Abstract
Objective
Cognitive behavioral therapy (CBT) is an empirically supported treatment for social phobia. However, not all individuals respond to treatment and many who show improvement do not maintain their gains over the long-term. Thus, alternative treatments are needed.
Method
The current study (N=87) was a 3-arm randomized clinical trial comparing CBT, Acceptance and Commitment therapy (ACT), and a waitlist control group (WL) in participants with a DSM-IV diagnosis of social phobia. Participants completed 12 sessions of CBT or ACT or a 12-week waiting period. All participants completed assessments at baseline and post-treatment, and participants assigned to CBT and ACT also completed assessments at 6 and 12 months following baseline. Assessments consisted of self-report measures, a public speaking task, and clinician ratings.
Results
Multilevel modeling was used to examine between-group differences on outcomes measures. Both treatment groups outperformed WL, with no differences observed between CBT and ACT on self-report, independent clinician, or public speaking outcomes. Lower self-reported psychological flexibility at baseline was associated with greater improvement by the 12-mo follow-up in CBT compared to ACT. Self-reported fear of negative evaluation significantly moderated outcomes as well, with trends for both extremes to be associated with superior outcomes from CBT and inferior outcomes from ACT. Across treatment groups, higher perceived control, and extraversion were associated with greater improvement, whereas comorbid depression was associated with poorer outcomes.
Conclusions
Implications for clinical practice and future research are discussed.
Keywords: social phobia, acceptance and commitment therapy, cognitive behavioral therapy, moderators, predictors, randomized controlled trial
Cognitive behavioral therapy (CBT) is well established as an effective treatment for anxiety disorders. However, a substantial number of patients remain symptomatic and response rates are low. Researchers have advocated better matching of treatments to individuals as one approach towards improving therapy outcomes, which in turn has motivated the search for alternative treatment approaches. Acceptance and commitment therapy (ACT), which emphasizes personal values and cognitive flexibility, offers one such alternative. The current study compares CBT to ACT for social phobia, a highly prevalent condition. Also, we evaluate differential moderators of outcomes for each treatment approach.
The effectiveness of CBT for anxiety disorders is unquestioned. A review of meta-analyses of RCTs involving no-treatment, wait-list or placebo controls reported a comparison-weighted grand mean effect size (Cohen’s d) of .95 from pre- to post- treatment (Butler, Chapman, Forman, & Beck, 2006). Similar results were reported from subsequent meta-analyses (Norton & Price, 2007), with moderate effect sizes (d=.43) when CBT was compared to active treatment comparisons including psychodynamic therapies (Tolin, 2010).
However, several factors have led to the search for different treatment models. Although CBT is statistically superior to control conditions, substantial numbers of patients fail to complete treatment or achieve clinically significant improvement. For example, the attrition rate in studies of CBT for anxiety disorders published since 2000 ranges from 0% to 53% (mean=15.5%, median=12.5%) (Loerinc, Meuret, Twohig, Rosenfield, & Craske, submitted for publication). Of those who complete treatment, the mean response rates (albeit defined in a variety of ways) range from 3% to 100% (mean=52.8%, median=50%) for anxiety disorders (Loerinc et al., submitted for publication). This finding begs for further research to either develop more effective methods overall, or identify which of several different treatment approaches works best for a particular individual.
Second, meta-analyses and reviews have suggested that key components of CBT, such as cognitive restructuring skills aimed at explicitly regulating cognitive errors and somatic regulatory strategies like breathing retraining, do not raise effect sizes or improve outcomes when combined with exposure therapy compared to exposure therapy alone (Norton & Price, 2007).1 As such, the extant data have raised significant concerns about the added value of therapeutic strategies that aim to directly regulate internal states.
Third, there is growing interest in behavioral approaches that do not rely on cognitive restructuring, such as behavioral activation treatment for depression (Dimidjian et al., 2006) and ACT (Hayes, Strosahl, & Wilson, 1999). ACT cultivates mindfulness, acceptance, and cognitive defusion (flexible distancing from the literal meaning of cognitions) to increase psychological flexibility and promote behavior change consistent with personal values. Psychological flexibility is defined as the ability to make contact with one’s experience in the present moment, and, based on what is possible in that moment, choosing behavior in the pursuit of goals and values (Hayes et al., 1999). Thus, ACT does not aim to correct cognitive errors or physiological dysregulation, but rather uses an acceptance-based approach to manage internal experiences. Experimental data support the value of this approach. Instructions for emotional acceptance have been shown to lower distress and increase tolerance for experimentally-induced symptoms of anxiety (Campbell-Sills, Barlow, Brown, & Hofmann, 2006; Levitt, Brown, Orsillo, & Barlow, 2004). In an open trial, patients with panic disorder (n=11) trained to observe and accept rather than control their anxiety during exposures showed decreases in panic symptom severity, on par with what is typically seen in CBT (Meuret, Twohig, Rosenfield, Hayes, & Craske, 2012). In the first randomized controlled trial comparing ACT to CBT in patients diagnosed with anxiety disorders (Arch et al., 2012), comparable outcomes were found between CBT and ACT. However, the sample was comprised of mixed anxiety disorders and was too small to evaluate the relative effects of CBT and ACT for specific anxiety disorders. ACT was also shown to be effective for social phobia in a single case design study (Dalrymple & Herbert, 2007).
