Abstract
Children with social dysfunction and a first-degree relative with schizophrenia are at elevated risk for schizophrenia; however, the nature of this dysfunction is unclear. It was hypothesized that familial high-risk (HR) children and adolescents (n = 17) would have social skill deficits relative to healthy controls (HC; n = 35). HR participants had a bimodal distribution of social skill scores (47% excellent; 53% poor). HR participants had worse social skills, assertion and empathy scores, suggesting possible developmental precursors to the social amotivation domain of negative symptoms. Characterizing HR children's social deficits could assist identification of those at risk for schizophrenia.
Keywords: High-risk, Schizophrenia, Social skills, Premorbid adjustment, Social anhedonia, Social amotivation, Negative symptoms
1. Introduction
Children and adolescents who have a first-degree relative with schizophrenia and manifest poor social functioning have 7–8 times greater odds of developing schizophrenia than high-risk and typical children and adolescents with intact social functioning (Tarbox and Pogue-Geile, 2008). A limitation of previous research is that the nature of social dysfunction in children at familial high risk for schizophrenia (HR) has not been well-characterized in terms of types of deficits and developmental timing, and thus is insufficiently specific as an indicator of liability for schizophrenia.
HR adolescents have impairments in academic and social adjustment (Dworkin et al., 1994; Hans et al., 2000; Niemi et al., 2003), peer and romantic relationships (Glatt et al., 2006), social cognition (Eack et al., 2010), and performance-based measures of social behavior (Schiffman et al., 2004; Gibson et al., 2010). However, less is known about specific domains and timing of deficits in younger HR children.
It is well-established in the literature that people with schizophrenia exhibit a variety of social deficits, and that these likely predate onset of illness by several years, possibly as early as childhood (Bearden et al, 2000; Tarbox and Pogue-Geile, 2008; Tsuji et al., 2013). A social deficit of particular relevance to adults with schizophrenia is social amotivation, a core negative symptom of schizophrenia possibly caused by a disruption in reward functioning, and characterized by reduced ability to anticipate and/or experience pleasure. Social amotivation is comprised of asociality and apathy (Foussias and Remington, 2010). However, few studies have attempted to examine whether there are early developmental precursors or similarities to social amotivation in HR children and adolescents. Social amotivation could be trait-like, and a specific aspect of it (i.e., social anhedonia) may be a sensitive and specific indicator of risk for schizophrenia (Kwapil, 1998). Research is needed to clarify whether early developmental precursors can be detected in this population.
We sought to examine the timing and nature of social deficits in familial HR children (i.e. those with a family history of schizophrenia). It was hypothesized that HR children and adolescents would have deficits in social skills and early indicators of social maladjustment, as contrasted with healthy controls (HC); it was further hypothesized that HR participants would experience impairments on a standardized measure of social skills that potentially represent developmental precursors to social amotivation. We selected the Social Skills Rating System (SSRS; Gresham and Elliot, 1990), a grade- and sex-normed measure that includes subscales tapping social reciprocity, motivation, and initiative (“empathy” and “assertion” subscales).
2. Methods
2.1. Participants
Participants included 52 (35 HC and 17 HR) individuals ages 5–19 who were successfully age- and sex-matched across conditions (see Table 1). Parents of participants were recruited from community churches and organizations, and advertisements in public areas and mental health services. We obtained written informed consent according to the guidelines of the Institutional Review Board. For both HC and HR participants, structured diagnostic assessments (SCID, supplemented by the K-SADS) were conducted to rule out the presence of current Axis I psychiatric disorders.
Table 1.
Demographic characteristics.
| Healthy controls (HC) n = 35 |
High risk (HR) n = 17 |
|
|---|---|---|
| Age [Mean, range, (SD)] | 12.2, 5–19, (3.9) | 13.9, 9–19, (3.3) |
| % Male | 37% | 41% |
| IQ: PPVT III [Mean (SD)] | 112.3 (14.2) | 104.7 (17.0) |
| Ethnicity* (% Non-White) | 22% | 41% |
| Years of child participants' education | 6.7 (3.9) | 9.4 (3.4) |
| Mother's highest level of education [Mean (SD)] | 5.5 (1.1) | 4.5 (1.7) |
| Father's highest level of education [Mean (SD)] | 5.3 (1.3) | 5.7 (1.2) |
| Mother's highest level of occupation* [Mean (SD)] | 6.3 (1.7) | 4.2 (1.9) |
| Father's highest level of occupation* [Mean (SD)] | 6.5 (2.2) | 4.4 (2.4) |
Indicates HC and HR groups significantly differed (p < 0.01).
