Abstract
Objective:
To examine the relationship between health conditions and the risk for membership in longitudinal trajectories of productivity loss.
Methods:
Trajectories of productivity loss from the ages of 25 to 44 years, previously identified in the National Longitudinal Survey of Youth (NLSY79), were combined with information on health conditions from the age 40 years health module in the NLSY79. Multinomial logistic regression was used to examine the relative risk of being in the low-risk, early-onset increasing risk, late-onset increasing risk, or high-risk trajectories compared with the no-risk trajectory for having various health conditions.
Results:
The trajectories with the greatest probability of productivity loss longitudinally had a greater prevalence of the individual health conditions and a greater total number of health conditions experienced.
Conclusions:
Health conditions are associated with specific longitudinal patterns of experiencing productivity loss.
Learning Objectives
Become familiar with the five distinct trajectories of health-related productivity loss, previously reported by Besen and Pransky.
Summarize the new findings on individual health conditions and numbers of health conditions associated with different productivity loss trajectories.
Discuss the potential implications for developing interventions to reduce the number of workers on trajectories of frequent and recurrent productivity loss.
Productivity loss at work as a result of health problems, including physical and mental health problems, is a major concern for employers.1–3 Productivity loss generally refers to sickness absence from work while employed, often termed absenteeism, reductions in productivity while at work due to health, often termed presenteeism, and withdrawal from the workforce completely as a result of health.4,5 Productivity loss is estimated to cost employers billions of dollars each year.6–10
Several studies have examined productivity loss in relation to specific chronic physical and mental health conditions. In a study of Australian workers, Holden and colleagues11 found an increased risk for absenteeism among those with drug and alcohol problems, psychological problems, cancers, and arthritis. Similarly, an increased risk for presenteeism was found among those with drug and alcohol problems, fatigue, and obesity.11 Another study of German workers found that the greatest number of days with productivity loss was due to arthritis and psychological problems.12 In the United States, the highest risk for absenteeism was associated with having diabetes, whereas presenteeism was associated with stress.13 The total cost burden per year per employee is estimated to be highest for hypertension at $392, followed by psychological problems at $348 and arthritis at $327.1 In all of these studies, mental health conditions seemed to be common conditions related to productivity loss. In particular, depression is a highly prevalent mental health condition, which is associated with various types of productivity loss including decreases in work performance, increases in absenteeism, increases in presenteeism, and greater unemployment.14–18 In fact, it is estimated that in the United States, depression results in $44 billion annually in lost productivity costs.19
Although previous research has examined the association between chronic health conditions and productivity loss on a cross-sectional basis, there has been little longitudinal investigation of how productivity loss develops across one's working career and how different chronic health conditions relate to differences in the patterns of these temporal changes. It is unclear if workers with certain chronic health conditions experience productivity loss only infrequently, or if certain chronic health conditions are related to long-term patterns of experiencing productivity loss that develop over time. Analyses of productivity loss on a one-time basis associated with chronic health conditions do not take into account the full impact of chronic health conditions on the lifetime prevalence of productivity loss and the true cost of productivity loss to employers.
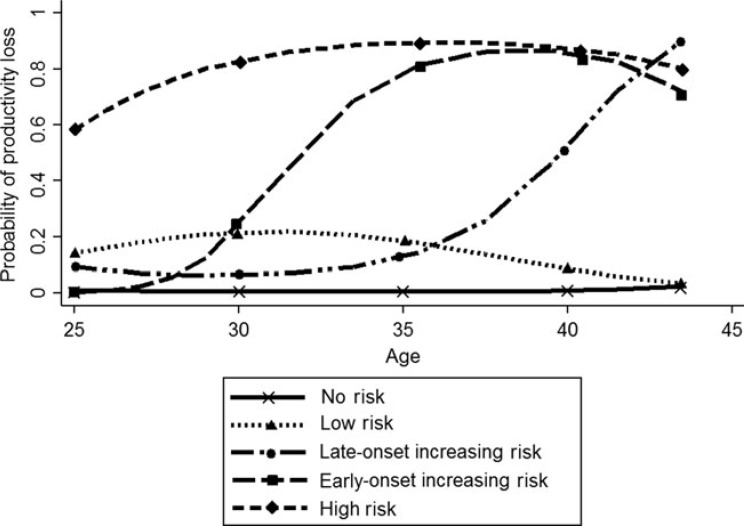
Besen and Pransky, in a study of adults aged 25 to 44 years, previously found five distinct trajectories of health-related productivity loss that were related to differences in employment status at the age of 45 years.20 In this previous study, health-related productivity loss was defined as being unable to work as a result of health or being limited in the amount or kind of work a person could do as a result of health. No specific health condition information was provided on the reasons for productivity loss. Productivity loss was assessed at 12 different waves (from ages 25 to 44 years) and participants had to have been employed in at least 1 of the 12 waves to be included in the trajectory model. These trajectories were then compared to employment status at the age of 45 years, using the first wave after the 12 waves used for the trajectory model (this wave was not used in the trajectory model), which was defined as working at least 10 weeks in the previous year. Figure 1 illustrates the temporal patterns for each of the trajectory groups in the probability of productivity loss from ages 25 to 44 years. Both no-risk trajectory and the low-risk trajectory were associated with a relatively low probability of having productivity loss at any age and, in both groups, more than 90% of respondents were employed at the age of 45 years. In contrast, in the other three trajectory groups, only about half of respondents were employed at the age of 45 years. The first of these groups, the high-risk trajectory, had a consistently high probability of productivity loss across the age span. The early-onset increasing risk trajectory had an increasing probability of productivity loss beginning around the age of 30 years, whereas the late-onset increasing risk trajectory had an increasing probability of productivity loss that did not begin until around the age of 35 years.
FIGURE 1.
Trajectories of the probability of productivity loss across ages 25 to 44 years. Reproduced with permission from Besen and Pransky.20
In the previous study examining longitudinal patterns of productivity loss, the authors did not focus on whether the trajectory groups differed in the types or number of chronic health conditions. Building on the previous work by Besen and Pransky, the goal of this study was to explore these differences.20 Specifically, we examine the relative risk of being in the low-risk trajectory, the high-risk trajectory, the early-onset increasing risk trajectory, or the late-onset increasing risk trajectory in comparison with the no-risk trajectory based on whether respondents reported having chronic health conditions at the age of 40 years. In addition, we assess differences among the trajectories of productivity loss based on the number of chronic health conditions reported.
