Abstract
Objective
While self-efficacy (SE) and outcome-expectancy (OE) have been well researched as predictors of outcome, few studies have investigated changes in these variables across treatments. We evaluated changes in OE and SE throughout treatment as predictors of outcomes in a large sample with panic disorder, generalized anxiety disorder, social anxiety disorder, or post-traumatic stress disorder. We hypothesized that increases in SE and OE would predict reductions in anxiety and depression as well as improvement in functioning.
Method
Participants (mean age = 43.3, SD=13.2, 71.1% female, 55.5% white) were recruited from primary care centers throughout the US and were randomized to receive either Coordinated Anxiety Learning and Management (CALM) treatment, comprised of cognitive-behavioral therapy, psychotropic medication, or both, or to usual care. SE and OE ratings were collected at each session for participants in the CALM treatment (n=482) and were entered into a structural equation model as predictors of changes in Brief Symptom Inventory, Anxiety Sensitivity Index, Patient Health Questionnaire, and Sheehan Disability Scale outcomes at 6, 12, and 18 months after baseline.
Results
The best fitting models predict symptom levels from OE and SE and not vice versa. The slopes and intercept of OE significantly predicted change in each outcome variable except PHQ-8. The slope and intercept of SE significantly predicted change in each outcome variable.
Conclusion
Over and above absolute level, increases in SE and OE were significant predictors of decreases in symptoms and increases in functioning. Implications for treatment are discussed, as well as future directions of research.
Keywords: Self-efficacy, outcome-expectancy, anxiety, cognitive behavioral therapy, primary care
Self-efficacy and outcome-expectancy have been written about extensively over decades. Outcome-expectancy is the degree to which one believes that a particular outcome will occur, whereas self-efficacy is the degree of conviction that one can successfully execute the behavior required to produce an outcome(1). In terms of treatment, outcome-expectancy is the belief that a particular treatment will reduce symptom levels or improve functioning(2), whereas self-efficacy is one’s judgment of capability for successfully participating in and completing treatment(3). While these are clearly related concepts, they are differentiated because individuals can believe that they are capable of completing treatment, and yet not believe that the treatment will be effective at reducing their distress, and vice versa(4). Outcome-expectancy and self-efficacy are both theorized to enhance task motivation and intention to complete a behavior, as well as to determine the degree of effort expended and persistence in the face of obstacles or aversive experiences(5, 6).
A number of studies have found that initial outcome expectancies, usually measured at completion of the first therapy session, predict treatment outcome. This is the case for various psychosocial treatment approaches, including cognitive behavioral therapy (CBT), non-directive therapy and applied relaxation for generalized anxiety disorder(7), cognitive-behavioral group therapy for social anxiety disorder(8, 9), in vivo exposure therapy and virtual reality therapy for specific phobia(10), and CBT and interpersonal therapy for depression(11). In addition, expectation for medication to work consistently predicts actual response to drug treatments(12). Similarly, self-efficacy has been shown to predict outcome across a variety of treatments and disorders. Results are similar for treatment-related self-efficacy (i.e., belief in an ability to complete the necessary steps of treatment)(5) and disorder-related self-efficacy (i.e., belief in ability to engage or not engage in a disorder-specific behavior)(13–16). Higher initial self-efficacy predicted better post-treatment outcomes from either CBT or a 12-step facilitation treatment for substance abuse with comorbid depression(13), six-month outcomes from ‘treatment as usual’ for substance abusers(14), and six-month outcomes from CBT and supportive therapy for depressed adolescents(15). Also, initial self-efficacy significantly predicted response to medication(15) and better maintenance of fear reduction following medication treatment(16). Therefore, baseline values of both self-efficacy and outcome-expectancy are robust predictors of outcome across a wide array of conditions and treatments.
Despite the extensive research on initial levels of self-efficacy and outcome-expectancy, little research has examined whether change in self-efficacy and outcome-expectancy throughout the course of treatment explains outcome, even though these expectancies are theorized to change over time and subsequently result in symptom improvement(3, 17). In the only study of change over time in outcome-expectancy, Newman and Fisher(18) found that rate of change in outcome-expectancy across multiple treatment sessions predicted reductions in generalized anxiety disorder severity at post-CBT. However, they neither examined self-efficacy nor did they evaluate long-term outcomes. Pre- to post-treatment changes in self-efficacy have been shown to precede symptom reduction(19) or to predict symptomatic improvement at post-treatment(20, 21). In the one study that conducted a true mediational analysis, changes in self-efficacy (measured at three time-points) did not predict changes in outcome)(22). Therefore, very little is known about the degree to which changes in expectancies predict treatment outcomes. Greater understanding of these predictive pathways has the potential to inform treatment strategies and in turn augment outcomes.
In the current investigation, we evaluated the directional relationship between session ratings of self-efficacy, outcome-expectancy, and symptoms/functioning using a cross-lagged panel analysis. This analysis will reveal the timing of changes in self-efficacy, outcome-expectancy, and symptoms/functioning, as well as provide justification for examining the predictive power of self-efficacy and outcome expectancy on symptom/functioning levels once treatment has ended. The current study is a secondary analyses as part of a larger, randomized-controlled trial comparing the efficacy of CBT, medications, or both to treatment as usual in primary care.(23, 24) We hypothesize that self-efficacy and outcome-expectancy from one session will be predictive of symptoms/functioning at a later session and not vice versa. This study also evaluated absolute level and change in outcome-expectancy and self-efficacy as predictors of treatment outcomes over 18 months in a large sample with various anxiety disorders. We hypothesize that greater improvements in self-efficacy and outcome-expectancy would predict greater reductions in anxiety and depression and greater improvements in functioning across 18 months.
Methods
Participants
Participants were recruited from primary care clinics throughout the United States as part of the CALM study(23, 24). They were diagnosed with a principal anxiety disorder of panic disorder (n=262), generalized anxiety disorder (n=549), social anxiety disorder (n=132), or post-traumatic stress disorder (n=61). Participants were at least 18 years-old, spoke either English or Spanish, were not currently suicidal, had no marked cognitive impairment or life-threatening medical conditions, and had no diagnoses of bipolar I disorder or psychosis. With the exception of alcohol and marijuana abuse, substance abuse or dependence were exclusion factors. More than half of participants had comorbid anxiety disorders and two-thirds had major depression. Participants were referred through their primary care physician or nursing staff and were screened for eligibility by an Anxiety Clinical Specialist (ACS) using the Mini- International Neuropsychiatric Interview(25). Full details about recruitment are available in Appendix I and in the primary outcome paper(23). Participants averaged 43.5 years (SD = 13.4), and were primarily white (69.6%) and female (71.1%).
Intervention
Participants were randomized to either usual care (UC) or the CALM intervention, comprised of CBT, medication recommendations, or both.
