Abstract
Ebolaviruses cause a severe hemorrhagic fever syndrome that is rapidly fatal to humans and non-human primates. Ebola protein interactions with host cellular proteins disrupt Type I and Type II interferon responses, RNAi anti-viral responses, antigen presentation, T-cell mediated antibody responses, humoral antibodies and cell mediated immunity. This multifaceted approach to evasion and suppression of innate and adaptive immune responses in their target hosts leads to the severe immune dysregulation and “cytokine storm” that is characteristic of fatal ebolavirus infection. Here we highlight some of the processes by which Ebola interacts with its mammalian hosts to evade anti-viral defenses.
Introduction
The Filoviridae family consists of three genera: Marburgvirus, Ebolavirus and the newly identified Cuevavirus. Within the Ebolavirus genus, there are five species including Zaire ebolavirus, Sudan ebolavirus, Bundibugyo ebolavirus, Tai Forest ebolavirus and Reston ebolavirus. Filoviruses were first identified as the causative agent of a hemorrhagic fever syndrome in Marburg, Germany in 1967. Nine years later, the first two ebolaviruses were described in the Democratic Republic of Congo (formerly Zaire) and Sudan. Since then, over 30 Ebola virus disease outbreaks have infected thousands with a mean case fatality rate of around 65% in humans (Hartman et al., 2010). The recent Ebola virus disease outbreak in West Africa began in March of 2014 and has thus far caused >7500 confirmed and probable cases with a case fatality rate of about 50% (for latest information see: http://www.who.int/csr/disease/ebola/en/).
Virus Life Cycle
Ebola particles are enveloped, filamentous, and contain a monopartite negative-sense RNA genome. While Ebola initially targets macrophages and dendritic cells it is able to infect almost all cell types with the exception of lymphocytes (Wool-Lewis and Bates, 1998). Virus particles have been proposed to attach to host cells through multiple plasma membrane surface-expressed proteins (e.g., C-type lectins, DC-SIGN, integrins, TIM-1, Axl) (Alvarez et al., 2002; Baribaud et al., 2002; Kondratowicz et al., 2011; Lin et al., 2003; Schornberg et al., 2009; Shimojima et al., 2006; Simmons et al., 2003; Takada et al., 2000). Once attached to the plasma membrane, the viral envelope glycoprotein induces particle uptake via macropinocytosis. The induction of macropinocytosis appears to be dependent on the action of cell surface proteins, including TIM-1 and Axl (Aleksandrowicz et al., 2011; Brindley et al., 2011; Hunt et al., 2011; Moller-Tank et al., 2013; Mulherkar et al., 2011; Nanbo et al., 2010; Quinn et al., 2009; Saeed et al., 2010; Shimojima et al., 2007, 2006; Wen et al., 2013). After uptake into macropinosomes, particles travel to low pH compartments of late endosomes and lysosomes where the viral envelope glycoprotein (GP) is proteolytically cleaved by endosomal cysteine proteases (i.e., cathepsin B and L). This cleavage removes a heavily glycosylated region from GP (Chandran et al., 2005; Dube et al., 2009; Hood et al., 2010; Misasi et al., 2012; Schornberg et al., 2006) and exposes a domain in GP that binds specifically to the endosomal/lysosomal resident filovirus receptor Niemann-Pick C1 protein (NPC1) (Carette et al., 2011; Côté et al., 2011). While current evidence suggests that NPC1 binding may be sufficient to trigger fusion of the viral and cellular membranes (Miller et al., 2012), it is as yet unclear whether additional host proteins or intracellular conditions are necessary (e.g., reducing conditions, altered pH, additional protease cleavage) (Brecher et al., 2011; Chandran et al., 2005).
Once the viral and internal cell membranes fuse, the virus particle uncoats and its anti-genome is transcribed into mRNA using nucleocapsid-associated viral proteins. The virus genome consists of seven viral genes, VP24, the nucleoprotein (NP), VP30, VP35, the matrix protein (VP40), the RNA-dependent RNA polymerase (L) and the glycoprotein gene, which are transcribed into mRNA resulting in the production of at least ten proteins. Transcription of the genome is mediated via a complex of VP30, VP35 and the viral polymerase L bound to an NP-coated genome (Bharat et al., 2012; Hartlieb et al., 2003, 2007; Modrof et al., 2003; Mühlberger et al., 1999; Sanchez and Kiley, 1987; Sanchez et al., 1993). VP30 phosphorylation leads to its dissociation from the VP35/L complex and is the signal to switch from transcription to replication (Biedenkopf et al., 2013; Martinez et al., 2011a). Following this switch, virus genomes are replicated and coated by NP, VP24, VP30 and VP35 (Mühlberger et al., 1999). During assembly, L associates with the ribonucleoprotein complex via an interaction withVP35. The ribonucleoproteins then associate with the matrix protein VP40 and viral particles are extruded through the plasma membrane within lipid raft microdomain regions (Stahelin, 2014).
Sneaking in with the Trash: Apoptotic mimicry
Ebolavirus particles can be up to a micron in length, making it difficult for the viruses to enter via classic clathrin or caveolin mediated endocytosis pathways. Recent evidence using pseudotyped viruses, virus-like particles and infectious Ebola particles suggests that after attachment to the plasma membrane, ebolavirus induces macropinocytosis in a process that is enhanced by the presence of TIM-1 and Axl (Hunt et al., 2011; Moller-Tank et al., 2013; Mulherkar et al., 2011; Nanbo et al., 2010; Quinn et al., 2009; Saeed et al., 2010; Shimojima et al., 2006). Interestingly, an increased amount of phosphatidylserine (PS) may be present on the surface of Ebola virus-like particles (Jemielity et al., 2013; Moller-Tank et al., 2013). PS is a lipid primarily present on the inner leaflet of plasma membranes (Zachowski, 1993). Upon cell death via apoptosis, PS is exposed to the outer leaflets of plasma membranes and apoptotic bodies. This alerts nearby cells, including phagocytic cells, to begin “eating” the debris via macropinocytosis in a process that is mediated by TIM-1 and Axl, and does not induce an inflammatory response (Biermann et al., 2013; Morizono and Chen, 2014; Zagórska et al., 2014). This suggests the possibility that, similar to other large viruses such as vaccinia virus (Mercer and Helenius, 2008), Ebola may induce macropinocytic uptake by appearing to be an apoptotic body to phagocytic cells. This “apoptotic mimicry” is anti-inflammatory and induces rapid uptake of a large virus into cells, thus avoiding humoral and cell surface immunity factors.
Snipping the Alarm-wire: Preventing the interferon alarm
Evasion of cellular innate immune responses is of particular importance to viruses and many have evolved mechanisms to circumvent innate immunity. Ebola inhibits both Type I and Type II interferon responses in target cells, especially macrophages, monocytes and dendritic cells. The ultimate result is a defect in dendritic cell maturation and diminished T-cell activation and proliferation along with apoptosis leading to lymphopenia, a key characteristic of Ebola virus disease. Studies in animal models and in tissue culture suggest that both pathogenesis and interferon antagonism are linked to VP35 and VP24 (Cilloniz et al., 2011; Ebihara et al., 2006; Hartman et al., 2008a, 2008b; Mateo et al., 2011; Prins et al., 2010; Reid et al., 2007).
VP35
VP35 is a viral polymerase cofactor that functions in RNA synthesis and has been proposed to link L to NP. In addition to these roles, VP35 plays a prominent role in Ebola’s inhibition of alpha and beta interferon induction through multiple mechanisms.
RIG-I and MDA-5 are innate pattern recognition receptors that detect foreign cytosolic RNA. RIG-I recognizes 5′-triphosphates of blunt-ended RNA and MDA-5 senses long double stranded RNA (dsRNA). Both signal via the downstream adapter IPS-1 (a.k.a. MAVS, VISA, Cardif) resulting in NF-κB, IRF-3 and IRF-7 activation and subsequent expression of Type-I interferon and pro-inflammatory cytokines. Activation of IRF-3/7 is the result of a signal cascade through which they are phosphorylated by TANK-binding kinase 1 (TBK-1) and IκB kinase-ε (IKKε) (Chiang et al., 2014). Early experiments determined that VP35 disrupted the RIG-I pathway by preventing IRF-3 phosphorylation (Basler et al., 2000, 2003). Later, VP35 was shown to interact with the N-terminal kinase domain of IKKε in preventing IRF-3 phosphorylation and acting as a decoy substrate for IKKε/TBK-1 kinases. Furthermore, binding of VP35 to IKKε prevents interactions with other proteins, including IRF-7 and IPS-1 (Prins et al., 2009). The net result of these interactions is inhibition of the induction of genes with interferon response promoters.
