INTRODUCTION
In the United States, there were nearly 50,000 new cases of HIV per year in adults between 2006 and 2009.[1] There are notable geographic differences in the distribution of HIV, with the largest burden of HIV in the Southern United States.[2,3] Complex social forces, including socioeconomic factors and gender, are thought to contribute to growing disparities in HIV incidence in the United States.[4] The HIV epidemic in the United States is considered a concentrated epidemic.[5] However, HIV prevalence among Americans living in urban poor areas exceeds 2%, calling into question whether HIV should be considered a generalized epidemic in the setting of poverty.[6] Research has shown that poverty, above other social determinants such as gender, race/ethnicity, and sexual orientation, is the driver of the changing shape of the HIV epidemic today.[6,7] Multiple studies have demonstrated an association between psychological factors, including major depression, substance use, and experiences of violence, and HIV risk behavior.[8–12] These factors are thought to increase HIV risk by fueling HIV risk-taking behaviors, including increased engagement unprotected sex and/or an increase in number of partners or partner concurrency.[13,14] While each risk factor may operate via separate pathways (e.g., through impaired decision making the ability to negotiate condom use), the co-occurrence of multiple psychological factors may further augment HIV risk-taking behavior. The co-occurrence of multiple, potentially interacting, factors has been labeled syndemics, and recognizes the crucial role of adverse social structures (e.g., poverty) in facilitating the clustering of health-related problems by person, place, or time.[15] As first proposed Singer in 1994[16], syndemics include both epidemics of disease and of the social conditions that independently and jointly contribute to adverse health. In relation to HIV, this recognizes that social inequality (e.g., poverty) plays a crucial role in the clustering of factors that facilitate HIV vulnerability leading to the heightened potential for transmission and acquisition of HIV infection[15–18]
Facilitated by the upstream impact of social inequalities, this co-occurrence of factors is thought to lead to negative health consequences, including increased vulnerability for HIV infection.[15,18,19] For example, an increasing number of childhood adverse experiences (i.e., abuse or neglect, witnessing or experiencing violent crime, family financial problems) have been shown to have a dose-response relationship with negative health outcomes.[20] With respect to HIV, a syndemic perspective has been readily employed to assess the with disproportionate burden of the epidemic among inner city racial and sexual minority populations (e.g., urban poor populations of color).[16] Although multiple studies have documented the importance of syndemics in HIV risk in key populations, particularly among men who have sex with men (MSM)[13,19,21–23], few studies have explicitly considered the role of syndemics on HIV incidence in the general population. Although it has been well established that the HIV epidemic in the United States disproportionately affects those living in poverty, few studies have considered the role of poverty on the relationship between syndemic factors and HIV incidence.
To better understand how psychological and socio-economic factors affect HIV transmission risk according to syndemic theory in the U.S. general population, and to determine if poverty affects this association, we investigated relationships between major depressive disorder, substance use disorder, alcohol use disorder, and intimate partner violence and self-reported newly-diagnosed HIV infection. In addition, we applied a syndemic model per Singer’s original proposed syndemic theory in 1994,[16] and tested whether poverty moderated the association between syndemic psychological factors and HIV infection. We hypothesized that, in the context of poverty, the effect of syndemic conditions on newly-diagnosed HIV infection would be exacerbated.