CALM Intervention (ITV) Treatment
CBT was delivered by a therapist who was guided by computer-program as a way of maintaining CBT fidelity. CBT included generic modules (self-monitoring, psychoeducation, fear hierarchies, breathing retraining, and relapse prevention) and modules that were tailored to the most distressing/disabling anxiety disorder (cognitive restructuring and exposure)(26). The sequence of module presentation was largely standardized, but therapists had some flexibility in choosing module order based on clinical need. Participants completed 7.0 CBT sessions on average, but flexibility in number of sessions was permitted (range = 0–21) based on session by session monitoring of symptom status and supervision. Full details of the computer-assisted CBT are described by Craske et al.(26).
Medications were monitored by an Anxiety Clinical Specialist (ACS, see below; 56% in person, 43% over the phone). This included tracking adherence to medication, as well as providing counseling to avoid alcohol and caffeine and improve sleep quality. The ACS was also involved in relaying information from the medication management sessions to primary care providers, who were the prescribers. After 10–12 weeks in ITV, patients who remained symptomatic (above the clinical cutoff score of 8 on the Overall Anxiety Severity and Impairment Scale (OASIS)) could opt to continue in the same modality (CBT or medication) or the alternative modality, for up to 12 months. Following active treatment, participants received monthly follow-up phone calls to reinforce CBT concepts and/or medication adherence, again up to 12 months following baseline.
Following baseline assessment, 482 of 503 patients (95%) in ITV had at least 1 intervention contact. Over the 12 months after study entry, patients had a mean (SD) of 7.0 (4.1) (median= 8) CBT visits and 2.24 (3.57) (median = 1) medication/care management visits. Of the total 482 patients, 166 (34%) had only CBT sessions, 43 (9%) had only medication/care management sessions, and 273 (57%) had both. Once patients were randomized to the ITV condition they were allowed to choose whether they would receive CBT only, medication only, or both. 424 patients (88%) had all visits by 6 months. For more details of ACS see Roy-Byrne and colleagues(23) and Appendix I and II.
Anxiety Clinical Specialists (ACS)
These individuals were selected to be relatively novice to the delivery of mental health treatment in order to increase the generalizability of the findings. They included 6 social workers, 5 registered nurses, 2 masters level clinicians, and 1 doctoral level psychologist. Only 9 of the 14 had prior experience in delivering mental health services (mean years of experience = 3.89), and none had expertise in treating anxiety disorders or in CBT. Full details of ACS training are available in Rose et al.(27).
Usual Care (UC)
Participants who were randomized to UC received continued care with their primary care provider. UC participants were excluded from the analyses reported herein, since outcome-expectancy and self-efficacy data were not collected throughout their treatment.
Measures
Predictor Variables
Outcome-expectancy (OE)
Participants answered “How likely is it that your anxiety can be successfully treated?” on a 0–8 Likert scale, where 0 = not at all, 2 = possibly, 4 = 50/50, 6 = very likely, and 8 = certainly, with anchors occurring on every other item on the Likert scale. OE ratings were gathered at the beginning of each treatment session.
Self-efficacy (SE)
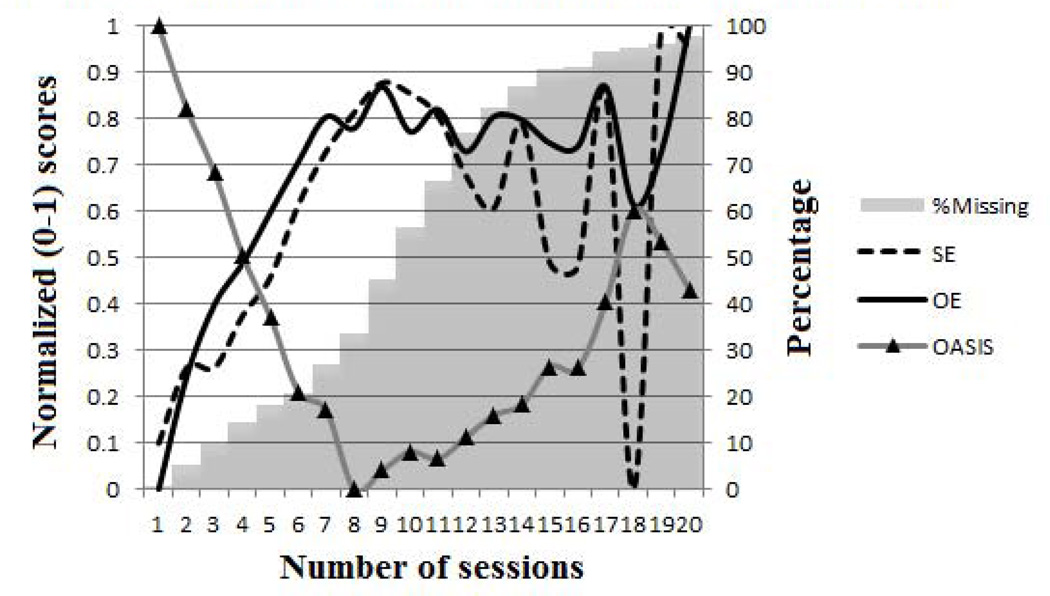
Participants answered “How likely is it you will be able to do what is necessary to make your anxiety treatment successful?” on a 0–8 Likert scale where 0 = not at all, 2 = possibly, 4 = 50/50, 6 = very likely, and 8 = certainly, with anchors occurring on every other item on the Likert scale. SE ratings were gathered at the beginning of each treatment session. See Figure 1 for a graph of both OE and SE throughout treatment, as well as information about the percentage of data drop-off as session numbers increased (due to a number of factors including participants completing treatment early, as well as attrition).
Figure 1.
Change in SE, OE, and OASIS over treatment and missing data
Overall Anxiety Severity and Impairment Scale (OASIS)(28)
This 5- item self-report measure captures severity of anxious symptoms as well as functional impairment associated with those symptoms. The measure is rated on a 0–4 point Likert scale. The measure has high internal consistency and good convergent validity(28) and was completed at the start of each session.
Outcomes
Outcome measures were administered during a telephone assessment conducted by RAND Corporation interviewers, blinded to treatment condition and timing of assessment, at baseline, 6 months, 12 months and 18 months.
Brief Symptom Inventory (BSI)(29)
The BSI-18 is a self-report measure of psychological symptoms. The current study used a 12-item version of the measure that included somatization and anxiety subscales, but excluded the depression subscale. The measure is rated on 0 to 4 Likert scale, where 0 = not at all and 4 = extremely. The BSI has demonstrated good test-retest reliability, as well as high correlations with its parent measure, the Symptom Checklist-90R(30). In the current sample, Cronbach’s alpha was .87, .90, .90, and .90 at baseline, 6 month, 12 month, and 18 month assessments, respectively.
Anxiety Sensitivity Index (ASI)(31)
The ASI is a 16-item self-report measure of beliefs that anxiety is harmful, rated on a 0–4 point Likert scale, where 0 = very little and 4 = very much. It has demonstrated good reliability and is factorally independent from other measures of anxiety(32). In the current sample, Cronbach’s alpha was .88, .91, .91, and .91 at baseline, 6 month, 12 month, and 18 month assessments, respectively.