The first goal of the current study was to complete the first examination of the efficacy of ACT relative to CBT for social phobia. We focused on social phobia to decrease heterogeneity in this first comparison study and because social phobia is one of the most common anxiety disorders, with lifetime prevalence rates of 16.6% (Kessler, Chiu, Demler, Merikangas, & Walters, 2005). Our second goal was to evaluate moderators of each treatment approach. Moderators establish subgroups of patients who respond differentially to one treatment versus the other, thereby increasing the utility of the findings for making treatment decisions (Kraemer, Wilson, Fairburn, & Agras, 2002). To our knowledge, only two studies have evaluated moderators of treatment outcomes for anxiety disorders in a comparison of two psychological treatments. In a panic disorder sample, Meuret et al. (2010) found that lower perceived control was associated with poorer outcomes from a treatment aimed at changing respiration, whereas higher cognitive misappraisal of anxiety symptoms (i.e., anxiety sensitivity) was related to poorer outcomes from cognitive therapy. In a mixed anxiety disorder sample, (Wolitzky-Taylor, Arch, Rosenfield, & Craske, 2012) CBT outperformed ACT among those with moderate levels of anxiety sensitivity, and with no comorbid mood disorder. Also, there were trends for CBT to outperform ACT at higher levels of experiential avoidance. ACT outperformed CBT among those with a comorbid mood disorder, and there were trends to outperform CBT at lower levels of experiential avoidance. Also, neuroticism was a predictor of poorer outcomes, regardless of treatment condition.
In our mixed anxiety disorder sample, we posited that ACT outperformed CBT among those with mood disorders because, whereas CBT for anxiety disorders targets anxiety symptoms specifically, ACT addresses negative affect globally. We also hypothesized that moderate levels of anxiety sensitivity were optimal for CBT outcomes and outperformed ACT at this level because high anxiety sensitivity may involve beliefs too rigid to modify in a twelve-session protocol, and low anxiety sensitivity may have led to a mismatch with a treatment targeting cognitive misappraisals. The current study sought to examine whether these findings would replicate with a social phobia sample, thereby providing stronger support for these treatment moderators.
Consistent with our previous work, we chose atheoretical (e.g., mood disorder status) and theory-relevant (e.g., experiential avoidance for ACT, fear of negative evaluation for CBT) putative moderators. We hypothesized that CBT would outperform ACT in a socially anxious sample among those who score in the moderate range on a measure of cognitive misappraisals specific to social phobia (i.e., beliefs about being negatively evaluated by others), as this parallels our findings with anxiety sensitivity (a measure of cognitive misappraisals relevant to anxiety generally) in the mixed anxiety disorder sample. Based on our prior study, we hypothesized that CBT would outperform ACT in those with higher experiential avoidance, and that CBT would outperform ACT among those without a comorbid mood disorder whereas ACT would outperform CBT in those with a comorbid mood disorder. We chose to examine perceived emotional control as a putative moderator because of the centrality of this construct to CBT and its antithesis to ACT which emphasizes acceptance rather than control. In line with our previous work showing that higher levels of neuroticism were generally associated with poorer outcomes, we examined whether this finding replicated in a social phobia sample. Finally, we speculated that extraversion would predict better outcomes in general, as extraverted individuals may be more willing to engage in social activities.
