) as previously reported (23). Only nuclear immunoreactivity was considered positive and the intensity of the staining was evaluated as: 0= no staining, 1=weak, 2=moderate, or 3=strong. Positive controls were placed on each section and negative controls were included in each IHC batch. For comparison with patient characteristics and clinical outcome, the results were expressed as the labeling index (LI) (i.e, the fraction of CD1 positive cells expressing a staining intensity ≥2); and the weighted mean index (WMI) (i.e, the sum of the intensity scale values (0 to 3) of each cell divided by the total number of evaluated cells) (15, 23). Two investigators (JGI, and TLC) evaluated CD1 immunolabeling in a blinded fashion and without knowledge of genotype, and clinical data. The final scores of each target tissue were calculated as the average score between the individual scores of each investigator. When the individual scores varied by more than 0.05, the cases were considered discrepant, were recounted and a final score was determined based on consensus of the two investigators.
Statistical analysis
Histological and clinical endpoints and analysis plan
The primary endpoint was histological response at 12 months. Secondary endpoints included clinical response, toxicity, comparing fenretinide with placebo in maintaining histological response, clinical responses in the induction and maintenance phases, and laryngeal cancer development.
We planned to enroll 100 eligible patients in the induction phase, based on an anticipated rate of response and stable disease of 80% and a standard error of 4%, thus 80 patients were expected to remain in progression-free status (i.e., with improved or stabilized histology of premalignant lesions) at 12 months and therefore eligible for the maintenance therapy. This sample size would be sufficient to detect a 30% difference in the relapse rate (histological PD after initial response or SD) (10% in the 4-HPR arm and 40% in the placebo arm) between the two groups with 80% power. The sample size calculation assumes a two-sided 5% type I error rate and a 5% lost-to-follow-up rate. The original study design included 3 years of accrual, 3 years of treatment and additional 2 years of follow-up.
CD1 analysis plan
To examine the relationship between CD1 genotype and clinical correlates, the analysis was conducted for two genotype forms (i.e., combined AA/AG and GG group), because of the biological functional dominant effect of the A allele (24). Fisher’s exact test and Wilcoxon rank sum tests were performed to examine the associations between clinical characteristics, CD1 genotype, CD1 expression, and response to treatment, when appropriate. To examine the relationship between CD1 protein expression and clinical correlates, CD1 expression was dichotomized into high and low expression based on the median of baseline LI and WMI values (CD1 expression vs response to intervention) and also on the mean of the baseline WMI values (CD1 expression and time to cancer). The cancer-free survival by CD1 genotypes (AA/AG vs GG) and CD1 WMI groups (high vs low) was estimated by Kaplan-Meier method and the difference was tested by Wald test when the robust sandwich estimate for covariance was used or log-rank test, when appropriate. Multicovariate Cox proportional hazards model was used to evaluate the effect of CD1 genotype and CD1 expression on cancer-free survival. P values ≤ 0.05 (two-sided) were considered to be statistically significant. Patients were pooled for these analyses as they all received uniform treatment during the induction period and the effect of fenretinide in the small subgroup of patients receiving fenretinide is considered negligible.
Results
Patients and treatment characteristics
We registered 40 patients from November 1, 1998, through May 30, 2004. Accrual was slow and did not allow for the projected number of patients to be entered into the randomized maintenance phase within the funding period of the trial. Thirty of the 40 registered patients were eligible for the trial, of which 27 began the 1-year induction phase and 3 refused to start treatment. As summarized in Table 1, patient characteristics included a predominance of males (59.3%) and current or former smokers (77.7%); no alcohol consumption in 66.7%; and gastroesophageal reflux in 96% of the patients.
Table 1.
