This study aims at systematically gathering leadership perspectives on the most pressing issues facing large, urban health departments and quantifying variation in policy involvement between Big Cities Health Coalition local health departments and other local health departments.
Keywords: Big Cities Health Coalition (BCHC), local health departments (LHDs), public health practice
Abstract
Context:
More than 2800 local health departments (LHDs) provide public health services to more than 300 million individuals in the United States. This study focuses on departments serving the most populous districts in the nation, including the members of the Big Cities Health Coalition (BCHC) in 2013.
Objective:
To systematically gather leadership perspectives on the most pressing issues facing large, urban health departments. In addition, to quantify variation in policy involvement between BCHC LHDs and other LHDs.
Design:
We used a parallel mixed-methods approach, including interviews with 45 leaders from the BCHC departments, together with secondary data analysis of the National Association of County & City Health Officials' (NACCHO) 2013 Profile data.
Participants:
Forty-five local health officials, chiefs of policy, and chief science/medical officers from 16 BCHC LHDs.
Results:
The BCHC departments are more actively involved in policy at the state and federal levels than are other LHDs. All BCHC members participated in at least 1 of the 5 policy areas that NACCHO tracks at the local level, 89% at the state level, and 74% at the federal level. Comparatively, overall 81% of all LHDs participated in any of the 5 areas at the local level, 57% at the state level, and 15% at the federal level. The BCHC leaders identified barriers they face in their work, including insufficient funding, political challenges, bureaucracy, lack of understanding of issues by key decision makers, and workforce competency.
Conclusions:
As more people in the United States are living in metropolitan areas, large, urban health departments are playing increasingly important roles in protecting and promoting public health. The BCHC LHDs are active in policy change to improve health, but are limited by insufficient funding, governmental bureaucracy, and workforce development challenges.
The United States faces a very different health landscape than it did a century ago. Where as the nation's public health system once focused on sanitation and infectious disease, public health today faces a new set of challenges dominated by chronic disease, but with tremendous breadth.1(p27) These challenges include, but are not limited to, opioid abuse,2,3 obesity,4 cancer prevention and control,5 climate-induced health risks,6 asthma,7 antimicrobial resistance,8 and reemerging infectious diseases.9 Despite spending far more on health care than our international peers, Americans die younger than people in almost all other industrialized nations.10,11
Health is shaped by biological and physiological processes, individual behaviors, and social determinants such as education and financial conditions.12 Prevention of many of today's major health problems require policy solutions that directly impact the root causes of illness and influence personal decision making. The nation's local health departments (LHDs) are a critical actor in this process. They can be innovators and advocates for health policy change because their authority, and focus, is at the local level.13,14 Policy innovations at the local level can drive national change. For example, LHDs were critical to the successful drafting and implementation of ordinances to restrict tobacco use in restaurants and bars in the early 2000s across the United States.15 Exposure to secondhand smoke declined by 83% among restaurant and bar employees.16 Today, 80% of all Americas live in jurisdictions with limits on smoking in restaurants and bars, protecting them from this unhealthy exposure.
The importance of LHDs is growing in the context of US Congressional stagnation and the increasing politicization of state legislatures.17–19 The extent of LHDs' role in the policy- making process warrants additional investigation. We used the 2013 National Association of County & City Health Officials (NACCHO) Profile to examine the influence of jurisdictional size and involvement in policy making. In addition, we interviewed leaders of public health departments who participate in NACCHO's Big Cities Health Coalition (BCHC)—a group of 20 LHDs that serves 46 million Americans20—to identify the factors that have facilitated and impeded their efforts to advance new public health policies. The BCHC is a forum for the leaders of America's largest metropolitan health departments to exchange strategies and best practices and jointly address issues to promote and protect most effectively the nation's health. The BCHC is made up of the LHDs of Atlanta, Baltimore, Boston, Chicago, Cleveland, Dallas, Denver, Detroit, Houston, Los Angeles, Miami, New York, Philadelphia, Phoenix, San Antonio, San Diego, San Francisco, San Jose, Seattle, and Washington, DC.
Methods
We used a parallel mixed-methods approach, with one track analyzing data from the NACCHO 2013 Profile to differentiate BCHC members from other LHDs with respect to policy involvement. We also conducted an interview phase of the study to systematically gather perspectives from leaders of the BCHC LHDs on related areas.