Patient Health Questionnaire (PHQ-8)(33)
The PHQ-8 is a measure of depression severity (the item assessing suicidal ideation and intent from the PHQ-9 was dropped due to the feasibility of conducting a thorough suicide risk assessment by the blind assessors and due to the exclusion of patients who were suicidal at baseline), with each item rated on a 0–3 Likert scale, where 0 = not at all and 3 = nearly every day. The PHQ-9 has demonstrated adequate reliability and validity(34). In the current sample, Cronbach’s alpha was .86, .90, .91, and .90 at baseline, 6 month, 12 month, and 18 month assessments, respectively.
Sheehan Disability Scale (SDS)(35)
The SDS measures functional impairment with 3 items that are rated on a 0–10 point scale, where 0 = not at all and 10 = extremely. It has demonstrated high internal consistency and construct validity(36). In this sample, the Cronbach’s alpha was .83, .90, .91, and .90 at baseline, 6 month, 12 month, and 18 month assessments, respectively.
Data analysis
Data analysis was conducted in three steps. First, cross-lagged panel analyses were used to examine whether SE and OE predict changes in OASIS, OASIS predicts changes in SE and OE, or both. Second, preliminary longitudinal growth models for each dependent and independent variable were developed. Third, we conducted our primary analyses using the growth parameters of the independent variables to predict change in the dependent variables.
Residual Covariance Structure
For all models, residual covariance structures from the growth modeling literature(37) were examined, including: homogenous, heterogenous, autoregressive, and Toeplitz as implemented in the mplusRcov function of MplusAutomation(38). Homogenous and heterogenous allow the variances to be identical or vary over time, and the autoregressive and Toeplitz allow correlations between the residuals. The structure resulting in best model fit was retained.
Missing Data
Full information maximum likelihood (FIML) was used to estimate the model with missing data. FIML yields unbiased estimates when data are missing completely at random or missing at random, and simulation studies demonstrate it is a more efficient estimator than listwise deletion(39). To examine possible predictors of missingness, the last time-point where participants had data on ASI, BSI, PHQ, or SDS in the overall study was coded. In addition, the last time-point for session variables (SE, OE, or OASIS) was coded. Neither dropout variable was significantly associated with baseline ASI, BSI, PHQ, SDS, nor self-efficacy, outcome-expectancy, or OASIS from the first treatment session. These analyses provide no evidence that the missing at random assumption was violated, although they cannot prove it was met.
Latent Growth Models
Latent Growth Models (LGMs) provide a flexible analysis of change over time and allow individual to vary in where they start (random intercept) and how they change (random slope). The intercept has loadings on the outcomes over time constrained to one, with a freely estimated mean (the overall intercept) and variance (the individual variability around the intercept), and the slope has loadings fixed at time intervals (such as 0, 1, 2, 3 for linear growth) and a freely estimated mean and variance.
Because a plateau effect was expected for the outcome variables, the time loadings were fixed at 0 and 6 for the first two time-points (0 and 6 months) and freely estimated for the third and fourth assessments (12 and 18 months). An example model for ASI is shown in Appendix III.
For the independent variables, eight assessments, corresponding to the first eight treatment sessions, were used. Linear and quadratic growth over sessions were tested and the best fit retained. For the growth model of OE which included both a random linear and quadratic slope, it was necessary to center time for model convergence. For consistency across models, we centered time in all predictor (SE, OE, and OASIS) models at the session midpoint, 4.5.
Statistical Methods
All models were estimated using Mplus version 7(40)). Good model fit was chosen as the combination of the Comparative Fit Index (CFI) > 0.95, standardized root mean squared residual (SRMR) < .08, and root mean squared error of approximation (RMSEA) < .06 based on Hu and Bentler(41). SRMR and CFI are sensitive to different types of model misspecification, reporting both provides information on model fit for factor covariances and factor loadings. The χ2 significance test is reported for all models although it was not included in determining a good fit because of the relatively large sample size. Modification indices were examined if necessary to detect parameters that should be freed, including residual variances and covariances, in order to specify a well-fitting model. Standardized path estimates are reported for all models.
Directionality Analysis
A cross-lagged panel analysis(42) was used to investigate the directional relationship between symptom outcomes and both self-efficacy and outcome-expectancy. Six possible models of the relationship between SE, OE, and OASIS were compared to identify the best-fitting model. These models include: 1) only the autoregressive paths 2) the autoregressive paths and paths predicting OASIS from SE; 3) the autoregressive paths and paths predicting OASIS OE; 4) a combination of models 2 and 3, 5) the autoregressive paths and paths predicting SE and OE from OASIS, and 6) a combination of models 4 and 5. There were 7 cross-lagged time-points modeled (between sessions 1 through 8). These 8 sessions were chosen because change in both OASIS, SE, and OE began to plateau following session 8. In addition, by session 9, 45.43% of data was missing either because people completed treatment by this point or due to attrition (see Figure 1). This provides additional justification for only including the first 8 treatment sessions in the analysis. In addition to the autoregressive paths, and cross-lagged paths, all directionality models also included predictive paths from the baseline observation of the measure to each follow-up time-point. Variables or error terms were freely covaried within a session (e.g., session 3 SE with session 3 OE and OASIS). As with all models, various residual covariance structures were tested and a banded Toeplitz residual covariance structure was chosen as the best fitting. By including residual covariances within a time-point as well as residual covariance structures within a variable over time, the independence and homogeneity of variances assumptions of panel analyses are relaxed. The fit statistics are mixed in their diagnosis of model fit for the model that includes prospective paths from SE and OE to OASIS. While some indices are well-within the recommendations (RMSEA = .049, recommended at <.06; CFI=.973, recommended at .95)(41, 43) others were elevated (SRMR=.114, recommended to be less than .08)(41) and the chi-square was significant, chi-square = 384.84, df = 178, p < .001) . This suggests that although the model fits relatively well, there is a small but statistically significant misfit between the model and data, perhaps due to relations between non adjacent sessions (e.g., session 2 and 4) that are not captured.
Preliminary Growth Analyses
Linear growth models for all four outcome variables fit the data well when freely estimating the last two time parameters to capture the plateau of change in outcomes following intervention (see Table 2).
Table 2.