In addition to these downstream events in the RIG-I pathway, VP35 interacts with dsRNA to prevent RIG-I and MDA-5 responses (Cárdenas et al., 2006). Structural and biochemical studies revealed that VP35 contains a C-terminal interferon inhibitory domain (IID) with two clusters of basic amino acids. One cluster centers on residue R312 and participates in binding to dsRNA. Further analysis revealed that VP35 binds to blunt ended dsRNA in a manner very similar to that seen with RIG-I (Cárdenas et al., 2006; Leung et al., 2009, 2010a). Structural studies of VP35 dsRNA binding are consistent with the finding that VP35 prevents both RIG-I and MDA-5 responses. Observations from RNA bound and unbound structures revealed that VP35 is able to bind both the phosphate backbone of dsRNA and end-capped RNA in VP35 dimers. Mutations of the basic patch centering on R312 abrogate dsRNA binding and structural analysis suggests that R312 mutations disrupt VP35 dimerization (Kimberlin et al., 2010). Experiments using recombinant viruses incorporating mutant VP35R312A showed attenuation of virulence and impairment of both virus growth and interferon antagonism, suggesting that IID binding to dsRNA and VP35 dimerization play a key roles in the virus life cycle and pathogenesis (Hartman et al., 2008a, 2008b; Kimberlin et al., 2010; Prins et al., 2010).
Interestingly, comparisons of VP35 IID from the pathogenic Zaire ebolavirus and Reston ebolavirus, thus far only pathogenic in monkeys, revealed a slight decrease in interferon antagonism and dsRNA binding by Reston. However, these decreases did not appear to contribute significantly to the differences in virulence between the Zaire and Reston viruses (Leung et al., 2010b). Furthermore, comparison of the structures of the Zaire and Reston VP35 did not reveal substantial differences between the dsRNA recognition mechanisms (Kimberlin et al., 2010). Together, these data suggest additional viral factors likely play a role in the differential host responses between these two viruses.
Recently, VP35 was found to interact with the PKR Activator (PACT) (Fabozzi et al., 2011). In addition to having activity in RNA silencing and PKR activation, PACT also binds to and activates RIG-I. Subsequent work showed that VP35 binding to PACT prevents PACT binding to RIG-I and inhibits RIG-I activation (Luthra et al., 2013). VP35 binding to PACT is mediated via the same central basic patch in IID that abrogates dsRNA binding described above, suggesting a possible role for dsRNA in this interaction. Surprisingly, PACT interaction with VP35 inhibits the binding of VP35 with L, causing a decreased efficiency of viral RNA synthesis and genome replication, a phenotype of “mutual antagonism”(Luthra et al., 2013). Taken together with previous data, these experiments point to the critical importance of VP35 antagonism of the RIG-I pathway during ebolavirus infection.
Additional VP35 interactions with cellular proteins have been explored using a yeast 2-hybrid system. These studies found that VP35 interacts with IRF-7, Ubc9 and PIAS1 (Chang et al., 2009). Ubc-9 and PIAS1 are key components of the small ubiquitin-related modifier (SUMO) system of post-translational modification, which regulates a variety of cellular pathways and proteins. During SUMOylation, SUMO proteins are activated by SUMO-specific proteases and transferred to a SUMO conjugating E2 enzyme (e.g., Ubc9). Next, an E3 ligase, such as PIAS1, is used to transfer the SUMO domain to a lysine on the target protein (Wimmer et al., 2012). Studies with Ebola VP35 found that it was able to block CpG-induced interferon induction involving the IRF3/7 pathway. Subsequent investigation revealed that PIAS1 is able to SUMOylate IRF7. VP35 expression enhanced SUMOylation of IRF7, leading to suppression of its activity and a decrease in interferon promoter activity. Similar findings were noted with IRF3 following expression of VP35 (Chang et al., 2009). Thus, VP35-induced SUMOylation of IRF-3 and IRF-7 leads to a further reduction in interferon α/β gene transcription.
Arenaviruses (e.g., Lassa, LCMV) have taken a similar multipronged approach to preventing type I interferon responses. Lassa hemorrhagic fever has many similar characteristics to Ebola virus disease, including the absence of interferon production and lymphoid depletion. On the molecular level, arenaviruses have been shown to suppress interferon production by targeting both upstream (i.e., RIG-I/MDA-5) and downstream signaling events (i.e., IKKε interactions, IRF-3 phosphorylation) (Koma et al., 2013). In this way each virus disrupts multiple access points in the pathways that lead to increased interferon production. Given the similarity in the clinical syndromes and the common approach to interferon antagonism, further investigations may provide insights into the underlying pathogenic mechanisms of hemorrhagic fever syndromes.
VP24
When innate immunity is intact, the host response to virus infection causes secretion of interferon in order to generate antiviral responses in neighboring cells, signal hematopoietic cell responses and increase antigen presentation in APC’s. Secreted interferon binds to Type I and II interferon receptors, inducing signaling via adapter proteins and results in the phosphorylation and subsequent dimerization of signal transducer and activator of transcription (STAT) proteins (e.g., STAT-1, STAT-2). Next, dimerized phosphorylated STATs are transported to the nucleus where they bind to interferon response elements and induce gene expression (Ivashkiv and Donlin, 2014; Platanias, 2005). Given the importance of these pathways for inducing anti-viral gene expression in response to interferon, they are commonly targeted by viruses. For example, Dengue virus blocks STAT-1 phosphorylation and acts to degrade STAT-2 via proteasomal degradation pathways (Green et al., 2014). Early experiments with Ebola found that the virus not only blocked the production of interferon, but also inhibited cellular responses that normally result from both interferon α/β (Type I) and interferon γ(Type II) signaling. This signaling block was associated with the expression of the Ebola VP24 protein, which was later shown to prevent the nuclear accumulation of dimerized phosphorylated STAT-1 (Reid et al., 2006), which participates in both Type I (i.e., STAT-1/STAT-2 phosphorylated-dimer) and Type II (STAT-1/STAT-1 phosphorylated- dimer) signal propigation cascades (Ivashkiv and Donlin, 2014; Platanias, 2005).
Phosphorylated STAT-1 dimer transport to the nucleus is mediated via interactions with members of the nucleoprotein interactor 1 family (i.e., karyopherin-α1, -α5 or -α6). Karyopherin-α binds to nuclear localization signals (NLS) on cargo destined for the nucleus. Downstream interactions with karyopherin-β and other proteins allow the cargo to cross the nuclear membrane. Unlike most nuclear proteins, dimerized phosphorylated STAT-1 interacts with karyopherin-α through a unique non-canonical NLS, allowing it preferential access to the nucleus. Biochemical and structural studies have shown that VP24 binds to karyopherin-α in the non-canonical NLS binding domain. This results in a block in phosphorylated STAT-1 dimer transport to the nucleus. Furthermore, VP24 binding to karyopherin-α does not appear to block access to the canonical NLS binding site (Mateo et al., 2010; Reid et al., 2007; Xu et al., 2014). Therefore, the virus is able to block both Type I and Type II interferon signaling without disrupting routine trafficking to the nucleus of the infected cell.
Unphosphorylated STAT-1 is able to enter the nucleus via a karyopherin-α independent mechanism, where it is able to induce and prolong the expression of interferon-induced immune regulatory genes (Cheon and Stark, 2009; Meyer and Vinkemeier, 2004). Biochemical and structural studies using a STAT-1 C-terminal truncation mutant demonstrated that VP24 binds efficiently to STAT-1 lacking the tyrosine target for phosphorylation (Zhang et al., 2012). This suggests an additional mechanism unrelated to phosphorylated STAT-1 dimer nuclear transport by which VP24 is able to inhibit the induction of the interferon response (i.e., by blocking the action of both forms of STAT-1).
In addition to the Jak-STAT pathway, Type I interferon receptors signal via the p38 MAP kinase pathway. In this pathway a signal cascade of MAP kinases results in the phosphorylation of p38-α (Ivashkiv and Donlin, 2014; Platanias, 2005). One study found that in HEK-293T cells, VP24 was able to block the interferon-β induced phosphorylation of p38-α. However, this finding was cell type-specific and the blocking mechanism has yet to be demonstrated or generalized to cells that are primary targets of infection (e.g., macrophages, dendritic cells) (Halfmann et al., 2011).
Like VP35, VP24 has been linked to Ebola pathogenesis. In particular, experiments using mouse- and guinea pig-adapted variants of Ebola demonstrated that VP24 in conjunction with other proteins such as NP are critical to virus lethality (Cilloniz et al., 2011; Ebihara et al., 2006; Mateo et al., 2011; Reid et al., 2007). Structural analysis and comparison of Sudan and Reston VP24 identified two conserved structural pockets that contain residues implicated in the pathogenesis of VP24. Solvent exchange studies showed that this region may be near a proposed STAT-1 binding region on VP24, suggesting that it may play a role in STAT-1 binding and pathogenesis (Zhang et al., 2012). Taken together with previous studies on karyopherin-α, VP24 plays a role in pathogenesis through the disruption of both Type I and Type II interferon signaling. Thus, Ebola not only diminishes the interferon alarm but inhibits the alarm response after it has been heard. This coordinated approach between VP35 and VP24 leads to a highly effective antagonism of the innate immune responses mediated by interferons.