Participants characteristics (N=27 patients who started induction therapy)
| Gender | |
| Female | 11 (40.7%) |
| Male | 16 (59.3%) |
|
| |
| Age | |
| Mean ± S. D.(Range) | 56.6 ± 10.7 (30.5, 75.3) |
|
| |
| Race | |
| White | 24 (88.9%) |
| Hispanic | 2 (7.4%) |
| Asian | 1 (3.7%) |
|
| |
| Cancer History | |
| No | 22 (81.5%) |
| Yes | 5 (18.5%) |
|
| |
| Previous Treatment for Cancer | |
| Radiation | 1 |
| Surgery | 3 |
| Radiation and Surgery | 1 |
|
| |
| Baseline Histology | |
| Moderate dysplasia | 14 (51.8%) |
| Severe dysplasia | 13 (48.1%) |
|
| |
| Smoking Status | |
| None | 6 (22.2%) |
| Former | 12 (44.4%) |
| Current | 9 (33.3%) |
|
| |
| Packs-Years, Mean ± S. D. (Range) | |
| Former | 39.9 ± 26.2 (5.0, 90.0) |
| Current | 44.6 ± 18.5 (22.5, 80.0) |
|
| |
| Smoking Quit Years for Former Smokers | |
| Mean±S.D. (Range) | 14.2 ± 8.8 (2.2, 26.4) |
|
| |
| Alcohol Usage | |
| None | 18 (66.7%) |
| Beer | 2 (7.4%) |
| Wine | 3 (11.1%) |
| Liquor | 3 (11.1%) |
| Unknown | 1 (3.7%) |
|
| |
| Reflux | |
| Present and treated | 26 (96.3%) |
| No reflux | 1 (3.7%) |
Eighteen patients completed the full 12-month course of induction therapy; 9 discontinued therapy because of disease progression (4 patients), patient preference [3], or toxicity [2]. Seventeen induction patients required dose reductions: 12 to dose-level minus 1, 4 to minus 2, and one to minus 3. Fifteen induction patients were eligible (responded or had SD) to proceed to the maintenance phase, and 14 were randomized to placebo (N=7) or fenretinide (N=7); 5 discontinued maintenance treatment because of disease progression (2 on placebo, 3 on fenretinide).
Histologic and clinical outcomes
Induction results are based on all 27 patients who entered the induction phase (tables 2 and 3). Two induction patients had histological CRs and 6 had PRs, for an overall response rate of 30%. Eight patients (30%) had SD, and 7 had PD (26%) (5 invasive laryngeal cancer and 2 worsening dysplasia). Four patients (15%) were inevaluable for the primary endpoint (early dropouts before response evaluation due to patient’s preference [2] or toxicity [2]; Table 2). There were no statistically significant differences in induction response rates according to gender, smoking status, or baseline histology (Table 3). Of the 23 evaluable patients 2 experienced clinical CR, 6 PR, 9 SD and 6 PD.
Table 2.
Histological response rates
| Response, N(%) | Induction Phase N=27 |
Maintenance Phase
|
|
|---|---|---|---|
| Placebo N=7 |
Fenretinide N=7 |
||
| CR | 2 (7%) | 2 (29%) | 1 (14%) |
| PR | 6 (22%) | 0 (0%) | 0 (0%) |
| SD | 8 (30%) | 2 (29%) | 1 (14%) |
| PD | 7 (26%) | 3 (43%) | 4 (57%) |
| INE | 4 (15%) | 0 (0%) | 1 (0%) |
Abbreviations: INE (inevaluable), CR (complete response), PD (progressive disease), PR (partial response), SD (stable disease)
Table 3.
Histological responses to induction therapy by patients characteristics (N=23, evaluable)
| Characteristic | Response, N(%)
|
P-value | ||
|---|---|---|---|---|
| CR/PR | SD | PD | ||
| Gender | ||||
| Female | 4(40%) | 3(30%) | 3(30%) | 1.00 |
| Male | 4 (30.8%) | 5 (38.5%) | 4 (30.8%) | |
|
| ||||
| Smoking Status | ||||
| None | 1(16.7%) | 1(16.7%) | 4(66.7%) | 0.058 |
| Former | 2 (20%) | 5 (50%) | 3 (30%) | |
| Current | 5 (71.4%) | 2 (28.6%) | 0 (0%) | |
|
| ||||
| Alcohol Usage | ||||
| None | 3 (20%) | 6 (40%) | 6 (40%) | 0.12 |
| Beer | 0(0%) | 1(50%) | 1(50%) | |
| Wine | 3 (100%) | 0 (0%) | 0 (0%) | |
| Liquor | 1 (50%) | 1 (50%) | 0 (0%) | |
|
| ||||
| Baseline Histology | ||||
| Moderate dysplasia | 3(25%) | 6(50%) | 3(25%) | 0.35 |
| Severe dysplasia | 5 (45.5%) | 2 (18.2%) | 4 (36.4%) | |
Abbreviations: CR (complete response), PD (progressive disease), PR (partial response), SD (stable disease)
The following histologic responses occurred during maintenance therapy (Table 2): 2 CRs, 2 SDs, 3 PDs (1 to invasive cancer and 2 to worsening dysplasia) in the placebo arm (N = 7); 1 CR, 1 SD, 4 PDs (3 to invasive cancer, and 1 to worsening dysplasia) and 1 patient was inevaluable due to poor quality of the biopsy obtained (clinical response: PR) in the fenretinide arm (N = 7). Clinical responses during the maintenance phase were 2 CR, 2 SD, 3 PD in the placebo arm and 1 CR, 1 PR, 1 SD and 4 PD in the fenretinide arm.