Fit indices and parameters of models
| Outcome measure | χ2 (p value, df) | CFI | SRMR | RMSEA | Slope (std error) | σslope | Intercept (std error) |
σintercept |
|---|---|---|---|---|---|---|---|---|
| BSI | 5.61 (.47, 6) | 1.00 | .02 | .00 | −1.26* (0.07) | 0.93 | 16.31* (.41) | 57.00 |
| ASI | 7.41 (.28, 6) | 1.00 | .03 | .02 | −1.77* (.10) | 2.18 | 29.51* (.63) | 139.20 |
| PHQ-8 | 6.93 (.33, 6) | 1.00 | .02 | .02 | −.88* (.05) | 0.37 | 12.48* (.28) | 26.68 |
| SDS | 9.60 (.14, 6) | 0.99 | .03 | .04 | −1.33* (.06) | 0.65 | 16.68* (.34) | 34.68 |
| OE-Base Model | 57.06 (.00, 27) | 0.99 | .04 | .05 | .13* (.01), −.01* (.00) | .03, .00 | 6.42* (.06) | 1.25 |
| SE-Base Model | 71.23 (.00, 34) | 0.98 | .07 | .05 | .05* (.01) | 0.01 | 6.56* (.05) | 0.87 |
| OASIS Base Model | 71.36 (.00, 37) | 0.98 | .08 | .04 | −.69** (.03) | 0.14 | 7.99** (0.15) | 9.10 |
| OE-Full Model | 306.14 (.00, 221) | 0.99 | .03 | .03 | See Figures 3 and 4 for parameter estimates. | |||
| SE-Full Model | 383.08 (.00, 229) | 0.98 | .06 | .04 | ||||
Note.
p < .05,
p < .01.
The first value of the slope parameter estimate for the OE base model is the linear growth, and the second parameter is the quadratic growth. The same holds true for the σ slope estimates. The BSI, ASI, PHQ-8, and SDS models all used 6 degrees of freedom (df). The SE base model used 34 df, the OE base model used 27 df, and the OASIS base model used 37 df.
In comparing variations of the OE model, quadratic growth with heterogenous residual variances was selected as the best fitting model (see Table 2). The mean linear slope, the instantaneous change at session midpoint, was significant, b = .1346, p < .001 as was the mean quadratic slope, b = -.014, p < .001, indicating that the growth in OE over time slows in later sessions (a slight inverted U shape curve). In comparing variations of the SE model, linear growth with an autoregressive residual structure was the best fit; however, it still did not meet our fit criteria. Based on modification indices, the residual variance at session eight as well as the residual covariance between sessions one and two and seven and eight were freed, and then the model fit well (see Table 2). There was a significant increase in SE over time with the average linear slope b = .054, p < .001, indicating that for each additional session, SE scores were .054 units higher, on average. In comparing variations of the OASIS model, linear growth with an autoregressive residual structure was the best fit and the model fit the data well (see Table 2). There was a significant decrease in OASIS over time with the average linear slope b = -.69, p < .001, indicating that for each additional session, OASIS scores were .69 units lower, on average.
Primary analysis
The outcome variables were BSI, ASI, PHQ-8, and SDS, and the independent variables were SE and OE. Parallel process latent growth models (Parallel LGMs)(44) were used to assess how change in SE and OE predict change in outcomes, while including random intercepts and slopes that are allowed to covary.
To examine the predictive effects of SE and OE, the latent slopes for all outcome variables were separately regressed on the linear slope of SE and the linear and quadratic slope of OE. The latent intercepts of outcomes and predictors were allowed to correlate. The residual covariance structure and handling of time (plateau effect, linear, or quadratic) used in the individual growth models was maintained in the combined parallel LGMs.
Results
Directionality: Outcome-expectancy, Self-efficacy, and OASIS
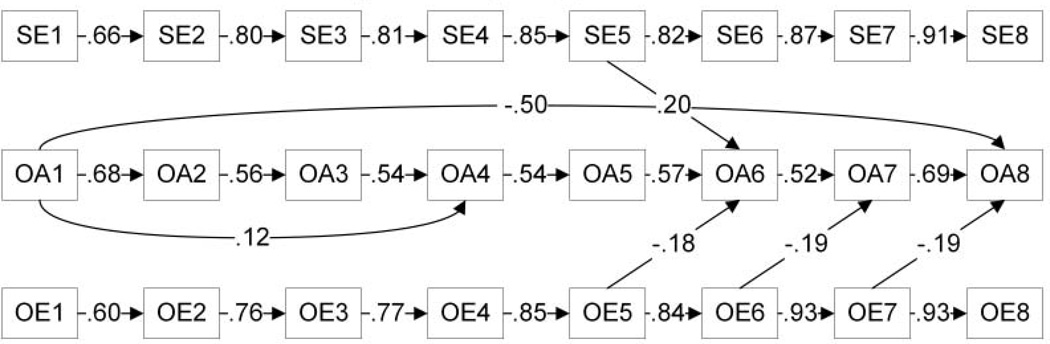
Table 1 reports the results of the directionality analysis. Chi-square difference tests revealed that when prospective paths predicting OASIS at time t from SE at time t-1 (the previous time-point) are added to the autoregressive model (i.e. Model 2), fit is significantly improved (p<.05). Similarly, when paths predicting OASIS at time t from OE at time t-1 are added to the model (i.e., Model 3), fit is significantly improved (p<.0001). Further, when prospective paths predicting OASIS from OE and SE simultaneously are added to the model (i.e., Model 4), fit is significantly improved compared to the autoregressive model (p<.001). In comparison, when paths predicting OE and SE at time t, from OASIS at time t – 1 were added to the autoregressive model (i.e., Model 5), there was not a significant improvement in model fit (p=.698). Model 4, which included prospective paths predicting OASIS from SE and OE simultaneously, was not significantly improved by adding prospective paths predicting SE and OE at time t, from OASIS at time t – 1 (i.e., Model 6, p=.687). An examination of the individual significant cross-lagged paths revealed that as OE increased, OASIS scores decreased (see Figure 2).
Table 1.
Autoregressive and Cross-Lagged Panel Analyses to Examine the Directionality of SE, OE, and OASIS
| SE/OE/OASIS | χ2 | df | Δχ2 from Model 1 | Δχ2 from Model 6 | CFI | SRMR | RMSEA |
|---|---|---|---|---|---|---|---|
| Model 1. Auto | 427.27 | 192 | -- | 53.41** | .969 | .124 | .051 |
| Model 2. SE-->OASIS | 411.72 | 185 | 15.55* | 37.87* | .970 | .121 | .051 |
| Model 3. OE-->OASIS | 397.05 | 185 | 30.21*** | 23.20 | .972 | .113 | .049 |
| Model 4. SE, OE-->OASIS | 384.84 | 178 | 42.42** | 10.99 | .973 | .114 | .049 |
| Model 5. OASIS-->SE, OE | 416.42 | 178 | 10.84 | 42.57** | .969 | .121 | .053 |
| Model 6. Full | 373.86 | 164 | 53.41** | -- | .972 | .111 | .052 |
Note. This table describes the results of the directionality analyses using cross lagged panel models where the predictor predicts the outcome at the following time-point (i.e., x[t – 1] -> y[t]). The analyses answer whether SE predicts OASIS (Model 2), OE predicts OASIS (Model 3), both SE and OE predict OASIS (Model 4), OASIS predicts both SE and OE (Model 5) or they all predict each other (Model 6). Results show that adding paths from SE to OASIS or from OE to OASIS significantly improve fit over the baseline model of no relations between SE, OE, and OASIS over time. Further, OASIS does not predict SE and OE.
p < .05,
p < .01.
See Figure 2 for parameter estimates from Model 4.
Figure 2.