METHODS
Study Population
This study utilized data from the National Longitudinal Survey of Youth (NLSY79). The NLSY79 is an ongoing, nationally representative, longitudinal study of 12,686 Americans aged 14 to 22 years in 1979, representing a cohort born between 1957 and 1964.21 The study is sponsored by the Bureau of Labor Statistics. Participants have been reinterviewed annually from 1980 to 1994, and then every other year from 1996 to the present. Data are publically available up to 2010 when participants were aged 45 to 53 years. Retention rates are relatively high with approximately 60% of the original 1979 sample still participating as of 2010. There were several reasons for attrition in this sample, including death (approximately 6% of the sample), portions of participants from the military and supplemental sample were deemed ineligible because of funding cutbacks (approximately 22% of the sample), and standard longitudinal attrition factors such as participants refusing to be interviewed and inability to locate participants (approximately 12% of the sample). More information on the sample attrition can be found at https://www.nlsinfo.org/content/cohorts/nlsy79/intro-to-the-sample/retention-reasons-noninterview. In 1979, roughly half of the sample was male, 59% were nonblack, non-Hispanic, 25% were black, and 16% were Hispanic/Latino. In 2010, 48% of the sample consisted of males, 50% were nonblack, non-Hispanic, 31% were black, and 19% were Hispanic/Latino. Proportional weights in each survey year are available to adjust the sample to its original sampling frame. The NLSY79 is primarily focused on labor force activities; however, it also gathers information about demographic characteristics, income and assets, education, and work limitations.
In this study, we build upon previously published findings of trajectories of productivity loss. As such, we are using the same subsample of the NLSY79 that was used in the original study identifying the trajectories of productivity loss. Specifically, the productivity loss trajectories were based on 12 waves of NLSY79 data, which were collected annually from ages 25 to 29 years (waves 1 through 5) and biennially from ages 30 to 44 years (waves 6 through 12). A subsample of 5699 participants was used who had valid data about productivity loss for at least 6 waves from the ages of 25 to 44 years, and who participated in the interviews for waves 1 and 12. Of the initial 12,686 participants in 1979, 6987 were excluded from the sample used in the trajectory model for not having valid data on productivity loss in at least six waves or for not participating in the first and last wave. Additional information about the trajectory model subsample is presented in the study by [Authors Names Omitted].20
Of the 5699 participants from the sample for the productivity loss trajectories, we further restrict the sample in this study to 5583 participants with valid data from the 40 and over health module in the NLSY79. The 40 and over health module asked participants questions about depression, health care utilization, chronic health conditions, and general health. Participants were asked the questions in this module in the first wave in which they participated once reaching the age of 40 years. This was primarily when the participants were aged 40 or 41 years, but in some cases, the module was asked slightly later. All participants in our sample completed the module by the age of 45 years. The 116 cases excluded because of missing health information did not differ with respect to membership in the different productivity loss trajectories.
Measures
Longitudinal Health-Related Productivity Loss Trajectories
The outcome variable in this study is a categorical variable indicating membership in one of several health-related productivity loss trajectories. The user-written program “traj” for STATA was used to estimate the trajectories.22 This program is used for implementing latent class growth analysis, a type of growth mixture modeling,23 which is able to identify distinct subgroups of individuals who follow similar developmental trajectories in a larger sample. The logit option was used to plot the probability of productivity loss across the age range in our sample. Each trajectory represents a different temporal pattern of the probability of having productivity loss from the age of 25 years to 44 years. Within each wave of the survey, participants were coded as having experienced productivity loss if they responded yes to at least one of the following questions: (1) “Would your health keep you from working on a job for pay now?” (2) “Are you/Would you be limited in the kind of work you (could) do on a job for pay because of your health?” and (3) “Are you/Would you be limited in the amount of work you (could) do because of your health?” Based on a trajectory model for 12 waves of responses about experiencing productivity loss, we will be using the five trajectories previously identified by [Authors Names Omitted].20 The five distinct trajectories that were identified (shown in Figure 1) are a no risk of productivity loss trajectory, a low risk of productivity loss trajectory, a late-onset increasing risk of productivity loss trajectory, an early-onset increasing risk of productivity loss trajectory, and a high risk of productivity loss trajectory. The percentage of the sample in each of the trajectories as well as basic demographics for each trajectory can be found in Table 1.
TABLE 1. Percentage of Participants by Trajectory (N = 5583).
| No Risk | Low Risk | Late Onset Increasing Risk (Late Onset) | Early Onset Increasing Risk (Early Onset) | High Risk | |
|---|---|---|---|---|---|
| N | 4211 | 641 | 306 | 207 | 218 |
| % of total sample | 75.4 | 11.5 | 5.5 | 3.7 | 3.9 |
| % Female | 43.4 | 70.6 | 47.3 | 46.4 | 66.8 |
| % White/non-Hispanic | 55.5 | 46.7 | 49.2 | 48.4 | 46.0 |
| % Employed 10+ hours/week at the age of 45 yrs | 95.2 | 90.6 | 48.5 | 50.5 | 46.6 |
| Years of education | 13.7 | 13.1 | 12.4 | 12.5 | 12.4 |
Chronic Health Conditions
In the age 40 and over health module, participants were asked whether they had any of several different chronic conditions. Twenty-eight different conditions, listed in Table 2, were included in the analyses. For the first seven conditions listed in table 2, participants were asked, “Have you ever had, or has a doctor ever told you that you have... [name of condition].” For the remaining conditions listed in Table 2, participants were asked, “Do you have any of the following health problems?” Respondents answered yes if they had the condition or no if they did not. This list of chronic conditions is not part of a standardized measure. The questions were created for use in the NLSY79. In addition to these chronic health conditions, we included two additional measures of health problems: obesity and depression. For obesity, we calculated body mass index (BMI) as reported weight in pounds divided by the square of height and then multiplied by a conversion factor of 703. Height was reported in 1985 when participants were aged 20 to 28 years. Weight was reported in the same wave in which participants completed the age 40 health module. Body mass index was bottom-coded at 14 and top-coded at 50. There were three participants with a BMI less than 14 and 28 participants with a BMI greater than 50. In addition to the continuous BMI variable, we created an obesity variable on the basis of BMI of 35 or higher. Finally, we included a continuous measure of depression based on a shortened version of the Center for Epidemiological Studies Depression Scale administered in the age 40 health module.24 The shortened measure included seven items from the original scale (α = 0.83). Respondents were asked how often in the past week they had loss of appetite, had trouble keeping their mind on tasks, felt depressed, felt that everything took effort, had restless sleep, felt sad, and could not get going. Response options were 0 (“rarely/none of the time/1 day”), 1 (“some/a little of the time/1 to 2 days”), 2 (“occasionally/moderate amount of the time/3 to 4 days”), and 3 (“most/all of the time/5 to 7 days”). Scores ranged from 0 to 21, with higher scores indicating greater depression.