The NACCHO Profile collects data approximately biannually from 2800 LHDs. These condense to N = 2532 reporting units. In 2013, the NACCHO Profile had a response rate of 78%. Nineteen of 20 BCHC agencies responded to the NACCHO Profile survey. We divided the non-BCHC LHDs into 3 categories of population size (as opposed to geographic size) on the basis of NACCHO's previously published standards: small LHDs with a population less than 50 000 residents, medium-sized LHDs with 50 000 to 499 999 residents, and large LHDs with 500 000 or more residents. We report descriptive statistics comparing departments in terms of involvement in policy and advocacy.
The second stage of this study involved key informant interviews. We interviewed 45 leaders from 16 participating BCHC LHDs.* In each jurisdiction, we interviewed leaders in each of 3 positions: the local health official, the chief policy/senior deputy, and the chief science/medical officer. Three jurisdictions did not have chiefs of policy. The interviews were conducted between August and October 2013 by a single interviewer, with each interview lasting approximately 1 hour; all were recorded. Interviews were transcribed, verified, and coded independently by 2 researchers. Interview data were independently coded in batches by the researchers. Disagreements in coding were resolved, and interviews were recoded using consensus decisions.
Participants also took part in a brief Web-based survey along with the interview.21 In the interview, all participants answered all questions. In the Web survey, however, participants answered only organizationally oriented questions related to their position and job duties. The survey mostly included items regarding organizational characteristics and capacities previously used in other NACCHO studies, as well as questions on data capacity that were used in previous studies by the Association of State and Territorial Health Officials. Additional questions were tailored to BCHC LHD needs and capacities and were a focal point of pretesting. Both the interview and survey instruments were pretested with 5 former health officials. Quantitative data were managed and analyzed in Stata 13 (StataCorp LP, College Station, Texas). Qualitative data were managed and analyzed in nViVo 10 (QSR International, Cambridge, Massachusetts).
Results
Policy activity by jurisdictional size—results from the 2013 NACCHO Profile
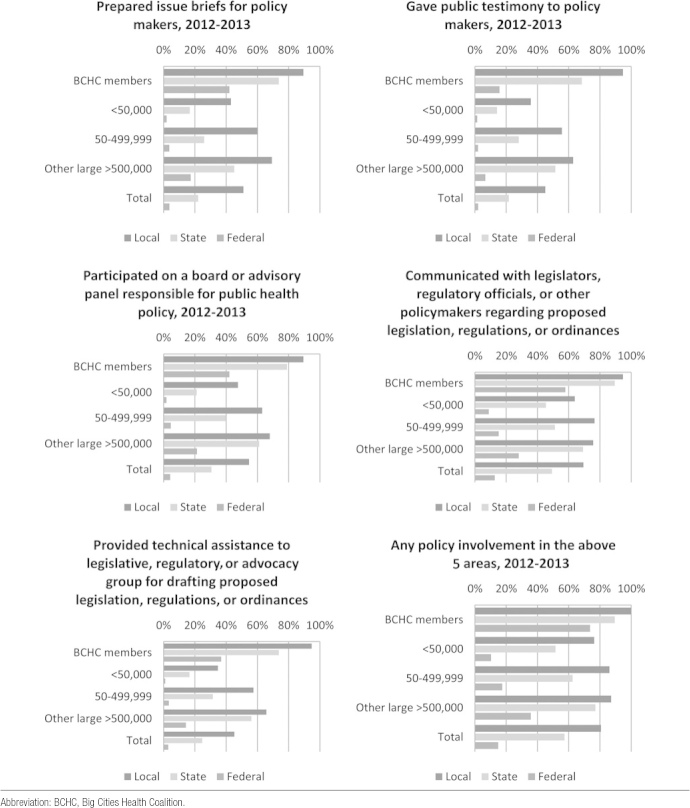
The NACCHO Profile asks about policy involvement in (1) writing issue briefs, (2) providing public testimony, (3) serving on advisory panels, (4) communicating with policymakers about specific policies, and (5) providing technical assistance to partners drafting public health policies—at the local, state, or federal level. There was a positive association between jurisdiction size and proportion performing each activity (Figure 1). There was a similar association for policy involvement at the local, state, and federal levels. Communicating with legislators, regulatory officials, or other policymakers was the most common activity across all groups. A greater proportion of BCHC member LHDs were active at the federal level than any other group. The proportion of BCHC member LHDs participating in these policy activities at the federal level was generally double that of other large LHDs. All BCHC members participated in at least 1 of these 5 areas at the local level compared with 81% of all LHDs. Approximately 74% of BCHC members participated in at least 1 area of policy involvement at the federal level, compared with 36% of other large LHDs and 15% of all LHDs (Figure 2).