2.2. Assessment
Social and academic adjustment was assessed using the Cannon-Spoor Premorbid Adjustment Scale (PAS; Cannon-Spoor et al., 1982). This measure retrospectively assesses levels of social and academic functioning within each of four periods of development: 1) Childhood (5–11 years), 2) Early Adolescence (12–15), 3) Late Adolescence (16–18), and 4) Adulthood (19+). Items are assessed on a 0–6 scale (0 = no dysfunction to 6 = extremely dysfunctional). We assessed IQ using the Peabody Picture Vocabulary Test-III (PPVT-III; Dunn and Dunn, 1997).
Social skills were assessed using the child-report version of the Social Skills Rating System (SSRS; Gresham and Elliot, 1990), a standardized instrument providing grade- and sex-normed scores on 5 domains (Assertion, Empathy, Cooperation, Responsibility and Self-Control). Items are assessed in terms of Frequency from 0 (never) to 2 (very often), and Importance from 0 (not important) to 2 (critical).
We confirmed a putative (self-reported) diagnosis of DSM-IV schizophrenia or schizoaffective disorder in parents of children in the HR group by SCID interview with the parent, and scored lifetime levels (1 to 9) of education and occupational achievement using the Hollingshead 4-Factor Index of Socioeconomic Status (1975).
3. Results
Demographics are presented in Table 1. HR children had greater minority representation and lower parental occupational achievement as compared to the HC group but did not differ on other key demographics, suggesting successful age- and sex-matching.
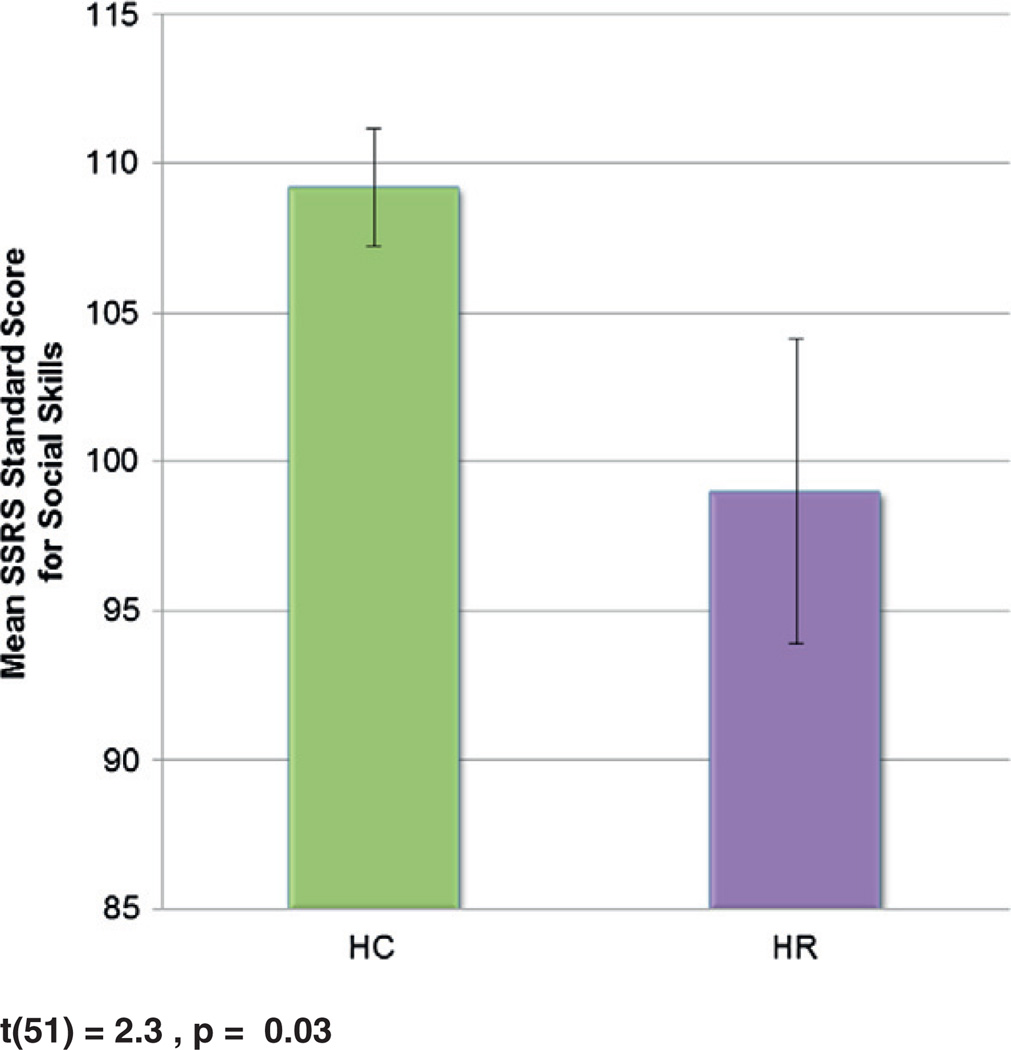
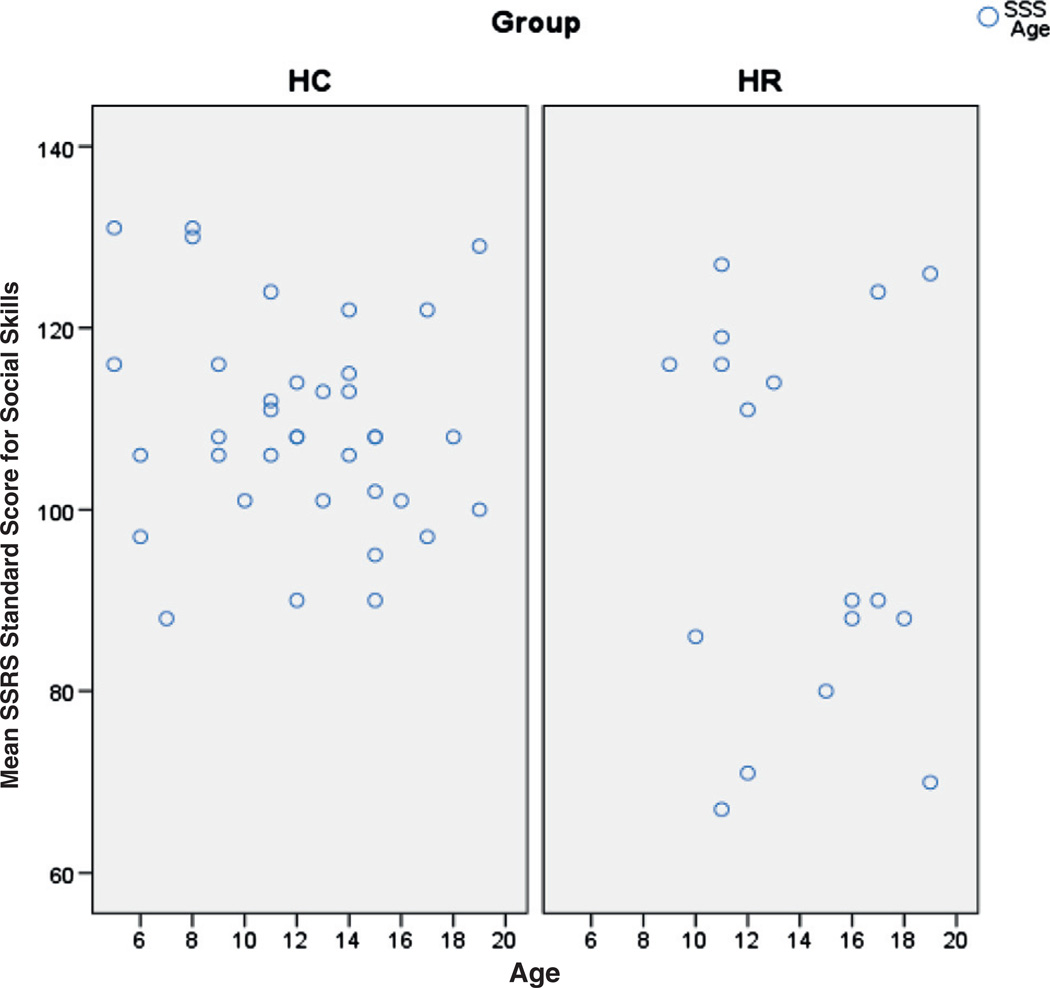
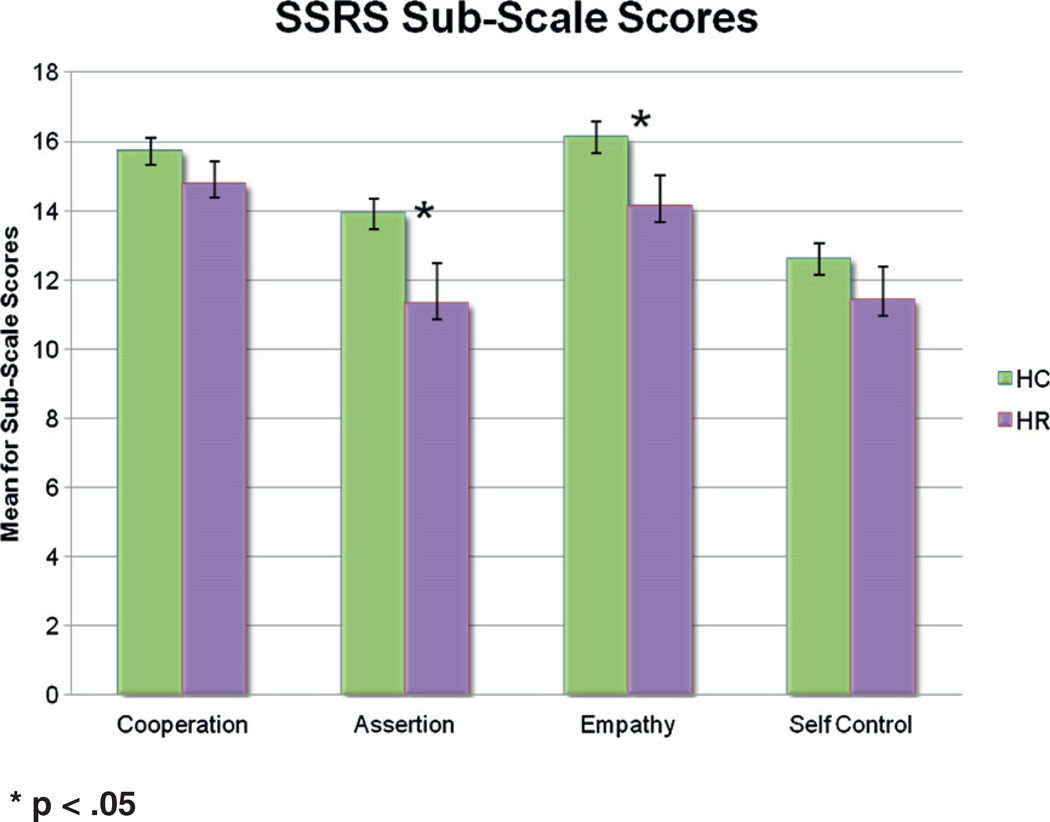
As hypothesized, HR subjects had poorer social skills overall (p < .03; see Fig. 1). The group effect was sustained in a post-hoc analysis of covariance, controlling for occupational status of parents F (1,35) = 6.28, p = 0.02. A striking, albeit unanticipated, finding was that unlike SSRS scores for HC participants, scores for HR participants had a clearly bimodal distribution, with eight participants exhibiting excellent social skills (77th–96th percentile for grade and sex; a ‘High-SS HR’ group) and nine participants exhibiting significantly below normative social skills (2nd–25th percentile; a ‘Low-SS HR’ group) with no individuals scoring in the mid-range (see Fig. 2). High-SS versus Low-SS HR children did not differ in terms of age, sex, education level or parental education and occupation levels. For HR children, poor overall social skills deficits appeared to be driven by specific deficits in “assertion” and “empathy” domains, as compared to other domains (p < .05; see Fig. 3).
Fig. 1.
Overall SSRS scores: HR and HC participants.
Fig. 2.
SSRS scores by age and group.
Fig. 3.
SSRS subscale scores.