Overall (induction and maintenance), PD occurred in 14 of 27 patients, and 9 patients (33%) developed cancer, while one cancer developed after the treatment period. After a median follow-up of 5.1 years, the cancer-free survival rates are 84% (95% CI:71%, 99.7%) at 1 year and 63% (95% CI:46.9%, 85.7%) at 2 years; median progression-free survival is 2.74 years (95% CI: 1.33, NA); and progression-free survival rates are 76% (95% CI: 61.1%, 94.8%) at 1 year, 55% (95% CI: 38.7%, 79.1%) at 2 years, and 46% (95% CI: 29.8%, 71.4%) at 3 years. Median cancer-free survival has not yet been reached.
Toxicity
The highest-grade adverse event during the induction phase was grade 2 in 8 patients, grade 3 in 17 patients, and grade 4 in 1 patient; the most common adverse events were mucocutaneous toxicities related to retinoids (i.e. cheilitis, conjunctivitis, dry skin) hypertriglyceridemia and IFN-related arthralgia, fatigue, myalgia, anorexia, fever, chills and injection-site reactions (Table 4). The maintenance phase was better tolerated in both placebo and fenretinide groups, with 3 patients experiencing at least one grade 2 adverse event in each arm. No grade 3 or 4 toxicities were observed.
Table 4.
Selected adverse events by participants - Induction Phase (n=27)
| Toxicity | Grade (number of participants) | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Cheilitis | 6 | 19 | 2 | 0 |
| Dry skin | 13 | 14 | 0 | 0 |
| Conjunctivitis | 8 | 14 | 0 | 0 |
| Epistaxis | 11 | 0 | 0 | 0 |
| Hair changes | 5 | 1 | 0 | 0 |
| Hypertriglyceridemia | 11 | 9 | 5 | 1 |
| Pancreatitis | 0 | 0 | 1 | 0 |
| Fatigue | 7 | 17 | 2 | 0 |
| Myalgia | 11 | 10 | 2 | 0 |
| Arthralgia | 9 | 9 | 6 | 0 |
| Injection site reaction | 17 | 3 | 0 | 0 |
| Fever | 13 | 2 | 0 | 0 |
| Chills | 13 | 4 | 0 | 0 |
| Headache | 8 | 2 | 1 | 0 |
| Dizziness | 3 | 2 | 1 | 0 |
| Depression | 3 | 3 | 0 | 0 |
| Memory loss | 11 | 5 | 0 | 0 |
| Alopecia | 16 | 1 | 0 | 0 |
| Hyperglycemia | 9 | 5 | 2 | 0 |
| Leukopenia | 12 | 3 | 0 | 0 |
| Granulocytopenia | 6 | 7 | 2 | 0 |
| Anemia | 10 | 1 | 0 | 0 |
| Diarrhea | 5 | 3 | 1 | 0 |
| Nausea | 12 | 2 | 0 | 0 |
| Anorexia | 13 | 4 | 0 | 0 |
| Elevated alkaline phosphatase | 8 | 1 | 0 | 0 |
| Elevated alanine aminotrasferase (ALT) | 8 | 1 | 0 | 0 |
CD1 genotype, and protein expression at baseline
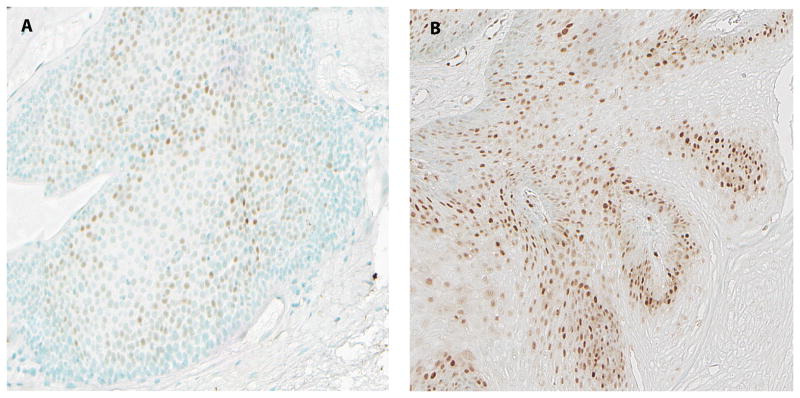