METHODS
Study Sample
Data from Wave 1 (2001–2002, N=43,093) and Wave 2 (2003–2004, N=34,653) of the National Epidemiologic Survey on Alcohol and Related Disorders (NESARC)[24] were analyzed. The NESARC is a longitudinal, population-based, nationally representative epidemiologic study that investigates the prevalence of mental health conditions in the U.S. general population among adults (over 18 years of age) who are non-institutionalized. Non-Latino African Americans, Latinos, and individuals aged 18–24 years were oversampled; data were adjusted for oversampling, and weighted to represent the U.S. general population based on the 2000 U.S. Census. Individuals interviewed in Wave 1 were re-interviewed in Wave 2. Individuals who were not followed up in Wave 2 were more likely to live in poverty, be Latino, male, younger, less educated, unmarried, living in urban areas, Southern, not have psychiatric disorders, and live in higher cost of living states.[25] Complete methods for the NESARC have been previously reported in detail.[24,26,27]
Measures
Psychological syndemic factors
Potential syndemic factors included a diagnosis of major depressive disorder, substance use disorder (including amphetamines, opioids, sedatives, tranquilizers, cocaine, inhalants, hallucinogens, and/or heroin), and alcohol use disorder in the 12-month period prior to Wave 1. Twelve-month major depressive disorder, substance use disorder, and alcohol use disorder were assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV) according to the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) definitions.[28] Because intimate partner violence (IPV) data was not collected in Wave 1, we included any IPV (physical and/or sexual) in the 12-month period prior to Wave 2 as a syndemic factor. IPV was assessed through 5 questions, including 1) “How often did your spouse/partner push, grab or shove you”; 2) “How often did your spouse/partner slap, kick, bite or hit you”; 3) “How often did your spouse/partner threaten you with a weapon like a knife or gun”; 4) “How often did your spouse/partner cut or bruise you”, 5) “How often did your spouse/partner force you to have sex with him/her”; and 6) “How often did your spouse/partner injure you enough that you had to get medical care”.[29] A response of more than never to any of the 6 questions was coded as having experienced IPV in the previous year. Individuals who reported not having a partner or dating during the year prior to Wave 2 were coded as not experiencing IPV.
Poverty
Living in poverty at Wave 1 was coded using 2001 U.S. Poverty Guidelines, and were based on household income and family size.[25,30] In the 48 continental United States, the poverty level was defined as (US$5570 + [number of persons in household]*US$3020), and individuals reporting a household income below this level were coded as living in poverty. For Alaska and Hawaii, slightly higher figures were used in accordance with the U.S. Poverty Guidelines.[30]
Newly-diagnosed HIV infection
Newly-diagnosed HIV infection in the 12-month period prior to Wave 2 was assessed with 2 questions: 1) If the individual tested positive for HIV in the past year prior to the Wave 2 interview and 2) if a doctor confirmed the diagnosis. An affirmative response to both questions was coded as incident HIV infection. Individuals who reported “unknown” if they had been diagnosed with HIV in the past year were coded as missing (N=226) and not included in the analysis.
Covariates
Several potentially confounding variables were included in all multivariable models. These variables were age, sex (female versus male), sexual identity (coded as identified as a sexual minority or no), race/ethnicity (categorized as White/Caucasian, Black/African American, Latino/a, or Other, due to small numbers of incident HIV infections among Asian and American Indian ethnic groups), urbanicity (coded by metropolitan statistical areas (MSA) including living in the central city, outside central city, or not in an MSA), and educational attainment (coded as greater than high school or high school or less).
Statistical Analysis
Proportions for categorical variables and means and standard deviations for continuous variables were obtained for all variables included in multivariable analyses. Bivariate associations between each syndemic factor as well as poverty were obtained using a logistic regression model to assess relationships between each factor.
To test the relationship between syndemic factors and newly-diagnosed HIV infection, first a series of multivariable logistic regression models were used to assess the relationship between each syndemic factor individually and newly-diagnosed HIV infection, adjusted for potentially confounding variables described previously. To test whether an increasing number of co-occurring syndemic factors was associated with a proportional increase in odds of newly-diagnosed HIV infection, syndemic factors were added together to create a variable that reflected the number of co-occurring syndemic factors in the period prior to HIV diagnosis. A multivariable logistic regression model was used to assess the relationship between number of syndemic factors and newly-diagnosed HIV infection.
Finally, we tested the effect of poverty on the relationship between the syndemic factors and newly-diagnosed HIV infection. Poverty was hypothesized to be a moderator of the relationship between syndemic factors and newly-diagnosed HIV infection, and as such would affect the strength of the relationship between the two variables.[31] To test if poverty was a modifier of this association, a product term between poverty and syndemic factors was included in a multivariable logistic regression model, allowing for identification of the effect of the syndemic term on newly-diagnosed HIV infection in subgroups living above and below federal poverty guidelines. Secondary analyses restricting the sample to 1) only males and 2) only females were conducted to assess this relationship in males and females separately. All analyses were appropriately survey-weighted and conducted in Stata 13.1 (StataCorp, College Station, TX).