Directionality of OE, SE, and OASIS
Outcomes
The growth models for all of the outcome measures fit the data well (see Table 2). All outcome measures significantly decreased over time, and their intercepts and slopes had significant variance.
Parallel Latent Growth Models
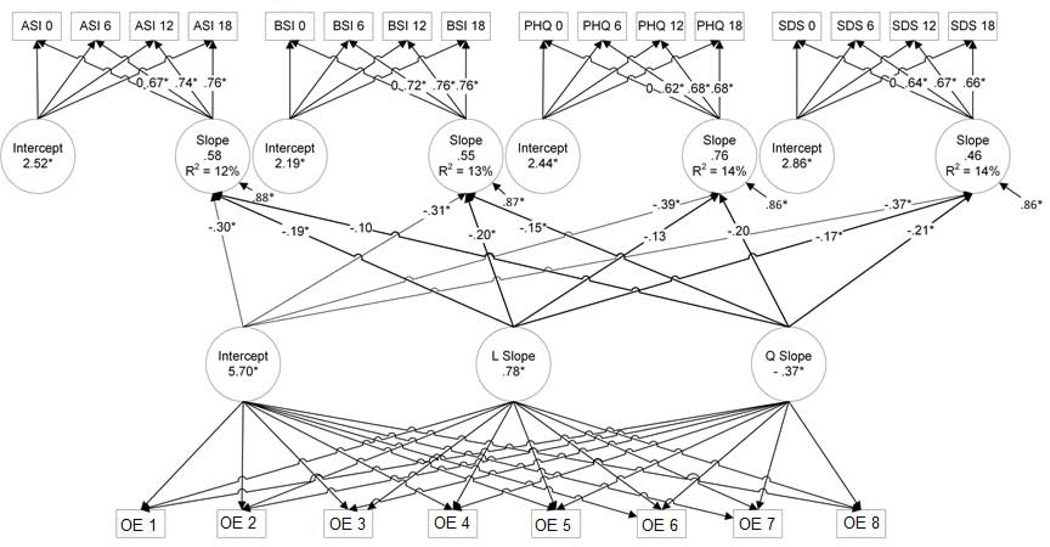
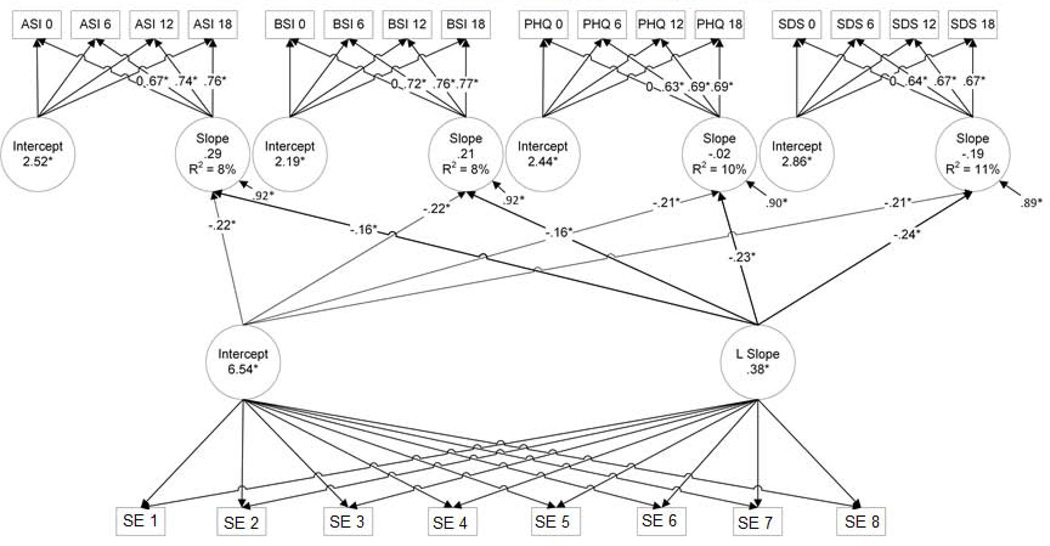
For the parallel latent growth models, individual LGMs were combined. Two variants on this model were fit, one with SE and the other with OE as the predictor of interest. The latent intercepts for OE and SE (centered at the midpoint of the 8 sessions) were correlated with the latent intercepts and predicted the latent slopes of the outcome variables. Also, the latent linear and quadratic slopes for OE were used to predict the latent slopes of the outcome variables (but not the latent intercepts), whereas only the latent linear slope for SE was used to predict the latent slopes of the outcome variables. The focal parts of the model and predictions for these two models are diagrammed in Figures 3 and 4.
Figure 3.
Parallel Latent Growth Model for OE
Figure 4.
Parallel Latent Growth Model for SE
Outcome-expectancy
The prediction model among latent variables for OE is diagrammed in Figure 3. The model fit the data well (see Table 2). None of the correlations between the outcome intercepts and the OE intercept were statistically significant. The latent slopes for all of the outcomes were significantly negatively predicted by the intercept of OE. The latent linear slope of OE significantly predicted the latent slopes of the BSI, ASI, and SDS (see Figure 3) but not the PHQ-8. All of the coefficients were negative, indicating that people who increased more in outcome-expectancy over time tended to decrease more in symptoms over time, and this was over and above their absolute level of outcome-expectancy. Wald tests were used for the main hypotheses that change in OE predicts change in the outcomes. These two degree of freedom tests test whether the effects of the linear and quadratic slopes of OE on the outcomes are both zero. Testing the linear and quadratic effects simultaneously, OE significantly predicted three of the outcomes’ latent slopes: for BSI p = .0069, for ASI p = .0201, for SDS p = .0420, but not PHQ-8 (p=.0904).
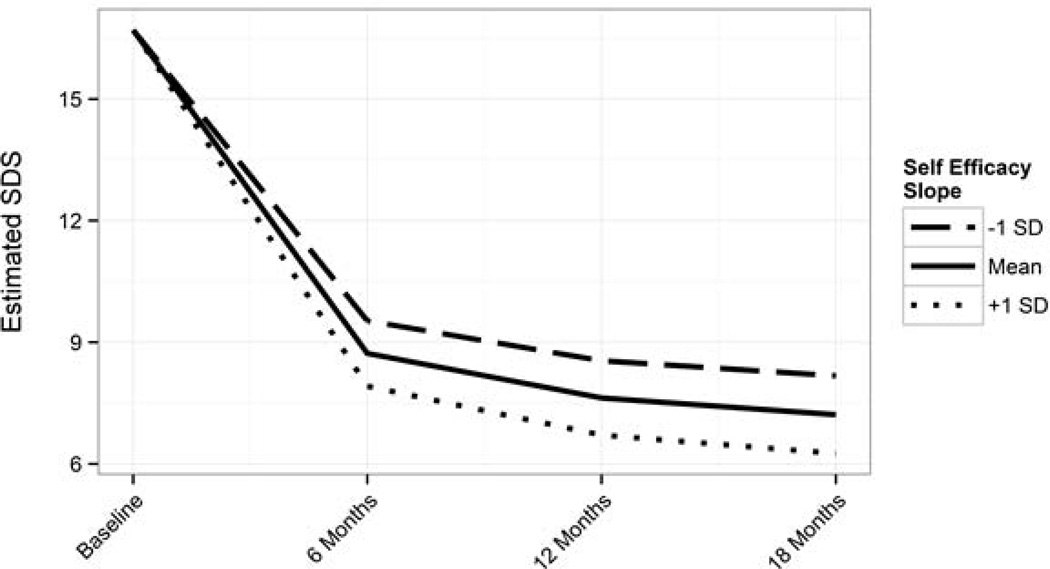
Self-efficacy
The prediction model among latent variables for SE is diagrammed in Figure 4. The model fit the data well (see Table 2). None of the correlations between the outcome intercepts and the SE intercept were statistically significant. The latent slopes for all of the outcomes were significantly negatively predicted by the intercept of SE. The linear slope of SE significantly predicted the slopes of all of the outcome variables (see Figure 4). For example, the slope of SE predicted the slope of ASI (β = −.16, p < .05) indicating that for a 1 standard deviation unit higher increase in SE per treatment session, ASI would decrease .16 standard deviation units more per month. See Figure 5 for an example graph of the effect of different slopes of SE on one of the outcome measures (SDS).
