Abstract
Objective:
Multiple studies show that behavioral couples therapy (BCT) is more efficacious than individually-based therapy (IBT) for substance use and relationship outcomes among men with alcohol use disorder (AUD). The present study compared BCT with IBT for women with AUD.
Method:
Participants were women with AUD (N = 105) and their male partners without SUD. Participants were mostly White and in their forties. Women were randomized to equally intensive treatments consisting of either BCT plus 12-step-oriented IBT or IBT only. Primary outcomes included: Timeline Followback Interview percentage days abstinent (PDA) and Inventory of Drug Use Consequences measure of substance-related problems. Secondary outcomes included: Dyadic Adjustment Scale (DAS), Relationship Happiness Scale (RHS), and Revised Conflict Tactics Scales measure of intimate partner violence (IPV). Outcome data were collected at baseline, post-treatment, and quarterly for 1-yr follow-up.
Results:
Compared to IBT only, BCT plus IBT had significantly better primary outcomes of higher PDA and fewer substance-related problems during the 1-yr follow-up period. Compared to IBT only, BCT had significantly higher male RHS during the 1-yr follow-up. Women with lower pretreatment DAS had significantly higher DAS following BCT versus IBT, and there was an increasing advantage for BCT on female DAS over the follow-up. IPV was significantly reduced from pretreatment to follow-up, with no differences between treatment conditions.
Conclusion:
Results showed that BCT for women with AUD was more efficacious than IBT in reducing substance use and substance-related problems and improving partner relationships.
Keywords: female alcoholism, couples therapy, treatment outcomes
There has been more research conducted on treatments for alcohol use disorder (AUD) among men than among women (Swearingen, Moyer, & Finney, 2003). This may be due to higher prevalence of AUD among men, as the National Epidemiologic Survey on Alcohol and Related Conditions estimates that approximately 17.5% of men versus 8.0% of women will exhibit lifetime alcohol dependence (Kahn et al., 2013). Although AUD may be less prevalent among women, women with AUD may suffer more adverse consequences than men as a result of their drinking. Women with AUD are shown to exhibit a later onset of AUD, and more quickly progress to serious AUD problems (Diehl et al., 2007). In comparison to men who are heavy drinkers, women who are heavy drinkers are prone to exhibit serious medical problems, such as liver cirrhosis (Rehm et al, 2010), and have higher mortality rates (Jacques-Lopez et al., 2001). Therefore, it is important for research to continue to progress in determining the forms of treatment that are most efficacious for women with AUD.
Relationship concerns appear to be especially prominent in women’s drinking behaviors and seeking help for AUD. In comparison to men, women are more unhappy in their couple relationships, and they are more likely to drink in response to these interpersonal stressors (Kelly, Halford & Young, 2002). Consistent with these findings, Lemke, Brennan, and Schultte (2007) found relationship problems and emotional distress over these problems were linked to relapse for alcoholic women. Finally, some women entering AUD treatment perceive a lack of partner support and are uncertain about the future of their relationships (McCrady, Epstein, Cook, Jensen & Ladd, 2011). Problems such as these with women’s relationship partners present challenges for women who are seeking help for AUD.
Given the prominent role of interpersonal factors in women’s AUD problems, women with AUD might benefit from treatments that simultaneously address relationship issues, while working to promote sobriety from alcohol and other drugs. One therapy that has the goals of simultaneously promoting sobriety and improving relationships is behavioral couples therapy (BCT). BCT is the most well-researched, family-based therapy for adults with AUD (Meis et al., 2013) and is shown to exhibit medium effect size advantages over individually-based treatment (IBT; Powers, Vedel, & Emmelkamp, 2008). However, the preponderance of studies examining the efficacy of BCT have involved couples in which the male partner has AUD, while the female partner does not exhibit a substance use disorder.
To date, there have been only two randomized, controlled clinical trials testing the efficacy of BCT versus IBT for women with AUD. Each of these studies used a different manualized version of BCT. The first study by Fals-Stewart, Birchler, and Kelly (2006) used the version of BCT that is described by O’Farrell and Schein (2011). This version of BCT uses a recovery contract to define and teach the couple specific behaviors to promote sobriety, while simultaneously teaching the couple skills to improve their relationship. In the Fals-Stewart et al (2006) study, women were recruited from a substance use treatment program and were mostly of lower-to-middle class socioeconomic status. Women were assigned to receive one of three equally intensive interventions: BCT plus IBT, IBT only, or a psychoeducational control condition. In comparison to the other conditions, women who received BCT exhibited greater abstinence from substances, fewer substance-related problems, better relationship satisfaction, and less intimate partner violence (IPV) during the twelve months following treatment.
The second study by McCrady et al. (2009) tested the efficacy of a stand-alone version of BCT versus IBT only. This study followed the approach described by McCrady and Epstein (2008), which emphasizes teaching the partner skills for coping with alcohol-related situations, the couple relationship enhancement skills, and the AUD patient individual coping skills for high-risk situations for drinking. Women were primarily recruited from the community mainly by advertising and were mostly of middle-to-upper class socioeconomic status. McCrady et al. (2009) found greater reductions in drinking behaviors in BCT versus IBT, and these differences were maintained during the twelve months following treatment. However, McCrady et al. did not examine differences between the BCT and IBT treatments on alcohol-related problems, or on relationship satisfaction or IPV outcomes.
The present study compared BCT with IBT for women with AUD. We sought to replicate and extend the findings from the two previous randomized studies of BCT among women with AUD. The present study improved over one or both prior studies in the following ways. First, it included a multifaceted outcome assessment of both drinking and relationship domains targeted by BCT. Second, all study patients met criteria for alcohol dependence (not abuse). Third, the 12-step oriented IBT treatment used as a comparison group has established utility and face validity for use in U.S. programs. Fourth, BCT and the comparison treatment were equated for number and length of sessions. Fifth, most measures were collected at multiple time points during the follow-up period. Finally, the analyses used tested not only whether BCT had an overall mean advantage over IBT but also whether BCT and IBT differed with regard to trajectories of change during the follow-up period.
In the present study, women with AUD were recruited from a substance abuse treatment program. They were randomly assigned to equally intensive treatments consisting of either (a) BCT plus 12-step oriented IBT or (b) IBT only. Outcome data were collected at baseline, post-treatment, and at 3-, 6-, 9- and 12-month follow-up. We tested the predictions that women AUD patients who received BCT plus IBT, as compared to those who got IBT only, would do better on primary outcomes of more days abstinent from alcohol and drugs and fewer substance-related problems. We also predicted that BCT plus IBT would do better than IBT only on secondary outcomes of higher relationship satisfaction and less IPV.
Method
Institutional review boards at Harvard Medical School and at VA Boston approved this study.
Participants
Participants were 105 women with alcohol dependence and their male relationship partners.1 They were recruited from patients seeking treatment at a large SUD treatment center in the northeastern U.S. from May 2006 to December 2009. Eligibility criteria were as follows: (1) both partners were between 18 and 65 years of age; (2) women met past 12 month alcohol dependence diagnosis according to the Structured Clinical Interview for the DSM-IV (SCID; First, Spitzer, Gibbons & Williams, 1996) and comorbid drug use disorders also were permitted; (3) women consumed alcohol in the 60 days prior to the study and consumed non-beverage alcohol products (e.g., mouthwash) on no more than 20% of drinking occasions during this time; (4) women's primary drug of abuse was alcohol according to an algorithm described in Fals-Stewart (1996); (5) women did not exhibit current alcohol or drug dependence that required inpatient treatment or medical detoxification, with the understanding that after completing needed detoxification or inpatient treatment they may be eligible for the study; (6) during study-based treatment, women were agreeable to the goal of abstinence, and willing to forgo other professional alcoholism counseling other than treatment required for a clinical emergency or to address clinical deterioration or self-help meeting attendance; (7) other than nicotine dependence, men did not meet past 12 month diagnosis for a substance use disorder according to the SCID (First et al., 1996); (8) neither partner met criteria for psychotic disorder according to the SCID (First et al., 1996); (9) neither partner at imminent risk for homicide or suicide; (10) couple married for at least 1 year or living together in a stable common-law relationship for at least 2 years; (11) couple lived apart for no more than 4 out of the past 12 months; (12) couple had no immediate plans to separate or divorce; (13) on brief IPV questions in the study screening interview, couple denied severe IPV (i.e., that which had resulted in injury) as occurring in the past 3 years on days when both partners were not using substances, 2 and female patient did not report fear that couples therapy might put her at risk for violence.