RESULTS
Table 1 presents characteristics of the study sample (N=34,427), stratified by number of concurrent syndemic factors. The overall percentage of individuals reporting newly-diagnosed HIV infection in the previous year was 0.22%, and increased from 0.19% among individuals with no syndemic factors to 5.1% among individuals with 4 concurrent syndemic factors. Individuals living below the federal poverty guidelines in 2001 experienced a greater burden of syndemic factors. Table 2 shows bivariate associations between each syndemic factor. The only relationship that did not reach statistical significance was the relationship between alcohol use disorder and poverty.
Table 1.
Descriptive characteristics by number of syndemic factors, weighted percent
| Number of Syndemic Factors | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| 0 (N=28,149) | 1 (N=5,344) | 2 (N=794) | 3 (N=123) | 4 (N=17) | Total (N=34,427) | |
|
| ||||||
| HIV seroconversion | 0.19% | 0.24% | 0.46% | 1.7% | 5.1% | 0.22% |
|
| ||||||
| Age (mean, SD), years | 48.0 (18.4) | 39.6 (15.1) | 33.8 (12.1) | 31.0 (10.6) | 25.9 (8.3) | 46.4 (18.2) |
|
| ||||||
| Race/ethnicity | ||||||
| White/Caucasian | 70.9% | 71.1% | 69.4% | 71.4% | 78.9% | 70.9% |
| Black/African American | 11.1% | 11.0% | 11.2% | 10.0% | 13.0% | 11.0% |
| Latino/a | 11.5% | 12.0% | 12.6% | 10.5% | 1.5% | 11.6% |
| Other | 6.6% | 5.9% | 6.9% | 8.1% | 6.6% | 6.5% |
|
| ||||||
| Female sex | 53.1% | 47.4% | 47.4% | 41.0% | 39.2% | 52.1% |
|
| ||||||
| Sexual minority identity (gay, lesbian, bisexual) | 2.5% | 3.6% | 5.0% | 6.0% | 12.4% | 2.7% |
|
| ||||||
| Urbanicity | ||||||
| In MSA1 – central city | 28.5% | 30.5% | 32.0% | 29.4% | 39.2% | 28.9% |
| In MSA1 – outside central city | 51.3% | 48.2% | 45.9% | 44.2% | 38.7% | 50.6% |
| Not in MSA1 | 20.3% | 21.4% | 22.2% | 26.3% | 22.1% | 20.5% |
|
| ||||||
| Greater than high school education | 59.8% | 61.5% | 58.2% | 50.6% | 55.3% | 60.0% |
|
| ||||||
| Living below federal poverty guidelines | 11.4% | 14.3% | 16.3% | 24.3% | 29.3% | 12.0% |
Metropolitan statistical areas (MSA)
Table 2.
Associations between each syndemic factor
| Major Depressive Disorder | Substance Use Disorder | Alcohol Use Disorder | Intimate Partner Violence | Poverty | |
|---|---|---|---|---|---|
| Major Depressive Disorder | |||||
| Substance Use Disorder | 6.72 (5.66 to 7.99) | ||||
| Alcohol Use Disorder | 2.26 (2.10 to 2.44) | 20.3 (17.7 to 23.3) | |||
| Intimate Partner Violence | 2.07 (1.86 to 2.29) | 4.93 (4.17 to 5.82) | 2.56 (2.37 to 2.77) | ||
| Poverty | 1.79 (1.66 to 1.94) | 2.01 (1.62 to 2.49) | 0.97 (0.88 to 1.07) | 1.33 (1.18 to 1.49) |
Bivariate weighted logistic regression model
Table 3 shows bivariate and multivariable associations between each syndemic factor individually and newly-diagnosed HIV infection, as well bivariate and multivariable models modeling the additive effect of syndemic factors on newly-diagnosed HIV infection. Other than major depressive disorder, all syndemic factors were individually associated with HIV incidence, including substance use disorder (aOR 3.71, 95% CI 3.12 to 4.40), alcohol use disorder (aOR 1.31, 95% CI 1.16 to 1.47), and IPV (aOR 2.30, 95% CI 1.65 to 3.19), adjusting for potentially confounding factors. In the additive syndemic model, every additional syndemic factor was associated with a 47% increase in odds of HIV infection (aOR 1.47, 95% CI 1.30 to 1.65).
Table 3.