Method
Participants
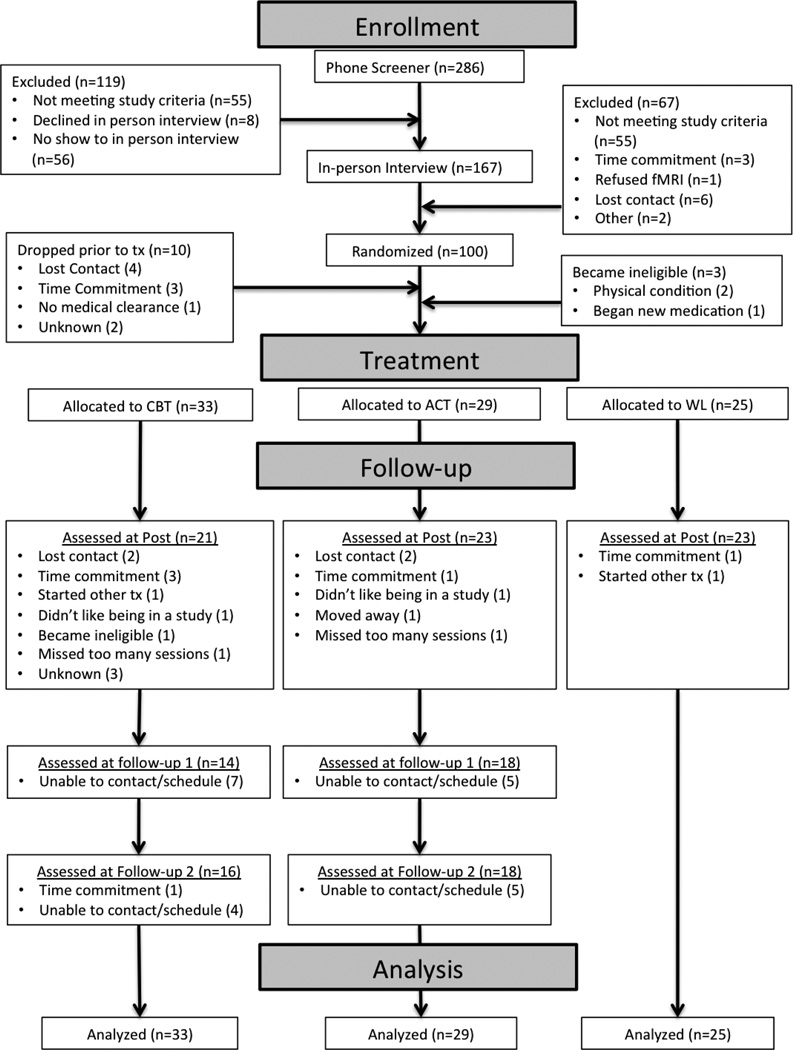
One hundred participants who met DSM-IV criteria for principal or co-principal social phobia, generalized type were randomized to ACT (n=34), CBT (n=40), or Wait List (WL; n=26). All participants who began treatment (n=87) were included in the intent-to-treat (ITT) sample (n=29 ACT, n=33 CBT, n=25 WL). We used a modified intent-to-treat approach in that we did not analyze 10 of the original 100 participants who dropped prior to treatment initiation before they were aware of their randomization to ACT or CBT: they did not differ from non-attriters on sociodemographic variables (ps>.12), clinical severity ratings (p=.85), or assignment to ACT (n=4) vs. CBT (n=5) vs. WL (n=1; p=.48). We chose this modified approach because pre-treatment attrition gave us no information about treatment preference or response. An additional 3 participants were subsequently identified as ineligible.2 See Table 1 for ITT sample characteristics and Figure 1 for patient flow.
Table 1.
Demographic and Clinical Characteristics of Randomized Participants
| Characteristic | TOTAL | CBT | ACT | WL |
F value or χ² |
p |
|---|---|---|---|---|---|---|
| Gender (Female) | 45.98% (40/87) |
42.42% (14/33) |
48.28% (14/29) |
48.00% (12/25) |
.27 | .873 |
| Age, in yearsb | 28.37 (6.76) Range: 19–44 |
29.80 (7.42) |
27.42 (5.56) |
27.64 (7.08) |
1.16 | .320 |
| Education, in years | 15.04 (1.95) Range: 11–19 |
15.55 (1.82) |
15.00 (1.87) |
14.44 (2.10) |
2.36 | .100 |
| Marital Status | 6.91 | .141 | ||||
| Married/Cohabiting | 11.49% (10/87) |
21.21% (7/33) |
0.00% (0/29) |
12.00% (3/25) |
||
| Single | 79.31% (69/87) |
69.70% (23/33) |
89.66% (26/29) |
80.00% (20/25) |
||
| Other | 9.20% (8/87) |
9.09% (3/33) |
10.34% (3/29) |
8.00% (2/25) |
||
| Reported race/ethnicitya | 1.02 | .602 | ||||
| White | 50.57% (44/87) |
57.58% (19/33) |
48.28% (14/29) |
44.00% (11/25) |
||
| Hispanic/ Latino/a | 17.24% (15/87) |
12.12% (4/33) |
17.24% (5/29) |
24.00% (6/25) |
||
| African-American/ Black |
2.30% (2/87) |
3.03% (1/33) |
3.45% (1/29) |
0.00% (0/25) |
||
| Asian-American/ Pacific Islander |
18.39% (16/87) |
15.15% (5/33) |
20.69% (6/29) |
20.00% (5/25) |
||
| Children (1+) | 5.75% (5/87) |
9.09% (3/33) |
3.45% (1/29) |
4.00% (1/25) |
1.01 | .576 |
| Social Phobia clinical severity rating (mean) |
5.59 (.97) Range: 4–7 |
5.73 (.91) |
5.45 (1.02) |
5.56 (1.00) |
.64 | .528 |
| Currently on psychotropic medicationc |
32.18% (28/87) |
27.27% (9/33) |
27.59% (8/29) |
44.00% (11/25) |
2.24 | .325 |
| Comorbid anxiety disorder (1+) d |
22.99% (20/87) |
27.27% (9/33) |
27.59% (8/29) |
12.00% (3/20) |
2.39 | .302 |
| Comorbid depressive disorder d |
18.39% (16/87) |
15.15% (5/33) |
20.69% (6/29) |
20.00% (5/25) |
.38 | .829 |
| Comorbid anxiety or depressive disorder |
22.99% (20/87) |
24.24% (8/33) |
20.69% (6/29) |
24.00% (6/25) |
.13 | .937 |
| Comorbid anxiety and depressive disorder |
9.20% (8/87) |
9.09% (3/33) |
13.79% (4/29) |
4.00% (1/25) |
1.54 | .462 |
For race/ ethnicity, analyses assessed group differences in minority versus white status.