TABLE 2. Chronic Health Conditions by Productivity Loss Trajectory.
| % of Respondents With Condition by Trajectory | |||||||
|---|---|---|---|---|---|---|---|
| No Risk | Low Risk | Late Onset | Early Onset | High Risk | Total Sample | ||
| Full name of condition | Short label | N = 4211 | N = 641 | N = 306 | N = 207 | N = 218 | N = 5583 |
| High blood pressure or hypertension | Hypertension | 15.36% | 17.77% | 25.95% | 24.41% | 31.56% | 17.21% |
| Diabetes or high blood sugar | Diabetes | 4.08% | 6.34% | 10.76% | 12.21% | 13.39% | 5.39% |
| Cancer or malignant tumor of any kind except skin cancer | Cancer | 1.50% | 2.16% | 6.01% | 4.69% | 6.67% | 2.15% |
| Chronic lung disease such as chronic bronchitis or emphysema | Lung disease | 1.78% | 2.94% | 6.01% | 9.86% | 12.00% | 2.86% |
| Heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems | Heart problems | 1.83% | 2.94% | 6.33% | 9.86% | 11.56% | 2.89% |
| Emotional, nervous, or psychiatric problems | Emotional problems | 3.80% | 7.11% | 21.20% | 24.88% | 27.56% | 6.88% |
| Arthritis or rheumatism | Arthritis | 7.70% | 14.84% | 26.50% | 38.03% | 35.11% | 11.79% |
| Asthma (shortness of breath or chronic cough) | Asthma | 5.40% | 8.39% | 12.97% | 18.87% | 24.11% | 7.41% |
| Problems with your back | Back problems | 19.21% | 27.36% | 45.74% | 55.19% | 53.33% | 24.33% |
| Problems with your feet and legs | Leg problems | 13.87% | 24.30% | 45.43% | 49.30% | 56.00% | 19.83% |
| Kidney or bladder problems | Kidney problems | 2.82% | 4.49% | 10.09% | 15.96% | 12.44% | 4.29% |
| Stomach or intestinal ulcers | GI ulcers | 3.50% | 6.50% | 11.08% | 12.26% | 19.28% | 5.22% |
| High cholesterol | Cholesterol | 10.89% | 9.78% | 13.83% | 17.62% | 19.73% | 11.53% |
| Pain or pressure in your chest, palpitation or pounding heart, or heart trouble | Chest pain | 3.64% | 5.89% | 13.29% | 14.55% | 20.89% | 5.53% |
| Low blood pressure | Low BP | 3.98% | 6.07% | 8.54% | 9.86% | 12.44% | 5.03% |
| Chronic or frequent colds, sinus problems, hay fever or allergies | Allergies | 22.19% | 26.51% | 31.33% | 36.15% | 39.56% | 24.41% |
| Frequent indigestion, stomach, liver or intestinal trouble, gall bladder trouble or gallstones | Indigestion | 6.95% | 9.44% | 18.93% | 15.96% | 24.89% | 8.96% |
| Depression or excessive worry or nervous trouble of any kind | Mood problems | 8.29% | 13.98% | 29.97% | 38.97% | 36.77% | 12.43% |
| Swollen or painful joints, frequent cramps in your legs or bursitis (nonarthritis/rheumatism) | Painful joints | 9.77% | 17.83% | 35.02% | 37.09% | 44.00% | 14.49% |
| Frequent or severe headaches, dizziness, or fainting spells | Headaches | 6.76% | 13.78% | 22.71% | 30.05% | 30.36% | 10.27% |
| Eye trouble, other than glasses or contacts | Eye problems | 2.75% | 6.04% | 12.93% | 15.09% | 19.56% | 4.82% |
| Ear, nose, or throat trouble | ENT problems | 4.39% | 6.20% | 13.25% | 15.49% | 16.96% | 6.01% |
| Severe tooth or gum trouble | Tooth problems | 4.32% | 6.66% | 10.41% | 11.27% | 16.44% | 5.67% |
| Skin diseases | Skin disease | 2.11% | 2.32% | 5.06% | 5.16% | 5.78% | 2.56% |
| Thyroid trouble or goiter | Thyroid problems | 3.05% | 5.11% | 2.53% | 4.72% | 10.27% | 3.61% |
| Frequent trouble sleeping | Sleep problems | 10.69% | 16.56% | 35.33% | 50.70% | 44.00% | 15.57% |
| Frequent urinary tract infections | UTI | 1.27% | 2.63% | 4.10% | 5.16% | 7.11% | 1.96% |
| Ulcer | Ulcers | 1.71% | 3.10% | 4.75% | 7.04% | 10.27% | 2.58% |
| Anemia | Anemia | 3.50% | 7.75% | 10.79% | 11.27% | 12.44% | 5.04% |
| Obesity (BMI > = 35) | Obesity | 29.38% | 35.93% | 37.38% | 36.54% | 40.48% | 31.25% |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | ||
| Body mass index | BMI | 28.0 (5.5) | 28.58 (6.2) | 29.12 (6.5) | 29.44 (8.6) | 29.35 (7.3) | 28.23 (5.9) |
| Depression (continuous scale) | Depression | 2.61 (3.4) | 3.38 (4.0) | 6.22 (5.7) | 6.87 (5.3) | 7.16 (6.0) | 3.24 (3.2) |
BMI, body mass index; BP, blood pressure; ENT, ear, nose, and throat; GI, gastrointestinal; UTI, urinary tract infection.
Control Variables
The relationships between chronic health conditions and sex, as well as between chronic health conditions and race/ethnicity, are well established.25–32 Thus, we controlled for sex and race/ethnicity in our analyses. Sex was coded 1 for female and 0 for male. Race/Ethnicity was coded 1 for white/non-Hispanic and 0 for nonwhite/Hispanic.