FIGURE 1 •.
Local Health Department's Involvement in Policy-making Activities at the Local, State, and Federal Levels, by Jurisdiction Size, 2012-2013.
FIGURE 2 •.
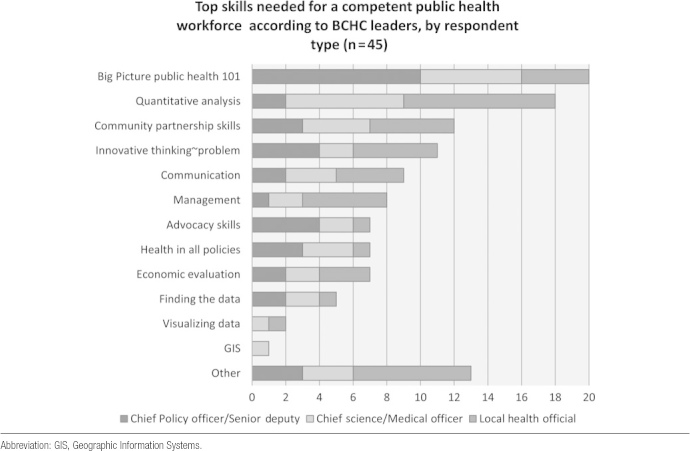
LHD Participation in Selected Chronic Disease Policy Areas.
Between 2011 and 2013, all BCHC members reported having been actively involved in policy or advocacy activities related to tobacco, alcohol, or other drugs, as well as obesity/chronic disease. More than two-thirds of BCHC members worked on smoke-free indoor air policy, smoke-free outdoor air policy, and reducing the sale of cigarettes to minors. About 30% worked on raising the cigarette tax and 47% on reducing advertising. No members reported working to alter alcohol taxes in their jurisdiction. In the area of obesity and chronic disease, more than three-quarters of BCHC members reported actively engaging in urban design policy, school physical activity policy, reducing unhealthy eating at schools, expanding recreational facilities, and increasing fruit/vegetable options in retail locations. Only 2 BCHC LHDs said that they worked on limiting access to fast food.
Ninety percent of BCHC members reported that a public health ordinance or regulation had been adopted in their jurisdiction in the past 2 years. Several jurisdictions passed multiple ordinances or regulations. Thirteen BCHC jurisdictions passed tobacco, alcohol, or other drug ordinances; 6 passed environmental health ordinances; 2 passed health care access-related ordinances; 3 passed occupational health-related ordinances; 6 passed obesity/chronic disease–related ordinances, 2 passed injury prevention ordinances, and 8 passed “other” ordinances. Sixty percent of other large LHDs, 44% of medium-sized LHDs, and 29% of smaller LHDs adopted a public health ordinance or regulation in the past 2 years.
Leadership perspectives from interview data
Demographics
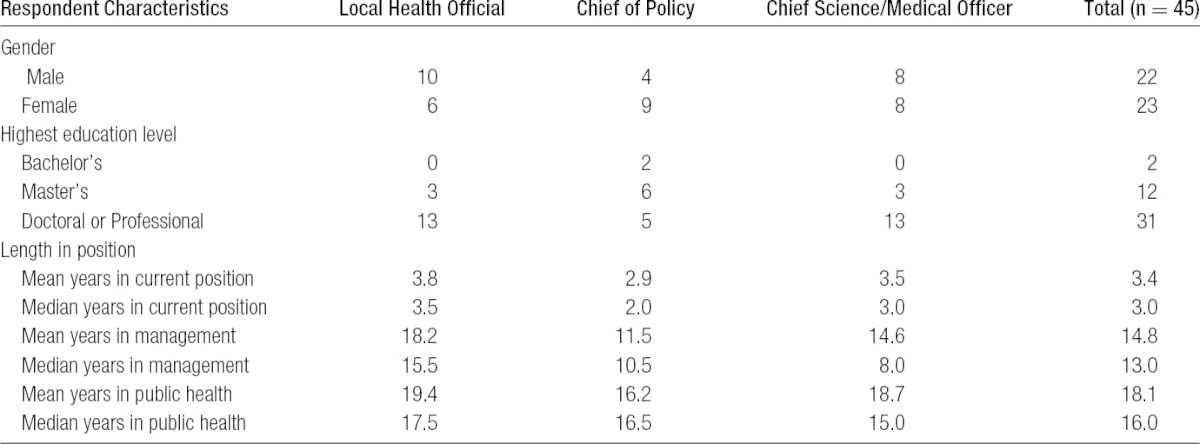
The 45 interview participants from the BCHC departments included 23 women and 22 men (Table 1). Thirty listed professional or doctoral degrees as their highest level of education. Participants indicated that they had worked in their current position 3.4 years on average (median 3 years), in management for 14.8 years on average, and had worked in public health for 18 years on average. Seven BCHC directors were appointed by a mayor, 1 by a board of health, 3 by a county executive, and 6 by some other arrangement (typically some combination of various state and local agencies).