Participants were, on average, in their forties (women M = 44.42, SD = 8.08; men M = 47.68, SD = 8.40) with about 14 years of education (women M = 14.39, SD = 2.23; men M = 14.44, SD = 2.34), and had been married or cohabitating for around 16 years (M = 15.96, SD = 9.72). Nearly half (48.6%) of the couples had children between the ages of 6 to 16. Participants’ ethnicity was mostly White (women = 97.1%, men = 94.1%). Women’s annual income in thousands of dollars (M = 31.79, SD = 29.43) was descriptively lower than their male partners (M = 80.44, SD = 80.64). Over half of the women were employed full- (38.1%) or part-time (19.0%). Women reported an average of 13.32 years of problematic alcohol use (SD = 10.19). A minority of women had a lifetime co-occurring drug use disorder diagnosis (11.4%). Women’s total scores on the Inventory of Drug Use Consequences - Lifetime (M = 32.82, SD = 5.88) were similar to those previously found among women entering outpatient substance use treatment (e.g., Tonigan & Miller, 2002). Finally, participants assigned to BCT did not differ from those in IBT on the variables just described (all ps ≥ .22; see Table 1).
Table 1.
Pretreatment Characteristics for Participants by Treatment Condition
| IBT (n = 53) | BCT (n = 52) | |||
|---|---|---|---|---|
| Characteristic | M(SD) or No (%) | M(SD) or No (%) | t or χ2 | p |
| Female age | 44.2 (8.6) | 44.6 (7.6) | 0.23 | 0.816 |
| Female education | 14.4 (2.2) | 14.5 (2.2) | 0.11 | 0.916 |
| Male age | 47.2 (8.8) | 48.2(8.1) | 0.65 | 0.520 |
| Male education | 14.4 (2.5) | 14.4 (2.2) | 0.11 | 0.914 |
| Years married or cohabiting | 16.6 (9.1) | 15.3 (10.3) | 0.68 | 0.497 |
| Child age 6-16 living in home | 26 (49) | 25 (48) | 0.01 | 0.450 |
| Annual female income (thousands) | 28.9 (28.7) | 34.7 (30.1) | 1.02 | 0.310 |
| Annual male income (thousands) | 84.4 (81.0) | 76.4 (80.9) | 0.51 | 0.614 |
| Female ethnicity: | 3.03 | 0.220 | ||
| White | 50 (94) | 52 (100) | ||
| African-American | 1 (2) | 0 | ||
| Hispanic | 0 | 0 | ||
| Asian | 0 | 0 | ||
| Other | 2 (4) | 0 | ||
| Male ethnicity: | 4. 03 | 0.258 | ||
| White | 48 (91) | 50 (96) | ||
| African-American | 3 (6) | 1 (2) | ||
| Hispanic | 2 (4) | 0 | ||
| Asian | 0 | 1 (2) | ||
| Other | 0 | 0 | ||
| Female employment: | 5.76 | 0.920 | ||
| Not employed | 16 (30) | 17 (33) | ||
| Employed full-time | 18 (34) | 22 (42) | ||
| Employed part-time | 11 (21) | 9 (17) | ||
| Homemaker | 4 (8) | 3 (6) | ||
| Other | 4 (8) | 1 (2) | ||
| Female with alcohol dependence dx | 53 (100) | 52 (100) | -- | -- |
| Years female problematic alcohol use | 13.7 (9.6) | 12.9 (10.8) | 0.40 | 0.692 |
| Female other substance use dx: | ||||
| Sedative/Hypnotic/Anxiolytics | 5 (9) | 3 (6) | 0.51 | 0.479 |
| Cannabis | 2 (4) | 2 (4) | 0.00 | 0.985 |
| Stimulants | 0 | 0 | -- | -- |
| Opiates | 3 (6) | 2 (4) | 0.19 | 0.663 |
| Cocaine | 2 (4) | 3 (6) | 0.23 | 0.631 |
| Hallucinogens | 0 | 0 | -- | -- |
| Other | 0 | 0 | -- | -- |
| Female InDUC-Lifetime total score | 32.57 (5.38) | 33.06 (6.39) | -- | -- |
Note. IBT = individual-based treatment. BCT = behavioral couples therapy.
Measures
Unless otherwise specified, measures were administered to both partners at pre- and post-treatment and then again at 3-, 6-, 9-, and 12-months following treatment.
Timeline Followback Interview (TLFB; Sobell & Sobell, 1996)
The TLFB uses a calendar and other memory aids to gather retrospective information about substance use behaviors over a specified period of time. The TLFB, which is widely used in alcoholism treatment research, has shown test-retest and patient-collateral correlations of ≥ .80 for alcohol and illicit drugs (Sobell & Sobell, 1996). Both partners completed the TLFB with reference to the woman's behaviors. Percentage days abstinent (PDA) was calculated by dividing the number of days on which the woman was not in a hospital or jail for alcohol-related reasons and she remained abstinent from alcohol and other drugs by the total days during a given time period. To reduce possible underreporting of women's substance use, we used the lowest reported PDA when both partners' data were available. When data was available from only one partner, we used the available partner's report.
Inventory of Drug Use Consquences (InDUC; Tonigan & Miler, 2002)
The InDUC is a 50-item self-report measure of adverse consequences of alcohol and drug use. The InDUC is shown to exhibit excellent test-retest reliability, good to excellent internal reliability, acceptable convergent validity, and good sensitivity to change in response to treatment (Tonigan & Miller, 2002). Both partners responded to the InDUC with reference to consequences of the woman's alcohol and drug use. At baseline, the current (past 3 months) and lifetime versions of the InDUC were both administered. At post-treatment, the InDUC referenced the time during treatment, and the InDUC referenced the prior 3 months during the other follow-up assessments. To reduce possible underreporting of women's substance-related problems, we used the highest report when both partners provided responses to an InDUC item. When data was available from only one partner on an InDUC item, we used the available partner's report.
Dyadic Adjustment Scale (DAS; Spanier, 2001)
The DAS is a widely used 32-item self-report measure of overall relationship adjustment. The DAS exhibits excellent internal and test-retest reliability as well as strong concurrent and criterion-related validity in differentiating distressed from non-distressed couples (Spanier, 2001).
Relationship Happiness Scale (RHS; Smith & Meyers, 2004)
On the RHS, respondents rate relationship satisfaction in 10 areas using Likert scales. The RHS was adapted from the Marital Happiness Scale (Azrin, Naster, & Jones, 1973). The RHS is shown to be sensitive to changes in response to treatment (e.g., Miller, Meyers, & Tonigan, 1999), but we are not aware of other psychometric information on the RHS.
Revised Conflict Tactics Scales (CTS2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996)
The 12 items comprising the physical assault scale from the CTS2 were used to measure intimate partner violence (IPV) during the prior 12 months. The CTS2 demonstrates acceptable internal reliability and good factor and criterion validity (Straus et al., 1996). Following procedures described by Straus et al. (1996), the weighted frequency scores were used to assess each partner's IPV. To address possible underreporting of IPV, we followed the suggestion to use whichever partner frequency was highest in reporting on each of the CTS2 items for a given partner (Straus et al., 1996). The CTS2 was administered twice, once at baseline and then again at the 12-month follow-up assessment.
Client Satisfaction Questionnaire-8 (CSQ-8; Attkinsson & Greenfield, 2004)
The CSQ-8 is an 8 item measure that was used to assess satisfaction with study-based treatment. Since some male partners were not directly involved with the study-treatment, the CSQ-8 was administered only to women at post-treatment. The CSQ-8 has been shown to perform consistently across a range of treatment settings, has very good internal reliability, and has demonstrated construct validity (Attkinsson & Greenfield, 2004).