Demographic data was missing for 1 P.
Medications include SSRIs/SNRIs, other antidepressants/mood stabilizers, benzodiazepines and prn medications
Comorbidity was defined as a clinical severity rating of 4 or above on the ADIS
Figure 1.
Patient flow chart
Participants were recruited from local flyers, internet and local newspaper advertisements, and referrals. The study took place at the Anxiety Disorders Research Center at the University of California Los Angeles, Department of Psychology. Participants were either medication-free or stabilized (including medications taken as needed) for 1 month for benzodiazepines and beta blockers and 3 months for SSRIs/SNRIs and heterocyclics). Also, they were psychotherapy-free or stabilized on alternative psychotherapies (not cognitive or behavioral therapies) that were not focused on their anxiety disorder for at least 6 months. Exclusion criteria were active suicidal ideation; severe depression (clinical severity rating>6, see below); history of bipolar disorder or psychosis; substance abuse or dependence within the last 6 months; and respiratory, cardiovascular,3 pulmonary, neurological, muscular-skeletal diseases or pregnancy. Because our study included neuroimaging (results reported elsewhere), additional exclusion criteria were left handedness, metal implants, and claustrophobia.
Design
Participants were assessed prior to treatment (Pre), immediately after treatment (Post), and at 6 months (6MFU) and 12 months (12MFU) after Pre. 6MFU refers to approximately 3 months after treatment completion and 12MFU refers to approximately 9 months after treatment completion. Assessments included a diagnostic interview, self-report questionnaires, and a 2 to 3 hour laboratory assessment that included tasks to assess public speaking, emotion regulation, and attentional bias (the laboratory assessment was not conducted at 6MFU). Participants were stratified by age and gender in CBT, ACT and WL.
Treatments
Participants in the CBT and ACT groups received twelve weekly, 1-hour, individual therapy sessions based on detailed treatment manuals.4 ACT and CBT were matched on number of sessions devoted to exposure but differed in framing of the intent of exposure. Following the 12 sessions, therapists conducted follow-up booster phone calls (20–35 mins) once per month for 6 months to reinforce progress consistent with the assigned therapy condition. The majority completed therapy within 12 to 16 weeks (range 11 – 18 weeks).
Cognitive behavioral therapy
CBT for social phobia was derived largely from standard CBT models (e.g., Hope, Heimberg, Juster, & Turk, 2000). This particular CBT has been effective for individuals with social phobia within larger primary care (Craske et al., 2011) and clinic samples (Arch et al., 2012). Session 1 focused on assessment, self-monitoring, and psychoeducation. Sessions 2–4 emphasized cognitive restructuring errors of overestimation and catastrophizing regarding negative evaluation, combined with hypothesis testing, self-monitoring, and breathing retraining. Exposure to feared social cues (including in-vivo, imaginal, and interoceptive exposure combined with in-vivo exposure) was introduced in Session 5, and emphasized strongly in Sessions 6–11. Cognitive restructuring and breathing retraining were encouraged as coping tools during exposure, with the goal of eventual fear reduction. Session 12 focused on relapse prevention.
Acceptance and commitment therapy
ACT for anxiety disorders followed a manual by Eifert and Forsyth (2005).5 Session 1 focused on psychoeducation, experiential exercises and discussion of acceptance and valued action. Sessions 2–3 explored creative hopelessness, or whether previous efforts to control anxiety had “worked” and how such efforts had led to the reduction of valued life activities, and encouraged acceptance. Sessions 4 and 5 emphasized mindfulness, acceptance and cognitive defusion, or the process of experiencing anxiety-related language (e.g., thoughts, self-talk, etc.) as part of the broader, ongoing stream of present experience rather than getting stuck in responding to its literal meaning. Sessions 6–11 continued to hone acceptance, mindfulness, and defusion, and added values exploration and clarification with the goal of increasing willingness to pursue valued life activities. Behavioral exposures, including interoceptive, in-vivo, and imaginal, were used to practice making room for, mindfully observing, and accepting anxiety and to practice engaging in valued activities while experiencing anxiety. Session 12 reviewed what worked and how to continue moving forward.
Waitlist
WL participants waited to begin treatment for 12 weeks from the date of their baseline fMRI assessment. They rated daily anxiety and depression and were contacted biweekly by the research coordinator who assessed whether symptoms had worsened and whether referrals were warranted (no WL participants were referred out of the study). After Post assessment, participants were offered treatment free of charge, and were able to choose either CBT or ACT. No follow-up assessments were conducted for the WL group.