CD1 G/A870 genotype and protein expression were evaluated in 24 of the 27 patients that initiated induction therapy. Two patients carried the AA (8.3%) genotype, thirteen carried the AA/AG (54.2%) and 9 patients carried the GG (37.5%) genotype. The calculated allele frequency distributions were 35.4% for the A allele and 64.6% for the G allele. Because the AA and AG genotypes harbor similar clinical phenotypes (15, 23) the AA and AG genotypes were combined for clinical analyses. There were no statistically significant differences in the distribution of CD1 genotype (AA/AG vs GG) by gender, smoking status, and baseline degree of dysplasia. The percentages of CD1 positive cells and the levels of nuclear CD1 expression detected in the target tissues were similar in both genotype groups (LI, mean±SD: 0.21±0.21 for AA/AG vs 0.21±0.21for GG; p=0.77, MWI, mean±SD: 0.48±0.58 for AA/AG vs 0.32±0.44 for GG; p=0.95, Wilcoxon rank sum test) (Figure 2).
Figure 2.
CD1 protein expression detected by immunohistochemistry. (A) GG genotype: low nuclear expression; (B) AG genotype: high nuclear expression.
CD1 genotype, protein expression and response to intervention
None of the CD1 genotypes were associated with response to induction therapy (p=0.19, Fisher’s exact test), similarly neither the degree nor the level of CD1 expression at baseline was predictive of histologic response (p=0.61 for both LI and WMI, Wilcoxon rank sum test).
CD1 genotype, protein expression and cancer development
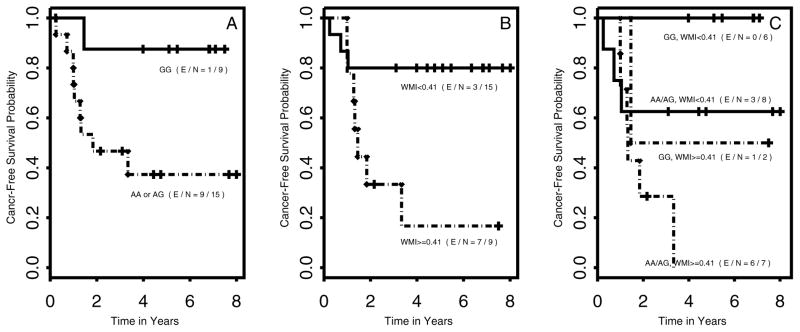
In univariate analysis, the CD1 AA/AG genotype was a significant predictor for shorter cancer-free survival compared to the GG group (HR; [95% confidence interval (CI)]: 7.21 [1.00, 52.06]; p=0.05). As shown in Figure 3A, the median time to cancer for patients with the AA or AG genotype was 1.84 years, while the median for the GG genotype has not been reached. High level of nuclear CD1 expression at baseline (cutoff value of 0.41, i.e. baseline CD1 WMI mean), was similarly a significant predictor of shorter cancer-free survival (HR [95%CI]: 4.58 [1.10, 19.14]; p=0.04) in univariate analysis. The median time to cancer for patients with baseline CD1 WMI ≥0.41 was 1.45 years while it was not reached for patients with baseline CD1 WMI<0.41 (Figure 3B). Notably, high CD1 expression was also associated with worse outcome within each genotype group (Figure 3C). In the AA/AG high-cancer risk group: 6 out of the 7 (85.7%) patients with baseline CD1 WMI ≥0.41 developed cancer compared to 3 of the 8 (37.5%) patients with <0.41. Similarly, in the GG group: 1 of the 2 (50%) patients with baseline CD1 WMI ≥0.41 developed cancer, compared to none with CD1 WMI <0.41.
Figure 3.