For all participants combined, there was a correlation between PAS scores and SSRS scores (r = −0.345, p < .05). In terms of the timing of social deficits, HR participants also had worse social adjustment on the PAS across developmental stages, including middle childhood [ages 5–8, t(43) = −2.70, p = .01]; late childhood [ages 9–11, t(37) = −2.46, p = .02]; early adolescence [ages 12–15, t(24) = −3.29, p = .003]; and late adolescence [ages 16–19, t(8) = −2.52, p < .05]. Notably, these differences were attributable to the subgroup of HR participants with poor social skills, as reflected by results of a repeated measures ANOVA comparing HC, High-SS HR, and Low-SS HR on early and middle childhood PAS scores revealing a trend (p < .055) for a group effect and a difference only between the HC and Low-SS HR groups (p = 0.003). Visual inspection of scatter plots for early and late adolescent PAS scores (for which sample was by definition restricted to the adolescent subjects), revealed the same pattern for each of these subsequent time periods; i.e. divergent scores for the two HR subgroups, with good PAS social adjustment scores characteristic of the High-SS HR group (and overlapping with scores for the HC group) and poor social adjustment characteristic of the Low-SS HR group.
4. Discussion
Given the finding of high- and low-social skill subgroups among familial HR children, future studies should examine whether other HR offspring samples reveal similarly divergent social skills clusters and, if so, probe for risk and protective factors that distinguish these clusters. Moreover, longitudinal studies should aim to determine whether a familial HR group with poor social skills is at greater risk for developing schizophrenia than an HR group with intact social skills. Given our finding that HR children with current social skills deficits also had significant social adjustment problems early in development (ages 5–8), the possibility exists that these difficulties may emerge early in life and persist over time. Both findings suggest that interventions targeting early social deficits in a subgroup could not only prove useful for early social remediation efforts but also may hold promise for future research on early preventive interventions in schizophrenia.
The finding that HR children showed evidence of specific deficiencies in the SSRS “assertion” and “empathy” social skill domains is noteworthy given that items in the “assertion” domain measure social motivation and initiative, and the “empathy” domain measures social reciprocity. Reduced social motivation and reciprocity are common in schizophrenia; amotivation has been conceptualized as a core defining feature reflecting impaired anticipatory pleasure/goal-directed behavior (Gard et al., 2007; Foussias and Remington, 2010). Our findings raise the possibility that developmental precursors of social amotivation may be evident in early childhood. Additional research is needed to clarify whether childhood social impairments in HR children confer risk for schizophrenia and, in particular, the negative symptom domain of social amotivation.
This study has several strengths, including the use of well-established and normed measures of social skills, and successful age- and sex-matching of HR and HC participants. It is not, however, without limitations. The PAS is a retrospective measure of social and academic functioning reported by parents; there may be systematic differences in reporting by parents with and without a diagnosis of schizophrenia. The sample size was relatively small; larger studies are needed to provide further support for these findings and for parsing specific domains of social skills and functioning.
Nonetheless, these findings offer a promising point of departure for future studies of social skill and functioning deficits in HR children and adolescents. There is a need for fine-grained analyses of the types of social impairment experienced by HR children and adolescents, and exploration of how specific social problems may contribute to risk for schizophrenia. Characterization of social skill and functioning deficits in HR children could also inform future efforts to develop more specific and individually-tailored targets for early intervention.
Acknowledgment
This work was supported, in part, by NARSAD Independent Investigator Grant #1098 to the senior author (G. Haas), and infrastructure support funding from the Department of Psychiatry of the University of Pittsburgh School of Medicine. We thank Dr. Matcheri S. Keshavan and Diana Mermon, MS, for their assistance in referral of some of the participants to this study. We thank Shelby Miller, Audrey Brie Latimore, Valerie Michael, and Nicole Pawloski for their assistance in data preparation efforts.
Role of the funding source
All authors declare that they are in compliance with funding body agreements and policies regarding publication.
Footnotes
Contributors
Author 1 managed the literature searches, conducted statistical analyses, and wrote the first draft of the manuscript. Author 2 contributed to the literature search and statistical analyses. Author 3 designed the study, wrote the protocol, and conducted statistical analyses. All authors contributed to and have approved the final manuscript.
Conflict of interest
All authors declare that they have no conflicts of interest.