Therapists
Study therapists were advanced clinical psychology doctoral students and recent PhDs at UCLA with at least two years of supervised training in delivering psychological treatments and at least one year training in CBT or ACT. In addition, therapists completed intensive in-person 2-day workshops for CBT or ACT. Therapists were assigned to ACT, CBT, or both (i.e., treated in both CBT and ACT, though never at the same time), depending on need.6 There were 28 therapists; 13 therapists worked exclusively in CBT, 12 worked exclusively in ACT, and three treated both ACT and CBT participants. There were no differences among therapists who provided CBT, ACT or both in terms of gender, age or years since entering graduate school (p’s>.39). Generally, therapists treated 1–2 patients at a time and 2–5 therapists worked within each treatment condition at a time. The mean number of patients treated by CBT-only therapists was M=2.38, SD=1.56 (range 1–6, total=31 participants), by ACT-only therapists was M=2.67, SD=1.30 (range 1–5, total=32 participants), and by therapists who treated both ACT and CBT was M=5.67, SD=2.52 (range 3–8, total=17 participants).
Weekly, 90-minute group supervision meetings were held separately for CBT and ACT. For CBT, the supervision was led by professors and postdoctoral fellows at UCLA, and was held in person. For ACT, supervision was led by advanced therapists from the University of Nevada, Reno, where ACT was originally developed, via Skype7.
Outcome Measures
Because CBT emphasized symptom reduction whereas ACT emphasized psychological flexibility and valued living, we investigated two sets of primary outcomes: symptom reduction, and quality of life. Also, we investigated outcomes during a public speaking task.
Social anxiety symptoms
Clinical Severity Rating (CSR)
Clinical diagnoses were ascertained using the Anxiety Disorders Interview Schedule-IV (ADIS-IV; Brown, Di Nardo, & Barlow, 1994). Doctoral students in clinical psychology or research assistants served as interviewers after completing 15–20 hours of training and demonstrating adequate diagnostic reliability on 3 consecutive interviews. ‘Clinical severity ratings’ (CSR) were assigned to each disorder on a 0 to 8 scale (0=none, 8=extremely severe). CSR ratings of “4” or higher indicated clinical severity and, in the case of social phobia, served as the cutoff for study eligibility. All interviews were audio-recorded and a subset were randomly selected (n=22) for blind rating by a second interviewer.8 Inter-rater reliability on the principal diagnosis (n=22) was 100%, and on dimensional CSR ratings for social phobia (n=10) was ICC=1.00 (100% agreement).
Fear and avoidance ratings
As part of the ADIS-IV, the clinician rated fear and avoidance, each on a 0 to 8 scale (none to extreme anxiety and avoidance), for 13 social situations (e.g., parties, public speaking, dating, and speaking with unfamiliar people). Scores were summed and ranged from 0 to 208. Cronbach’s αs=.88 (Pre) and .93 (Post). Fear and avoidance ratings are similar in structure and content to the widely used, clinician-administered Liebowitz Social Anxiety Scale (Liebowitz, 1987).
Self-report scales
We selected three widely used and well-validated self-report measures of social anxiety symptoms. The Liebowitz Social Anxiety Scale – Self Report (LSAS-SR; Fresco et al., 2001) is a 24-item measure that assesses fear and avoidance of social interactional and performance situations. Each item is rated on a scale from 0 to 3, with 0=no fear/never avoid and 3=severe fear/usually avoid. Scores were calculated as the sum of fear and avoidance ratings across social and performance situations. In the current sample, Cronbach’s αs=.97 (Pre) and .94 (Post). The Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998) is a 20-item measure of cognitive, affective or behavioral reactions to social interaction in dyads or groups. Participants respond on a Likert scale from 0 (not at all characteristic or true of me) to 4 (extremely characteristic or true of me). Cronbach’s αs=.96 (Pre) and .95 (Post). The Social Phobia Scale (SPS; Mattick & Clarke, 1998) is a 20-item measure describing situations or themes related to being observed by others. Participants rate the extent to which each item is characteristic of them on a 0 to 4 scale. In the current sample, αs=.93 (Pre) and .90 (Post).
Composite scale
A composite was created from the LSAS, SIAS and SPS, to generate a more reliable and valid index of social anxiety symptoms. Z-scores were calculated for each measure at Pre and standardization was based on Pre means and SDs for each subsequent assessment using the equation (time 2 score – time 1 mean)/(time 1 standard deviation). The composite score represented averages of the three measures.
Quality of life
The Quality of Life Inventory (QOLI; Frisch, 1994) assesses 16 life domains and has good test-retest reliability and internal validity (Frisch et al., 2005). The QOLI was selected since its measurement of importance of, as well as satisfaction with, different life domains parallels ACT therapeutic strategies. In the current sample, Cronbach’s αs=.85 (Pre) and .84 (Post).