A, Cancer-free survival by cyclin D1 870A genotype. The difference between the groups AA or AG vs GG was tested by Wald test, p=0.05. E = number of events, N = total number of patients per arm. B, Cancer-free survival by cyclin D1 protein expression using weighted mean index (WMI) cut-off of 0.41, (Wald test, p=0.04). C. Cancer-free survival by CD1 G870A genotype stratified by CD1 protein expression using weighted mean index (WMI) cut-off of 0.41. (log-rank test comparing CD1 ≥ 0.41 vs <0.41, p=0.08 for GG group and p=0.17 for AA/AG group, overall log-rank test p=0.04) E = number of events, N = total number of patients per arm.
In a multicovariate analysis evaluating the effect of both CD1 genotype and baseline protein expression on time to cancer,similar to the univariate analysis trends were observed; the hazard ratio for the level of CD1 nuclear expression ≥0.41 was 3.51 (95%CI: [0.78, 15.83], p=0.10) and for CD1 AA/AG genotype was 5.54 (95% CI: [0.83, 37.09], p=0.08).
Discussion
The overall 30% response rate (regression of laryngeal lesions) during induction was substantially lower than that of the laryngeal lesions in our earlier trial of this regimen (64% at 12 months) (13). This difference may reflect the exclusion of approximately one-third of the patients screened for the study because their gastroesophageal reflux improved with anti-reflux measures and medications. In fact, several observational studies have described reversal of carcinoma-in situ with treatment of reflux (25, 26) as well as regression of premalignant changes and decreased incidence of cancer recurrences after initiating H2-receptor antagonists (27), and a meta-analysis suggests that GERD may be a factor in the pathogenesis of laryngeal cancer. (28) Our previous trial could have been biased by including patients with lesions responsive to gastroesophageal-reflux control alone. Therefore, future trials in laryngeal premalignancy patients should control for a concurrent diagnosis and/or treatment of gastroesophageal reflux.
Cancers developed in 37% of the present study’s patients, close to the expected (historical) incidence of cancer in this setting (27, 29–31). Half of the cancers occurred during induction, half occurred after, suggesting little or no effect of induction or maintenance on laryngeal cancer development in these patients. In sum, the two-phase regimen did not prevent laryngeal cancer despite objective responses of premalignant laryngeal lesions. This result contrasts with results of a phase II trial of combined 13-cRA, IFN-α and α-tocopherol to prevent new cancer in curatively treated stage III–IV HNSCC patients (32); the regimen produced remarkable 5-year rates of overall survival (79%) and disease-free survival (80%) confirmed by longer-term follow-up (33).
We believe that the present findings with the greatest implications for head and neck cancer prevention involve CD1 genotype and protein expression. The current study confirmed the increased risk of cancer in patients with the CD1 AA and AG genotype (vs the GG genotype) detected in the earlier study but also added important new findings. Baseline expression of CD1 protein correlated with cancer risk within both the unfavorable and favorable CD1 genotypes. Interestingly neither the level of CD1 protein expression nor the genotype correlated with lesion response. This finding raises again the issue of the validity of premalignant lesion response as a surrogate for cancer development as has been recently observed in a large chemoprevention trial in oral premalignancy. (34)
The CD1 G/A870 polymorphism is functionally important since it is occurring at a splicing donor site, resulting in two different splice variant transcripts, CD1a and CD1b. CD1a encodes for the full-length native form of the CD1 protein, which has a short nuclear half-life and is tightly regulated by phosphorylation of residues in exon 5, following which it undergoes nuclear export and ubiquination. CD1b encodes for a truncated alternate CD1 protein, which lacks exon 5 and has a longer nuclear half-life (14). Although the mechanisms underlying the regulation of splicing at the 870 site are not fully characterized, the A870 allele impairs the normal splicing, and enhances the production of CD1b, which appears to hold oncogenic properties (14). At the time of the present study, there were no specific antibodies to CD1b. Therefore, we used an antibody that detects both CD1 forms and presented our data in two different ways, LI and WMI, the latter reflecting more accurately the levels of protein expression. As in our previous report (15), the A870 (i.e., AA and AG genotypes) background was associated with a significantly shorter cancer-free survival and modulation of CD1 expression (downregulation from baseline levels) was significantly associated with phenotypic reversal of the target lesions. The novel finding of the present study, however, is the prognostic significance of high baseline CD1 expression, which appears to have the strongest association with an increased risk of cancer and impacts both CD1 genotype groups. Although limited by a small sample size, our results suggest that baseline nuclear CD1 levels may be useful in identifying the shortest cancer-free survival within high-risk patients having CD1 AA or AG genotypes. A recent case-control study also found that CD1 genotype correlated with head and neck cancer risk (35). Validation of the findings in a larger cohort and utilizing an antibody detecting the oncogenic CD1b is certainly warranted.