Association between syndemic factors and HIV incidence
| Unadjusted Models1 | Multivariable Models2 | |||
|---|---|---|---|---|
| OR (95% CI) | P-value | aOR (95% CI) | P-value | |
| Major depressive disorder | 1.44 (1.15 to 1.81) | 0.002 | 1.19 (0.94 to 1.51) | 0.15 |
| Substance use disorder | 5.79 (4.99 to 6.73) | <0.001 | 3.71 (3.12 to 4.40) | <0.001 |
| Alcohol use disorder | 1.68 (1.47 to 1.92) | <0.001 | 1.31 (1.16 to 1.47) | <0.001 |
| Intimate partner violence | 2.93 (2.22 to 3.86) | <0.001 | 2.28 (1.64 to 3.18) | <0.001 |
| Additive syndemic factors | 1.73 (1.56 to 1.93) | <0.001 | 1.46 (1.30 to 1.65) | <0.001 |
| Restricted to Women Only | ||||
| Major depressive disorder | 1.64 (1.29 to 2.10) | <0.001 | 1.60 (1.22 to 2.09) | 0.001 |
| Substance use disorder | ** | ** | ||
| Alcohol use disorder | 1.01 (0.82 to 1.24) | 0.95 | 1.00 (0.78 to 1.27) | 0.97 |
| Intimate partner violence | 3.81 (2.11 to 6.86) | <0.001 | 2.32 (1.18 to 4.55) | 0.015 |
| Additive syndemic factors | 1.62 (1.28 to 2.04) | <0.001 | 1.47 (1.11 to 1.95) | 0.008 |
| Restricted to Men Only | ||||
| Major depressive disorder | 1.44 (0.89 to 2.33) | 0.13 | 0.93 (0.57 to 1.52) | 0.78 |
| Substance use disorder | 7.85 (6.52 to 9.44) | <0.001 | 4.27 (3.35 to 4.45) | <0.001 |
| Alcohol use disorder | 1.72 (1.49 to 1.98) | <0.001 | 1.44 (1.29 to 1.61) | <0.001 |
| Intimate partner violence | 2.32 (2.05 to 2.63) | <0.001 | 2.33 (1.87 to 2.89) | <0.001 |
| Additive syndemic factors | 1.76 (1.60 to 1.94) | <0.001 | 1.49 (1.32 to 1.68) | <0.001 |
No women with substance use disorder had a newly diagnosed HIV infection;
Survey-weighted bivariate logistic regression models;
Survey-weighted multivariable logistic regression models adjusting for age, sex, sexual identity, race/ethnicity, urbanicity, and education
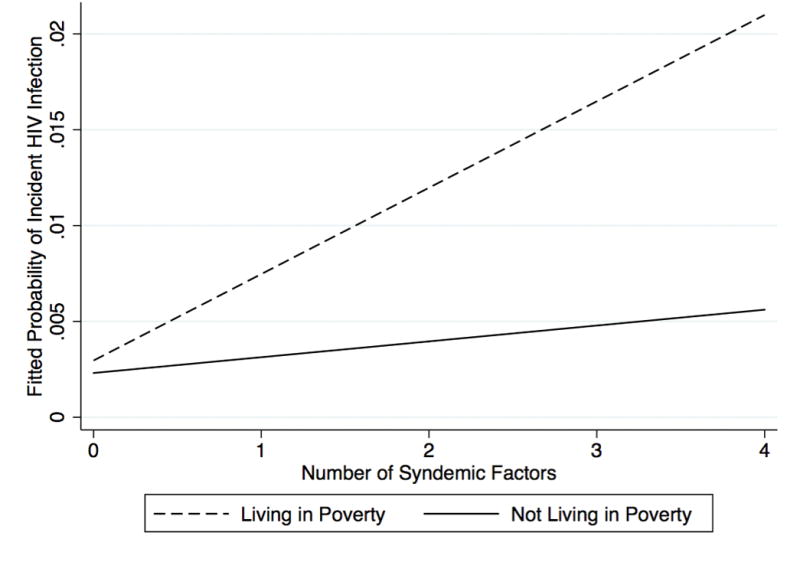
Table 4 displays results of a multivariable model assessing modification of the relationship between syndemic factors and newly-diagnosed HIV infection by poverty status. Figure 1 graphically displays regression slopes for the additive effect of syndemic factors on probability of incident HIV infection among individuals living above compared to below poverty guidelines. Among individuals who lived below federal poverty guidelines, every additional syndemic factor was associated with a 96% increase in odds of incident HIV (aOR 1.96, 95% CI 1.57 to 2.44), compared to a 21% increase among individuals living above federal poverty guidelines (aOR 1.21, 95% CI 1.07 to 1.36). In an analysis stratifying by sex, the strongest association between syndemic factors and newly diagnosed HIV infection was among males who lived below the poverty line (aOR 4.15, 95% CI 2.71 to 6.37).