Statistical Analyses
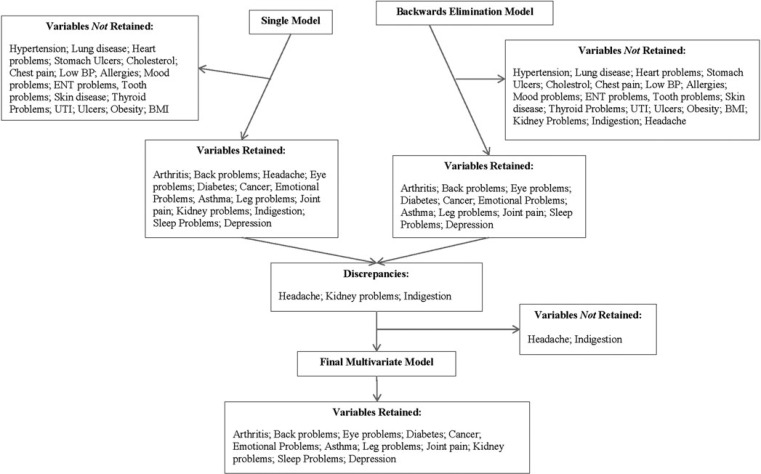
Multinomial logistic regression was used to examine the association between chronic health conditions and membership in the different productivity loss trajectories. All 28 chronic health conditions (listed in table 2), as well as obesity, BMI (continuous), and depression (continuous), were entered into a single model. All conditions reaching an alpha level of 0.05 were retained. In addition, a second model with all 28 chronic health conditions, as well as obesity, BMI (continuous), and depression (continuous), was created using backward elimination with an alpha level of 0.05 to reduce the number of conditions retained. The results of the two models were then compared. When there were discrepancies between the two models in the chronic conditions retained, one at a time, those conditions that resulted in discrepancies were entered into a multivariate model with just the conditions that were retained using both methods (the single model and the backward elimination model). The discrepancy conditions reaching an alpha level of 0.05 when being entered into the model one at a time were kept in the final multivariate model along with the conditions that were retained in both the single model and the backward elimination model. A flow chart of the conditions that were retained in each model is presented in Figure 2.
FIGURE 2.
Flow chart of chronic health conditions included and excluded in analyses. BMI, body mass index; BP, blood pressure; ENT, ear, nose and throat; UTI, urinary tract infection.
The no-risk trajectory was used as the reference group in the multinomial logistic regression model. The relative risk ratios were estimated on the basis of the final model after the backward elimination. The relative risk ratios indicate the risk of the outcome occurring in the given comparison group relative to the risk of the outcome occurring in the reference group.33 In the current study, the comparisons presented are as follows: (1) the low-risk trajectory relative to the no-risk trajectory, (2) the high-risk trajectory relative to the no-risk trajectory, (3) the early-onset increasing risk trajectory relative to the no-risk trajectory, and (4) the late-onset increasing risk trajectory relative to the no-risk trajectory. In addition to these comparisons, Wald tests with one degree of freedom were used to compare the coefficients among the nonreference groups in the model.34 The nonreference group comparisons included (1) low risk compared with high risk, (2) low risk compared with late onset, (3) low risk compared with early onset, (4) high risk compared with late onset, (5) high risk compared with early onset, and (6) late onset compared with early onset. The comparisons were conducted for each of the health conditions included in the final multivariate model. The model was adjusted for sex and race/ethnicity. Using the chronic health conditions from the final multinomial logistic regression model, we examined differences using one-way analysis of variance among the trajectories in the total number of conditions experienced by participants. All analyses were conducted using STATA 13.1 (StataCorp LP, College Station, TX).
RESULTS
Table 2 presents the percentage of respondents in each trajectory who reported experiencing a given chronic health condition. Across the entire sample, the most prevalent condition was obesity, experienced by 31% of the sample, followed by allergies, frequent colds or sinus problems (24%), and back problems (24%). In both the no-risk and low-risk trajectories, the most prevalent conditions were similar to those in the entire sample; however, the most prevalent conditions varied slightly in the remaining three trajectories. For the late-onset trajectory, the most prevalent condition was back problems (46%), followed by foot and leg problems (45%) and obesity (37%). In the early-onset trajectory, back problems (55%) and foot and leg problems (49%) were highly prevalent, but sleep problems (51%) were as well. Finally, in the high-risk trajectory, the most prevalent conditions were joint pains (nonarthritis) (44%), back problems (53%), and foot and leg problems (56%).
Multinomial Logistic Regression Model
Twelve health conditions remained in our final multivariate model after our elimination procedures. The results are presented in Table 3. The 12 conditions were diabetes, cancer, emotional problems, arthritis, asthma, back problems, foot and leg problems, painful joints, eye problems, sleep problems, kidney problems, and depression. Respondents with arthritis, back problems, foot and leg problems, and eye problems were more likely to be in the low-risk trajectory rather than the no-risk trajectory. More specifically, the relative risk of being in the low-risk trajectory compared with the no-risk trajectory was 1.5 times greater if a respondent had arthritis, 1.4 times greater if a respondent had back problems, 1.4 times greater if a respondent had foot and leg problems, and 1.9 times greater if a respondent had eye problems.
TABLE 3. Multinomial Logistic Regression for Chronic Health Conditions and Productivity Loss Trajectories (N = 5583)*.
| Low Risk‡ (LR) | Late Onset‡ (LO) | Early Onset‡ (EO) | High Risk‡ (HR) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 641) | (N = 306) | (N = 207) | (N = 218) | |||||||||
| Chronic Health Condition† | RRR | P | 95% CIs | RRR | P | 95% CIs | RRR | P | 95% CIs | RRR | P | 95% CIs |
| Diabetes | 1.24 | 0.247 | 0.86–1.78 | 1.96 | 0.002 | 1.28–3.00 | 1.98 | 0.007 | 1.21–3.25 | 1.94 | 0.007 | 1.20–3.15 |
| Cancer | 1.19 | 0.580 | 0.65–2.17 | 3.13 | 0.001 | 1.70–5.77 | 2.26 | 0.038 | 1.05–4.89 | 2.86 | 0.003 | 1.43–5.71 |
| Emotional problems | 1.41 | 0.063 | 0.98–2.04 | 3.10 | 0.001 | 2.13–4.51 | 3.47 | 0.001 | 2.27–5.32 | 3.45 | 0.001 | 2.28–5.20 |
| Arthritis | 1.48 | 0.005 | 1.13–1.93 | 1.92 | 0.001 | 1.39–2.66 | 3.20 | 0.001 | 2.23–4.59 | 2.22 | 0.001 | 1.54–3.20 |
| Asthma | 1.24 | 0.192 | 0.90–1.71 | 1.54 | 0.033 | 1.04–2.30 | 2.12 | 0.001 | 1.39–3.24 | 2.92 | 0.001 | 1.98–4.30 |
| Back problems | 1.43 | 0.001 | 1.16–1.76 | 1.85 | 0.001 | 1.41–2.42 | 2.29 | 0.001 | 1.66–3.17 | 2.02 | 0.001 | 1.46–2.80 |
| Leg problems | 1.38 | 0.008 | 1.09–1.74 | 2.18 | 0.001 | 1.62–2.94 | 1.97 | 0.001 | 1.37–2.82 | 2.56 | 0.001 | 1.79–3.65 |
| Painful joints | 1.25 | 0.106 | 0.95–1.64 | 1.53 | 0.011 | 1.10–2.12 | 1.11 | 0.601 | 0.75–1.64 | 1.59 | 0.016 | 1.09–2.32 |
| Eye problems | 1.85 | 0.002 | 1.25–2.75 | 2.81 | 0.001 | 1.83–4.32 | 3.04 | 0.001 | 1.88–4.93 | 3.93 | 0.001 | 2.50–6.17 |
| Sleep problems | 1.03 | 0.804 | 0.79–1.35 | 1.33 | 0.079 | 0.97–1.82 | 2.38 | 0.001 | 1.66–3.41 | 1.41 | 0.060 | 0.99–2.03 |
| Kidney problems | 1.03 | 0.890 | 0.67–1.60 | 1.31 | 0.265 | 0.81–2.11 | 1.85 | 0.014 | 1.13–3.04 | 1.13 | 0.648 | 0.67–1.91 |
| Depression | 1.02 | 0.226 | 0.99–1.04 | 1.10 | 0.001 | 1.07–1.13 | 1.09 | 0.001 | 1.05–1.13 | 1.11 | 0.001 | 1.07–1.14 |
| Covariates | ||||||||||||
| Sex§ | 2.98 | 0.001 | 2.48–3.59 | 0.79 | 0.075 | 0.61–1.02 | 0.70 | 0.023 | 0.51–0.95 | 1.74 | 0.001 | 1.27–2.40 |
| Race‖ | 0.65 | 0.001 | 0.55–0.78 | 0.67 | 0.002 | 1.07–1.14 | 0.60 | 0.001 | 0.44–0.81 | 0.59 | 0.001 | 0.43–0.80 |
*Bolded coefficients represent those with an alpha level of less than 0.05. Model fit: Pseudo R2 = 0.147; LR χ2(56) = 1424.98, P < 0.001.