In conclusion, the combination of 13-cRA, alpha-IFN and alpha-tocopherol had modest activity in advanced laryngeal premalignancy. Our current CD1 findings add to our understanding of the biology of head and neck carcinogenesis and cancer risk and should be integrated along with other high-risk molecular characteristics [e.g. loss of heterozygosity at 9p and 3p, (36) and chromosome instability (37)] in the screening of patients suitable for intervention. We believe that the present results warrant future molecular-targeted prevention trials of an agent or combination that can target upstream regulators of CD1 transcription and protein expression in patients selected for a high risk of head and neck cancer based on their CD1 genotype and protein profile. With the personalizing aspects of high risk (38) and medicine targeting a component of this risk, such a trial promises to advance personalized cancer prevention in the head and neck.
Acknowledgments
Grant support: Supported by the National Cancer Institute, NIH, Department of Health and Human Services grant U01-CA-79437-01
References
- 1.Lippman SM, Benner SE, Hong WK. Chemoprevention. Strategies for the control of cancer. Cancer. 1993;72(3 Suppl):984–90. doi: 10.1002/1097-0142(19930801)72:3+<984::aid-cncr2820721306>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 2.Silverman S, Jr, Gorsky M, Lozada F. Oral leukoplakia and malignant transformation. A follow-up study of 257 patients. Cancer. 1984;53(3):563–8. doi: 10.1002/1097-0142(19840201)53:3<563::aid-cncr2820530332>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 3.Hong WK, Endicott J, Itri LM, et al. 13-cis-retinoic acid in the treatment of oral leukoplakia. N Engl J Med. 1986;315(24):1501–5. doi: 10.1056/NEJM198612113152401. [DOI] [PubMed] [Google Scholar]
- 4.Lippman SM, Batsakis JG, Toth BB, et al. Comparison of low-dose isotretinoin with beta carotene to prevent oral carcinogenesis. N Engl J Med. 1993;328(1):15–20. doi: 10.1056/NEJM199301073280103. [DOI] [PubMed] [Google Scholar]
- 5.Smith MA, Parkinson DR, Cheson BD, Friedman MA. Retinoids in cancer therapy. J Clin Oncol. 1992;10(5):839–64. doi: 10.1200/JCO.1992.10.5.839. [DOI] [PubMed] [Google Scholar]
- 6.Lindner DJ, Borden EC, Kalvakolanu DV. Synergistic antitumor effects of a combination of interferons and retinoic acid on human tumor cells in vitro and in vivo. Clin Cancer Res. 1997;3(6):931–7. [PubMed] [Google Scholar]
- 7.Lingen MW, Polverini PJ, Bouck NP. Retinoic acid and interferon alpha act synergistically as antiangiogenic and antitumor agents against human head and neck squamous cell carcinoma. Cancer Res. 1998;58(23):5551–8. [PubMed] [Google Scholar]
- 8.Pelicano L, Li F, Schindler C, Chelbi-Alix MK. Retinoic acid enhances the expression of interferon-induced proteins: evidence for multiple mechanisms of action. Oncogene. 1997;15(19):2349–59. doi: 10.1038/sj.onc.1201410. [DOI] [PubMed] [Google Scholar]
- 9.Lippman SM, Kavanagh JJ, Paredes-Espinoza M, et al. 13-cis-retinoic acid plus interferon alpha-2a: highly active systemic therapy for squamous cell carcinoma of the cervix. J Natl Cancer Inst. 1992;84(4):241–5. doi: 10.1093/jnci/84.4.241. [DOI] [PubMed] [Google Scholar]
- 10.Lippman SM, Parkinson DR, Itri LM, et al. 13-cis-retinoic acid and interferon alpha-2a: effective combination therapy for advanced squamous cell carcinoma of the skin. J Natl Cancer Inst. 1992;84(4):235–41. doi: 10.1093/jnci/84.4.235. [DOI] [PubMed] [Google Scholar]