Silence Will Fall: Disrupting the RNAi response
Infection of cells by RNA viruses activates an RNA-specific inhibition (RNAi) pathway in host cells that silences viral gene expression by cleaving viral RNA into small interfering RNAs (siRNA) that bind and disrupt complementary RNA transcripts. Therefore, this host antiviral response is often a target for viral proteins. For example, HIV-1 Tat is thought to suppress RNAi responses by blocking Dicer activity, a key component of the RNA silencing complex. Ebola VP35 suppresses cellular RNAi silencing and can complement HIV-1 Tat− mutants. This suppression was lost when mutations were made in the dsRNA binding domains of VP35, suggesting that VP35 may bind to siRNA or the dsRNA precursors of siRNA (Haasnoot et al., 2007). While subsequent studies found that the C-terminal domain of VP35 bound to siRNA and not to dsRNA, the RNAi silencing suppression activity of VP35 did not correlate with binding to siRNA. It was hypothesized that suppression via RNA binding-independent mechanisms could instead occur through binding to the RISC complex or sequestration of RISC complex proteins prior to their incorporation into the complex (Zhu et al., 2012). This theory is supported by prior experiments that found VP35 interacts with transactivation response RNA-binding protein (TRBP) and PACT (Fabozzi et al., 2011), both components of the RISC RNAi complex and thus proposed to mediate the VP35-dependent RNA silencing suppressor activity. Interestingly, another Ebola protein, VP30, also binds to components of the RISC complex and acts as a suppressor of RNAi silencing (Fabozzi et al., 2011). Similar to Ebola’s tactics for interferon antagonism, the virus uses two different viral proteins to disrupt the mammalian RNAi innate immune response.
Plundering the Factories: Coopting host cellular functions
Protein Translation
Host cells thwart viral infection by decreasing cellular protein synthesis in an effort to prevent or slow viral replication. This is accomplished through the double stranded RNA-dependent Protein Kinase, PKR. Upon binding of dsRNA and activation, PKR phosphorylates the alpha subunit of the eukaryotic translation initiation factor-2 (eIF-2α). Ebola VP35 expression has been shown to block PKR activity and enhance expression of proteins after cells were treated with Type I interferons. VP35 blocks PKR by impairing phosphorylation of both PKR and the eIF-2α Current data suggests this effect is mediated by the VP35 IID domain; however, further work to elucidate the molecular mechanism is required (Feng et al., 2007; Schümann et al., 2009).
RNA stability and replication
The heterogeneous nuclear protein complex C1/C2 proteins (hnRNP C1/C2) are typically found in the nucleus where they bind poly-U regions (>4) in mRNA and assist splicing prior to mRNA export to the cytoplasm. They have also been shown to be able to participate in cap-independent, IRES-dependent translation in the cytoplasm during mitosis (Shabman et al., 2011). Several viruses, including Dengue and poliovirus, have been found to co-opt this function to enhance viral protein synthesis and replication (Brunner et al., 2005, 2010; Noisakran et al., 2008; Pettit Kneller et al., 2009). Ebola VP24 expression causes the relocalization of hnRNP C1/C2 from the nucleus to the cytoplasm. Interestingly, hnRNP C1/C2 also binds to karyopherin-α via the same non-canonical NLS sequence STAT-1 and VP24 use, suggesting a possible mechanism for redistribution. It was hypothesized that since the Ebola genomic and mRNA sequences contain many poly-U tracts, hnRNP C1/C2 may interact with Ebola RNA to stabilize viral mRNA and enhance genome replication (Shabman et al., 2011). Thus, through PKR inhibition and hnRNP C1/C2 relocalization, ebolaviruses coopt cellular machinery to optimize translation of gene products and potentially prolong the half-life of viral messenger and genomic RNA.
Escape from Alcatraz: The tetherin release program
Tetherin is a Type I interferon inducible cellular factor that has been shown to prevent enveloped virus budding from plasma membranes. Tetherin contains two membrane-anchored domains and is thought to mediate inhibition of budding by having one anchor linked to the cellular and viral membranes (Neil et al., 2008). Tetherin was first described to antagonize retrovirus and HIV-1 particle budding. These studies found that particle budding was rescued by the expression of HIV-1 Vpu (Neil et al., 2008). When Ebola virus-like particles (VLP) were made with VP40 in the presence of overexpressed tetherin, a similar decrease in VLP release was noted and simultaneous expression of HIV-1 Vpu rescued particle release. VLPs were then expressed with or without GP, and GP was found to antagonize tetherin activity and co-immunoprecipitate tetherin (Kaletsky et al., 2009). Recent experiments suggest that residues within the transmembrane domain of GP contribute to GP-dependent tetherin antagonism (Gnirß et al., 2014; Kühl et al., 2011). Mechanisms proposed for GP-tetherin antagonism include interference with tetherin integrity, steric hindrance by GP that interferes with the formation of the tetherin connection between the viral and cellular membranes, and GP-dependent exclusion of tetherin from the region of the plasma membrane from which Ebola virus particles bud (Kaletsky et al., 2009). In HIV-1, Vpu mediates cell surface downregulation, relocalization and degradation of tetherin (Lopez et al., 2012). However, Ebola GP does not appear to downregulate or alter tetherin localization (Lopez et al., 2010, 2012), suggesting a novel anti-tetherin mechanism.
The Host Strikes Back: Blocking the entrances and exits
The trade-off between efficient viral replication and pathogenicity is a delicate balance that when mismatched can lead to host demise. Therefore, viruses have evolved to suppress immune responses in a selective and regulated manner that facilitates controlled virus replication and progeny transmission. In this section we highlight two interferon inducible genes that to date are not known to be directly countered during Ebola infection.
Interferon-induced transmembrane proteins (IFITMs) are broadly active interferon responsive restriction factors that were first described as inhibitors of influenza A and have been shown to be active against many enveloped viruses including Ebola and its cousin Marburg virus (Huang et al., 2011). IFITIMs are transmembrane proteins that are found in multiple membrane surfaces along cellular uptake pathways and have been proposed to act by blocking virus entry (Huang et al., 2011; Perreira et al., 2003). Several anti-viral mechanisms have been proposed including cholesterol accumulation, inhibition of back fusion of virus containing vesicles in multivesicular bodies, changes to membrane fluid dynamics, or alterations in membrane curvature (i.e., restricting the capacity for fusion between the virus and cellular membranes)(Amini-Bavil-Olyaee et al., 2013; Perreira et al., 2013). Recent experiments with IFITM-3 and influenza A virus suggest that IFITM-3 acts by blocking an as yet undefined step between virus-cell membrane hemi-fusion and fusion pore formation (Desai et al., 2014). Thus, IFITM-3 allows the virus and celluar membrane lipids to mix but does not allow the formation of a complete fusion pore. This prevents the ribonucleoprotein core of the virus from gaining access to the cytoplasm and blocks infection. Future experiments will need to be performed to determine if this mechanism is applicable to Ebola and how some enveloped viruses (i.e., arenaviruses) are able to avoid restriction by IFITMs.
Another interferon-stimulated gene that blocks Ebola infection is ISG-15, a broadly active antiviral gene product that, when conjugated to a target protein, causes alterations to target protein activity, cellular location and stability. It has been shown to affect many viruses including influenza A/B, hepatitis B, HIV-1, herpes simplex type-1, LCMV and Ebola (Harty et al., 2009). In the case of Ebola, the anti-viral activity of ISG-15 was linked to a disruption in VP40-mediated budding using virus-like particle (VLP) assays. Ebola budding is in part mediated by Nedd4 ubiquitination of VP40. Two groups found that ISG-15 interacts with Nedd4 and prevents the ubiquitination of VP40, leading to inefficient particle budding (Liu and Harty, 2010). Thus, together with IFITMs and tetherin, these observations suggest that interferon stimulated genes have potent antiviral activities targeted against ebolavirus during both entry and egress.
The resistance of freshly isolated monocytes to Ebola infection illustrates one example where these factors may be playing a role during entry. Experiments with Ebola GP-pseudotyped VLPs found that particles were able to bind but not enter freshly isolated monocytes. However, once the monocytes underwent differentiation, the previously bound virus was able to infect the monocytes, a result recapitulated using replicating Ebola viruses (Martinez et al., 2013). Detailed analysis found that, as the monocytes matured, IFITMs were downregulated while both cysteine protease cathepsin B and NPC1 expression were upregulated. These findings demonstrate how IFITM restriction factors might play a role in the relative resistance to infection of interferon-activated cells, and also confirm the importance of NPC1 for Ebola infection.