Table 4.
Association between syndemic factors and newly diagnosed HIV by poverty status and sex
| Multivariable Models1, Entire Sample | Multivariable Models2, Women Only | Multivariable Models3, Men Only | |||||||
|---|---|---|---|---|---|---|---|---|---|
| aOR (95% CI) | P-value | P-value for Interaction | aOR (95% CI) | P-value | P-value for Interaction | aOR (95% CI) | P-value | P-value for Interaction | |
| Additive syndemic factors among individuals living below the poverty line | 1.96 (1.57 to 2.44) | <0.001 | 1.64 (1.15 to 2.34) | 0.007 | 4.15 (2.71 to 6.37) | <0.001 | |||
| Additive syndemic factors among individuals living above the poverty line | 1.21 (1.07 to 1.36) | 0.002 | <0.001 | 1.15 (0.86 to 1.54) | 0.34 | 0.08 | 1.15 (1.01 to 1.32) | 0.03 | <0.001 |
Survey-weighted multivariable logistic regression model with main effect terms for syndemic factors and poverty and interaction term for syndemic factors*poverty adjusted for age, sex, sexual identity, race/ethnicity, urbanicity, and education;
Survey-weighted multivariable logistic regression model with main effect terms for syndemic factors and poverty and interaction term for syndemic factors*poverty adjusted for age, sexual identity, race/ethnicity, urbanicity, and education and restricted only to participants reporting female sex;
Survey-weighted multivariable logistic regression model with main effect terms for syndemic factors and poverty and interaction term for syndemic factors*poverty adjusted for age, sexual identity, race/ethnicity, urbanicity, and education and restricted only to participants reporting male sex
Figure 1.
DISCUSSION
Our results indicate a significant association between co-morbid psychological conditions and partner violence and newly-diagnosed HIV infection in the U.S. general population, constituting a syndemic condition of psychological factors and HIV risk. The existence of a syndemic condition between psychological factors and both HIV risk and incident HIV infection has been well established among MSM.[13,19,21,22] Results of studies among MSM have consistently shown that odds of HIV and/or HIV risk are proportional to increasing numbers of syndemic factors.[13,21,32,33] The results of the present study indicate that there may be a similar relationship between syndemic factors and newly-diagnosed HIV infection in the U.S. general population, and that this relationship may be amplified in the setting of poverty.
Here, we found evidence that poverty is a modifier of the relationship between syndemic factors and newly-diagnosed HIV infection. Among females in particular, an increase in the number of syndemic conditions was only associated with HIV in the context of poverty, and among males this relationship was considerably stronger in the context of poverty. Individuals of lower socio-economic status may be more likely to experience a greater number of co-occurring syndemic factors and thus have increased vulnerability to HIV infection. It is well established that the HIV epidemic in the United States is concentrated geographically in areas that are economically disadvantaged and among those living in poverty.[3,36] In the United States, lower socio-economic status has been described as both a risk factor for and a result of psychiatric disorders.[37] Conditions associated with living in poverty, such as crowding, underemployment, financial and other stress, and exposure to violence may increase the risk of one or more psychiatric disorders.[38] Moreover, IPV is differentially distributed and more prevalent in areas of lower socio-economic status, which could be due to chronic stress of poverty and/or gender inequality.[39] Guided by syndemic theory, we recognize the importance of social context by assessing the association between syndemic factors, poverty, and HIV risk. Whereas the clustering of risk factors, or co-occurrence alone, is important, these results demonstrate that social inequality, here defined as poverty, modifies this relationship. These results suggest that poverty potentiates the association between these syndemic factors and HIV infection. For example, stress related to living in poverty could increase risk for psychiatric conditions, or exacerbate responses to syndemic factors in the form of increased HIV risk-taking behavior. Further work elucidating this pathway specifically will be important to understand how best to design interventions that address the heightened effect of syndemic factors in the setting of poverty.