- 11.Besa EC, Abrahm JL, Bartholomew MJ, Hyzinski M, Nowell PC. Treatment with 13-cis-retinoic acid in transfusion-dependent patients with myelodysplastic syndrome and decreased toxicity with addition of alpha-tocopherol. Am J Med. 1990;89(6):739–47. doi: 10.1016/0002-9343(90)90215-y. [DOI] [PubMed] [Google Scholar]
- 12.Dimery IW, Hong WK, Lee JJ, et al. Phase I trial of alpha-tocopherol effects on 13-cis-retinoic acid toxicity. Ann Oncol. 1997;8(1):85–9. doi: 10.1023/a:1008209525671. [DOI] [PubMed] [Google Scholar]
- 13.Papadimitrakopoulou VA, Clayman GL, Shin DM, et al. Biochemoprevention for dysplastic lesions of the upper aerodigestive tract. Archives of otolaryngology--head & neck surgery. 1999;125(10):1083–9. doi: 10.1001/archotol.125.10.1083. [DOI] [PubMed] [Google Scholar]
- 14.Lu F, Gladden AB, Diehl JA. An alternatively spliced cyclin D1 isoform, cyclin D1b, is a nuclear oncogene. Cancer Res. 2003;63(21):7056–61. [PubMed] [Google Scholar]
- 15.Izzo JG, Papadimitrakopoulou VA, Liu DD, et al. Cyclin D1 genotype, response to biochemoprevention, and progression rate to upper aerodigestive tract cancer. J Natl Cancer Inst. 2003;95(3):198–205. doi: 10.1093/jnci/95.3.198. [DOI] [PubMed] [Google Scholar]
- 16.Delia D, Aiello A, Lombardi L, et al. N-(4-hydroxyphenyl)retinamide induces apoptosis of malignant hemopoietic cell lines including those unresponsive to retinoic acid. Cancer Res. 1993;53(24):6036–41. [PubMed] [Google Scholar]
- 17.Lotan R. Retinoids and apoptosis: implications for cancer chemoprevention and therapy. J Natl Cancer Inst. 1995;87(22):1655–7. doi: 10.1093/jnci/87.22.1655. [DOI] [PubMed] [Google Scholar]
- 18.Oridate N, Lotan D, Xu XC, Hong WK, Lotan R. Differential induction of apoptosis by all-trans-retinoic acid and N-(4-hydroxyphenyl)retinamide in human head and neck squamous cell carcinoma cell lines. Clin Cancer Res. 1996;2(5):855–63. [PubMed] [Google Scholar]
- 19.Rotmensz N, De Palo G, Formelli F, et al. Long-term tolerability of fenretinide (4-HPR) in breast cancer patients. Eur J Cancer. 1991;27(9):1127–31. doi: 10.1016/0277-5379(91)90309-2. [DOI] [PubMed] [Google Scholar]
- 20.Meyskens FJ, Goodman G, Alberts D. 13-Cis-retinoic avid: pharmacology, toxicology, and clinical applications for the prevention and treatment of human cancer. Crit Rev Oncol Hematol. 1985;(3):75–101. doi: 10.1016/s1040-8428(85)80040-8. [DOI] [PubMed] [Google Scholar]
- 21.Shin DM, Mao L, Papadimitrakopoulou VM, et al. Biochemopreventive therapy for patients with premalignant lesions of the head and neck and p53 gene expression. J Natl Cancer Inst. 2000;92(1):69–73. doi: 10.1093/jnci/92.1.69. [DOI] [PubMed] [Google Scholar]
- 22.Huang M, Spitz MR, Gu J, et al. Cyclin D1 gene polymorphism as a risk factor for oral premalignant lesions. Carcinogenesis. 2006;27(10):2034–7. doi: 10.1093/carcin/bgl048. [DOI] [PubMed] [Google Scholar]
- 23.Izzo JG, Wu TT, Wu X, et al. Cyclin D1 guanine/adenine 870 polymorphism with altered protein expression is associated with genomic instability and aggressive clinical biology of esophageal adenocarcinoma. J Clin Oncol. 2007;25(6):698–707. doi: 10.1200/JCO.2006.08.0283. [DOI] [PubMed] [Google Scholar]
- 24.Betticher DC, Thatcher N, Altermatt HJ, Hoban P, Ryder WD, Heighway J. Alternate splicing produces a novel cyclin D1 transcript. Oncogene. 1995;11(5):1005–11. [PubMed] [Google Scholar]