TABLE 1 •. Demographic Characteristics.
Perceived needs and barriers in BCHC LHDs
We asked BCHC leaders about perceived needs of large, urban health departments. The majority thought that the biggest barrier faced by health departments was the lack of funding for public health activities, especially those considered to be core public health and infrastructure. Information management needs were also commonly mentioned. Overall, BCHC leaders identified 3 key policy areas as priorities over the coming years: core funding for public health activities, “health in all policies” (where the effects of, for example, transportation, housing, or education policies on health are taken into account and public health is at the table), and LHDs participation in the implementation of the Affordable Care Act (ACA). Participants commonly cited political barriers, including ideological stances on where to assign blame for poor health outcomes, as well as outdated laws (Table 2). As one participant noted:
TABLE 2 •. Greatest Barriers to Local Health Department Improving Population Health.
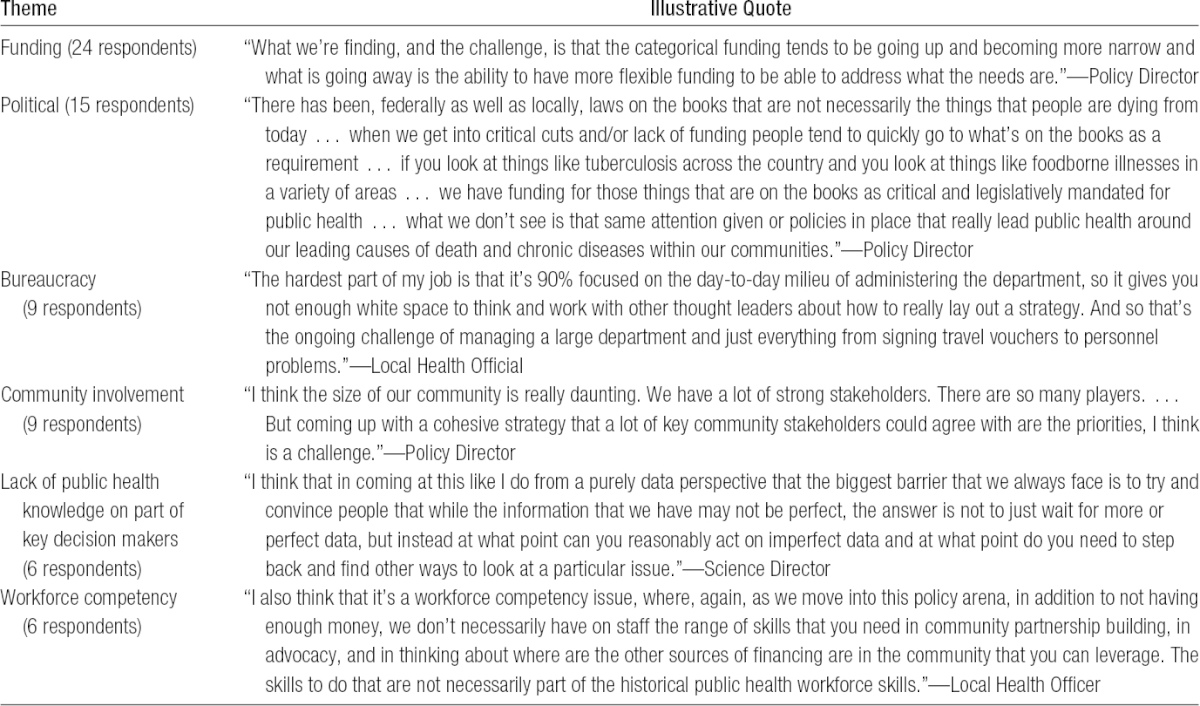
Among the decision-makers and also to a large extent among the electorate, the attitude is that there is not a role for government to undertake steps that are communal in nature to benefit all. There is an underlying culture that people should be responsible for themselves and that if you made a bad health decision in some way, that's your own fault.... As opposed to recognizing that it's not about blame; it's about where do we know that we can make interventions that will lead to fewer people making bad choices.