The results of this study must be considered in the context of several limitations. HIV diagnoses were obtained via self-report, and HIV testing was not done as part of the NESARC study. This could introduce misclassification bias especially in that to be diagnosed with HIV infection, one must be tested for HIV. A differential distribution in access to HIV testing access could therefore bias results. In the United States, there are disparities in access to HIV testing and care services with respect to poverty, urbanicity, and ethnic or racial background.[40] If individuals living below the poverty line or who had more syndemic factors were less likely to have been tested and thus know their result, there may be a downward bias in study results. Similarly, individuals may not wish to disclose HIV status, which could introduce bias. Future work should consider the effect of syndemics on biological assay-confirmed HIV incidence. However, this study represents one of the largest prospective studies that includes measures of newly-diagnosed HIV infection with validated measures of psychiatric disorders, which gives this study the ability to consider not only the effect of syndemic factors but how they are modified by poverty. An additional limitation is that we were unable to control for sexual risk-taking behavior in this study, due to lack of assessment of recent HIV sexual risk behavior prior to the period on which HIV incidence was assessed. In addition, IPV was only assessed among participants who reported being in a relationship in the year prior to Wave 2. It is possible that individuals experienced IPV outside of a relationship, which would not be captured here and thus could introduce misclassification. Poverty is only a single dimension of adverse social context. Although we believe this is a robust measure, it is possible that important dimensions of inequalities (i.e., stigma, security, neighborhood environment) are not captured by this analysis. Finally, given the relatively small number of new HIV diagnoses recorded in this study, we were unable to stratify more finely and assess the relationship between syndemic factors and specific subgroups of the population beyond those living in poverty. Future work should consider the moderating role of poverty on the relationship between syndemic factors and HIV incidence within specific subgroups, such as racial/ethnic minorities, in order to better understand how poverty affects this relationship.
This study provides additional evidence that co-occurring psychological and socio-economic conditions increase vulnerability to new HIV infection among the general population in the United States in a similar fashion as seen in MSM.[13,21,22] Importantly, this effect was considerably stronger among people living below federal poverty guidelines, and particularly among males living in the context of poverty. These results underscore that poverty is a key social determinant of health inequity and a core aspect of syndemic theory.[16] We recommend that future analyses examine the association between co-occurring individual psychological factors and HIV infection explicitly consider and incorporate socio-economic factors, such as poverty.
Acknowledgments
Funding
CEO was supported by a National Institute of Allergy and Infectious Disease T32 NRSA grant (T32AI007535; PI: Seage) and is currently supported by a National Institute of Drug Abuse T32 NRSA (T32DA0131911; PI: Flanigan). APB is supported by Eunice Kennedy Shriver National Institute of Child Health & Human Development T32 HD049339 (PI: Nathanson) and the National Institutes of Mental Health R25 MH083620 (PI: Flanigan).
Footnotes
Conflicts of Interest
None to declare.
Author Contributions
CEO designed the study, conducted analyses, interpreted results, and drafted the manuscript. APB designed the study, interpreted results, and drafted the manuscript. SLR designed the study, interpreted results, and drafted the manuscript. All authors critically reviewed and approved the final version of the manuscript.