- 25.Richtsmeier WJ, Eisele D. In vivo anergy reversal with cimetidine in patients with cancer. Archives of otolaryngology--head & neck surgery. 1986;112(10):1074–7. doi: 10.1001/archotol.1986.03780100062009. [DOI] [PubMed] [Google Scholar]
- 26.Richtsmeier WJ, Rothman W. Reflux as an etiologic factor of carcinoma of the laryngopharynx. The Laryngoscope. 1989;99(6 Pt 1):666. doi: 10.1288/00005537-198906000-00021. [DOI] [PubMed] [Google Scholar]
- 27.Freije JE, Beatty TW, Campbell BH, Woodson BT, Schultz CJ, Toohill RJ. Carcinoma of the larynx in patients with gastroesophageal reflux. Am J Otolaryngol. 1996;17(6):386–90. doi: 10.1016/s0196-0709(96)90071-x. [DOI] [PubMed] [Google Scholar]
- 28.Qadeer MA, Colabianchi N, Vaezi MF. Is GERD a risk factor for laryngeal cancer? The Laryngoscope. 2005;115(3):486–91. doi: 10.1097/01.mlg.0000157851.24272.41. [DOI] [PubMed] [Google Scholar]
- 29.Hojslet PE, Nielsen VM, Palvio D. Premalignant lesions of the larynx. A follow-up study. Acta Otolaryngol. 1989;107(1–2):150–5. doi: 10.3109/00016488909127492. [DOI] [PubMed] [Google Scholar]
- 30.Miller AH, Fisher HR. Clues to the life history of carcinoma in situ of the larynx. The Laryngoscope. 1971;81(9):1475–80. doi: 10.1288/00005537-197109000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Zeitels SM. Premalignant epithelium and microinvasive cancer of the vocal fold: the evolution of phonomicrosurgical management. The Laryngoscope. 1995;105(3 Pt 2):1–51. doi: 10.1288/00005537-199503001-00001. [DOI] [PubMed] [Google Scholar]
- 32.Shin DM, Khuri FR, Murphy B, et al. Combined interferon-alfa, 13-cis-retinoic acid, and alpha-tocopherol in locally advanced head and neck squamous cell carcinoma: novel bioadjuvant phase II trial. J Clin Oncol. 2001;19(12):3010–7. doi: 10.1200/JCO.2001.19.12.3010. [DOI] [PubMed] [Google Scholar]
- 33.Seixas-Silva JA, Jr, Richards T, Khuri FR, et al. Phase 2 bioadjuvant study of interferon alfa-2a, isotretinoin, and vitamin E in locally advanced squamous cell carcinoma of the head and neck: long-term follow-up. Archives of otolaryngology--head & neck surgery. 2005;131(4):304–7. doi: 10.1001/archotol.131.4.304. [DOI] [PubMed] [Google Scholar]
- 34.Papadimitrakopoulou V, Lee J, William W, et al. Randomized trial of 13-cis retinoic acid versus retinyl palmitate with or without beta-carotene in oral premalignancy. J Clin Oncol. 2008 doi: 10.1200/JCO.2008.17.1850. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marsit CJ, Black CC, Posner MR, Kelsey KT. A genotype-phenotype examination of cyclin D1 on risk and outcome of squamous cell carcinoma of the head and neck. Clin Cancer Res. 2008;14(8):2371–7. doi: 10.1158/1078-0432.CCR-07-4368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mao L, El-Naggar AK, Papadimitrakopoulou V, et al. Phenotype and genotype of advanced premalignant head and neck lesions after chemopreventive therapy. J Natl Cancer Inst. 1998;90(20):1545–51. doi: 10.1093/jnci/90.20.1545. [DOI] [PubMed] [Google Scholar]
- 37.Veltman JA, Bot FJ, Huynen FC, Ramaekers FC, Manni JJ, Hopman AH. Chromosome instability as an indicator of malignant progression in laryngeal mucosa. J Clin Oncol. 2000;18(8):1644–51. doi: 10.1200/JCO.2000.18.8.1644. [DOI] [PubMed] [Google Scholar]
- 38.Lippman SM, Heymach JV. The convergent development of molecular-targeted drugs for cancer treatment and prevention. Clin Cancer Res. 2007;13(14):4035–41. doi: 10.1158/1078-0432.CCR-07-0063. [DOI] [PubMed] [Google Scholar]