Balancing the scales of the immune response
A paradox in Ebola virus disease is that both survival and mortality are linked to the generation of strong immune signaling responses in the host. Survivors and asymptomatic patients have increased numbers of T cells and an early cytotoxic T-cell mediated response (Baize et al., 1999; Sanchez et al., 2004; Wauquier et al., 2010). Rapid uptake of Ebola by macrophages and dendritic cells results not only in translocation to lymphoid and peripheral tissues, but may explain the deficit in non-survivors of inflammatory cytokine secretion needed early after exposure for the control of infection. Experiments using in vitro cultured monocyte-derived macrophages found that Ebola infection inhibited the secretion of TNF-α, IL-6, and IL-10, consistent with impairments observed in association with fatal disease outcome (Mahanty et al., 2003). Furthermore, dendritic cells exposed to either live or inactivated virus failed to upregulate molecules needed for T-cell co-stimulation, resulting in an inhibition of CD4 T-cell proliferation. Studies using blood samples obtained from infected human subjects found that IL-6 and TNF-α responses were higher in survivors than non-survivors at early time points. At later time points, IL-6 remained higher in survivors, but the difference from non-survivors was less dramatic due to increases in the latter group. In contrast to IL-6, TNF-α in non-survivors was much higher than survivors late after disease onset. It is interesting to note that IL-10 may play a critical role in modulating these responses. While IL-10 was mildly elevated in survivors, likely as a feedback mechanism to control the inflammatory response, the increase was short lived, as would be expected once cytokine levels return to normal. However, IL-10 was 6–10 fold higher in fatal cases and remained elevated until death. In addition, monocyte/macrophage activation as measured by neopterin levels was 2–10 fold higher and consistently elevated in fatal cases (Baize et al., 2002; Leroy et al., 2000, 2001), suggesting unregulated immune activation. While more recent studies showed different patterns for specific cytokines (Wauquier et al., 2010), there is a general trend toward survivors having a short-lived, balanced pro- and anti-inflammatory response and non-survivors having a prolonged inflammatory response that leads to “cytokine storm”.
Together these observations suggest that subjects able to overcome innate immune response blocking by VP24, VP30 and VP35 are more likely to establish an early, balanced and beneficial secretion of pro-inflammatory/anti-inflammatory cytokines. In contrast, when early host anti-viral innate responses are blocked, uncontrolled virus replication and lysis of hematopoietic cells leads to late, unbalanced cytokine release, overall dysregulation of immune responses and the development of advanced Ebola virus disease.
Camouflage & Misdirection: Avoiding adaptive immune responses
A fatal irreversible consequence of hematopoietic cell destruction by Ebola is reduced antigen presentation. This outcome is consistent with the observation of poor IgG responses observed in fatal infection, while high levels of IgG are associated with survival (Baize et al., 1999; Ksiazek et al., 1999). Compounding inhibition of IgG production, Ebola has evolved multiple properties that could circumvent antibody effectiveness. Large filamentous virions containing high density, stable glycoprotein present a potential obstacle for efficient inhibition by antibodies, and virus filament folding may create “pockets” of glycoprotein inaccessible to antibody binding. Furthermore, heavy glycosylation in the mucin-like domain of GP may limit access to critical epitopes required for efficient neutralization (Martinez et al., 2011b). Antibody access is restricted further due to rapid virion uptake via macropinocytosis and intracellular receptor binding. Additionally, ebolavirus hidesits critical receptor binding domain beneath a glycan cap, with exposure and receptor binding occurring only after cathepsin mediated removal of the cap. This protection of a critical functional domain is analogous to HIV where CD4 engagement of gp120 exposes the co-receptor binding site (Harrison, 2008). Furthermore, the use of an intracellular receptor is a novel immune evasion strategy that may be important for other viruses (e.g., Lassa fever virus (Jae et al., 2014)).
Besides membrane anchored GP, the glycoproteingene of Ebola encodes sGP, a 364 a.a. protein which is identical to GP in its 205 N-terminal residues but is secreted by infected cells and is not present in virions. The default transcript of the glycoprotein gene is surprisingly not the virion-associated GP trimer, but instead dimerics GP, a process that is governed by polymerase stuttering at an RNA editing site. This has led to speculation that sGP functions to modulate or misdirect host immune responses (Kindzelskii et al., 2000; Yang et al., 1998). The best evidence for this hypothesis comes from a recent paper showing in mice that sGP promotes immune evasion by serving as an antibody decoy for GP or by presenting alternative non-neutralizing antibody epitopes for the humoral immune response (Mohan et al., 2012). Remarkably, evidence suggests that about 80% of glycoprotein gene expression is sGP. This may be due, in part, to selective pressures seeking to balance toxicity due to cytopathic effects of GP with the requirement for GP on virus particles, and avoidance of host immune responses directed against GP (Yang et al., 2000, Volchkova et al., 2011). Taken together, these data suggest that Ebola expression of sGP and GP is a tightly regulated process in which immune shielding and virus particle production are balanced via RNA editing.
In addition to immune evasion achieved through virion and GP structural characteristics, GP exhibits direct immunosuppressive properties (Chepurnov et al., 1999). sGP interacts with neutrophils and disrupts the linkage between Fc gamma RIIIB and CR3 (Kindzelskii et al., 2000). Furthermore, the Ebola transmembrane glycoprotein, GP2, bears structurally similarity to retroviral glycoproteins possessing an immunosuppressive peptide motif (Volchkov et al., 1992) that was found to inhibit lymphocyte activation and proliferation (Yaddanapudi et al., 2006). Of particular interest was the observation that the analogous immunosuppressive peptide from Reston virus was inhibitory only in macaque, but not human, peripheral blood cells, implicating this motif in Ebola pathogenicity.
Studies measuring in vivo antigen-specific T-cell responses are limited by the difficulty in obtaining and preserving viable lymphocyte samples from Ebola-infected subjects and survivors. Nonetheless, data suggests that there is a dramatic decrease in the absolute numbers of T cells due to bystander apoptosis. This impairs both direct cell-mediated killing of virus-infected cells and the T-cell dependent antiviral antibody responses (Sanchez et al., 2004). Indirect measures of T-cell function based on serum cytokine levels and RNA expression in isolated lymphocytes suggest, as with immunoglobulin levels, an association between intact cell-mediated immunity and survival (Baize et al., 1999; Ksiazek et al., 1999; Sanchez et al., 2004; Wauquier et al., 2010). In macaques, CD8+ T cells are essential for vaccine-induced immune protection (Stanley et al., 2014; Sullivan et al., 2011). Antibodies clearly play a beneficial role in containing virus but are not required for protection against some Ebola species (Hensley et al., 2010; Stanley et al., 2014; Sullivan et al., 2011), but participate in effective virus clearance and likely require the presence of intact host cell-mediated responses (Wong et al., 2012). One speculative interpretation of both human and macaque data is that immunoglobulin and innate immune responses participate in containing early viral loads, but that cell-mediated immunity is needed for efficient virus clearance. The interplay and necessity of broad immune response mechanisms is also suggested by Ebola evolution of strategies to counteract each of these host antiviral defenses. Taken together these data suggest a complex interplay between pro- and anti-inflammatory factors resulting in either a balanced immune response and host survival or dysregulation and death.
Summary
Fatal Ebola infection is marked by a catastrophic failure of innate and adaptive immunity that is mediated by virus-encoded proteins as well as properties associated with virus structure. At the heart of Ebola-induced immune dysregulation is a multipronged attack on host antiviral immunity. Early and coordinated disruption of host innate responses by VP24, VP30 and VP35 leads to elevated levels of virus replication, a cascade of inappropriately timed cytokine release and death of both antigen-presenting and responding immune cells. This results in a poorly activated adaptive immune response that is further compromised by the induction of lymphocyte apoptosis and antibody decoy mechanisms. In incidental hosts, this multifaceted approach to subversion of the immune system results in high mortality that would be expected to limit virus persistence in the absence of a distinct reservoir species.
Since first being identified almost 40 years ago, the genome of Ebola has shown remarkable stability, an unusual feature for RNA viruses with an error-prone polymerase. This suggests Ebola is highly adapted in its reservoir host. One intriguing hypothesis is that additional host restriction factors limit pathogenicity in a natural reservoir species. These factors would play a role in the balance between immunity and sustained viral replication, allowing the virus to propagate and persist over time in the reservoir species. Outside this reservoir, sustained large outbreaks such as the one in West Africa may lead to ebolavirus adaptations being observed longitudinally, resulting in altered pathogenicity as the virus adapts to humans. Overall, the multifaceted approach of Ebola to selectively regulate immune responses and its variable pathogenicity in different host species makes this virus both scientifically interesting and a challenging foe.
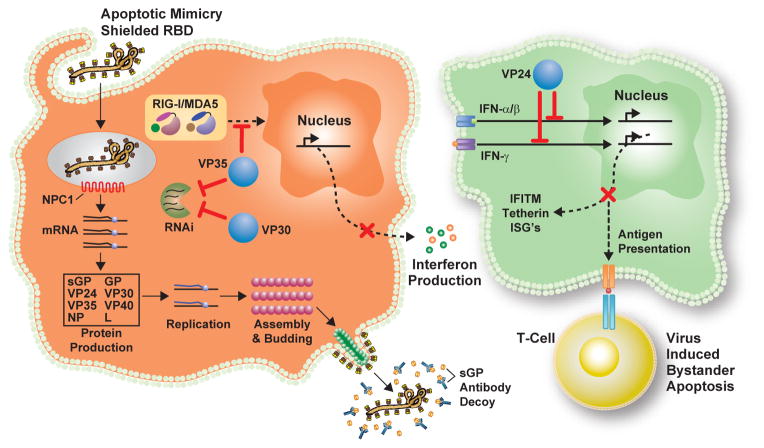
Figure 1.