Similarly, participants explained that it was sometimes difficult to convince decision makers of how to proceed with public health policy and programming because of their lack of understanding of public health or of how to interpret data. Local bureaucracy was considered to be a major barrier by several participants, who explained that the governmental systems in place in their particular jurisdictions made it nearly impossible to hire appropriate staff, execute purchase orders, or accept grants in a timely fashion. Some interviewees noted the difficulty in engaging diverse community stakeholders to formulate comprehensive and unified strategies, indicating that a lack of resources and many different community agendas made it difficult to facilitate collaboration.
Workforce Needs
Participants uniformly reported that workforce needs are substantial in BCHC LHDs. These needs relate to workforce development in terms of continuing education and the acquisition of new skills, as well as the ability to hire the right people for the job. Participants reported that their departments lacked employees with the skills required to carry out the full range of activities critical to public health services, especially advocating for policy change and engaging the community. From their perspectives, these problems are exacerbated by complex and restrictive hiring practices as well as low employee mobility.
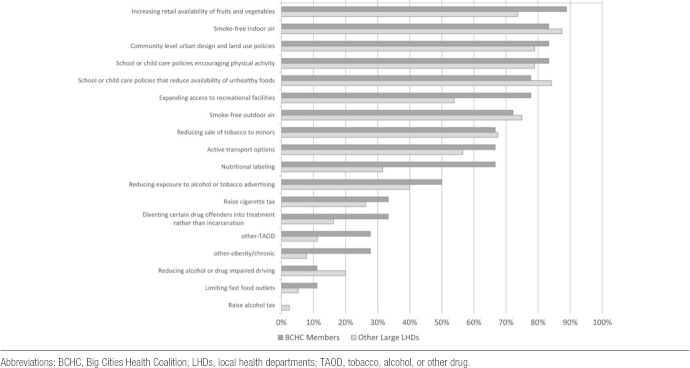
The BCHC leaders were asked specifically about the most important types of skills their staff needed to be effective (Figure 3). The most commonly-cited skills needed by staff were “big picture” or “public health 101” training. Systems thinking constituted abilities were needed to interconnect departmental programs, as well as to understand how the health department fits within the broader city environment. Skills in quantitative analysis were also mentioned as being necessary. Finally, many said that it was difficult to hire staff in a timely way. One participant illustrated her point with the following response when talking about running into challenges while trying to hire for policy-oriented positions:
FIGURE 3 •.
Top Skills.
There just isn't a policy position [in the HR system]. And we do have things like a Research Assistant III or an Epidemiologist II but we don't have this kind of position carved out and recognized. So for example I had a really hard time hiring a health economist. We had to go through a third party contractor to hire them because we had no items that he could fit on. There's no such thing as a health economist before. And yet we're trying to do more of this kind of work, like health impact assessments. So that is a really big challenge.
Programmatic Budget Cuts
The majority of BCHC departments had approximately the same budget in 2013 as 2012 in nominal dollars; 4 had budget cuts greater than 10%. Although many BCHC LHDs had relatively small changes to total expenditures between fiscal year 2012 and fiscal year 2013, programmatic budget changes did occur. The BCHC policy chiefs (1 per LHD) were asked to quantify any changes in programmatic areas over the previous fiscal year. Most participants reported some fluctuation in their programmatic budgets, with more cuts reported than growth. Those with budget growth had it in areas such as immunization (1 LHD), communicable disease control (1 LHD), chronic disease (3 LHDs), maternal and child health (2 LHDs), other personal health services (2 LHDs), population-based primary prevention (2 LHDs), and in other environmental health programs (1 LHD). More commonly, BCHC LHDs reported cuts, especially in immunizations, epidemiology, and population-based prevention services (Figure 4).
FIGURE 4 •.