Subjective Units of Distress (SUDS) during public speaking
During the laboratory assessment, participants spoke before a two-member audience for three minutes on an experimenter-selected topic, while being videotaped. They were given five minutes to prepare their speech. A two-minute anticipation period preceded the speech. Participants who refused to give the speech were offered three alternatives: give the speech with no audience (Pre: n=2, 2.3%; Post: n=2, 3.0%; 12MFU: n=3, 10.0%), read in front of the audience (Pre: n=5, 5.8%; Post: n=1, 1.5%; 12MFU: n=1, 3.3%), or read with no audience (Pre: n=3, 3.5%; Post: n=1, 1.52%; 12MFU: n=0, 0%). Participants rated their anxiety (SUDS) on a scale from 0 to 100 four times: before beginning and at one-minute intervals throughout (mean of the four ratings were analyzed). Those who chose an alternative speaking task were given SUDS ratings of 100.
Moderator Measures
Demographics
Demographic information (i.e., age, gender, and ethnicity) was collected during the ADIS-IV interview.
Theory-relevant moderators
The 10-item Self Statements During Public Speaking questionnaire (Hofmann & DiBartolo, 2000) assesses fears of negative evaluation. After public speaking, participants rated the extent to which they experienced five negative and five positive thoughts during the speaking task. Sample items include “I’m a loser” and “What I say will probably sound stupid.” The SSPS shows good internal consistency (α=.86) and test-retest reliability (r=.80) (Hofmann & DiBartolo, 2000). Mean ratings for negative thoughts are analyzed in the current sample: αs were .88 (Pre) and .90 (Post). The 16-item Acceptance and Action Questionnaire-16 (AAQ; Hayes et al., 2004) assesses psychological flexibility (Bond et al., 2011). Sample items include “It’s OK to feel depressed or anxious” and “There are not many activities that I stop doing when I am feeling depressed or anxious.” The AAQ is sensitive to clinical change, and has good internal consistency (α=.70) and test-retest reliability (r=.64) (Hayes et al., 2004). One and two-factor solutions have been fit to the 16-item AAQ (Bond & Bunce, 2000). Herein, a one-factor scale was used, with higher scores indicating greater psychological flexibility: αs were .83 (Pre) and .88 (Post).
Comorbidity, personality and perceived control
From the ADIS-IV, we examined co-occurring anxiety disorders (yes=1 and no=0) and co-occurring mood disorders (yes=1 and no=0) with a CSR of 4+. The Eysenck Personality Questionnaire (EPQ; Eysenck & Eysenck, 1975) assessed neuroticism and extroversion, each with 12 yes-no items. Items were summed and higher scores represent higher neuroticism or extroversion. The questionnaire is well validated in adult samples, and neuroticism and extroversion consistently emerge as distinct personality factors (Kline & Barrett, 1983). Current αs for neuroticism were .86 (Pre) and .84 (Post) and for extroversion were .90 (Pre) and .85 (Post). The Anxiety Control Questionnaire (ACQ; Rapee, Craske, Brown, & Barlow, 1996) assesses perceived control over anxiety. We used the revised 15-item version (Brown, White, Forsyth, & Barlow, 2004). Participants identify how much they agree with each statement with higher scores indicating greater perceived control. The 15-item version has demonstrated adequate reliability (Brown et al., 2004). Current αs were .89 (Pre) and .90 (Post).
Treatment Credibility
Prior to the second therapy session, after treatment rationales, participants completed a 6-item treatment credibility questionnaire adapted from Borkovec and Nau (1972) (α=.95).
Treatment Adherence and Therapist competence
45 audio-taped sessions from 24 participants (12 in CBT, 12 in ACT) were randomly selected for treatment adherence and therapist competency ratings using the Drexel University ACT/CT Therapist Adherence and Competence Rating Scale (McGrath, Forman, & Herbert, in preparation) which yielded five adherence items scales: general therapy adherence (7 items), general behavioral therapy adherence (7 items), cognitive therapy adherence (9 items), ACT adherence (11 items), and therapist competence (5 items). A blind rater who had no involvement with the study, but had extensive training in both ACT and CBT and had previously rated over 200 therapy sessions of ACT and CBT noted which adherence item occurred in each 5-minute segment of therapy. Adherence scale scores were the percentage of time spent on treatment-specific behavior (0=no time spent; 1=entire session was devoted to the treatment-specific behavior). Overall adherence scores ranged from .17 to 1.0. Therapist competence was rated on 5 items (e.g., “knowledge of treatment,” “skill in delivering treatment,” and “relationship with client;” 1=poor, 3=good, 5=excellent) and the mean was calculated. Rater reliability was assessed from audio-taped sessions from the current study and an earlier study using the same treatment protocols (Arch et al., 2012). Inter-rater reliability on 35 sessions was excellent (ICCs for scales ranged from .78 to .97). Intra-rater reliability of the primary rater, which was assessed on 18 sessions, was excellent (ICCs for scales ranged from .98 to 1.0).
Statistical Analyses
Raw data were inspected graphically; one outlier (+/- 3SD) was replaced with the next highest value using the Winsor method (Guttman, 1973).9 Longitudinal data were analyzed with multi-level modeling (MLM) in Stata 12.0 using the xtmixed command. MLM accounts for nesting of time-points within subjects, allowing examination of within and between subject change across Time (Pre, Post, 6MFU, 12MFU) and by group (ACT, CBT and WL). MLM includes participants with missing data and uses all available data to estimate the models. To test whether data were missing at random, participant dropout was coded using a dummy variable (0=no dropout, 1=dropout), and models were run controlling for dropout status using the guidelines proposed by Hedeker and Gibbons (2006). Results did not differ between models that included dropout as a predictor and those that did not. Residuals were normally distributed across all models.