Non-study-based treatment
Participants were interviewed about substance-related treatment that they received during the 60 days prior to joining the study. Non-study-based treatment was defined as the total number of days of hospitalization for detoxification, residential substance-related treatment, and day treatment/intensive outpatient treatment.
Procedure
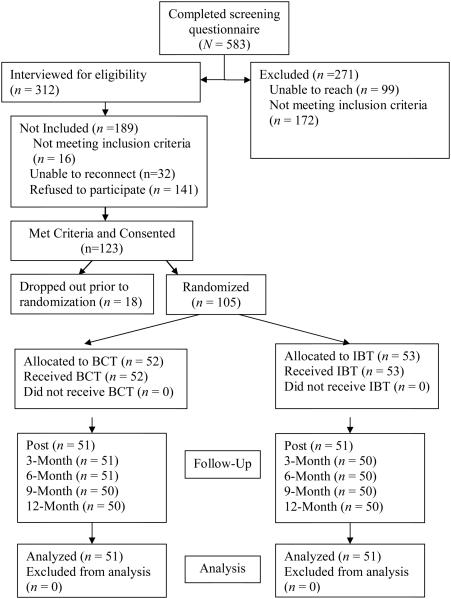
Married and cohabiting women seeking treatment for an alcohol use disorder (N = 583) completed a self-report screening questionnaire to determine possible eligibility for the study. Based upon the initial responses to the screening questionnaire, 172 were ineligible and 411 were deemed potentially eligible. Research staff attempted to contact women identified as potentially eligible but were not able to reach 99 women. Staff were able to speak with 312 potentially eligible women. Of the potentially eligible women that spoke with staff, 141 reported that they were not interested in the study and were not further assessed. 3 Another 32 reported initial interest in the study, but staff were unable to reconnect with the women to confirm final interest and eligibility. For those who were potentially eligible, reported interest in the study, and responded to staff, interviews were privately and separately completed with the female patient and her male partner to further assess eligibility. Of the couples who completed these interviews, 16 couples were determined to be ineligible. Participant flow into the trial is shown in Figure 1.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flowchart. BCT = behavioral couples therapy. IBT = individual-based treatment. Post = post-treatment.
A total of 123 couples met study criteria, signed informed consent, and were scheduled to complete baseline assessments with a research assistant. Following baseline assessments, the couple was scheduled to attend the first treatment session together. Randomization was conducted after couples had completed their baseline assessments and had scheduled their first treatment session. Of the 123 consented couples, 18 couples were not randomized because they dropped out prior to completing their baseline assessment (n = 12) or prior to scheduling their first treatment session (n = 6). The remaining 105 couples were put into an urn randomization computer program (Stout, Wirtz, Carbonari, & Del Boca, 1994) designed to balance the treatment groups in terms of age (34 or younger versus 35 or older), married versus cohabitation status, and whether or not the couple had a child between the ages of 6 and 16 living at home. Treatment assignment was concealed from participants until they arrived for their first treatment session. All couples attending one or more treatment sessions were followed and included in the analyses (N =105; see Figure 1).
We compared those randomized to treatment (N = 105) with those determined to be eligible but who were not randomized (N = 191; i.e., unable to reconnect n = 32, refused to participate n = 141, or who dropped out prior to randomization n = 18). Results showed there were no significant differences (all ps > .18) between these two groups of patients on age, education, race, employment status, relationship happiness, alcohol problem severity, and IPV.4
Treatment Conditions
Women in either treatment condition were assigned to receive a total of 26, 60-minute therapy sessions over the course of 20 weeks. The BCT condition had half BCT session plus half individual counseling sessions, and the IBT condition had individual sessions only.
BCT condition
Women assigned to the BCT condition were planned to receive 13 BCT sessions attended together by the woman and her partner. The O'Farrell and Fals-Stewart (2006) 12-session BCT manual was modified only slightly so that session 1 incorporated a couple-based clinical interview and the session 1 topics described by O'Farrell and Fals-Stewart (2006) were delivered over the course of the first 2 sessions. The order and content of sessions 3 through 13 otherwise corresponded to sessions 2 through 12 in the published manual.
BCT sessions aimed to build support for abstinence and improve relationship functioning. BCT substance-focused interventions to directly build support for abstinence included (a) a Recovery Contract with a calendar to record AA meetings attended, drug urine screen results, and completion of a daily "trust discussion" in which the patient states an intent to stay abstinent that day and the spouse expresses support for the patient's efforts; (b) teaching partners to decrease behaviors that may trigger or enable substance use; and (c) helping the couple decrease the patient’s exposure to alcohol and drugs by removing alcohol from the home and avoiding or managing alcohol-related family and social gatherings. BCT relationship-focused interventions were designed to increase positive feelings, shared activities, and constructive communication.
Women in the BCT condition also were planned to receive 13 individual, twelve-step oriented sessions for treatment of alcoholism, which the male partners did not attend. These individual sessions were drawn from the individual drug counseling manual (Mercer & Woody, 1999), which was slightly modified to focus on alcohol dependence; as noted in the manual, such modification is acceptable due to the generic nature of the intervention itself. This approach is based on the concept that alcoholism is a spiritual and medical disease, consistent with the philosophy of Alcoholics Anonymous (AA), and that recovery is a gradual process achieved by staying abstinent from alcohol and drugs and attending AA self-help groups. Individual drug counseling produced better outcomes than professional psychotherapy in the NIDA Collaborative Cocaine Treatment Study (Crits-Christoph, et al, 1999). It also served as a comparison group in a prior study of BCT for women with AUD (Fals-Stewart et al, 2006).
For the first 6 weeks, women in the BCT condition attended 1 BCT and 1 IBT session. Then during weeks 7 through 13, women continued to attend BCT weekly while attending IBT sessions on a biweekly basis. Finally, during weeks 14 through 20, women did not attend BCT sessions but continued to attend IBT sessions on a biweekly basis. This format was chosen as a way to engage women and their partners more intensively toward the beginning and then taper off toward the end of treatment.
IBT condition
Women assigned to the IBT condition were planned to attend 26 individual, twelve-step oriented sessions for treatment of alcoholism. In the IBT condition male partners did not participate in treatment. Sessions were based upon an adapted version of the individual drug counseling manual (Mercer & Woody, 1999) that was also the basis for individual therapy sessions received in the BCT condition. Specifically, patients in this condition received the 13 individual-based sessions that were provided to patients in the BCT condition in addition to 13 other sessions with a 12-step oriented focus.
The frequency of therapy sessions was yoked between the IBT and BCT conditions. Namely, women assigned to IBT attended twice weekly IBT sessions for the first six weeks. Then during weeks 7 through 13, women alternated between receiving 1 and 2 IBT sessions per week (e.g., 1 session in week 7, 2 sessions in week 8, 1 session in week 9, etc.). Finally, during weeks 14 through 20, women received biweekly IBT sessions.
Study therapists
Study therapists were 2 masters-level, licensed addiction counselors, and one doctoral-level psychologist. Therapists provided treatment in both the BCT and the IBT conditions. Specifically, participants were randomly assigned to either the BCT or IBT condition, and then one of the 3 therapists delivered the full course of the assigned treatment condition. This was chosen to increase the generalizability of the findings and to reduce the likelihood that differences across conditions were due to therapist-specific effects. Therapists received a 1 day didactic training in BCT and IBT, respectively, and each of these trainings was delivered by one of the authors of each particular treatment manual. Therapists also received weekly supervision from authors of the study (Schumm and O’Farrell), which involved review of audiotaped sessions and feedback about delivery of BCT and IBT.
Treatment fidelity
Sessions were audio-taped, and measures were developed to assess therapist adherence and competency in delivering the manualized treatments. Items were rated on a 5-point scale (not at all to extensively). Adherence and competency rating scales assessing fidelity to the individual drug counseling protocol, included 7 and 6 items, respectively. Examples of items included degree to which the therapist focused upon abstinence from substance use and degree to which the therapist incorporated strategies for promoting abstinence that are consistent with a 12-step orientation. The BCT adherence and competency rating scales were specific to each session of the manual and ranged from 5 to 20 items, depending upon session content.