References
- 1.Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, et al. Estimated HIV Incidence in the United States, 2006–2009. PLoS ONE. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adimora AA, Ramirez C, Schoenbach VJ, Cohen MS. Policies and politics that promote HIV infection in the Southern United States. AIDS. 2014:1. doi: 10.1097/QAD.0000000000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nunn A, Yolken A, Cutler B, Trooskin S, Wilson P, Little S, et al. Geography Should Not Be Destiny: Focusing HIV/AIDS Implementation Research and Programs on Microepidemics in US Neighborhoods. Am J Public Health. 2014:775–780. doi: 10.2105/AJPH.2013.301864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aral SO, Adimora AA, Fenton KA. Understanding and responding to disparities in HIV and other sexually transmitted infections in African Americans. The Lancet. 2008;372:337–340. doi: 10.1016/S0140-6736(08)61118-6. [DOI] [PubMed] [Google Scholar]
- 5.Campsmith ML, Rhodes P, Hall HI, Green T. HIV Prevalence Estimates — United States, 2006. MMWR Recomm Rep. 2008;57:1073–1076. [PubMed] [Google Scholar]
- 6.Denning P, DiNenno E. Communities in Crisis: Is there a generalized HIV epidemic in impoverished urban areas of the United States? [Google Scholar]
- 7.Centers for Disease Control and Prevention. Characteristics Associated with HIV Infection Among Heterosexuals in Urban Areas with High AIDS Prevalence — 24 Cities, United States, 2006–2007. MMWR Recomm Rep. 2011;60:1045–1049. [PubMed] [Google Scholar]
- 8.Armstrong G, Jorm AF, Samson L, Joubert L, Nuken A, Singh S, et al. Association of Depression, Anxiety, and Suicidal Ideation With High-Risk Behaviors Among Men Who Inject Drugs in Delhi, India. J Acquir Immune Defic Syndr. 2013;64:502–510. doi: 10.1097/QAI.0b013e3182a7ef21. [DOI] [PubMed] [Google Scholar]
- 9.Reisner SL, Falb KL, Mimiaga MJ. Early Life Traumatic Stressors and the Mediating Role of PTSD in Incident HIV Infection Among US Men, Comparisons by Sexual Orientation and Race/Ethnicity: Results From the NESARC, 2004–2005. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2011;57:340–350. doi: 10.1097/QAI.0b013e31821d36b4. [DOI] [PubMed] [Google Scholar]
- 10.Bedoya CA, Mimiaga MJ, Beauchamp G, Donnell D, Mayer KH, Safren SA. Predictors of HIV Transmission Risk Behavior and Seroconversion Among Latino Men Who have Sex with Men in Project EXPLORE. AIDS Behav. 2011;16:608–617. doi: 10.1007/s10461-011-9911-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mimiaga MJ, Noonan E, Donnell D, Safren SA, Koenen KC, Gortmaker S, et al. Childhood Sexual Abuse Is Highly Associated With HIV Risk–Taking Behavior and Infection Among MSM in the EXPLORE Study. J Acquir Immune Defic Syndr. 2009;51:340348. doi: 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reisner S, Mimiaga M, Bland S, Skeer M, Cranston K, Isenberg D, et al. Problematic alcohol use and HIV risk among Black men who have sex with men in Massachusetts. AIDS Care. 2010;22:577–587. doi: 10.1080/09540120903311482. [DOI] [PubMed] [Google Scholar]
- 13.Biello KB, Colby D, Closson E, Mimiaga MJ. The Syndemic Condition of Psychosocial Problems and HIV Risk Among Male Sex Workers in Ho Chi Minh City, Vietnam. AIDS Behav. doi: 10.1007/s10461-013-0632-8. Published Online First: 1 October 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mimiaga MJ, Reisner SL, Pantalone DW, O’Cleirigh C, Mayer KH, Safren SA. A Pilot Trial of Integrated Behavioral Activation and Sexual Risk Reduction Counseling for HIV-Uninfected Men Who Have Sex with Men Abusing Crystal Methamphetamine. AIDS Patient Care and STDs. 2012;26:681–693. doi: 10.1089/apc.2012.0216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singer MC, Clair S. Syndemics and Public Health: Reconceptualizing Disease in Bio-Social Context. Medical Anthropology Quarterly. 2004;17:423–441. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- 16.Singer MC. AIDS and the health crisis of the U.S. urban poor; the perspective of critical medical anthropology. Soc Sci Med. 1994;39:931–948. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- 17.Singer MC. Introduction to Syndemics: A Systems Approach to Public and Community Health. San Francisco: Jossey-Bass; 2009. [Google Scholar]
- 18.Singer MC, Erickson PI, Badiane L, Diaz R, Ortiz D, Abraham T, et al. Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Social Science & Medicine. 2006;63:2010–2021. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of Co-Occurring Psychosocial Health Problems and Increased Vulnerability to HIV/AIDS Among Urban Men who have Sex with Men. Am J Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the U. S. Child Abuse & Neglect. 2013;37:917–925. doi: 10.1016/j.chiabu.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wim VB, Christiana N, Marie L. Syndemic and Other Risk Factors for Unprotected Anal Intercourse Among an Online Sample of Belgian HIV Negative Men Who have Sex with Men. AIDS Behav. 2013;18:50–58. doi: 10.1007/s10461-013-0516-y. [DOI] [PubMed] [Google Scholar]