Main effects of treatment
In the MLM, Time was modeled at Level 1 (Pre, Post, 6MFU, 12MFU) using a piecewise approach (e.g. Roy-Byrne et al., 2005), which specifies a linear segment between Pre and Post (S1), and another linear segment for the subsequent 6MFU and 12MFU (S2). The two segments, S1 and S2, meet at Post. This approach models typical trends in treatment studies, where the greatest effects occur by Post and change levels off over follow-up. Treatment group (CBT, ACT, WL) was included at Level 2. All models included random effects of the intercept, and random effects for S1 and S2 were included when significant. Unstructured versus heterogeneous variance/covariance structures were examined for model fit using likelihood ratio tests. The model with the best fit was selected, and if models did not significantly differ, the model with the fewest parameters was chosen. The variance/covariance structure of Level 1 residuals was modeled as independent (which was not significantly different from an autoregressive or exchangeable structure). Between-group differences were assessed via marginal means at each time point, and by comparing S1 in ACT, CBT and WL, and S2 in ACT and CBT. The MLM equation for a model with random effects for the intercept only is depicted below:
L1:
Yti=b0i+b1iS1i+b2iS2i+eti
L2:
b0i=g00 + g01CACT+g02CWL+ u0i
b1i=g10 + g11CACT+g12CWL
b2i=g20 + g21CACT
Yti=Score on dependent variable (DV) at time t for individual i; S1i=Immediate treatment effect; S2i=Follow-up treatment effect; CACT=Treatment Group (0=CBT, 1=ACT); CWL=Treatment Group (0=CBT, 1=WL); b0i=intercept of the DV for individual i; b1i and b2i=growth parameters; g00=mean score on DV at Pre in CBT; g01=mean difference between score on DV at Pre in ACT vs. CBT; g02=mean difference between score on DV at Pre in WL vs. CBT; g10=mean change on DV at Post in CBT; g11=mean difference between change on DV at Post in ACT vs. CBT; g12=mean difference between change on DV at Post in WL vs. CBT; g20=mean change in DV at each subsequent follow up in CBT; g21=mean difference in change in DV at each subsequent follow-up between ACT vs. CBT; u0i=random error component for the deviation of the intercept of an individual i from the overall intercept; eti= level 1 variance at time t for individual i.
Moderated effects
Consistent with prior studies of moderators (Wolitzky-Taylor et al., 2012), we chose a MLM, repeated measures analysis of covariance (ANCOVA)-like design, implemented using the xtmixed command in Stata 12.0. Pre values of the dependent measures were included as a covariate, and Post, 6MFU, and 12MFU were levels of the repeated measures independent variable (Time). Therefore, only participants with Post scores were included in the moderator analysis.10 Intercept was included as a random effect, and the variance/covariance structure of the Level 1 residuals was modeled as independent.
Between subjects variables consisted of Group (CBT or ACT; WL was not included in moderator analyses), Pre level of the dependent variable (as a covariate), and moderators. A separate MLM analysis was performed for each moderator. Interactions with Group and Time and the triple interaction between moderator, Group, and Time were included. Quadratic terms for the moderator and its interaction with Group and Time were tested. When non-significant, the quadratic term was dropped and linear relationships were tested. Similarly, when Time did not significantly interact with the moderator or Group, Time was dropped and two-way interactions were tested. Moderator analyses were limited to composite symptoms and fear and avoidance outcomes; CSR was excluded due to limited range in the data, and anxiety during public speaking was excluded due to a non-normal distribution that produced inaccurate parameter estimates in the model.
Results
Pre-Treatment Group Differences
No significant differences emerged between ACT, CBT and WL on any outcome measures at Pre (ps>.495). No group differences were found in previous or concurrent use of psychotherapy [CBT=52%, 17/33, ACT=55%, 16/29, WL=72%, 18/25, χ2 (df=2)=2.67, p=.263] or psychotropic medication [CBT=27%, 9/33, ACT=28%, 8/29, WL=44%, 11/25, χ2 (df=2)=2.24, p=.302] (see Table 1). ACT, CBT and WL did not differ on socio-demographic or clinical characteristics at Pre (Table 1).
Treatment Credibility
Treatment credibility ratings did not differ significantly between ACT (M=4.83, SD=2.5) and CBT (M=4.2, SD=2.4), t(60)=−1.02, p=.311.