Sessions were randomly selected to be rated, and ratings were performed by 2 independent raters trained in delivering both treatments. Sixty-eight individual counseling and 58 BCT sessions were rated, and 5 individual counseling and 8 BCT sessions were independently coded by both raters. For sessions coded independently by both raters, level of agreement between the raters was high, and the percentage of items that were rated within 1 point difference between raters were as follows: 97.1% individual counseling adherence, 100% individual counseling competency, 92.6% BCT adherence, 90.2% BCT competency.
Adherence and competency ratings were acceptable for both treatment formats. Mean ratings of BCT sessions were 4.38 (SD = 0.48) and 4.41 (SD = 0.50) for adherence and competency, respectively, which is in the range between scale ratings of 4 = "considerably" and the maximum score of 5 = "extensively." Mean adherence and competency ratings were also in this range for individual counseling sessions, M = 4.54, SD = 0.46, and M = 4.60, SD = 0.48. The BCT and IBT conditions did not differ significantly on aggregate mean competency ratings, F(1, 124) = 0.01, p = .95, or aggregate mean adherence ratings, F(1, 124) = 0.29, p = .59.
Analyses
We used generalized estimating equations (GEE) to test our hypotheses involving substance-related outcomes and relationship satisfaction outcomes. GEE has several advantages, including the ability to include participants who have covariate-dependent missing data on the repeated measures outcome, the capability to account for and appropriately model variable non-independence, and the capacity to directly include time as a predictor within the regression equations (Hall et al., 2001). Given the ability for GEE models to include participants with missing outcomes, those with data on at least one follow-up time period were included in the models. For all GEE analyses continuous predictor and outcome variables were z score-transformed to allow ready calculation of effect size estimates and to reduce multicollinearity between main effects and interaction terms. Treatment condition was dummy-coded with IBT as the reference group. Following prior research (McCrady, et al 2009), PDA was arcsine-transformed to improve normality. Baseline days of non-study-based treatment was square root-transformed to improve normality.
Analyses were conducted in steps. The first model included the following variables: time, the baseline outcome of interest, and baseline days of non-study-based treatment. We then compared relative model fits for exchangeable, unstructured, and autoregressive dependent variable correlation structures and selected the structure with the lowest Quasi Likelihood under Independence Model Criterion (QIC) value.5 Once the best-fitting correlational structure was determined, we added treatment condition to the model. We then entered the interaction between treatment condition and time to determine whether treatment effects were diminished or enhanced over the course of follow-up. Finally, in an exploratory analysis, we tested interactions between treatment condition and the respective dependent variable at baseline and baseline days of non-study-based treatment. These interactions were nonsignificant in all cases but one, which is detailed below.6
Due to severe negative skewness and the existence of severe outliers, CTS2 IPV frequency scores were dichotomized to capture the presence or absence of IPV, and logistic regression was used. The first regression model included the pre-treatment outcome of interest, baseline days of non-study-based treatment, and treatment condition; and the second exploratory model added interactions between treatment and the covariates.
Results
Female Non-Study-Based Treatment
Treatment conditions did not differ on the amount of female non-study-based treatment during the 60 days prior to joining the study, t(103) = −0.13, p = .90. Women received an average of over 8 total days of detoxification, residential rehabilitation, and intensive outpatient treatment during the 60 days prior to the study, IBT M = 8.36, SD = 9.00; BCT M = 8.37, SD = 8.24.
Treatment Attendance and Satisfaction
Treatment conditions did not differ on number of female study-based psychotherapy sessions that were attended, t(103) = −0.51, p > .61. Women in both conditions attended an average of over 20 study therapy sessions: BCT M = 20.98, SD = 7.41; IBT M = 20.26, SD = 7.00. In addition, the conditions did not differ with regard to the number of women completing at least 50% (i.e., 13 or more) of the prescribed study psychotherapy sessions, χ2(N = 105, 1) = 0.04, p > .83. In BCT, 82.7% completed at least 50% of the study sessions, and in IBT, 81.1% completed at least 50% of the study sessions.
According to the CSQ-8, women, on average, were very satisfied with their study-based treatment. The total CSQ-8 scores in IBT, M = 28.70, SD = 4.29, and BCT, M = 28.12, SD = 5.04, did not differ significantly, t(98) = 0.62, p = .54. These CSQ-8 total scores were similar to large-scale samples of individuals seeking mental health care (Attkisson & Greenfield, 2004).
Primary Outcomes of Substance Use and Related Problems
For the GEE models involving PDA, results supported a better fit for an unstructured correlation model (QIC = 511.93) versus exchangeable (QIC = 512.22) or autoregressive (QIC = 513.31). The GEE analyses using an unstructured correlation model showed that while controlling for baseline PDA and baseline non-study-based treatment, there was a significant main effect of study treatment condition. The interaction between treatment condition and time was non-significant. Consistent with the observed means (see Table 2), the GEE model showed that on average, women who received BCT had higher PDA during treatment and during the 12-month follow-up (see Table 3).
Table 2.
Substance Use Outcomes Observed M (SD) and Sample Size by Treatment Condition and Assessment Period
| Percentage days abstinent
(PDA) | ||||||
| Treatment | Baseline | Post | 3-month | 6-month | 9-month | 12-month |
|
| ||||||
| BCT | 26.14 (30.29) n = 53 |
86.38 (24.73) n = 51 |
85.18 (25.14) n = 51 |
87.17 (23.08) n = 51 |
82.62 (27.57) n = 50 |
81.50 (27.00) n = 50 |
| IBT | 33.46 (31.90) n = 52 |
82.80 (23.64) n = 51 |
80.87 (31.38) n = 50 |
74.24 (36.21) n = 50 |
71.45 (38.49) n = 50 |
72.74 (37.82) n = 50 |
|
| ||||||
| Inventory of Drug Use
Consequences (InDUC) | ||||||
| Treatment | Baseline | Post | 3-month | 6-month | 9-month | 12-month |
|
| ||||||
| BCT | 67.97 (23.02) n = 53 |
30.31 (33.53) n = 51 |
19.02 (23.63) n = 50 |
14.76 (23.40) n = 51 |
12.57 (17.98) n = 46 |
17.17 (24.22) n = 50 |
| IBT | 57.64 (22.64) n = 52 |
26.66 (25.14) n = 50 |
20.43 (22.66) n = 49 |
22.27 (29.23) n = 48 |
21.60 (26.39) n = 48 |
23.25 (28.33) n = 50 |
Note. BCT = behavioral couples therapy. IBT = individual-based treatment. Post = post-treatment.
Table 3.
Generalized Estimating Equation (GEE) Results for Substance Use Outcomes During Follow-up
| Percentage days abstinent
(PDA) (N = 102) | ||||
| Predictor | d | 95% CI | χ 2 | P |
|
| ||||
| Treatment condition | .330 | .003, .658 | 3.901 | .048 |
| Baseline PDA | .145 | −.021, .312 | 2.920 | .088 |
| Baseline non-study female SUD tx | .151 | −.015, .316 | 3.181 | .075 |
| Time | −.006 | −.041, .029 | 0.111 | .739 |
|
| ||||
| Treatment × time | −.026 | −.093, .042 | 0.553 | .457 |
|
| ||||
| Inventory of Drug Use Consequences (InDUC) (N = 101) | ||||
|
| ||||
| Predictor | d | 95% CI | χ 2 | P |
|
| ||||
| Treatment condition | −.316 | −.616, −.017 | 4.277 | .039 |
| Baseline InDUC | .308 | .145, .472 | 13.668 | <.001 |
| Baseline non-study female SUD tx | −.149 | −.306, .008 | 3.447 | .063 |
| Time | .006 | −.037, .049 | 0.069 | .793 |
|
| ||||
| Treatment × time | −.094 | −.179, −.008 | 4.592 | .032 |
Note. Coding for treatment condition: 0 = individual-based treatment, 1 = behavioral couples therapy.