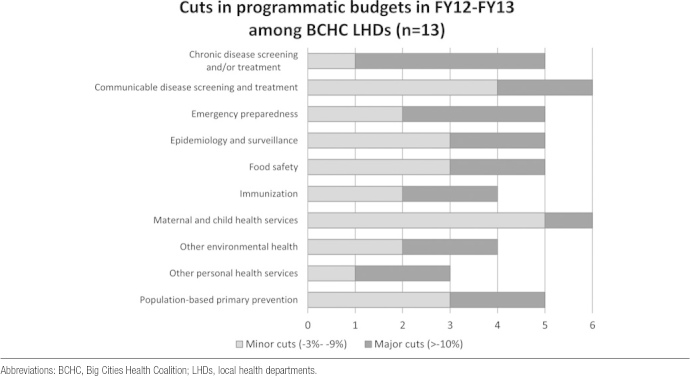
Cuts in Programmatic Budgets Between Fiscal Year 2012 and Fiscal Year 2013.
Discretion to Reallocate Dollars
One policy chief per department was asked to indicate the level of control associated with various revenue streams, including local revenue, state direct, federal pass-through dollars, federal direct sources, Medicare and Medicaid, other clinical revenue, and all other sources. With the exception of local sources, the majority of participants indicated that they had no or only a small amount of control. Six of 13 policy chiefs said that they felt that they had a great deal of control for local sources of revenue, while 3 others felt that they had moderate control. Nine participants indicated that they felt that they had no discretion to reallocate dollars from federal direct or pass-through funds. Three said that they felt that they had no control over state sources; 6 said that they felt that they had a small amount of control over state sources.
Discussion
Public health policy has the potential to impact large portions of a population and contribute to an environment in which the healthy option is the default option. This is especially the case in metropolitan areas, which are now home to almost 83% of Americans.22 With the United States facing important health challenges in the 21st century—from obesity rates to opioid abuse—large urban jurisdictions and their public health systems are serving as key hubs for the greatest returns on health investments.
Increasingly, over the past decade, big city and large metro governments have become incubators of policy innovation and strong executive leadership.23 In the field of public health, local leadership is critical, particularly during a time of federal paralysis. Cities are better positioned to respond quickly to emerging threats than the slow-moving federal bureaucracy and are able to take strong stances on governance and local issues when partisan gridlock stalls federal efforts. Mayors across the country have taken risky stands on health issues from tobacco control to childhood obesity.24–27
The BCHC member LHDs have been the most active in policymaking among all LHDs nationally. All but 1 BCHC jurisdiction passed at least 1 public health ordinance in the past between 2011 and 2013, with all working on policy on 2 key fronts: tobacco, alcohol, and other drugs; and obesity and other chronic diseases. National leadership on new strategies and health challenges has arisen from urban jurisdictions. For example, Los Angeles County Department of Public Health drove the development of public letter grading for restaurants, which resulted in improved hygiene, reduced restaurant inspection violations, and a lower incidence of foodborne illness.28 In addition, Seattle-King County was one of the first to regulate electronic cigarettes as tobacco products with the aim to decrease adolescent nicotine addiction.29 Finally, New York City instituted a wide scope of new policies, such as restaurant calorie postings, school and vending machine food standards, and bonus food stamp coupons for fruits and vegetables.30,31
Thomas Frieden, former commissioner of the New York City Department of Health and Mental Hygiene and current director of the Centers for Disease Control and Prevention, noted a decade ago that many public health agencies had failed to implement effective policies and programs to prevent current health problems, in part due to structural inadequacies and insufficient funding.30 While large metropolitan health departments have advanced important policy initiatives in the past decade, the results of the current study confirm the challenges remaining that prevent LHDs from achieving optimal impact on improving the population's health.
Insufficient funding is the most frequently identified barrier to LHD impact improving the population's health. Big city spending per capita varies tremendously, which is partially attributable to local support but largely due to variable levels of federal funds reaching urban centers, because state health agencies are allocating those federal dollars differently. Greater transparency is needed to track this variable distribution and its impacts on effective investments in public health. The barriers are not merely having too little money, but that the fiscal environment hampers departments' potential impact in policymaking process because of restricted fiscal flexibility and discretion, inadequate workforce skills, and limited policymaker knowledge.