Figure 5.
Graph of the estimated Sheehan Disability Scale (SDS) scores for different self-efficacy (SE) slopes
Discussion
Self-efficacy and outcome-expectancy have a documented relationship to treatment outcome dating back to the 1970s(1). However, the extent to which changes in these constructs predict changes in outcome, a major premise of self-efficacy theory, has received very little empirical attention. To fill this gap in the literature, the current study addressed the degree to which change in these constructs throughout the course of treatment predicted symptom and functioning outcomes over 18 months in a large sample with multiple anxiety disorders. This study also attempted to clarify the directionality of the relationship between self-efficacy, outcome-expectancy, and symptoms/functioning.
The results of the directionality analysis revealed that the best model of outcome-expectancy and symptom/functioning levels included predictive paths from expectancy to symptom levels but not the converse. A similar pattern emerged for the relationship between self-efficacy and symptom/functioning levels. Therefore, there is evidence that both outcome-expectancy and self-efficacy are important in the prediction of symptoms and related functioning, yet the latter are not predictors of self-efficacy or outcome-expectancy. It is important to keep in mind that some of the fit indices for this model were outside of the recommended ranges. Although we explored a variety of possible relationships between these variables and their error terms as well as modification indices, no clear better-fitting model emerged. One possibility is that self-efficacy, outcome-expectancy, and symptom/functioning levels are dependent upon more than simply their baseline ratings and prior session ratings. These ratings may also be influenced by sessions that were two or three sessions prior to current session. It is also possible that due to the nature of the CALM study, in which the module that the ACS implemented on a particular session was more variable than in a traditional CBT manual, there may have emerged a less clear pattern of predictability in self-efficacy, outcome-expectancy, and symptoms during treatment. Further, it is difficult to achieve good model fit with eight time-points across three measures in a parsimonious model. Despite these limitations, there is still value in understanding the general relationships among these variables. The data show the important predictive power of self-efficacy and outcome-expectancy on symptom levels and functioning (measured via the OASIS) throughout treatment. It is recommended that future researchers attempt to model the relationships between these variables in other samples to understand their predictive pattern throughout the course of treatment.
Next, outcome-expectancy and self-efficacy were examined as predictors of long-term symptom and functioning. Consistent with prior research(7, 13), higher levels of outcome-expectancy and self-efficacy were associated with superior treatment outcomes across multiple measures. This implies that individuals with low self-efficacy and low outcome-expectancy may benefit from additional therapeutic strategies designed to enhance their expectancies, though further research is needed to confirm that directly manipulating expectancies and self-efficacy leads to an added benefit.
In addition, the results indicated that outcome-expectancy and self-efficacy change over the course of treatment, and that such change significantly predicts symptom and functioning outcome improvement over 18 months controlling for the absolute level of outcome-expectancy and self-efficacy. That is, independent of whether a patient has high or low outcome-expectancy, the amount of increase in outcome-expectancy during treatment predicts the amount of decrease in symptoms and increase in functioning up to 18 months later. A similar pattern was found for self-efficacy. Possible reasons why outcome expectancies and self-efficacy predict beneficial effects include increased motivation to engage in therapeutic activities(45), such as exposure and cognitive restructuring, that lead to greater improvements in symptoms and functioning. Additionally, increases in outcome expectancies and self-efficacy may provide a sense of control that directly lessen symptoms and distress(46, 47).
Together, these data point to the value of strategies that directly target self-efficacy and outcome-expectancy throughout treatment. Strategies for raising outcome-expectancy include psychoeducation about positive response rates of a particular treatment for patients with the same disorder(48), as well as convincing treatment rationales and reminders of positive changes an individual has achieved thus far in treatment. These strategies may be especially helpful as treatment becomes more challenging (e.g., during a crisis, when approaching more anxiety-provoking stimuli, following a set-back in treatment). Also, motivational interviewing techniques such as discussing the pros and cons of behavioral change, have been shown to increase outcome-expectancy(49).
Bandura(4) argued that performance accomplishments are the most powerful strategy for enhancing self-efficacy. Performance accomplishment (e.g., approaching and coping with a previously avoided situation) is likely to impact outcome expectancies as well. Thus, behavioral mastery during exposure therapy for anxiety disorders may be particularly effective in raising both self-efficacy and outcome-expectancy. Also, therapist modeling of approach to feared stimuli and verbal encouragement from the therapist about confidence in the client’s ability to complete treatment can improve self-efficacy(50). Similarly, discussions with clients about the requirement for courage during exposure and therapist belief in their ability to be courageous may be beneficial. Additional methods for enhancing self-efficacy from the Motivational Interviewing literature include actively praising small successes, reframing perceived failures as intermediate successes, and preventing or removing barriers through problem solving skills(51).
Strengths of this study include the large sample size and multiple measures of predictors and outcomes. It is the only study of which we are aware that simultaneously examines session by session changes in outcome-expectancy and self-efficacy to investigate their relationship to outcome over an extended time-period. In addition, this study takes advantage of an analytic approach that allows for a thorough investigation of the relationships between treatment outcome and both self-efficacy and outcome-expectancy.