Ebolavirus life cycle: (Left) Virus particles attach to cell surface, inducing macropinocytosis and virus uptake, possibly using apoptotic mimicry to suppress inflammatory responses. The particle is brought to a low pH compartment where it is cleaved by cysteine proteases to reveal its NPC1 receptor binding domain (RBD). Following fusion and uncoating, the viral genome is transcribed into mRNA and viral proteins produced. Eventually, a signal to begin genome replication occurs, followed by particle assembly and budding.
Immune avoidance mechanisms: Expression and secretion of sGP serves as an antibody decoy for antibodies generated against GP. Viral proteins VP35, VP30 and VP24 are expressed and mediate innate immune avoidance in all cell types. (Left) VP35 interferes with RIG-I/MDA-5 signaling and induction of interferon. Additionally, VP35 and VP30 block the RNAi response against viral gene expression. (Right) VP24 acts to inhibit Type I and II interferon (IFN) signaling. This prevents interferon-induced gene expression and in antigen presenting cells blocks enhancement of antigen presentation to T cells.
Acknowledgments
The authors thank B. Hartman for graphics and A. Tislerics for editing the manuscript.
References
- Aleksandrowicz P, Marzi A, Biedenkopf N, Beimforde N, Becker S, Hoenen T, Feldmann H, Schnittler H-J. Ebola virus enters host cells by macropinocytosis and clathrin-mediated endocytosis. J Infect Dis. 2011;204(Suppl):S957–67. doi: 10.1093/infdis/jir326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez CP, Lasala F, Carrillo J, Muñiz O, Corbí AL, Delgado R. C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in trans. J Virol. 2002;76:6841–6844. doi: 10.1128/JVI.76.13.6841-6844.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amini-Bavil-Olyaee S, Choi YJJ, Lee JHH, Shi M, Huang IC, Farzan M, Jung JUU. The antiviral effector IFITM3 disrupts intracellular cholesterol homeostasis to block viral entry. Cell Host Microbe. 2013;13:452–464. doi: 10.1016/j.chom.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baize S, Leroy EM, Georges-Courbot MC, Capron M, Lansoud-Soukate J, Debré P, Fisher-Hoch SP, McCormick JB, Georges aJ. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat Med. 1999;5:423–426. doi: 10.1038/7422. [DOI] [PubMed] [Google Scholar]
- Baize S, Leroy EM, Georges aJ, Georges-Courbot MC, Capron M, Bedjabaga I, Lansoud-Soukate J, Mavoungou E. Inflammatory responses in Ebola virus-infected patients. Clin Exp Immunol. 2002;128:163–168. doi: 10.1046/j.1365-2249.2002.01800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baribaud F, Pöhlmann S, Leslie G, Mortari F, Doms RW. Quantitative expression and virus transmission analysis of DC-SIGN on monocyte-derived dendritic cells. J Virol. 2002;76:9135–9142. doi: 10.1128/JVI.76.18.9135-9142.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basler CF, Wang X, Mühlberger E, Volchkov V, Paragas J, Klenk HD, García-Sastre a, Palese P. The Ebola virus VP35 protein functions as a type I IFN antagonist. Proc Natl Acad Sci U S A. 2000;97:12289–12294. doi: 10.1073/pnas.220398297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basler CF, Mikulasova A, Martinez-Sobrido L, Paragas J, Mühlberger E, Bray M, Klenk HD, Palese P, García-Sastre A. The Ebola virus VP35 protein inhibits activation of interferon regulatory factor 3. J Virol. 2003;77:7945–7956. doi: 10.1128/JVI.77.14.7945-7956.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharat TaM, Noda T, Riches JD, Kraehling V, Kolesnikova L, Becker S, Kawaoka Y, Briggs JaG. Structural dissection of Ebola virus and its assembly determinants using cryo-electron tomography. Proc Natl Acad Sci U S A. 2012;109:4275–4280. doi: 10.1073/pnas.1120453109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biedenkopf N, Hartlieb B, Hoenen T, Becker S. Phosphorylation of Ebola virus VP30 influences the composition of the viral nucleocapsid complex: impact on viral transcription and replication. J Biol Chem. 2013;288:11165–11174. doi: 10.1074/jbc.M113.461285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biermann M, Maueröder C, Brauner JM, Chaurio R, Janko C, Herrmann M, Muñoz LE. Surface code--biophysical signals for apoptotic cell clearance. Phys Biol. 2013;10:065007. doi: 10.1088/1478-3975/10/6/065007. [DOI] [PubMed] [Google Scholar]
- Brecher M, Schornberg KL, Delos SE, Fusco ML, Saphire EO, White JM. Cathepsin Cleavage Potentiates the Ebola Virus Glycoprotein to Undergo a Subsequent Fusion Relevant Conformational Change. J Virol. 2011;86:364–372. doi: 10.1128/JVI.05708-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brindley Ma, Hunt CL, Kondratowicz AS, Bowman J, Sinn PL, McCray PB, Quinn K, Weller ML, Chiorini Ja, Maury W. Tyrosine kinase receptor Axl enhances entry of Zaire ebolavirus without direct interactions with the viral glycoprotein. Virology. 2011;415:83–94. doi: 10.1016/j.virol.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunner JE, Nguyen JHC, Roehl HH, Ho TV, et al. Functional Interaction of Heterogeneous Nuclear Ribonucleoprotein C with Poliovirus RNA Synthesis Initiation Complexes Functional Interaction of Heterogeneous Nuclear Ribonucleoprotein C with Poliovirus RNA Synthesis Initiation Complexes. J Virol. 2005;79:3254–3266. doi: 10.1128/JVI.79.6.3254-3266.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunner JE, Ertel KJ, Rozovics JM, Semler BL. Delayed kinetics of poliovirus RNA synthesis in a human cell line with reduced levels of hnRNP C proteins. Virology. 2010;400:240–247. doi: 10.1016/j.virol.2010.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cárdenas WB, Loo YM, Gale M, Hartman AL, Kimberlin CR, Martínez-Sobrido L, Saphire EO, Basler CF. Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. J Virol. 2006;80:5168–5178. doi: 10.1128/JVI.02199-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. 2011;477:340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005;308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang TH, Kubota T, Matsuoka M, Jones S, Bradfute SB, Bray M, Ozato K. Ebola Zaire virus blocks type I interferon production by exploiting the host SUMO modification machinery. PLoS Pathog. 2009;5:e1000493. doi: 10.1371/journal.ppat.1000493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheon H, Stark GR. Unphosphorylated STAT1 prolongs the expression of interferon-induced immune regulatory genes. Proc Natl Acad Sci U S A. 2009;106:9373–9378. doi: 10.1073/pnas.0903487106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chepurnov aa, Tuzova MN, Ternovoy Va, Chernukhin IV. Suppressive effect of Ebola virus on T cell proliferation in vitro is provided by a 125-kDa GP viral protein. Immunol Lett. 1999;68:257–261. doi: 10.1016/s0165-2478(99)00058-9. [DOI] [PubMed] [Google Scholar]
- Chiang JJ, Davis ME, Gack MU. Regulation of RIG-I-like receptor signaling by host and viral proteins. Cytokine Growth Factor Rev. 2014 doi: 10.1016/j.cytogfr.2014.06.005. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cilloniz C, Ebihara H, Ni C, Neumann G, Korth MJ, Kelly SM, Kawaoka Y, Feldmann H, Katze MG. Functional genomics reveals the induction of inflammatory response and metalloproteinase gene expression during lethal Ebola virus infection. J Virol. 2011;85:9060–9068. doi: 10.1128/JVI.00659-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Côté M, Misasi J, Ren T, Bruchez A, Lee K, Filone CM, Hensley L, Li Q, Ory D, Chandran K, et al. Small molecule inhibitors reveal Niemann-Pick C1 is essential for ebolavirus infection. Nature. 2011;477:344–348. doi: 10.1038/nature10380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai TM, Marin M, Chin CR, Savidis G, Brass AL, Melikyan GB. IFITM3 restricts influenza A virus entry by blocking the formation of fusion pores following virus-endosome hemifusion. PLoS Pathog. 2014;10:e1004048. doi: 10.1371/journal.ppat.1004048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube D, Brecher MB, Delos SE, Rose SC, Park EW, Schornberg KL, Kuhn JH, White JM. The primed ebolavirus glycoprotein (19-kilodalton GP1,2): sequence and residues critical for host cell binding. J Virol. 2009;83:2883–2891. doi: 10.1128/JVI.01956-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebihara H, Takada A, Kobasa D, Jones S, Neumann G, Theriault S, Bray M, Feldmann H, Kawaoka Y. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2006;2:e73. doi: 10.1371/journal.ppat.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabozzi G, Nabel CS, Dolan Ma, Sullivan NJ. Ebolavirus proteins suppress the effects of small interfering RNA by direct interaction with the mammalian RNA interference pathway. J Virol. 2011;85:2512–2523. doi: 10.1128/JVI.01160-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z, Cerveny M, Yan Z, He B. The VP35 protein of Ebola virus inhibits the antiviral effect mediated by double-stranded RNA-dependent protein kinase PKR. J Virol. 2007;81:182–192. doi: 10.1128/JVI.01006-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnirß K, Fiedler M, Krämer-Kühl A, Bolduan S, Mittler E, Becker S, Schindler M, Pöhlmann S. Analysis of determinants in filovirus glycoproteins required for tetherin antagonism. Viruses. 2014;6:1654–1671. doi: 10.3390/v6041654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green AM, Beatty PR, Hadjilaou A, Harris E. Innate immunity to dengue virus infection and subversion of antiviral responses. Journal of Molecular Biology. 2014;426(6):1148–60. doi: 10.1016/j.jmb.2013.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haasnoot J, de Vries W, Geutjes EJ, Prins M, de Haan P, Berkhout B. The Ebola virus VP35 protein is a suppressor of RNA silencing. PLoS Pathog. 2007;3:e86. doi: 10.1371/journal.ppat.0030086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfmann P, Neumann G, Kawaoka Y. The Ebolavirus VP24 protein blocks phosphorylation of p38 mitogen-activated protein kinase. J Infect Dis. 2011;204(Suppl):S953–6. doi: 10.1093/infdis/jir325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison SC. Viral membrane fusion. Nat Struct Mol Biol. 2008;15:690–698. doi: 10.1038/nsmb.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartlieb B, Modrof J, Mühlberger E, Klenk HD, Becker S. Oligomerization of Ebola virus VP30 is essential for viral transcription and can be inhibited by a synthetic peptide. J Biol Chem. 2003;278:41830–41836. doi: 10.1074/jbc.M307036200. [DOI] [PubMed] [Google Scholar]
- Hartlieb B, Muziol T, Weissenhorn W, Becker S. Crystal structure of the C-terminal domain of Ebola virus VP30 reveals a role in transcription and nucleocapsid association. Proc Natl Acad Sci U S A. 2007;104:624–629. doi: 10.1073/pnas.0606730104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman AL, Ling L, Nichol ST, Hibberd ML. Whole-genome expression profiling reveals that inhibition of host innate immune response pathways by Ebola virus can be reversed by a single amino acid change in the VP35 protein. J Virol. 2008a;82:5348–5358. doi: 10.1128/JVI.00215-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman AL, Bird BH, Towner JS, Antoniadou ZA, Zaki SR, Nichol ST. Inhibition of IRF-3 activation by VP35 is critical for the high level of virulence of ebola virus. J Virol. 2008b;82:2699–2704. doi: 10.1128/JVI.02344-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman AL, Towner JS, Nichol ST. Ebola and marburg hemorrhagic fever. Clin Lab Med. 2010;30:161–177. doi: 10.1016/j.cll.2009.12.001. [DOI] [PubMed] [Google Scholar]
- Harty RN, Pitha PM, Okumura A. Antiviral activity of innate immune protein ISG15. J Innate Immun. 2009;1:397–404. doi: 10.1159/000226245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensley LE, Mulangu S, Asiedu C, Johnson J, Honko AN, Stanley D, Fabozzi G, Nichol ST, Ksiazek TG, Rollin PE, et al. Demonstration of cross-protective vaccine immunity against an emerging pathogenic Ebolavirus Species. PLoS Pathog. 2010;6:e1000904. doi: 10.1371/journal.ppat.1000904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood CL, Abraham J, Boyington JC, Leung K, Kwong PD, Nabel GJ. Biochemical and structural characterization of cathepsin L-processed Ebola virus glycoprotein: implications for viral entry and immunogenicity. J Virol. 2010;84:2972–2982. doi: 10.1128/JVI.02151-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang IC, Bailey CC, Weyer JL, Radoshitzky SR, Becker MM, Chiang JJ, Brass AL, Ahmed Aa, Chi X, Dong L, et al. Distinct patterns of IFITM-mediated restriction of filoviruses, SARS coronavirus, and influenza A virus. PLoS Pathog. 2011;7:e1001258. doi: 10.1371/journal.ppat.1001258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt CL, Kolokoltsov Aa, Davey Ra, Maury W. The Tyro3 receptor kinase Axl enhances macropinocytosis of Zaire ebolavirus. J Virol. 2011;85:334–347. doi: 10.1128/JVI.01278-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivashkiv LB, Donlin LT. Regulation of type I interferon responses. Nat Rev Immunol. 2014;14:36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jae LT, Raaben M, Herbert AS, Kuehne AI, Wirchnianski AS, Soh TK, Stubbs SH, Janssen H, Damme M, Saftig P, et al. Virus entry. Lassa virus entry requires a trigger-induced receptor switch. Science. 2014;344:1506–1510. doi: 10.1126/science.1252480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemielity S, Wang JJ, Chan YK, Ahmed Aa, Li W, Monahan S, Bu X, Farzan M, Freeman GJ, Umetsu DT, et al. TIM-family proteins promote infection of multiple enveloped viruses through virion-associated phosphatidylserine. PLoS Pathog. 2013;9:e1003232. doi: 10.1371/journal.ppat.1003232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaletsky RL, Francica JR, Agrawal-Gamse C, Bates P. Tetherin-mediated restriction of filovirus budding is antagonized by the Ebola glycoprotein. Proc Natl Acad Sci U S A. 2009;106:2886–2891. doi: 10.1073/pnas.0811014106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimberlin CR, Bornholdt Za, Li S, Woods VL, MacRae IJ, Saphire EO. Ebolavirus VP35 uses a bimodal strategy to bind dsRNA for innate immune suppression. Proc Natl Acad Sci U S A. 2010;107:314–319. doi: 10.1073/pnas.0910547107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindzelskii aL, Yang Z, Nabel GJ, Todd RF, Petty HR. Ebola virus secretory glycoprotein (sGP) diminishes Fc gamma RIIIB-to-CR3 proximity on neutrophils. J Immunol. 2000;164:953–958. doi: 10.4049/jimmunol.164.2.953. [DOI] [PubMed] [Google Scholar]
- Koma T, Huang C, Kolokoltsova Oa, Brasier AR, Paessler S. Innate immune response to arenaviral infection: a focus on the highly pathogenic New World hemorrhagic arenaviruses. Journal of Molecular Biology. 2013;425(24):4893–903. doi: 10.1016/j.jmb.2013.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondratowicz AS, Lennemann NJ, Sinn PL, Davey Ra, Hunt CL, Moller-Tank S, Meyerholz DK, Rennert P, Mullins RF, Brindley M, et al. T-cell immunoglobulin and mucin domain 1 (TIM-1) is a receptor for Zaire Ebolavirus and Lake Victoria Marburgvirus. Proc Natl Acad Sci U S A. 2011;108:8426–8431. doi: 10.1073/pnas.1019030108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ksiazek TG, Rollin PE, Williams aJ, Bressler DS, Martin ML, Swanepoel R, Burt FJ, Leman Pa, Khan aS, Rowe aK, et al. Clinical virology of Ebola hemorrhagic fever (EHF): virus, virus antigen, and IgG and IgM antibody findings among EHF patients in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis. 1999;179(Suppl):S177–87. doi: 10.1086/514321. [DOI] [PubMed] [Google Scholar]
- Kühl A, Banning C, Marzi A, Votteler J, Steffen I, Bertram S, Glowacka I, Konrad A, Stürzl M, Guo J-T, et al. The Ebola virus glycoprotein and HIV-1 Vpu employ different strategies to counteract the antiviral factor tetherin. J Infect Dis. 2011;204(Suppl):S850–60. doi: 10.1093/infdis/jir378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leroy EM, Baize S, Volchkov VE, Fisher-Hoch SP, Georges-Courbot MC, Lansoud-Soukate J, Capron M, Debré P, McCormick JB, Georges AJ. Human asymptomatic Ebola infection and strong inflammatory response. Lancet. 2000;355:2210–2215. doi: 10.1016/s0140-6736(00)02405-3. [DOI] [PubMed] [Google Scholar]