References
- Bearden CE, Rosso IM, Hollister JM, Sanchez LE, Hadley T, Cannon TD. A prospective cohort study of childhood behavioral deviance and language abnormalities as predictors of adult schizophrenia. Schizophr. Bull. 2000;26(2):395–410. doi: 10.1093/oxfordjournals.schbul.a033461. [DOI] [PubMed] [Google Scholar]
- Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr. Bull. 1982;8:470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. Peabody Picture Vocabulary Test. 3rd edition. Circle Pines, MN: American Guidance Service; 1997. [Google Scholar]
- Dworkin RH, Lewis JA, Cornblatt BA, Erlenmeyer-Kimling L. Social competence in adolescents at risk for schizophrenia. J. Nerv. Ment. Dis. 1994;182(2):103–108. doi: 10.1097/00005053-199402000-00007. [DOI] [PubMed] [Google Scholar]
- Eack SM, Mermon DE, Montrose DM, Miewald J, Gur RE, Gur RC, Sweeney JA, Keshavan MS. Social cognition deficits among individuals at familial high risk for schizophrenia. Schizophr. Bull. 2010;36(6):1081–1088. doi: 10.1093/schbul/sbp026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foussias G, Remington G. Negative symptoms in schizophrenia: avolition and Occam's razor. Schizophr. Bull. 2010;36(2):359–369. doi: 10.1093/schbul/sbn094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gard DE, Kring AM, Gard MG, Horan WP, Green MF. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr. Res. 2007;93:253–260. doi: 10.1016/j.schres.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson CM, Penn DL, Prinstein MJ, Perkins DO, Belger A. Social skill and social cognition in adolescents at genetic risk for psychosis. Schizophr. Res. 2010;122(1–3):179–184. doi: 10.1016/j.schres.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glatt SJ, Stone WS, Faraone SV, Seidman LJ, Tsuang MT. Psychopathology, personality traits, and social development of young first-degree relatives of patients with schizophrenia. Br. J. Psychiatry. 2006;189:337–345. doi: 10.1192/bjp.bp.105.016998. [DOI] [PubMed] [Google Scholar]
- Gresham FM, Elliot SN. Social Skills Rating System. New York: American Guidance Service, Inc.; 1990. [Google Scholar]
- Hans SL, Auerbach JG, Asarnow JR, Styr B, Marcus J. Social adjustment of adolescents at risk for schizophrenia: the Jerusalem Infant Development Study. J. Am. Acad. Child Adolesc. Psychiatry. 2000;39:1406–1414. doi: 10.1097/00004583-200011000-00015. [DOI] [PubMed] [Google Scholar]
- Hollingshead AA. Four-Factor Index of Social Status. New Haven, CT: Yale University; 1975. Unpublished manuscript. [Google Scholar]
- Kwapil TR. Social anhedonia as a predictor of the development of schizophrenia-spectrum disorders. J. Abnorm. Psychol. 1998;107:558–565. doi: 10.1037//0021-843x.107.4.558. [DOI] [PubMed] [Google Scholar]
- Niemi LT, Suvisaari JM, Tuulio-Henriksson AT, Lonnqvist JK. Childhood developmental abnormalities in schizophrenia: evidence from high-risk studies. Schizophr. Res. 2003;60:239–258. doi: 10.1016/s0920-9964(02)00234-7. [DOI] [PubMed] [Google Scholar]
- Schiffman J, Walker E, Ekstrom M, Schulsinger F, Sorensen H, Mednick S. Childhood videotaped social and neuromotor precursors of schizophrenia: a prospective investigation. Am. J. Psychiatry. 2004;161:2021–2027. doi: 10.1176/appi.ajp.161.11.2021. [DOI] [PubMed] [Google Scholar]
- Tarbox SI, Pogue-Geile MF. Development of social functioning in preschizophrenia children and adolescents: a systematic review. Psychol. Bull. 2008;134:561–583. doi: 10.1037/0033-2909.34.4.561. [DOI] [PubMed] [Google Scholar]
- Tsuji T, Kline E, Sorensen HJ, Mortensen EL, Michelesen NM, Ekstrom M, Mednick S, Schiffman J. Premorbid teacher-rated social functioning predicts adult schizophrenia-spectrum disorder: a high-risk prospective investigation. Schizophr. Res. 2013;151:270–273. doi: 10.1016/j.schres.2013.10.022. [DOI] [PubMed] [Google Scholar]