Limitations include reliance on single-items to measure self-efficacy and outcome-expectancy, which could be detrimental to the ability to capture these constructs accurately. However, research within smoking cessation and substance abuse literature has demonstrated equal or superior predictive validity of one-item measures of self-efficacy compared to multi-item measures(52, 53). Further, each item was assessed eight times and overall levels and change over time were analyzed, reducing the impact of measurement error at any given time-point. A second limitation is that the treatment represented a combination of CBT, medication management or both. Thus, it is not possible to attribute changes in expectancies or symptoms/functioning specifically to one treatment strategy over another. Third, more research needs to be done to understand the directionality between outcome-expectancy and self-efficacy. Fourth, the results only apply to clients with an anxiety disorder as their principal diagnosis. Therefore, it is not clear whether the results would translate to other disorders. Fifth, therapeutic alliance was not measured for the entire sample and thus was not analyzed herein; other research has shown that therapeutic alliance drives change in self-efficacy and outcome-expectancy, which then predicts outcome(54). Sixth, consistent with epidemiology research on the higher prevalence of anxiety in women(55) this sample included more women (71.1%). Therefore, these patterns of results observed may be particularly relevant to females. Seventh, a plateau effect was observed following session 8, and patients were given the choice of switching treatment modalities after 10–12 weeks if their symptoms were not in remission. It is possible that if patients were given the opportunity to switch treatments, their trajectories may have differed. Given that many patients completed treatment prior to the opportunity to switch treatment modalities, this hypothesis could not be further explored. Finally, inadequate power prevented a detection of differences in the pattern of results based on principal anxiety disorder. However, it is possible that future research may be able to address this research question.
Overall, these results indicate that not only are levels of self-efficacy and outcome-expectancy important, changes in self-efficacy and outcome-expectancy throughout treatment play a role in influencing long term outcomes for anxiety disorders. The results indicate that assessing the change in brief single-item assessments of treatment-related self-efficacy or outcome-expectancy during treatment is a useful prognostic indicator for long-term outcome and can help identify patients who may require additional support. They also indicate that augmentation of beliefs that a treatment can work and of beliefs that patients are capable of successfully completing treatment are strong predictors of treatment outcome and should be investigated as key targets of interventions.
Supplementary Material
Acknowledgments
This work was supported by the following National Institute of Mental Health grants: U01 MH070018, U01 MH058915, U01 MH057835, UO1 MH057858, U01 MH070022, K24 MH64122, K24 MH065324, and NIGMS T32GM084903 fellowship to Wiley.
Appendix
Appendix I: See file entitled “AppendixI_DepressionandAnxiety”
Appendix II.
Table 1.
Treatment received within the Intervention
| Participants who received at least 1 intervention contact | 482 (95%) |
| Mean CBT visits (SD) | 7.0 (4.1) |
| Median CBT contacts | 8 |
| Mean medication visits (SD) | 2.24 (3.57) |
| Median medication visits | 1 |
| Patients who only received CBT only | 166 (34%) |
| Patients who received medication management only | 43 (9%) |
| Patients who received CBT and medication management | 273 (57%) |
| Patients who completed all visits by 6 months | 424 (88%) |
Note. Table 1 displays important details the number of patients who received CBT, medication management, or both, as well as other key study characteristics.
Appendix III: See file entitled “Appendix III”
References
- 1.Bandura A. Social learning theory. New Jersey: Prentice-Hall; 1977. [Google Scholar]
- 2.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3(4):257–260. [Google Scholar]
- 3.Bandura A. Self-efficacy mechanism in human agency. American Psychologist. 1982;37(2):122–147. [Google Scholar]
- 4.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 5.Bandura A, Reese L, Adams NE. Microanalysis of action and fear arousal as a function of differential levels of perceived self-efficacy. Journal of Personality and Social Psychology. 1982;43:5–21. doi: 10.1037//0022-3514.43.1.5. [DOI] [PubMed] [Google Scholar]
- 6.Maddux JE, Sherer M, Rogers RW. Self-efficacy expectancy and outcome expectancy: Their relationship and their effects on behavioral intentions. Cognitive Therapy and Research. 1982;6(2):207–211. [Google Scholar]
- 7.Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1993;61:611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- 8.Chambless DL, Tran GQ, Glass CR. Predictors of Response to Cognitive-Behavioral Group Therapy for Social Phobia. Journal of Anxiety Disorders. 1997;11:221–240. doi: 10.1016/s0887-6185(97)00008-x. [DOI] [PubMed] [Google Scholar]
- 9.Safren SA, Heimberg RG, Juster HR. Clients' Expectancies and Their Relationship to Pretreatment Symptomatology and Outcome of Cognitive- Behavioral Group Treatment for Social Phobia. Journal of Consulting and Clinical Psychology. 1997;65:694–698. doi: 10.1037//0022-006x.65.4.694. [DOI] [PubMed] [Google Scholar]
- 10.Price M, Anderson P, Henrich CC, Rothbaum BO. Greater Expectations: Using Hierarchical Linear Modeling to Examine Expectancy for Treatment Outcome as a Predictor of Treatment Response. Behavior Therapy. 2008;39(4):398–405. doi: 10.1016/j.beth.2007.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sotsky SM, Glass DR, Shea T, Pilkonis PA, Collins F, Elkin I, et al. Patient predictors of response to psychotherapy and pharmacotherapy: Findings in the NIMH Treatment of Depression Collaborative Research Program. American Journal of Psychiatry. 2006;148:997–1008. doi: 10.1176/ajp.148.8.997. [DOI] [PubMed] [Google Scholar]
- 12.Stewart-Williams S, Podd J. The placebo effect: Dissolving the expectancy versus conditiong debate. Psychological Bulletin. 2004;130:324–340. doi: 10.1037/0033-2909.130.2.324. [DOI] [PubMed] [Google Scholar]
- 13.Tate SR, Wu J, McQuaid JR, Cummins K, Shrive C, Krenek M, et al. Comorbidity of Substance Dependence and Depression: Role of Life Stress and Self-Efficacy in Sustaining Abstinence. Psychology of Addictive Behaviors. 2008;22:47–57. doi: 10.1037/0893-164X.22.1.47. [DOI] [PubMed] [Google Scholar]
- 14.Kuusisto K, Knuuttila V, Saarnio P. Clients' self-efficacy and outcome expectations: Impact on retention and effectiveness in outpatient substance abuse treatment. Addictive Disorders & Their Treatment. 2011;10:157–168. doi: 10.1017/S1352465810000846. [DOI] [PubMed] [Google Scholar]
- 15.Gordon MS, Tonge B, Melvin GA. Outcome of adolescent depression: 6 months after treatment. Australian and New Zealand Journal of Psychiatry. 2011;45:232–239. doi: 10.3109/00048674.2010.538838. [DOI] [PubMed] [Google Scholar]
- 16.Powers MB, Smits JAJ, Whitley D, Bystritsky A, Telch MJ. The effect of attributional processes concerning medication taking on return of fear. Journal of Consulting and Clinical Psychology. 2008;76:478–490. doi: 10.1037/0022-006X.76.3.478. [DOI] [PubMed] [Google Scholar]