†Respondents without the specific chronic health condition are used as the reference for each respective condition.
‡The no risk trajectory (n = 4211) is the reference group for the model.
§Male is the reference group.
‖Nonwhite/Hispanic is the reference group.
CIs, confidence interval; RRR, relative risk ratio.
For all chronic health conditions with the exception of sleep problems and kidney problems, the likelihood was greater for being in the late-onset trajectory relative to the no-risk trajectory. The relative risk of being in the late-onset trajectory compared with the no-risk trajectory was approximately three times greater if a respondent had cancer or emotional problems, and more than two times greater if a respondent had foot or leg problems or eye problems.
There was a greater likelihood of being in the early-onset trajectory relative to the no-risk trajectory for all chronic health conditions with the exception of painful joints. Most notably, the relative risk was more than three times greater for being in the early-onset trajectory compared with the no-risk trajectory if a respondent had emotional problems, arthritis, or eye problems. In addition, the relative risk of being in the early-onset trajectory was more than two times greater if a respondent had cancer, asthma, back problems, or sleep problems.
The highest relative risks for the high-risk trajectory compared with the no-risk trajectory were for emotional problems (3.5) and eye problems (3.9). The relative risk for being in the high-risk trajectory compared with the no-risk trajectory was over two times greater if a respondent had cancer, arthritis, asthma, back problems, or foot and leg problems.
In addition to the comparisons with the reference group (the no-risk trajectory), we also examined differences in the coefficients for the nonreference groups. The results are presented in Table 4. The coefficient for cancer was significantly greater for the late-onset and high-risk trajectories than for the low-risk trajectory. For emotional problems, the coefficients were significantly greater for the late-onset, early-onset, and high-risk trajectories than for the low-risk trajectory. Similarly, for depression, the coefficients were also significantly greater for the late-onset, early-onset, and high-risk trajectories than for the low-risk trajectory. For arthritis, the early-onset trajectory coefficient was significantly greater than both the late-onset and low-risk trajectories, and the high-risk trajectory coefficient was greater than the low-risk trajectory coefficient. For asthma, the high-risk trajectory had a larger coefficient than both the late-onset and low-risk trajectories, and the early-onset trajectory also had a larger coefficient than the low-risk trajectory. The coefficients for back problems and kidney problems were greater for the early-onset trajectory than the low-risk trajectory; for foot and leg problems, the coefficients were greater for the late-onset and high-risk trajectories than for the low-risk trajectory. Finally, for eye problems the high-risk trajectory coefficient was greater than that for the low-risk trajectory; for sleep problems, the coefficient was greater for the early-onset trajectory than for the late-onset, high-risk, or low-risk trajectories.
TABLE 4. Wald Test Comparisons Among Nonreference Trajectories*.
| Early Onset vs | Early Onset vs | Late Onset vs | Late Onset vs | High Risk vs | Early Onset vs | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Late Onset | High Risk | High Risk | Low Risk | Low Risk | Low Risk | |||||||
| Chronic Health Condition | χ2 | P | χ2 | P | χ2 | P | χ2 | P | χ2 | P | χ2 | P |
| Diabetes | 0.00 | 0.971 | 0.00 | 0.949 | 0.00 | 0.975 | 3.16 | 0.076 | 2.60 | 0.107 | 2.66 | 0.103 |
| Cancer | 0.61 | 0.436 | 0.29 | 0.587 | 0.06 | 0.812 | 6.41 | 0.011 | 4.57 | 0.033 | 2.05 | 0.152 |
| Emotional problems | 0.22 | 0.636 | 0.00 | 0.973 | 0.20 | 0.651 | 11.40 | 0.001 | 13.35 | 0.001 | 12.62 | 0.001 |
| Arthritis | 5.51 | 0.019 | 2.52 | 0.113 | 0.45 | 0.503 | 1.84 | 0.175 | 3.83 | 0.050 | 13.60 | 0.001 |
| Asthma | 1.59 | 0.208 | 1.65 | 0.199 | 6.99 | 0.008 | 0.87 | 0.352 | 14.05 | 0.001 | 4.83 | 0.028 |
| Back problems | 1.18 | 0.277 | 0.34 | 0.561 | 0.21 | 0.647 | 2.52 | 0.112 | 3.57 | 0.059 | 6.48 | 0.011 |
| Leg problems | 0.22 | 0.641 | 1.21 | 0.271 | 0.54 | 0.462 | 6.59 | 0.010 | 9.36 | 0.002 | 3.00 | 0.083 |
| Painful joints | 1.90 | 0.168 | 2.10 | 0.147 | 0.03 | 0.861 | 1.07 | 0.302 | 1.26 | 0.261 | 0.28 | 0.598 |
| Eye problems | 0.09 | 0.771 | 0.87 | 0.350 | 1.72 | 0.190 | 2.67 | 0.102 | 8.34 | 0.004 | 3.18 | 0.075 |
| Sleep problems | 7.10 | 0.008 | 4.95 | 0.026 | 0.09 | 0.769 | 1.68 | 0.195 | 2.24 | 0.134 | 15.57 | 0.001 |
| Kidney problems | 1.49 | 0.222 | 2.74 | 0.098 | 0.25 | 0.619 | 0.69 | 0.401 | 0.09 | 0.764 | 3.94 | 0.047 |
| Depression | 0.46 | 0.497 | 0.59 | 0.444 | 0.02 | 0.892 | 22.54 | 0.001 | 20.14 | 0.001 | 12.25 | 0.001 |
*Bolded coefficients represent those with an alpha level of less than 0.05.