- 22.Santos GM, Do T, Beck J, Makofane K, Arreola S, Pyun T, et al. Syndemic conditions associated with increased HIV risk in a global sample of men who have sex with men. Sexually Transmitted Infections. doi: 10.1136/sextrans-2013-051318. Published Online First: 15 January 2014. [DOI] [PubMed] [Google Scholar]
- 23.Jie W, Ciyong L, Xueqing D, Hui W, Lingyao H. A Syndemic of Psychosocial Problems Places the MSM (Men Who Have Sex with Men) Population at Greater Risk of HIV Infection. PLoS ONE. 2012;7:e32312. doi: 10.1371/journal.pone.0032312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grant BF, Kaplan K. National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Source and Accuracy Statement. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2005. [Google Scholar]
- 25.Thompson RG, Jr, Wall MM, Greenstein E, Grant BF, Hasin DS. Substance-Use Disorders and Poverty as Prospective Predictors of First-Time Homelessness in the United States. Am J Public Health. 2013;103:S282–S288. doi: 10.2105/AJPH.2013.301302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grant BF, Kaplan K, Shepard J. Source and Accuracy Statement for Wave 1 of the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 27.Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, et al. Prevalence and Co-occurrence of Substance Use Disorders and Independent Moodand Anxiety Disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 28.Grant BF, Harford TC, Dawson DA, Chou P, Pickering RP. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- 29.Hahn JW, McCormick MC, Silverman JG, Robinson EB, Koenen KC. Examining the Impact of Disability Status on Intimate Partner Violence Victimization in a Population Sample. Journal of Interpersonal Violence. doi: 10.1177/0886260514534527. Published Online First: 23 May 2014. [DOI] [PubMed] [Google Scholar]
- 30.Federal Communications Commission. Fed Regist. 2001. Public Safety Communications. [Google Scholar]
- 31.Baron RM, Kenny DA. The Moderator-Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 32.O’Leary A, Jemmott JB, Stevens R, Rutledge SE, Icard LD. Optimism and Education Buffer the Effects of Syndemic Conditions on HIV Status Among African American Men Who Have Sex with Men. AIDS Behav. doi: 10.1007/s10461-014-0708-0. Published Online First: 6 April 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O’Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, Safren SA. Moderate Levels of Depression Predict Sexual Transmission Risk in HIV-Infected MSM: A Longitudinal Analysis of Data From Six Sites Involved in a “Prevention for Positives” Study. AIDS Behav. 2013;17:1764–1769. doi: 10.1007/s10461-013-0462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCabe BE, Feaster DJ, Mitrani VB. Addictive Behaviors. Addictive Behaviors. 2014;39:725–728. doi: 10.1016/j.addbeh.2013.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reingle JM, Jennings WG, Connell NM, Businelle MS, Chartier K. On the Pervasiveness of Event-Specific Alcohol Use, General Substance Use, and Mental Health Problems as Risk Factors for Intimate Partner Violence. Journal of Interpersonal Violence. doi: 10.1177/0886260514527172. Published Online First: 24 March 2014. [DOI] [PubMed] [Google Scholar]
- 36.Buot M-LG, Docena JP, Ratemo BK, Bittner MJ, Burlew JT, Nuritdinov AR, et al. Beyond Race and Place: Distal Sociological Determinants of HIV Disparities. PLoS ONE. 2014;9:e91711. doi: 10.1371/journal.pone.0091711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Anakwenze U, Zuberi D. Mental Health and Poverty in the Inner City. Health & Social Work. 2013;38:147–157. doi: 10.1093/hsw/hlt013. [DOI] [PubMed] [Google Scholar]
- 38.Cromley EK, Wilson-Genderson M, Pruchno RA. Neighborhood characteristics and depressive symptoms of older people: Local spatial analyses. Social Science & Medicine. 2012;75:2307–2316. doi: 10.1016/j.socscimed.2012.08.033. [DOI] [PubMed] [Google Scholar]
- 39.Tsai AC. Intimate Partner Violence and Population Mental Health: Why Poverty and Gender Inequities Matter. PLoS Medicine. 2013;10:1–3. doi: 10.1371/journal.pmed.1001440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Penner M, Leone PA. Integration of Testing for, Prevention of, and Access to Treatment for HIV Infection: State and Local Perspectives. Clinical Infectious Diseases. 2007;45:S281–S286. doi: 10.1086/522551. [DOI] [PubMed] [Google Scholar]