For the InDUC measure of substance-related problems, an exchangeable GEE correlational structure (QIC = 481.99) fit better than unstructured (QIC = 482.21) or autoregressive (QIC = 482.70) structures. The GEE analyses using an exchangeable structure, showed a significant main effect for treatment. This treatment effect was qualified by a significant treatment by time interaction (see Table 3). Model-based GEE results probing the treatment by time interaction showed that the effect of treatment was non-significant at post (d = −.130, 95% CI = −.475, .214, p = .458) and 3-month (d = −.224, 95% CI = −.535, .087, p = .158) but was significant at 6-month (d = −.318, 95% CI = −.617, −.018, p = .038), 9-month (d = −.411, 95% CI = −.723, −.099, p = .010), and 12-month (d = −.505, 95% CI = −.851, −.159, p = .004) follow-ups. These results were consistent with the observed means (see Table 2) in showing that on the InDUC, there was an increasing advantage over the course of the follow-up period for BCT versus IBT, such that BCT had significantly fewer substance-related problems in the last 9 months of the 12-month follow-up period.
Secondary Outcomes of Relationship Satisfaction and IPV
Female Relationship Satisfaction
For the female-reported DAS, an unstructured GEE model (QIC = 297.31) produced better fit versus an exchangeable (QIC = 298.48) or autoregressive (QIC = 298.09) model. The GEE analyses using an unstructured correlation matrix did not produce a significant main effect for treatment condition. However, there were significant interactions involving treatment condition by time, treatment condition by baseline female-reported DAS, and treatment condition by baseline female non-study-based treatment (see Table 5). Post hoc probing of the treatment by time interaction did not show significant differences between treatment conditions at any of the individual time periods (ps > .06), although Table 4 and the interaction term GEE estimate showed an increasingly pronounced effect of treatment over time, which favored BCT. In addition, the interaction terms showed that the treatment effect favoring BCT was greater for women with lower baseline DAS scores and for women who received less baseline non-study treatment (see Table 5).
Table 5.
Generalized Estimating Equation (GEE) Results for Relationship Outcomes During Follow-up
| Female-reported Dyadic Adjustment Scale (DAS) (N = 100) | ||||
|
| ||||
| Predictor | d | 95% CI | X2 | p |
|
| ||||
| Treatment condition | .063 | −.158, .285 | 0.314 | .575 |
| Baseline female-reported DAS | .654 | .542, .766 | 131.569 | <.001 |
| Baseline non-study female SUD tx | .075 | −.037, .187 | 1.725 | .189 |
| Time | −.003 | −.042, .036 | 0.029 | .864 |
|
| ||||
| Treatment × time | .130 | .067, .194 | 15.989 | <.001 |
| Treatment × baseline DAS | −.498 | −.734, −.262 | 17.167 | <.001 |
| Treatment × baseline non-study tx | −.356 | −.596, −.116 | 8.479 | .004 |
|
| ||||
| Male-reported Dyadic Adjustment Scale (DAS) (N = 100) | ||||
|
| ||||
| Predictor | d | 95% CI | χ 2 | p |
|
| ||||
| Treatment condition | .172 | −.085, .428 | 1.718 | .190 |
| Baseline male-reported DAS | .615 | .484, .746 | 84.527 | <.001 |
| Baseline non-study female SUD tx | .056 | −.071, .183 | 0.758 | .384 |
| Time | .002 | −.033, .037 | 0.008 | .927 |
|
| ||||
| Treatment × time | .069 | −.001, .139 | 3.744 | .053 |
|
| ||||
| Female-reported Relationship Happiness Scale (RHS) (N = 100) | ||||
|
| ||||
| Predictor | d | 95% CI | χ 2 | p |
|
| ||||
| Treatment condition | .140 | −.083, .362 | 1.519 | .218 |
| Baseline female-reported RHS | .547 | .435, .660 | 90.886 | <.001 |
| Baseline non-study female SUD tx | .061 | −.051, .173 | 1.131 | .288 |
| Time | .001 | −.055, .056 | 0.000 | .985 |
|
| ||||
| Treatment × time | .067 | −.045, .178 | 1.364 | .243 |
|
| ||||
| Male-reported Relationship Happiness Scale (RHS) (N= 100) | ||||
|
| ||||
| Predictor | d | 95% CI | χ 2 | p |
|
| ||||
| Treatment condition | .325 | .050, .601 | 5.348 | .021 |
| Baseline male-reported RHS | .477 | .338, .616 | 45.100 | <.001 |
| Baseline non-study female SUD tx | .108 | −.032, .247 | 2.293 | .130 |
| Time | −.003 | −.040, .035 | 0.018 | .893 |
|
| ||||
| Treatment × time | .067 | −.007, .142 | 3.168 | .075 |
Note. Coding for treatment condition: 0 = individual-based treatment, 1 = behavioral couples therapy.
Table 4.
Relationship Outcomes Observed M (SD) or % and Sample Size by Treatment Condition and Assessment Period
| Female-reported Dyadic Adjustment Scale (DAS) | ||||||
|
| ||||||
| Treatment | Baseline | Post | 3-month | 6-month | 9-month | 12-month |
|
| ||||||
| BCT | 105.03 (20.26) n =52 |
105.12 (24.52) n =50 |
111.44 (21.54) n = 47 |
107.76 (23.84) n = 49 |
110.70 (26.29) n = 44 |
111.32 (20.91) n = 46 |
| IBT | 105.78 (19.43) n = 53 |
108.91 (22.03) n = 49 |
107.14 (23.35) n = 48 |
105.39 (26.92) n =50 |
102.02 (32.02) n = 47 |
104.15 (26.05) n = 47 |
|
| ||||||
| Male-reported Dyadic Adjustment Scale (DAS) | ||||||
|
| ||||||
| Treatment | Baseline | Post | 3-month | 6-month | 9-month | 12-month |
|
| ||||||
| BCT | 96.63 (18.74) n =52 |
105.12 (24.52) n = 50 |
106.46 (20.44) n = 48 |
105.30 (22.71) n = 49 |
107.18 (22.48) n = 45 |
107.81 (22.47) n = 46 |
| IBT | 103.30 (14.78) n = 53 |
107.94 (20.18) n = 48 |
108.79 (20.36) n = 48 |
108.95 (21.86) n = 47 |
107.23 (23.34) n = 45 |
104.50 (27.45) n = 47 |
|
| ||||||
| Female-reported Relationship Happiness Scale (RHS) | ||||||
|
| ||||||
| Treatment | Baseline | Post | 3-month | 6-month | 9-month | 12-month |
|
| ||||||
| BCT | 61.27 (18.24) n =52 |
73.46 (22.92) n = 50 |
77.40 (16.78) n = 47 |
75.45 (20.95) n = 48 |
77.24 (20.37) n = 44 |
74.58 (19.45) n = 45 |
| IBT | 63.33 (21.93) n = 53 |
75.55 (19.02) n = 50 |
73.15 (20.48) n = 48 |
72.81 (21.17) n = 49 |
68.82 (24.01) n = 47 |
69.98 (23.95) n = 48 |
|
| ||||||
| Male-reported Relationship Happiness Scale (RHS) | ||||||
|
| ||||||
| Treatment | Baseline | Post | 3-month | 6-month | 9-month | 12-month |
|
| ||||||
| BCT | 45.95 (19.32) n = 52 |
67.53 (24.45) n = 50 |
71.83 (19.81) n = 48 |
71.76 (20.41) n = 49 |
74.37 (19.37) n = 45 |
73.07 (20.00) n = 46 |
| IBT | 49.05 (19.65) n = 53 |
66.87 (22.44) n = 49 |
67.22 (23.14) n = 48 |
66.83 (22.30) n = 47 |
66.96 (22.69) n = 45 |
65.37 (24.84) n = 47 |
|
| ||||||
|
| ||||||
| % Female-perpetrated physical aggression | ||||||
|
| ||||||
| Treatment | Baseline | Post | 3-month | 6-month | 9-month | 12-month |
|
| ||||||
| BCT | 57.8 n = 52 |
--- | --- | --- | --- | 24.5 n = 49 |
| IBT | 52.8 n = 53 |
--- | --- | --- | --- | 24.5 n = 49 |
|
| ||||||
| % Male-perpetrated physical aggression | ||||||
|
| ||||||
| Treatment | Baseline | Post | 3-month | 6-month | 9-month | 12-month |
|
| ||||||
| BCT | 61.5a
n = 52 |
--- | --- | --- | --- | 28.6 n = 49 |
| IBT | 35.8a
n = 53 |
--- | --- | --- | --- | 20.4 n = 49 |
Note. BCT = behavioral couples therapy. IBT = individual-based treatment. Post = post-treatment.