Total Number of Chronic Health Conditions
Using all the chronic health conditions from the multinomial logistic regression model (with the exception of the continuous measure of depression), specifically diabetes, cancer, emotional problems, arthritis, asthma, back problems, leg problems, joint pain, eye problems, sleep problems, and kidney problems, we found differences among the trajectories in the total number of chronic health conditions experienced [F(4,5579) = 418.21, P < 0.0001]. On average, the no-risk trajectory experienced 0.81 conditions (SD = 1.17), the low-risk trajectory experienced 1.35 conditions (SD = 1.49), the late-onset trajectory experienced 2.61 conditions (SD = 1.91), the early-onset trajectory experienced 3.20 conditions (SD = 2.11), and the high-risk trajectory experienced 3.34 conditions (SD = 2.28). Results from post hoc tests using Bonferroni comparisons revealed that all groups differed significantly from each other (P < 0.001) with the exception of the early-onset trajectory compared with the high-risk trajectory. In Table 5, we present the percentage of the sample within each trajectory by the number of chronic health conditions experienced. As can be seen in the table, more than half of the respondents (55%) in the no-risk trajectory reported no chronic health conditions. In the low-risk trajectory, the majority (64%) of respondents reported either no chronic health conditions or just one condition. In the late-onset trajectory, the largest percentage of respondents (23%) reported two conditions, whereas in the early-onset trajectory, the largest percentage of respondents (17%) reported three conditions and in the high-risk trajectory, the largest percentage of respondents (17%) reported four conditions.
TABLE 5. Percentage of Respondents in Each of the Trajectories by the Number of Chronic Health Conditions Reported*.
| Number of Chronic Conditions | No Risk, % | Low Risk, % | Late Onset, % | Early Onset, % | High Risk, % |
|---|---|---|---|---|---|
| 0 | 54.98 | 37.29 | 15.21 | 11.00 | 11.01 |
| 1 | 24.54 | 26.68 | 15.31 | 13.88 | 14.68 |
| 2 | 11.12 | 15.91 | 23.13 | 15.31 | 14.22 |
| 3 | 5.61 | 10.14 | 15.64 | 16.75 | 13.76 |
| 4 | 2.26 | 5.46 | 13.36 | 15.31 | 16.51 |
| 5 | 0.95 | 3.28 | 8.14 | 11.00 | 11.01 |
| 6 | 0.40 | 0.62 | 6.19 | 11.00 | 9.17 |
| 7 | 0.10 | 0.47 | 2.61 | 2.87 | 5.50 |
| 8 | 0.05 | 0.16 | 0.00 | 2.87 | 2.75 |
| 9 | 0.00 | 0.00 | 0.33 | 0.00 | 0.92 |
| 10 | 0.00 | 0.00 | 0.00 | 0.00 | 0.46 |
*Chronic health conditions included diabetes, cancer, emotional problems, arthritis, asthma, back problems, foot and leg problems, painful joints, eye problems, sleep problems, and kidney problems.
DISCUSSION
In this study, we examined the relative risk for being in different longitudinal trajectories of health-related productivity loss based on having experienced certain physical and mental chronic health conditions by the age of 40 years. For individuals with a very low (approximately zero) probability for productivity loss, the relative risk of being in a higher risk trajectory was related to having certain chronic health conditions, specifically diabetes, cancer, emotional problems, arthritis, asthma, back problems, foot and leg problems, painful joints, eye problems, sleep problems, kidney problems, and depression. In general, we found that similar conditions were associated with having a greater relative risk of being in one of the other four trajectories (low risk, early-onset increasing risk, late-onset increasing risk, and high risk) compared with the no-risk trajectory.
The relative risks of being in the low-risk trajectory compared with the no-risk trajectory, based on the chronic conditions, were consistently weaker than the relative risks for being in the high-risk, early-onset, or late-onset trajectories compared with the no-risk trajectory. The main conditions distinguishing the low-risk trajectory from the no-risk trajectory were musculoskeletal conditions, including arthritis, back problems, and foot and leg problems, as well as eye problems. In the late-onset trajectory, the highest relative risks were for cancer, emotional problems, and eye problems. In the early-onset trajectory, the highest relative risks were for emotional problems, arthritis, and eye problems. Finally, for the high-risk group, the highest relative risks were for emotional problems, eye problems, and asthma. These results are consistent with previous research, suggesting that the chronic health conditions in our model are related to productivity loss.3,11,12,19,35–38
Overall, the probability of being in a productivity loss trajectory associated with a high level of productivity loss over time was greater for having the various chronic conditions. In the previous study identifying the productivity loss trajectories, the high-risk trajectory had the greatest overall probability of productivity loss over time, followed by the early-onset increasing risk trajectory, then the late-onset increasing risk trajectory, then the low-risk trajectory, and finally the no-risk trajectory. Accordingly, the relative risks in this study were generally higher for the high-risk, early-onset, and late-onset trajectories than for the low-risk and no-risk trajectories. In addition, when looking at the total number of chronic conditions experienced, the high-risk and early-onset trajectories had a greater average number of chronic conditions experienced than the other groups. The next highest was the late-onset trajectory followed by the low-risk trajectory. The no-risk trajectory had an average of less than one chronic health condition. In fact, more than half of the no-risk trajectory did not experience any of the chronic health conditions in our model. In contrast, fewer than a quarter of the high-risk and early-onset trajectories did not experience any of the conditions, while more than a quarter of the respondents in these trajectories reported five or more chronic conditions. This is consistent with previous studies, suggesting that work impairment increases with the number of chronic health conditions experienced.37
Implications
There are several implications for our findings. First, our finding of a relationship between chronic health conditions and membership in the different productivity loss trajectories suggests that lifetime patterns of experiencing productivity loss are likely dependent on experiencing chronic health conditions. For the most part, we did not find different conditions influencing the relative risk of being in the different trajectories; rather, we found a greater prevalence of experiencing similar conditions based on the probability of productivity loss for the trajectories. For example, foot and leg problems were one of the more frequently experienced chronic health conditions and the prevalence of foot and leg problems in the different trajectories steadily increased from the no-risk trajectory to the high-risk trajectory. Because the same types of conditions differentiate the groups, this suggests that health promotion programs aimed at reducing the prevalence and effects of chronic health conditions may help reduce the frequency of individuals falling into one of the higher-risk trajectories of productivity loss.