Data from the 2013 NACCHO Profile identified opportunities for greater involvement for LHDs in the policymaking process. Policy development should be a priority among LHDs individually and in NACCHO collectively.32,33 A key message of the Institute of Medicine's recent report is for government agencies to familiarize themselves with the toolbox of public health legal and policy interventions at their disposal.1(p27)
The BCHC member LHDs were active at the local, state, and federal levels for all policy activities queried, but this was not the case for other large LHDs or LHDs with small or medium-sized jurisdictions. It may be that federal-level policy involvement from all LHDs is an unrealistic expectation except for the largest LHDs. However, some policy activity at the local level, regardless of jurisdictional size, should be universal. Policy development is a core function of public health practice and has been instantiated as such in the Ten Essential Services34 and, more recently, both as part of the Foundational Public Health Services model35 and the health department accreditation process by the Public Health Accreditation Board.36
Gaps in funding, lack of political support, and needs for strengthening professional staff are not new challenges in the management of public health departments. For the past 20 years, there has been a steady drumbeat of calls for sustained and strategic funding streams that would allow governmental public health to respond to emerging health threats, build capacity to address and prevent chronic conditions, and institute policies to improve conditions for healthy living. These needs persist. With their dense populations, strong leadership, and demonstrated commitment to engage in public health policy innovations, large metropolitan centers must become a greater priority at the federal and state levels for achieving improved returns on health investments.
Limitations
This study had several limitations. It is a cross-sectional study and focuses primarily on the members of the BCHC. Data from the 2013 NACCHO Profile are widely used but do have limitations. These include potential issues due to nonresponse bias, though a 78% response rate is relatively robust for surveys of this type.1(p27) In addition, the data are self-reported. Qualitative results should be interpreted within the context of the large, urban health departments that constitute the BCHC.
Conclusion
The need and opportunity exist to increase all LHDs' policy activities. The BCHC members have become incubators of policy innovation and strong executive leadership. However, even those departments in the BCHC have been hindered from making further gains in prevention and public health by continued inadequate funding and constraints in targeting resources to address local priorities. Leaders from BCHC member LHDs need to engage leaders in other large LHDs and medium-sized LHDs to increase their policy involvement at the local and state levels to create stronger support for public health investments. Public health leaders need greater political and financial support to make concrete progress on the most winnable health battles.
At the time of the interview portion of this study, 18 LHDs constituted the BCHC. Two additional LHDs have since joined: those serving San Antonio, Texas, and San Diego, California.
The authors declare no conflicts of interest.
REFERENCES
- 1.Institute of Medicine. For the Public's Health: Investing in a Healthier Future. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 2.Paulozzi LJ. Opioid analgesic involvement in drug abuse deaths in American metropolitan areas. Am J Public Health. 2006;96:1755–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paulozzi LJ, Budnitz DS, Yongli X. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15:618–627. [DOI] [PubMed] [Google Scholar]
- 4.Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The spread of the obesity epidemic in the United States, 1991-1998. JAMA. 1999;282(16):1519–1522. [DOI] [PubMed] [Google Scholar]
- 5.American Cancer Society. Cancer Facts & Figures 2014. Atlanta, GA: American Cancer Society; 2014. [Google Scholar]
- 6.Luber G, Hess J. Climate change and human health in the United States. J Env Health. 2007;70(5):43–44. [PubMed] [Google Scholar]
- 7.Bousquet J, Bousquet PJ, Godard P, Daures JP. The public health implications of asthma. Bull World Health Organ. 2005;83(7):548–554. [PMC free article] [PubMed] [Google Scholar]
- 8.Diekema DJ, BootsMiller BJ, Vaughn TE, et al. Antimicrobial resistance trends and outbreak frequency in United States hospitals. Clin Infect Dis. 2004;38(1):78–85. [DOI] [PubMed] [Google Scholar]
- 9.Fauci AS, Morens DM. The perpetual challenge of infectious diseases. N Engl J Med 2012;366:454–461. 10.1056/nejmra1108296. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Death and Mortality. NCHS FastStats Web site; http://www.cdc.gov/nchs/fastats/deaths.htm Accessed December 20, 2013. [Google Scholar]
- 11.Institute of Medicine. U.S. Health in International Perspective: Shorter Lives, Poorer Health, Report Brief. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 12.Adler NE. Reaching for a Healthier Life: Facts on Socioeconomic Status and Health in the US. Chicago, IL: The John D. and Catherine T. MacArthur Foundation Research Network on Socioeconomic Status an Health; 2007. [Google Scholar]
- 13.Koplin A. The future of public health: a local health department view. J Public Health Policy. Winter 1990;11(4): 420–437 Palgrave Macmillan JournalsStable Web site. http://www.jstor.org/stable/3342922. Accessed August 5, 2014. [PubMed] [Google Scholar]
- 14.Pomeranz JL. The unique authority of state and local health departments to address obesity. Am J Public Health. 2011;101(7):1192–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gostin LO. Bloomberg's Health Legacy: urban innovator or meddling nanny? Hastings Center Rep. 2013;43(5):19–25 SSRN Web site. http://ssrn.com/abstract=2334823. [DOI] [PubMed] [Google Scholar]
- 16.American Cancer Society. “The effects of secondhand smoke on worker health.” http://acction.acscan.org/site/Doc-Server/Effects-Secondhand-Smoke.pdf Published 2008.