- Leroy EM, Baize S, Debre P, Lansoud-Soukate J, Mavoungou E. Early immune responses accompanying human asymptomatic Ebola infections. Clin Exp Immunol. 2001;124:453–460. doi: 10.1046/j.1365-2249.2001.01517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, Ginder ND, Fulton DB, Nix J, Basler CF, Honzatko RB, Amarasinghe GK. Structure of the Ebola VP35 interferon inhibitory domain. Proc Natl Acad Sci U S A. 2009;106:411–416. doi: 10.1073/pnas.0807854106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, Prins KC, Borek DM, Farahbakhsh M, Tufariello JM, Ramanan P, Nix JC, Helgeson La, Otwinowski Z, Honzatko RB, et al. Structural basis for dsRNA recognition and interferon antagonism by Ebola VP35. Nat Struct Mol Biol. 2010a;17:165–172. doi: 10.1038/nsmb.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, Shabman RS, Farahbakhsh M, Prins KC, Borek DM, Wang T, Mühlberger E, Basler CF, Amarasinghe GK. Structural and functional characterization of Reston Ebola virus VP35 interferon inhibitory domain. J Mol Biol. 2010b;399:347–357. doi: 10.1016/j.jmb.2010.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin G, Simmons G, Pöhlmann S, Baribaud F, Ni H, Leslie GJ, Haggarty BS, Bates P, Weissman D, Hoxie JA, et al. Differential N-linked glycosylation of human immunodeficiency virus and Ebola virus envelope glycoproteins modulates interactions with DC-SIGN and DC-SIGNR. J Virol. 2003;77:1337–1346. doi: 10.1128/JVI.77.2.1337-1346.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Harty RN. Viral and host proteins that modulate filovirus budding. Future Virol. 2010;5:481–491. doi: 10.2217/FVL.10.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez La, Yang SJ, Hauser H, Exline CM, Haworth KG, Oldenburg J, Cannon PM. Ebola virus glycoprotein counteracts BST-2/Tetherin restriction in a sequence-independent manner that does not require tetherin surface removal. J Virol. 2010;84:7243–7255. doi: 10.1128/JVI.02636-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez La, Yang SJ, Exline CM, Rengarajan S, Haworth KG, Cannon PM. Anti-tetherin activities of HIV-1 Vpu and Ebola virus glycoprotein do not involve removal of tetherin from lipid rafts. J Virol. 2012;86:5467–5480. doi: 10.1128/JVI.06280-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthra P, Ramanan P, Mire CE, Weisend C, Tsuda Y, Yen B, Liu G, Leung DW, Geisbert TW, Ebihara H, et al. Mutual antagonism between the Ebola virus VP35 protein and the RIG-I activator PACT determines infection outcome. Cell Host Microbe. 2013;14:74–84. doi: 10.1016/j.chom.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahanty S, Hutchinson K, Agarwal S, McRae M, Rollin PE, Pulendran B. Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. J Immunol. 2003;170:2797–2801. doi: 10.4049/jimmunol.170.6.2797. [DOI] [PubMed] [Google Scholar]
- Martinez MJ, Volchkova Va, Raoul H, Alazard-Dany N, Reynard O, Volchkov VE. Role of VP30 phosphorylation in the Ebola virus replication cycle. J Infect Dis. 2011a;204(Suppl):S934–40. doi: 10.1093/infdis/jir320. [DOI] [PubMed] [Google Scholar]
- Martinez O, Tantral L, Mulherkar N, Chandran K, Basler CF. Impact of Ebola mucin-like domain on antiglycoprotein antibody responses induced by Ebola virus-like particles. J Infect Dis. 2011b;204(Suppl):S825–32. doi: 10.1093/infdis/jir295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Johnson JC, Honko A, Yen B, Shabman RS, Hensley LE, Olinger GG, Basler CF. Ebola virus exploits a monocyte differentiation program to promote its entry. J Virol. 2013 doi: 10.1128/JVI.02695-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateo M, Reid SP, Leung LW, Basler CF, Volchkov VE. Ebolavirus VP24 binding to karyopherins is required for inhibition of interferon signaling. J Virol. 2010;84:1169–1175. doi: 10.1128/JVI.01372-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateo M, Carbonnelle C, Reynard O, Kolesnikova L, Nemirov K, Page A, Volchkova Va, Volchkov VE. VP24 is a molecular determinant of Ebola virus virulence in guinea pigs. J Infect Dis. 2011;204(Suppl):S1011–20. doi: 10.1093/infdis/jir338. [DOI] [PubMed] [Google Scholar]
- Mercer J, Helenius A. Vaccinia virus uses macropinocytosis and apoptotic mimicry to enter host cells. Science. 2008;320:531–535. doi: 10.1126/science.1155164. [DOI] [PubMed] [Google Scholar]
- Meyer T, Vinkemeier U. Nucleocytoplasmic shuttling of STAT transcription factors. Eur J Biochem. 2004;271:4606–4612. doi: 10.1111/j.1432-1033.2004.04423.x. [DOI] [PubMed] [Google Scholar]
- Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI, et al. Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J. 2012;31:1947–1960. doi: 10.1038/emboj.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misasi J, Chandran K, Yang JY, Considine B, Filone CM, Côté M, Sullivan N, Fabozzi G, Hensley L, Cunningham J. Filoviruses require endosomal cysteine proteases for entry but exhibit distinct protease preferences. J Virol. 2012;86:3284–3292. doi: 10.1128/JVI.06346-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modrof J, Becker S, Mühlberger E. Ebola virus transcription activator VP30 is a zinc-binding protein. J Virol. 2003;77:3334–3338. doi: 10.1128/JVI.77.5.3334-3338.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohan GS, Li W, Ye L, Compans RW, Yang C. Antigenic subversion: a novel mechanism of host immune evasion by Ebola virus. PLoS Pathog. 2012;8:e1003065. doi: 10.1371/journal.ppat.1003065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moller-Tank S, Kondratowicz AS, Davey Ra, Rennert PD, Maury W. Role of the phosphatidylserine receptor TIM-1 in enveloped-virus entry. J Virol. 2013;87:8327–8341. doi: 10.1128/JVI.01025-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morizono K, Chen ISY. Role of phosphatidylserine receptors in enveloped virus infection. J Virol. 2014;88:4275–4290. doi: 10.1128/JVI.03287-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mühlberger E, Weik M, Volchkov VE, Klenk HD, Becker S. Comparison of the transcription and replication strategies of marburg virus and Ebola virus by using artificial replication systems. J Virol. 1999;73:2333–2342. doi: 10.1128/jvi.73.3.2333-2342.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulherkar N, Raaben M, de la Torre JC, Whelan SP, Chandran K. The Ebola virus glycoprotein mediates entry via a non-classical dynamin-dependent macropinocytic pathway. Virology. 2011;419:72–83. doi: 10.1016/j.virol.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathog. 2010:6. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neil SJD, Zang T, Bieniasz PD. Tetherin inhibits retrovirus release and is antagonized by HIV-1 Vpu. Nature. 2008;451:425–430. doi: 10.1038/nature06553. [DOI] [PubMed] [Google Scholar]
- Noisakran S, Sengsai S, Thongboonkerd V, Kanlaya R, Sinchaikul S, Chen ST, Puttikhunt C, Kasinrerk W, Limjindaporn T, Wongwiwat W, et al. Identification of human hnRNP C1/C2 as a dengue virus NS1-interacting protein. Biochem Biophys Res Commun. 2008;372:67–72. doi: 10.1016/j.bbrc.2008.04.165. [DOI] [PubMed] [Google Scholar]
- Perreira JM, Chin CR, Feeley EM, Brass AL. IFITMs restrict the replication of multiple pathogenic viruses. Journal of Molecular Biology. 2013;425(24):4937–55. doi: 10.1016/j.jmb.2013.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit Kneller EL, Connor JH, Lyles DS. hnRNPs Relocalize to the cytoplasm following infection with vesicular stomatitis virus. J Virol. 2009;83:770–780. doi: 10.1128/JVI.01279-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platanias LC. Mechanisms of type-I- and type-II-interferon-mediated signalling. Nat Rev Immunol. 2005;5:375–386. doi: 10.1038/nri1604. [DOI] [PubMed] [Google Scholar]