Second, we found that the total number of chronic health conditions experienced varied by the productivity loss trajectories. From this perspective, it may be that individuals with a persistent history of productivity loss do not experience just one chronic health condition, instead these individuals suffer a greater number of chronic health conditions. For example, we did not find that people in the high-risk trajectory experienced only back problems or depression, whereas those in the no-risk trajectory experienced only obesity, but that individuals in the higher-risk trajectories experienced multiple chronic health conditions, suggesting that comorbidities may play a role in having a high probability of productivity loss across the working years.
Third, although many of the chronic health conditions in our analyses were physical health conditions, it is important to note that both emotional problems and depression were key conditions associated with the relative risks of being in the different trajectories. This finding further underscores the importance of research examining the relationship between mental health and productivity loss, in particular depression, which is one of the leading mental health conditions impacting productivity loss at work.16
Finally, in this study, obesity was eliminated from our multinomial logistic regression model because of a lack of significance. Several previous studies have illustrated a relationship between obesity and productivity loss.13,39–41 In the current study, we found a generally high incidence of obesity regardless of the trajectory group, suggesting that obesity is not highly related to being in the different productivity loss trajectories. Instead, the chronic health conditions, such as diabetes, asthma, and arthritis, that are associated with obesity may be what impacts the likelihood of having productivity loss from ages 25 to 44 years.42 Nevertheless, to the extent that obesity increases the chances of developing these other conditions, programs targeting weight loss may be effective for lowering the risk of individuals falling into one of the higher-risk trajectories by decreasing the likelihood of developing chronic health conditions.
Strengths and Limitations
Strengths of this study include long-term follow-up, a high retention rate, unique data on work productivity impacts ascertained repeatedly over time, and evaluation of several common chronic health conditions. There are several limitations in this study that need to be acknowledged when considering the findings. One of the biggest limitations is that our analyses were unable to assess causation. We have no way of knowing whether the chronic health conditions actually caused or preceded the productivity loss resulting in membership in the different trajectories. It is possible that individuals happened to have a minor temporary health condition that led to a report of productivity loss, but this was unlikely to result in assignment to a higher-risk trajectory, as this required multiple waves with productivity loss. Future research should aim to ask individuals experiencing health-related productivity loss to identify the health conditions causing the loss.
A second limitation is that we examined trajectories of productivity loss based on a combination of absenteeism and presenteeism. Previous research has often analyzed productivity loss separately for absenteeism and presenteeism and has found differences in risk factors across the two.1,11,13,43 It is possible that there would be differences in the types of chronic health conditions associated with the different productivity loss trajectories based on whether the loss was the result of presenteeism or absenteeism. Future research may seek to identify longitudinal patterns of presenteeism and absenteeism separately to assess the independent relationships of these types of productivity loss with chronic health conditions.
A third limitation is the age range used in this study. We focused on workers aged 25 to 44 years in the trajectories and examined health conditions at the age of 40 years. This age is relatively young for many of the health conditions included. It is likely that many additional individuals will experience the conditions we examined at later points in their lives and there is no way to identify these individuals in our analyses. In addition, patterns of productivity loss will continue throughout one's working career, which normally goes beyond the age of 44 years. We are unable to capture the full pattern of productivity loss at this time. Future analyses may continue to explore the trajectories examined here as more data on this cohort become available. As additional waves of data become available, future research may also explore the relationship between the trajectories with the timing of experiencing chronic health conditions, specifically before the age of 40 years, between ages 40 and 60 years, and after the age of 60 years to assess whether the trajectories are predictive of the timing.
A fourth limitation is with the sample size. Although the overall sample size for our analyses was high (more than 5000 cases), the within-trajectory sample sizes that had the various chronic conditions were relatively low. This limited our ability to stratify our analyses by sex and/or race. For example, there were no male respondents in the low-risk trajectory who experienced cancer by the age of 40 years. As a result, if we were to estimate separate models by sex, cancer would not be able to be included in the model. Based on the wealth of previous research showing sex and racial differences in chronic health conditions, future research may attempt to analyze the relationships assessed in this study in stratified models for sex and race.
Another limitation is with the measure of chronic health conditions. These questions were asked at a single time point. Only a few of the conditions were asked in relation to whether a doctor had diagnosed them with the condition. Also, information was not available for all of the conditions on when the condition started and, if appropriate, ended. In addition, there was no information on severity of the condition. For example, some individuals may have suffered from severe asthma whereas others had very mild asthma. The severity of a given condition would likely have a major impact on the productivity loss associated with it. Along the lines of measurement issues, in this study we used previously identified trajectories of productivity loss.20 Accordingly, the limitations discussed in the previous work warrant attention here. Most notable is the limitation associated with the way the productivity loss questions were asked, specifically, for just a single week in a given interview year. Future longitudinal research with more detailed measures is needed to more fully understand the relationship between temporal patterns of productivity loss and chronic health conditions.
CONCLUSIONS
Chronic health conditions are related to the relative risks of being in different health-related productivity loss trajectories. Similar conditions occur in the different trajectories, but the prevalence of various chronic conditions and the total number of chronic conditions is higher in the trajectories with a greater probability of productivity loss over time. In sum, interventions aimed at decreasing the occurrence and severity of chronic health conditions may help reduce the percentage of individuals who find themselves on a longitudinal trajectory of having frequent and recurrent productivity loss in one's working years.
Footnotes
Authors Besen and Pransky have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
This work was funded by the Liberty Mutual Research Institute for Safety.