Differences between BCT and IBT were significant, χ2 (1) = 6.93, p < .05.
For the female-reported RHS, an autoregressive model (QIC = 349.98) fit better than exchangeable (QIC = 350.45) or unstructured (QIC = 350.45) GEE models. The GEE analyses using the autoregressive model did not produce a significant effect for treatment or a treatment by time interaction (see Table 5).
Male Relationship Satisfaction
For the male-reported DAS, an exchangeable GEE model (QIC = 321.21) produced better fit versus an unstructured (QIC = 322.49) or autoregressive (QIC = 322.52) model. As shown in Table 5, results failed to support a significant effect for treatment or a treatment by time interaction.
For male-reported RHS scores, the exchangeable GEE model (QIC = 386.97) was superior to the unstructured (QIC = 387.49) or autoregressive (QIC = 388.56) models. The GEE model using an exchangeable structure showed a main effect of treatment, while the treatment by time interaction was not significant (see Table 5). The main effect of treatment was consistent with the observed means showing that on average, men in BCT had higher RHS scores during treatment and during the 12-month follow-up (see Table 4).
Female- and Male-Perpetrated IPV
McNemar's chi-square tests showed overall reductions in the occurrence of female-perpetrated IPV, χ2 (1, N =98) = 25.71, p < .001, and male-perpetrated IPV, χ2 (1, N =98) = 17.63, p < .001, from baseline to 12-month follow-up (see Table 4). However, logistic regression showed that BCT and IBT did not differ on female-perpetrated IPV [χ2 (1) = 0.93, p = .34; OR = 0.78, 95% CI = 0.48, 1.29] or male-perpetrated IPV [χ2(1) = 0.10, p = .75; OR = 0.84, 95% CI = 0.29, 2.47] at 12-month follow-up. This suggests that BCT and IBT showed similar improvements in IPV. The models were not improved by adding treatment interactions in step 2 [female-perpetrated IPV, χ2(2) = 2.68, p = .26; male-perpetrated IPV, χ2(2) = 0.64, p =.73].
An incidental, unexpected finding showed that baseline prevalence of male IPV was greater for BCT than IBT participants (see Table 4).
Discussion
Primary study outcomes followed predictions in this randomized clinical trial comparing BCT with IBT among women with AUD. BCT did better than IBT on primary study outcomes of greater abstinence from alcohol and drugs and fewer substance-related problems. Specifically, BCT had greater PDA during treatment and in the 12-month follow-up period, and BCT had fewer substance-related problems during most of the follow-up period. Convergent findings of better outcomes for BCT both on substance use and on substance-related problems suggest that the differences observed are clinically meaningful. Further, the effect sizes observed favoring BCT over IBT on these primary study outcomes are of a magnitude that have been considered clinically meaningful.7 These findings suggest that clinicians and substance use treatment programs should offer BCT as a first-line treatment option for women with AUD who are living with a male partner.
Primary substance-related outcomes in the present study replicate and expand upon the two prior studies of BCT among women with AUD. Our results replicated previous research in showing that women who received BCT had significantly greater PDA during the 12 months following treatment than those who received IBT only (Fals-Stewart et al, 2006; McCrady et al., 2009). Our results also replicated findings by Fals-Stewart et al. (2006) in showing that women in BCT had fewer substance-related problems during the 12 month follow-up than those in IBT. In contrast to the present study, which assessed substance-related problems at multiple time points over the course of the follow-up period, Fals-Stewart et al. compared BCT to IBT at only two assessments: pre-treatment and 12-month follow-up. By assessing substance-related problems at multiple time points during the follow-up period, we demonstrated a significant treatment condition by time interaction, such that there was an increasing advantage over the course of the follow-up period for BCT versus IBT on women's substance-related problems.
Secondary study outcomes of relationship satisfaction and IPV provided some support for study predictions. Relationship satisfaction of male partners followed study predictions. For male partners in the present study, advantages for BCT over IBT were observed on the RHS following treatment as predicted. During the 12-months following treatment, men who received BCT had significantly greater relationship satisfaction on the RHS versus those whose female alcoholic partners received IBT only. Hence, male partners in BCT reported greater relationship happiness following treatment, and this advantage over IBT was consistently maintained over the duration of the follow-up. These findings have implications for potentially helping to improve involvement of male partners in women’s AUD treatment. Specifically, it may be a useful engagement strategy to inform male partners that they are likely to personally experience greater relationship happiness if they are agreeable to participate with their female partners in BCT versus if their female partners participate in individual AUD therapy alone.
Relationship satisfaction of the female alcoholic patients also showed findings that were consistent with study predictions, as well as interesting unpredicted results. We found that changes in women's DAS scores differed between BCT and IBT during the 12-months following treatment. First, the significant treatment by time interaction showed that there was an increasing advantage over the course of the 12-month follow-up period for BCT versus IBT on women’s DAS scores. Better drinking outcomes for BCT over IBT – PDA stably over the follow-up months and substance problems increasingly over the course of the follow-up – may have led to an increasing advantage of BCT over IBT on women’s DAS scores during the follow-up period. Second, the significant interaction between women's pre-treatment DAS scores and treatment condition (BCT versus IBT) showed that the advantage of BCT over IBT on women's follow-up DAS scores was greater for women who reported lower relationship satisfaction on the DAS at baseline. The present unpredicted results may reflect that women with more relationship distress have more room for improvement with a relationally oriented treatment like BCT. A clinical implication of this finding is that treatment providers should be especially encouraging of women with AUD who have high relationship distress to participate in BCT versus individual therapy alone. Neither prior study (Fals-Stewart et al, 2006; McCrady et al, 2009) examined baseline relationship satisfaction as a moderator of relationship outcomes after BCT versus IBT. Finally, another unpredicted interaction showed that women who had a lower amount of intensive SUD treatment in the 60 days prior to starting study-based treatment had better DAS scores following treatment if they received BCT instead of IBT. This is probably best considered a chance finding because we did a number of analyses examining non-study treatment as a predictor or moderator, and this was the only result that reached a customary level of statistical significance. One result would have been expected to reach significance by chance.
The prediction that IPV for the year after treatment would be lower in BCT than in IBT was not supported. IPV did not differ for BCT versus IBT for either male- or female-perpetrated violence. Significant reductions in IPV occurred for both BCT and IBT, but the two treatments did not differ. This was only the second study to compare the efficacy of BCT versus IBT in reducing IPV among women with AUD. Unlike Fals-Stewart et al (2006), who reported superiority of BCT over IBT in reducing rates of IPV, our study failed to show differences in the amount of improvement on IPV for BCT versus IBT. The differing results merit consideration. First, measures of IPV differed across the two studies. The present study used the well-established CTS2 and the other study used a more recently developed calendar-based TLFB measure. Second, the broader AUD literature shows that 5 studies found reduced IPV after BCT: 3 naturalistic studies (O’Farrell & Murphy, 1995, and O’Farrell et al 2004 with male patients; and Schumm et al 2009 with female patients); and 2 RCTs showing BCT had less IPV than IBT (Fals-Stewart & Clinton-Sherrod, 2009 with male patients; and Fals-Stewart et al 2006 with female patients). Thus greater IPV reductions for BCT than IBT may not be a well-established finding coming as it does from two studies by the same researcher and failing to be replicated in the current study. Further attempts at replication are needed. Also multiple naturalistic studies of IBT show significant reductions in IPV (e.g., Maiden, 1997; Stuart et al, 2002, 2003), like those found in the present study.
This study had multiple strengths. Our use of individual drug counseling as the comparison condition permits us to draw conclusions about the efficacy of BCT in comparison to a treatment that has demonstrated benefits to reducing substance-related problems (Crits-Christoph et al., 1999). We are, therefore, able to draw conclusions about the relative efficacy of BCT in comparison to a treatment that has known benefits for substance use disorders. Another advantage of using individual drug counseling as the comparator is that this treatment is based in a 12-step philosophy, which is the most widely adopted treatment orientation among substance use programs in the U.S. (Roman & Johnson, 2004), thereby improving the generalizability of findings. Other strengths included: the high treatment fidelity ratings achieved by the study therapists, the high session attendance rates and therapy satisfactions ratings in both BCT and IBT suggesting they were equally credible and satisfying treatments, use of accepted outcome measures and collateral reports to reduce under-reporting, use of an intent-to-treat sample and accepted statistical analyses, low degree of missing data, and low attrition rates. Such factors strengthened the internal validity of the study.