- 17.Bootzin R, Lick J. Expectancies in therapy research: interpretive artifact or mediating mechanism? Journal of Consulting and Clinical Psychology. 1979;47:852–855. [PubMed] [Google Scholar]
- 18.Newman MG, Fisher AJ. Expectancy/credibility change as a mediator of cognitive behavioral therapy for generalized anxiety disorder: mechanism of action or proxy for symptom change? International Journal of Cognitive Therapy. 2010;3:245–261. doi: 10.1521/ijct.2010.3.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bouchard S, Gauthier J, Nouwen A, Ivers H, Vallières A, Simard S, et al. Temporal relationship between dysfunctional beliefs, self-efficacy and panic apprehension in the treatment of panic disorder with agoraphobia. Journal of Behavior Therapy and Experimental Psychiatry. 2007;38(3):275–292. doi: 10.1016/j.jbtep.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Black JJ, Tran GQ, Goldsmith AA, Thompson RD, Smith JP, Welge JA. Alcohol expectancies and social self-efficacy as mediators of differential intervention outcomes for college hazardous drinkers with social anxiety. Addictive Behaviors. 2012;37(3):248–255. doi: 10.1016/j.addbeh.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Bandura A, Adams NE. Analysis of self-efficacy theory of behavioral change. Cognitive Therapy and Research. 1977;1(4):287–310. [Google Scholar]
- 22.Hoffart A. Cognitive and guided mastery therapy of agoraphobia: Long-term outcome and mechanisms of change. Cognitive therapy and research. 1998;22:195–207. [Google Scholar]
- 23.Roy-Byrne P, Craske MG, Sullivan G, Rose RD, Edlund MJ, Lang AJ, et al. Delivery of Evidence-Based Treatment for Multiple Anxiety Disorders in Primary Care. JAMA: The Journal of the American Medical Association. 2010;303(19):1921–1928. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craske MG, Stein MB, Sullivan G, Bystritsky A, Rose RD, Lang AJ, et al. Disorder-specific impact of coordinated anxiety learning and management treatment for anxiety disorders in primary care. Arch Gen Psychiatry. 2011;68:378–388. doi: 10.1001/archgenpsychiatry.2011.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 26.Craske MG, Rose RD, Lang AJ, Welch SS, Campbell-Sills L, Sullivan G, et al. Computer-assisted delivery of cognitive behavioral therapy for anxiety disorders in primary-care settings. Depression and Anxiety. 2009;26:235–242. doi: 10.1002/da.20542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rose RD, Lang AJ, Welch SS, Campbell-Sills L, Chavira DA, Sullivan G, et al. Training primary care staff to deliver a computer-assisted cognitive-behavioral therapy program for anxiety disorders. General Hospital Psychiatry. 2011;33:336–342. doi: 10.1016/j.genhosppsych.2011.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campbell-Sills L, Norman SB, Craske MG, Sullivan G, Lang AJ, Chavira DA, et al. Validation of a brief measure of anxiety-related severity and impairment: the Overall Anxiety Severity and Impairment Scale (OASIS) Journal of Affective Disorders. 2009;112:92–101. doi: 10.1016/j.jad.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13(03):595–605. [PubMed] [Google Scholar]
- 30.Derogatis LR. Symptom Checklist-90-R (SCL-90-R): Administration, scoring, and procedures manual. Minneapolis, MN: NCS; 1994. [Google Scholar]
- 31.Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency, and the prediction of fearfulness. Behavior research and therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 32.Peterson RA, Heilbronner RL. The anxiety sensitivity index: Construct validity and factor analytic structure. Journal of Anxiety Disorders. 1987;1(2):117–121. [Google Scholar]
- 33.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of Mental Disorders. Patient Health Questionnaire. JAMA: The Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:601–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheehan DV. The anxiety disease. New York: Scribner; 1983. [Google Scholar]
- 36.Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the sheehan disability scale. The international journal of psychiatry in medicine. 1997;27:93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- 37.Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford, UK: Oxford University Press; 2003. [Google Scholar]
- 38.Hallquist M, Wiley JF. Mplus Automation: Automating Mplus Model Estimation and Interpretation (Version 0.6-1) 2013 [Google Scholar]
- 39.Enders CK, Bandalos DL. The Relative Performance of Full Information Maximum Likelihood Estimation for Missing Data in Structural Equation Models. Structural Equation Modeling. 2001;8:430–457. [Google Scholar]
- 40.Muthén LK, Muthén BO. Mplus User's Guide. Seventh Edition ed. Los Angeles, CA: Muthén & Muthén; pp. 1998–2012. [Google Scholar]
- 41.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- 42.Martens MP, Haase RH. Advanced applications of structural equation modeling in counseling psychology research. The Counseling Psychologist. 2006;34:806–838. [Google Scholar]
- 43.Bentler PM. EQS: Structural equations program manual. Encino, CA: Multivariate Software; 1995. [Google Scholar]
- 44.Cheong J, MacKinnon DP, Khoo ST. Investigation of Mediational Processes Using Parallel Process Latent Growth Curve Modeling. Structural Equation Modeling: A Multidisciplinary Journal. 2003;10:238–262. doi: 10.1207/S15328007SEM1002_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Seligman MEP. Helplessness: On depression, development, and death. San Francisco: Freeman; 1975. [Google Scholar]
- 46.Starr MD, Mineka S. Determinants of fear over the course of avoidance learning. Learning and Motivation. 1977;8:332–350. [Google Scholar]
- 47.Barlow DH. Anxiety and its disorders. New York: Guilford; 1988. [Google Scholar]
- 48.Greenberg RP, Constantino MJ, Bruce N. Are patient expectations still relevant for psychotherapy process and outcome? Clinical Psychology Review. 2006;26(6):657–678. doi: 10.1016/j.cpr.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 49.Westra HA, Dozois DJA. Preparing clients for cognitive behavioral therapy: a randomized pilot study of motivational interviewing for anxiety. Cognitive Therapy and Research. 2006;30:481–498. [Google Scholar]
- 50.Dupree K, Jones C, Burckhardt S, Bennett JA. Motivational Interviewing May Encourage Exercise in Persons With Fibromyalgia by Enhancing Self Efficacy. Arthritis & Rheumatism (Arthritis Care & Research) 2004;51:864–867. doi: 10.1002/art.20684. [DOI] [PubMed] [Google Scholar]
- 51.Chou CC, Ditchman N, Pruett SR, Chan F, Hunter C. Applications of social cognitive theory in psychosocial interventions. New York: Springer; 2009. [Google Scholar]
- 52.Gwaltney CJ, Metrik J, Kahler CW, Shiffman S. Self-efficacy and smoking cessation: a meta-analysis. Psychology of Addictive Behaviors. 2009;23:56–66. doi: 10.1037/a0013529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hoeppner BB, Kelly JF, Urbanoski KA, Slaymaker V. Comparative utility of a single-item versus multiple-item measure of self-efficacy in predicting relapse among young adults. Journal of Substance Abuse Treatment. 2011;41:305–312. doi: 10.1016/j.jsat.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abouguendia M, Joyce AS, Piper WE, Ogrodniczuk JS. Alliance as a mediator of expectancy effects in short-term group psychotherapy. Group dynamics: theory, research, and practice. 2004;8:3–12. [Google Scholar]
- 55.McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender difference in Anxiety Disorders: Prevalence, Course of Ilness, Comorbidity, and Burden of Illness. Journal of Psychiatry Research. 2011;45:1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.