- 17.Shor B, McCarty N. The ideological mapping of American legislatures. Am Pol Sci Rev. 2011;105(3):530–551. [Google Scholar]
- 18.Diller PA. Why do cities innovate in public health? implications of scale and structure. Wash Univ Law Rev. 2014;91(5):1–75. [Google Scholar]
- 19.Kleiman N, Forman A, Ko J, Giles D, Bowles J. Innovation and the city center for urban future. http://wagner.nyu.edu/files/labs/Innovation-and-the-City.pdf Published 2013.
- 20.Leider JP, Castrucci BCC, Hearne S, Russo P. Organizational characteristics of large urban health departments. J Public Health Manag Pract. 2015;21(1):S14–S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications, Inc; 2007. [Google Scholar]
- 22.United Nations Department of Economic and Social Affairs. World urbanization prospects: the 2011 revision: file 1: population of urban and rural areas and percentage urban, 2011 [table]. http://esa.un.org/unup/CD-ROM/Urban-Rural-Population.htm Published 2012.
- 23.Katz B, Bradley J. The Metropolitan Revolution: How Cities and Metros are Fixing Our Broken Politics and Fragile Economy. Washington, DC: Brookings Institution Press; 2013. [Google Scholar]
- 24.Grinbaum M. Judge blocks New York City's limits on big sugary drinks. The New York Times; March 11, 2013. http://www.nytimes.com/2013/03/12/nyregion/judge-invalidates-bloombergs-soda-ban.html. [Google Scholar]
- 25.Nutter M. Keynote remarks. National Soda Summit. http://cityofphiladelphia.wordpress.com/2012/06/07/mayor-nutters-soda-summit-address/ Published June 7, 2013.
- 26.Balde L. Rahm Cracks Down on Chicago Vending Machines. NBC Chicago; http://www.nbcchicago.com/blogs/ward-room/Rahm-Cracks-Down-on-Chicago-Vending-Machines-179282661.html Published November 15, 2012. [Google Scholar]
- 27.Lazar K. Merino long championed public health. The Boston Globe. March 29, 2013. http://www.bostonglobe.com/metro/massachusetts/2013/03/28/mayor-menino-has-long-championed-public-health/7t9mGv3WBhoY1tN1hXasTM/story.html.
- 28.Simon PA, Leslie P, Run G, et al. Impact of restaurant hygiene grade cards on foodborne-disease hospitalizations in Los Angeles county. J Environ Health. 2005;67(7):32–36. [PubMed] [Google Scholar]
- 29.Gilroy J. Electronic cigarette regulations in King County. Wash State J Publ Health Pract. 2012;4(suppl 1), 15. [Google Scholar]
- 30.Frieden T, Bassett M, Thorpe L, Farley T. Public health in New York City, 2002-2007: confronting epidemics of the modern era [published online ahead of print June 7, 2008]. Int J Epidemiol. 2008. 37(5):966–977 http://www.pubfacts.com/author/Thomas+A+Farley. [DOI] [PubMed] [Google Scholar]
- 31.Alcorn T. Redefining public health in New York City. Lancet. 2012;379(9831):2037–2038. [DOI] [PubMed] [Google Scholar]
- 32.Beitsch LM, Brooks RG, Menachemi N, Libbey PM. Public health at center stage: New roles, old props. Health Aff (Millwood). 2006;25(4):911–922. 25/4/911 [pii] 10.1377/hlthaff.25.4.911. [DOI] [PubMed] [Google Scholar]
- 33.Harris JK, Mueller NL. Policy activity and policy adoption in rural, suburban, and urban local health departments. J Public Health Manag Pract. 2013;19(2):E1–E8. 10.1097/PHH.0b013e318252ee8c. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Ten essential services of public health. http://www.cdc.gov/nphpsp/essentialServices.html.
- 35.Public Health Leadership Forum. Defining and constituting foundational “Capabilities” and “Areas” version 1. 2014.
- 36.Riley WJ, Bender K, Lownik E. Public health department accreditation implementation: Transforming public health department performance. Am J Public Health. 2012;102(2):237–242. [DOI] [PMC free article] [PubMed] [Google Scholar]