Limitations of the study and suggestions for future research should also be noted. The current study's results do not generalize to women whose partners have an active substance use disorder. Although there is data from an uncontrolled study which suggests that BCT may be effective for couples in which both partners have AUD (Schumm, O'Farrell, & Burdzovec Andreas, 2012), controlled studies are needed to test the efficacy of BCT when both partners have a substance use disorder. Another limitation is that we did not include information on women's mental health disorder diagnoses that were co-occurring with their substance use disorders. McCrady et al. (2009) found that the superiority of BCT versus IBT on drinking outcomes was stronger among women with alcoholism who exhibited co-occurring mental health disorders. Hence, there is a need for additional studies to replicate this finding. Finally, our results also do not generalize beyond women who are agreeable to try either BCT or IBT. A recent study suggests that when given a choice, women may be more prone to choose IBT due to a variety of factors, such as perceived lack of partner support and logistical issues (McCrady et al, 2011). It is not clear if informing women about the demonstrated superiority of BCT would affect their decision about treatment choice; however, additional studies are needed to expand the understanding of how treatment choice might impact outcomes for women seeking alcoholism treatment. Research is also needed to address other barriers to BCT, such as the belief that one's partner is not supportive enough to be involved in treatment.
In conclusion, results from this study build upon prior research that shows BCT is superior to IBT for the treatment of men with AUD (Powers, Vedel, & Emmelkamp, 2008). First, there are only two other published randomized clinical trials of BCT among women with AUD (Fals-Stewart et al, 2006; McCrady et al., 2009), The present study's findings are important to expanding and extending the evidence for BCT as an efficacious treatment for women with AUD. These three studies of BCT with women AUD patients all show better drinking outcomes for BCT than IBT, and better relationship outcomes for BCT in the two studies that examined relationship outcomes. These convergent findings are especially significant when one considers the various procedural and methodological aspects on which the studies differed. Three different groups of investigators conducted the studies. Two different BCT treatment manuals were used, with one study (McCrady et al, 2009) emphasizing teaching the spouse specific skills to deal with alcohol-related situations (McCrady & Epstein, 2008), and the other studies using the recovery contract approach (O’Farrell & Fals-Stewart, 2006) used in the present study. One study used BCT as a stand alone intervention compared with individual CBT (McCrady et al, 2009), and the other studies used BCT combined with 12-step oriented individual counseling as compared with a 12-step oriented comparison group. One study used middle and upper middle class women recruited by advertising (McCrady et al, 2009), and the other studies recruited their sample from established treatment centers. Despite all these differences among the three studies, results favoring BCT on drinking and relationship outcomes seem robust across the studies. Second, additional research on the efficacy of BCT is needed among women with primary drug use disorders, women whose partners also have a substance use disorder, and women in same sex relationships. Third, studies are needed that deconstruct BCT in order to understand the necessary and active ingredients of this therapy and to potentially make the therapy delivery more efficient. Finally, as indicated by recent literature reviews (Meis et al 2013; O’Farrell & Clements, 2012), dissemination of BCT is the highest priority goal for future research on BCT.
Acknowledgments
This research was supported by grant R01AA14700 awarded to the second author by the National Institute on Alcohol Abuse and Alcoholism and by the Department of Veterans Affairs. We gratefully acknowledge assistance from Fay Larkin, Anne Gribauskas, and Leslie Reid.
Footnotes
Two same sex female couples were excluded from the study, and they were referred for couple therapy outside the study protocol.
This criteria means that some couples could have had severe violence on days when drinking or using drugs, but systematic data on this point were not collected.
About half (52%, n=74) of the 141 prospective participants who refused to participate simply stated that they were not interested with no further details offered. The remaining half of those who refused provided a variety of reasons for their lack of interest. The most common reason (22%, n=31/141) concerned the male partners’ inability to participate either because he was not interested (n=16) or he was too busy/his schedule did not allow (n=15). The other reasons mentioned in descending frequency of occurrence are as follows: female patient was too busy or felt time commitment was too great (n=14), the female patient did not want more treatment (n=5), female patient wanted a different type of treatment (n=4), no transportation (n=3), female patient only wanted couples treatment (n=3), lack of childcare (n=2), female patient wanted to receive treatment at a different agency (n=2), female patient did not want to do couples treatment (n=2), and a recent family death (n=1).
In order to examine possible differences between patients randomized to treatment (N=105) vs. patients who were eligible but not randomized (N=191), we utilized data collected on the self-report screening questionnaire. The screening questionnaire contained demographic information and several other questions: relationship happiness (i.e., global happiness rating from the Dyadic Adjustment Scale on a fully-anchored scale ranging from 0 ‘Extremely unhappy’ to 6 ‘Perfect’); alcohol problem severity (i.e., anchored scale ranging from 0 ‘Not a problem’ to 6 ‘Extremely severe problem’); and IPV (i.e., assessment of behaviors committed by the patient and partner during the past 3 years when the patient and partner fought or argued that included three violence items: push, grab or shove; slap; hit).
We also added a quadratic effect of time to the GEE models. The quadratic effect of time was non-significant for all models, and the addition of a quadratic effect of time did not improve model fit in any model. Hence, we present the GEE models that included a linear effect of time.
Interactions between the baseline outcome and treatment condition and between baseline non-study-based treatment and treatment condition were explored but were found to be non-significant in all GEE analyses except the model involving female-reported DAS. Therefore, only the GEE model for female-reported DAS includes the additional baseline outcome by treatment condition and baseline non-study-based treatment by treatment condition interactions.
Using Cohen’s (1988) conventions, an effect size of d = .10 is small, d = .50 is medium, and d = .80 is a large effect. An effect size has been considered clinically meaningful if the size of the difference between two treatments is at least midway between a small and a medium effect size (i.e., d of .30 or greater; O’Farrell, Murphy, Alter & Fals-Stewart, 2010).
Contributor Information
Jeremiah A. Schumm, Cincinnati VA Medical Center and University of Cincinnati
Timothy J. O’Farrell, VA Boston Healthcare System and Harvard Medical School
Christopher W. Kahler, Brown University
Marie M. Murphy, VA Boston Healthcare System and Harvard Medical School
Patrice Muchowski, AdCare Hospital of Worcester, Inc..