REFERENCES
- 1.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med. 2004;46:398–412. [DOI] [PubMed] [Google Scholar]
- 2.Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the “Top 10” physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med. 2003;45:5–14. [DOI] [PubMed] [Google Scholar]
- 3.Collins JJ, Baase CM, Sharda CE, et al. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J Occup Environ Med. 2005;47:547–557 [DOI] [PubMed] [Google Scholar]
- 4.Burton W, Morrison A, Maclean R, Ruderman E. Systematic review of studies of productivity loss due to rheumatoid arthritis. Occup Med. 2006;56:18–27. [DOI] [PubMed] [Google Scholar]
- 5.Koopmanschap M, Burdorf A, Lotters F. Work absenteeism and productivity loss at work. In: Loisel P, Anema JR, eds. Handbook of Work Disability: New York: Springer; 2013:31–41. [Google Scholar]
- 6.Witters D, Agrawal S. Unhealthy U.S. Workers' Absenteeism Costs $153 Billion. Washington, D.C.: Gallup Well-Being; 2011. [Google Scholar]
- 7.Davis K, Collins S, Doty M, Ho A, Holmgren A. Health and productivity among US workers. Issue Brief New York: Commonwealth Fund; 2005:1–10. [PubMed] [Google Scholar]
- 8.Integrated Benefits Institute. Poor Health Costs U.S. Economy $576 Billion. San Francisco, CA: Integrated Benefits Institute; 2012. [Google Scholar]
- 9.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. J Occup Environ Med. 2003;45:1234–1246. [DOI] [PubMed] [Google Scholar]
- 10.Witters D, Liu D. In U.S., Poor Health Tied to Big Losses for All Job Types. Washington, D.C.: Gallup Well-Being; 2013. [Google Scholar]
- 11.Holden L, Scuffham PA, Hilton MF, Ware RS, Vecchio N, Whiteford HA. Which health conditions impact on productivity in working Australians? J Occup Environ Med. 2011;53:253–257. [DOI] [PubMed] [Google Scholar]
- 12.Iverson D, Lewis KL, Caputi P, Knospe S. The cumulative impact and associated costs of multiple health conditions on employee productivity. J Occup Environ Med. 2010;52:1206–1211. [DOI] [PubMed] [Google Scholar]
- 13.Boles M, Pelletier B, Lynch W. The relationship between health risks and work productivity. J Occup Environ Med. 2004;46:737–745. [DOI] [PubMed] [Google Scholar]
- 14.Berndt ER, Finkelstein SN, Greenberg PE, et al. Workplace performance effects from chronic depression and its treatment. J Health Econ. 1998;17:511–535. [DOI] [PubMed] [Google Scholar]
- 15.Kessler RC, Barber C, Birnbaum HG, et al. Depression in the workplace: effects on short-term disability. Health Aff. 1999;18:163–171. [DOI] [PubMed] [Google Scholar]
- 16.Lerner D, Adler DA, Chang H, et al. Unemployment, job retention, and productivity loss among employees with depression. Psychiatr Serv. 2004;55:1371–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lerner D, Adler DA, Chang H, et al. The clinical and occupational correlates of work productivity loss among employed patients with depression. J Occup Environ Med. 2004;46:S46–S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lerner D, Henke RM. What does research tell us about depression, job performance, and work productivity? J Occup Environ Med. 2008;50:401–410. [DOI] [PubMed] [Google Scholar]
- 19.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003;289:3135–3144. [DOI] [PubMed] [Google Scholar]
- 20.Besen E, Pransky G. Trajectories of productivity loss over a 20-year period: an analysis of the National Longitudinal Survey of Youth. Scand J Work Environ Health. 2014;40:380–389. [DOI] [PubMed] [Google Scholar]
- 21.Bureau of Labor Statistics. The NLSY79: NLS handbook. Washington, DC: US Department of Labor; 2005. [Google Scholar]
- 22.Jones BL, Nagin DS. A note on a Stata plugin for estimating group-based trajectory models. Sociol Methods Res. 2013;42:608–613. [Google Scholar]
- 23.Jung T, Wickrama K. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2008;2:302–317. [Google Scholar]
- 24.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 25.Verbrugge LM. Gender and health: an update on hypotheses and evidence. J Health Soc Behav. 1985:156–182. [PubMed] [Google Scholar]
- 26.Strauss J, Gertler PJ, Rahman O, Fox K. Gender and life-cycle differentials in the patterns and determinants of adult health. J Hum Resour. 1993;28:791–837. [Google Scholar]
- 27.Bird CE, Rieker PP. Gender matters: an integrated model for understanding men's and women's health. Soc Sci Med. 1999;48:745–755. [DOI] [PubMed] [Google Scholar]
- 28.Kornstein SG, Schatzberg AF, Thase ME, et al. Gender differences in chronic major and double depression. J Affect Disord. 2000;60:1–11. [DOI] [PubMed] [Google Scholar]
- 29.Denton M, Prus S, Walters V. Gender differences in health: a Canadian study of the psychosocial, structural and behavioural determinants of health. Soc Sci Med. 2004;58:2585–2600. [DOI] [PubMed] [Google Scholar]
- 30.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff. 2005;24:325–334. [DOI] [PubMed] [Google Scholar]
- 31.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995:349–386. [Google Scholar]
- 32.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. [DOI] [PubMed] [Google Scholar]
- 33.UCLA: Statistical Consulting Group. Multinomial Logistic Regression. Los Angeles: University of California Los Angeles. [Google Scholar]
- 34.Fox J. Applied Regression Analysis, Linear Models, and Related Methods. Thousand Oaks, CA: Sage Publications; 1997. [Google Scholar]
- 35.Burton WN, Chen C-Y, Schultz AB, Conti DJ, Pransky G, Edington DW. Worker productivity loss associated with arthritis. Dis Manag. 2006;9:131–143. [DOI] [PubMed] [Google Scholar]
- 36.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290:2443–2454. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Greenberg PE, Mickelson KD, Meneades LM, Wang PS. The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med. 2001;43:218–225. [DOI] [PubMed] [Google Scholar]
- 38.Burton WN, Pransky G, Conti DJ, Chen C-Y, Edington DW. The association of medical conditions and presenteeism. J Occup Environ Med. 2004;46:S38–S45. [DOI] [PubMed] [Google Scholar]
- 39.Musich S, Hook D, Baaner S, Edington DW. The association of two productivity measures with health risks and medical conditions in an Australian employee population. Am J Health Promot. 2006;20:353–363. [DOI] [PubMed] [Google Scholar]
- 40.Hertz RP, Unger AN, McDonald M, Lustik MB, Biddulph-Krentar J. The impact of obesity on work limitations and cardiovascular risk factors in the US workforce. J Occup Environ Med. 2004;46:1196–1203. [PubMed] [Google Scholar]
- 41.Gates DM, Succop P, Brehm BJ, Gillespie GL, Sommers BD. Obesity and presenteeism: the impact of body mass index on workplace productivity. J Occup Environ Med. 2008;50:39–45. 10.1097/JOM.1090b1013e31815d31818db31812. [DOI] [PubMed] [Google Scholar]
- 42.Østbye T, Malhotra R, Landerman LR. Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 Cohort (1981–2006). Int J Epidemiol. 2011;40:240–250. [DOI] [PubMed] [Google Scholar]
- 43.Caverley N, Cunningham JB, MacGregor JN. Sickness presenteeism, sickness absenteeism, and health following restructuring in a public service organization. J Manage Stud. 2007;44:304–319. [Google Scholar]