- Prins KC, Cárdenas WB, Basler CF. Ebola virus protein VP35 impairs the function of interferon regulatory factor-activating kinases IKK epsilon and TBK-1. J Virol. 2009;83:3069–3077. doi: 10.1128/JVI.01875-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins KC, Delpeut S, Leung DW, Reynard O, Volchkova Va, Reid SP, Ramanan P, Cárdenas WB, Amarasinghe GK, Volchkov VE, et al. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus a virulent in guinea pigs. J Virol. 2010;84:3004–3015. doi: 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn K, Brindley Ma, Weller ML, Kaludov N, Kondratowicz A, Hunt CL, Sinn PL, McCray PB, Stein CS, Davidson BL, et al. Rho GTPases modulate entry of Ebola virus and vesicular stomatitis virus pseudotyped vectors. J Virol. 2009;83:10176–10186. doi: 10.1128/JVI.00422-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid SP, Leung LW, Hartman AL, Martinez O, Shaw ML, Carbonnelle C, Volchkov VE, Nichol ST, Basler CF. Ebola virus VP24 binds karyopherin alpha1 and blocks STAT1 nuclear accumulation. J Virol. 2006;80:5156–5167. doi: 10.1128/JVI.02349-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid SP, Valmas C, Martinez O, Sanchez FM, Basler CF. Ebola virus VP24 proteins inhibit the interaction of NPI-1 subfamily karyopherin alpha proteins with activated STAT1. J Virol. 2007;81:13469–13477. doi: 10.1128/JVI.01097-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed MF, Kolokoltsov Aa, Albrecht T, Davey Ra. Cellular Entry of Ebola Virus Involves Uptake by a Macropinocytosis-Like Mechanism and Subsequent Trafficking through Early and Late Endosomes. PLoS Pathog. 2010;6:e1001110. doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez a, Kiley MP. Identification and analysis of Ebola virus messenger RNA. Virology. 1987;157:414–420. doi: 10.1016/0042-6822(87)90283-2. [DOI] [PubMed] [Google Scholar]
- Sanchez A, Kiley MP, Holloway BP, Auperin DD. Sequence analysis of the Ebola virus genome: organization, genetic elements, and comparison with the genome of Marburg virus. Virus Res. 1993;29:215–240. doi: 10.1016/0168-1702(93)90063-s. [DOI] [PubMed] [Google Scholar]
- Sanchez AAJ, Lukwiya M, Bausch D, Mahanty S, Wagoner KD, Rollin PE. Analysis of human peripheral blood samples from fatal and nonfatal cases of Ebola (Sudan) hemorrhagic fever: cellular responses, virus load, and nitric oxide levels. J Virol. 2004;78:10370–10377. doi: 10.1128/JVI.78.19.10370-10377.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schornberg K, Matsuyama S, Kabsch K, Delos S, Bouton A, White J. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J Virol. 2006;80:4174–4178. doi: 10.1128/JVI.80.8.4174-4178.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schornberg KL, Shoemaker CJ, Dube D, Abshire MY, Delos SE, Bouton AH, White JM. Alpha5beta1-integrin controls ebolavirus entry by regulating endosomal cathepsins. Proc Natl Acad Sci U S A. 2009;106:8003–8008. doi: 10.1073/pnas.0807578106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schümann M, Gantke T, Mühlberger E. Ebola virus VP35 antagonizes PKR activity through its C-terminal interferon inhibitory domain. J Virol. 2009;83:8993–8997. doi: 10.1128/JVI.00523-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shabman RS, Gulcicek EE, Stone KL, Basler CF. The Ebola virus VP24 protein prevents hnRNP C1/C2 binding to karyopherin α1 and partially alters its nuclear import. J Infect Dis. 2011;204(Suppl):S904–10. doi: 10.1093/infdis/jir323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimojima M, Takada A, Ebihara H, Neumann G, Fujioka K, Irimura T, Jones S, Feldmann H, Kawaoka Y. Tyro3 family-mediated cell entry of Ebola and Marburg viruses. J Virol. 2006;80:10109–10116. doi: 10.1128/JVI.01157-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimojima M, Ikeda Y, Kawaoka Y. The mechanism of Axl-mediated Ebola virus infection. J Infect Dis. 2007;196(Suppl):S259–63. doi: 10.1086/520594. [DOI] [PubMed] [Google Scholar]
- Simmons G, Reeves JD, Grogan CC, Vandenberghe LH, Baribaud F, Whitbeck JC, Burke E, Buchmeier MJ, Soilleux EJ, Riley JL, et al. DC-SIGN and DC-SIGNR bind ebola glycoproteins and enhance infection of macrophages and endothelial cells. Virology. 2003;305:115–123. doi: 10.1006/viro.2002.1730. [DOI] [PubMed] [Google Scholar]
- Stahelin RV. Membrane binding and bending in Ebola VP40 assembly and egress. Front Microbiol. 2014;5:300. doi: 10.3389/fmicb.2014.00300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley DA, Honko AN, Asiedu C, Trefry JC, Lau-Kilby AW, Johnson JC, Hensley L, Ammendola V, Abbate A, Grazioli F, et al. Chimpanzee adenovirus vaccine generates acute and durable protective immunity against ebolavirus challenge. Nat Med. 2014:18–23. doi: 10.1038/nm.3702. [DOI] [PubMed] [Google Scholar]
- Sullivan NJ, Hensley L, Asiedu C, Geisbert TW, Stanley D, Johnson J, Honko A, Olinger G, Bailey M, Geisbert JB, et al. CD8+ cellular immunity mediates rAd5 vaccine protection against Ebola virus infection of nonhuman primates. Nat Med. 2011;17:1128–1131. doi: 10.1038/nm.2447. [DOI] [PubMed] [Google Scholar]
- Takada A, Watanabe S, Ito H, Okazaki K, Kida H, Kawaoka Y. Downregulation of beta1 integrins by Ebola virus glycoprotein: implication for virus entry. Virology. 2000;278:20–26. doi: 10.1006/viro.2000.0601. [DOI] [PubMed] [Google Scholar]
- Volchkov VE, Blinov VM, Netesov SV. The envelope glycoprotein of Ebola virus contains an immunosuppressive-like domain similar to oncogenic retroviruses. FEBS Lett. 1992;305:181–184. doi: 10.1016/0014-5793(92)80662-z. [DOI] [PubMed] [Google Scholar]
- Volchkova Va, Dolnik O, Martinez MJ, Reynard O, Volchkov VE. Genomic RNA editing and its impact on Ebola virus adaptation during serial passages in cell culture and infection of guinea pigs. J Infect Dis. 2011;204(Suppl):S941–6. doi: 10.1093/infdis/jir321. [DOI] [PubMed] [Google Scholar]
- Wauquier N, Becquart P, Padilla C, Baize S, Leroy EM. Human fatal zaire ebola virus infection is associated with an aberrant innate immunity and with massive lymphocyte apoptosis. PLoS Negl Trop Dis. 2010:4. doi: 10.1371/journal.pntd.0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Z, Zhao B, Song K, Hu X, Chen W, Kong D, Ge J, Bu Z. Recombinant lentogenic Newcastle disease virus expressing Ebola virus GP infects cells independently of exogenous trypsin and uses macropinocytosis as the major pathway for cell entry. Virol J. 2013;10:331. doi: 10.1186/1743-422X-10-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wimmer P, Schreiner S, Dobner T. Human pathogens and the host cell SUMOylation system. J Virol. 2012;86:642–654. doi: 10.1128/JVI.06227-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wool-Lewis RJ, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong G, Richardson JS, Pillet S, Patel A, Qiu X, Alimonti J, Hogan J, Zhang Y, Takada A, Feldmann H, et al. Immune parameters correlate with protection against ebola virus infection in rodents and nonhuman primates. Sci Transl Med. 2012;4:158ra146. doi: 10.1126/scitranslmed.3004582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu W, Edwards MRR, Borek DMM, Feagins ARR, Mittal A, Alinger JBB, Berry KNN, Yen B, Hamilton J, Brett TJJ, et al. Ebola Virus VP24 Targets a Unique NLS Binding Site on Karyopherin Alpha 5 to Selectively Compete with Nuclear Import of Phosphorylated STAT1. Cell Host Microbe. 2014;16:187–200. doi: 10.1016/j.chom.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaddanapudi K, Palacios G, Towner JS, Chen I, Sariol Ca, Nichol ST, Lipkin WI. Implication of a retrovirus-like glycoprotein peptide in the immunopathogenesis of Ebola and Marburg viruses. FASEB J. 2006;20:2519–2530. doi: 10.1096/fj.06-6151com. [DOI] [PubMed] [Google Scholar]
- Yang Z, Delgado R, Xu L, Todd RF, Nabel EG, Sanchez A, Nabel GJ. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science. 1998;279:1034–1037. doi: 10.1126/science.279.5353.1034. [DOI] [PubMed] [Google Scholar]
- Yang ZY, Duckers HJ, Sullivan NJ, Sanchez a, Nabel EG, Nabel GJ. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med. 2000;6:886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]
- Zachowski A. Phospholipids in animal eukaryotic membranes: transverse asymmetry and movement. Biochem J. 1993;294:1–14. doi: 10.1042/bj2940001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagórska A, Través PG, Lew ED, Dransfield I, Lemke G. Diversification of TAM receptor tyrosine kinase function. Nat Immunol. 2014;15:920–930. doi: 10.1038/ni.2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang APP, Bornholdt Za, Liu T, Abelson DM, Lee DE, Li S, Woods VL, Saphire EO. The ebola virus interferon antagonist VP24 directly binds STAT1 and has a novel, pyramidal fold. PLoS Pathog. 2012;8:e1002550. doi: 10.1371/journal.ppat.1002550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Cherukuri NC, Jackel JN, Wu Z, Crary M, Buckley KJ, Bisaro DM, Parris DS. Characterization of the RNA silencing suppression activity of the Ebola virus VP35 protein in plants and mammalian cells. J Virol. 2012;86:3038–3049. doi: 10.1128/JVI.05741-11. [DOI] [PMC free article] [PubMed] [Google Scholar]