References
- Attkisson CC, Greenfield TK. The UCSF client satisfaction scales: I. The client satisfaction questionnaire-8. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 2004. pp. 1333–1346. [Google Scholar]
- Azrin NH, Naster BJ, Jones R. Reciprocity counseling: A rapid learning-based procedure for marital counseling. Behaviour Research and Therapy. 1973;11:365–382. doi: 10.1016/0005-7967(73)90095-8. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the social sciences. 2nd Lawrence Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken L, Beck A. Psychosocial treatment for cocaine dependence: National Institute on Drug Abuse collaborative cocaine treatment study. Archives of General Psychiatry. 1999;56:493–502. doi: 10.1001/archpsyc.56.6.493. [DOI] [PubMed] [Google Scholar]
- Diehl A, Croissant B, Batra A, Mundle G, Nakovics V, Mann K. Alcoholism in women: Is it different in onset and outcome compared to men? European Archives of Psychiatry and Clinical Neuroscience. 2007;257:344–351. doi: 10.1007/s00406-007-0737-z. Doi: 10.1007/s00406-007-0737-z. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W. Intermediate length neuropsychological screening of impairment among psychoactive substance-abusing patients: A comparison of two batteries. Journal of Substance Abuse. 1996;8:1–17. doi: 10.1016/s0899-3289(96)90043-7. Doi: 10.1016/S0899-3289(96)90043-7. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Birchler GR, Kelley ML. Learning sobriety together: A randomized clinical trial examining behavioral couples therapy with alcoholic female patients. Journal of Consulting and Clinical Psychology. 2006;74:579–591. doi: 10.1037/0022-006X.74.3.579. Doi: 10.1037/0022-006X.74.3.579. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Clinton-Sherrod M. Treating intimate partner violence among substance-abusing dyads: The effect of couples therapy. Professional Psychology: Research and Practice. 2009;40:257–263. Doi: 10.1037/aa0012708. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. American Psychiatric Press; Washington, D.C.: 1996. [Google Scholar]
- Hall SM, Delucchi K, Velicer W, Kahler C, Ranger-Moore J, Hedeker D, Niaura R. Statistical analysis of randomized trials in tobacco treatment: Longitudinal designs with dichotomous outcome. Nicotine & Tobacco Research. 2001;3:193–202. doi: 10.1080/14622200110050411. Doi: 10.1080/14622200110050411. [DOI] [PubMed] [Google Scholar]
- Jacques-López A, González-Reimers E, Rodríguez-Moreno F, Santaloria-Fernández F, López-Lirola A, Ros-Vilamajo R, Martínez-Riera A. Prevalence and mortality of heavy drinkers in a general medical hospital unit. Alcohol and Alcoholism. 2001;36:335–338. doi: 10.1093/alcalc/36.4.335. [DOI] [PubMed] [Google Scholar]
- Khan S, Okuda M, Hasin DS, Secades-Villa R, Keyes K, Lin K-H, Blanco C. Gender differences in lifetime alcohol dependence: Results from the National Epidemiologic Survey On Alcohol And Related Conditions. Alcoholism: Clinical and Experimental Research. 2013;37:1696–1705. doi: 10.1111/acer.12158. doi: 10.1111/acer.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly ML, Halford WK, Young RM. Couple communication and female problem drinking. Psychology of Addictive Behaviors. 2002;16:269–271. [PubMed] [Google Scholar]
- Lemke S, Brennan PL, Schutte KK. Upward pressure on drinking: Exposure and reactivity in adulthood. Journal of Studies on Alcohol and Drugs. 2007;68:437–445. doi: 10.15288/jsad.2007.68.437. [DOI] [PubMed] [Google Scholar]
- Maiden R. Alcohol dependence and domestic violence: Incidence and treatment implications. Alcoholism Treatment Quarterly. 1997;15:31–50. Doi: 10.1300/J020v15n02_03. [Google Scholar]
- McCrady BS, Epstein EE. Overcoming alcohol problems: A couples-focused program therapist guide. Oxford University Press; New York: 2008. [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen NK, Hildebrant T. A randomized trial of individual and couple behavioral alcohol treatment for women. Journal of Consulting and Clinical Psychology. 2009;77:243–56. doi: 10.1037/a0014686. Doi: 10.1037/a0014686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen NK, Ladd BO. What do women want? Alcohol treatment choices, treatment entry, and retention. Psychology of Addictive Behaviors. 2011;25:521–529. doi: 10.1037/a0024037. Doi: 10.1037/a0024037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meis LA, Griffin JM, Greer N, Jensen AC, MacDonald R, Carlyle M, Wilt TJ. Couple and family involvement in adult mental health treatment: A systematic review. Clinical Psychology Review. 2013;33:275–286. doi: 10.1016/j.cpr.2012.12.003. Doi: 10.1016/j.cpr.2012.12.003. [DOI] [PubMed] [Google Scholar]
- Mercer D, Woody GE. An Individual Drug Counseling Approach to Treating Cocaine Addiction: The Collaborative Cocaine Treatment Study Model. National Institute on Drug Abuse; Rockville, MD: 1999. Manual 3: Therapy Manuals for Drug Addiction. [Google Scholar]
- Miller WR, Meyers RJ, Tonigan JS. Engaging the unmotivated in treatment for alcohol problems: A comparison of three strategies for intervention through family members. Journal of Consulting and Clinical Psychology. 1999;67:688–697. doi: 10.1037//0022-006x.67.5.688. Doi: 10.1037/0022-006X.67.5.688. [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, Clements K. Review of outcome research on marital and family therapy in treatment of alcoholism. Journal of Marital and Family Therapy. 2012;38:122–144. doi: 10.1111/j.1752-0606.2011.00242.x. Doi: 10.1111/j.1752-0606.2011.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Fals-Stewart W. Behavioral couples therapy for alcoholism and drug abuse. Guilford Press; New York: 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Murphy CM. Marital violence before and after alcoholism treatment. Journal of Consulting and Clinical Psychology. 1995;63:256–262. doi: 10.1037//0022-006x.63.2.256. [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, Murphy CM, Stephen S, Fals-Stewart W, Murphy M. Partner violence before and after couples-based alcoholism treatment for male alcoholic patients: The role of treatment involvement and abstinence. Journal of Consulting and Clinical Psychology. 2004;72:202–217. doi: 10.1037/0022-006X.72.2.202. Doi: 10.037/0022-006X.72.2.202. [DOI] [PubMed] [Google Scholar]
- O'Farrell TJ, Murphy M, Alter J, Fals-Stewart W. Behavioral family counseling for substance abuse: A treatment development pilot study. Addictive Behaviors. 2010;35:1–6. doi: 10.1016/j.addbeh.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Schein AZ. Behavioral couples therapy for alcoholism and drug abuse. Journal of Family Psychotherapy. 2011;22:1–23. [Google Scholar]
- Powers MB, Vedel E, Emmelkamp PMG. Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clinical Psychology Review. 2008;28:952–962. doi: 10.1016/j.cpr.2008.02.002. Doi:10.1016/j.cpr.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Rehm J, Taylor B, Mohapatra S, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug and Alcohol Review. 2010;29:437–445. doi: 10.1111/j.1465-3362.2009.00153.x. [DOI] [PubMed] [Google Scholar]
- Roman PM, Johnson JA. National Treatment Center Study Summary Report. Institute for Behavioral Research, University of Georgia; Athens, GA: 2004. [Google Scholar]
- Schumm JA, O’Farrell TJ, Burdzovic Andreas J. Drinking outcomes following behavioral couples therapy for couples in which both partners have a current alcohol use disorder. Alcoholism Treatment Quarterly. 2012;30:407–421. doi: 10.1080/07347324.2012.718963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumm J, O’Farrell TJ, Murphy CM, Fals-Stewart W. Partner violence before and after couples-based alcoholism treatment for women alcoholic patients and their male partners. Journal of Consulting and Clinical Psychology. 2009;77:1136–1146. doi: 10.1037/a0017389. Doi: 10.1037/a0017389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JE, Meyers RJ. Motivating substance abusers to enter treatment. Guilford Press; New York NY: 2004. [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback user’s guide: a calendar method for assessing alcohol and drug use. Addiction Research Foundation; Toronto, Canada: 1996. [Google Scholar]
- Spanier GB. Dyadic adjustment scale: User's manual. Multi-Health Systems; Toronto: 2001. [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. Doi: 10.1177/019251396017003001. [Google Scholar]
- Stuart GL, Ramsey SE, Moore TM, Kahler CW, Farrell LE, Recupero PR, Brown RA. Marital violence victimization and perpetration among women substance abusers: A descriptive study. Violence Against Women. 2002;8:934–952. Doi: 10.1177/107780102400447078. [Google Scholar]
- Stuart GL, Ramsey SE, Moore TM, Kahler CW, Farrell LE, Recupero PR, Brown RA. Reductions in marital violence following treatment for alcohol dependence. Journal of Interpersonal Violence. 2003;18:1113–1131. doi: 10.1177/0886260503255550. Do1: 10.1177/0886260503255550. [DOI] [PubMed] [Google Scholar]
- Swearingen CE, Moyer A, Finney JW. Alcoholism treatment outcome studies, 1970-1998: An expanded look at the nature of the research. Addictive Behaviors. 2003;28:415–436. doi: 10.1016/s0306-4603(01)00251-9. Doi: 10.1016/S0306-4603(01)00251-9. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Miller WR. The inventory of drug use consequences (InDUC): Test retest stability and sensitivity to detect change. Psychology of Addictive Behaviors. 2002;16:165–168. Doi: 10.1037//0893-164X.16.2.165. [PubMed] [Google Scholar]