Therapist Competence and Treatment Integrity
Therapist competence scores indicated “good” therapist skills in CBT (M=3.06, SD=.67) and ACT (M=3.21, SD=.57) that did not significantly differ, t(42)=−.76, p=.449. As expected, cognitive therapy adherence was higher in CBT (M=.55, SD=.29) than ACT (M=.05, SD=.06), t(42)=7.87, p<.001, and ACT adherence was higher in ACT (M=.87, SD=.17) than CBT (M=.04, SD=.08), t(42)=−20.19, p<.001. Scores for adherence to behavioral exposure were higher in CBT (M=.61, SD=.29) than ACT (M=.16, SD=.23), t(42)=5.68, p<.001. Overall, therapy adherence ratings were higher in ACT (M=.87, SD=.17) than CBT (M=.55, SD=.29), t(42)=−4.56, p<.001, although therapists adhered strongly to their assigned treatments in both groups.
Regression analyses were conducted within the subsample of participants whose sessions had been rated to test whether therapist adherence to behavioral exposures was a significant predictor of symptoms, clinical severity rating, fear and avoidance ratings, quality of life, and SUDS during public speaking at Post, controlling for symptoms at Pre. Adherence to behavioral exposure was not a significant predictor of any outcome (ps > .233). In addition, therapist rated homework compliance averaged across sessions 6 to 12 (sessions in which exposure was emphasized) was examined as a predictor of the five treatment outcomes at Post. Homework compliance did not significantly predict any outcome (ps > .302).
Treatment Attrition
46 of 62 participants (74%) completed all 12-treatment sessions: CBT=67% (22/33), ACT=83% (24/29). Two completed one session and 14 completed between 2 and 11 sessions. Attrition did not differ between CBT and ACT, χ2 (df=1)=2.09, p=.149. One participant dropped from WL.
Treatment Outcomes
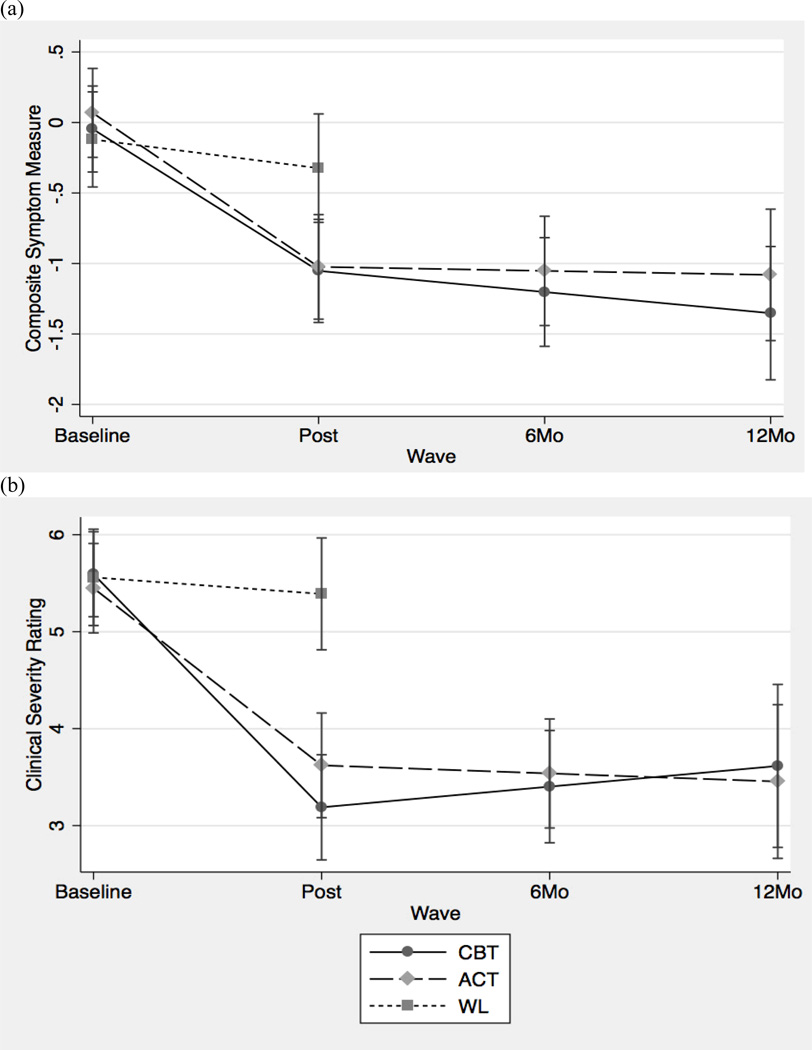
First, p-values from the Group × Time interaction are presented for S1 (modeling Pre to Post) and S2 (modeling Post through 12MFU). S1 compares ACT, CBT and WL, and S2 compares ACT and CBT. Second, for significant Group × Time interactions, we present beta values for pair-wise slope comparisons (i.e., simple effects) and associated p-values. Third, p values for S1 and S2 within each group are presented, comparing whether each slope differs significantly from zero. Results are displayed in Figure 2. Estimated means and 95% confidence intervals (CI) from the piecewise model for each group are displayed in Table 2. CIs and effect sizes for pair-wise group slope comparisons11 are displayed in Table 3.
Figure 2.
Main effects of cognitive behavioral therapy (CBT), acceptance and commitment therapy (ACT) and wait-list (WL) on (a) social anxiety symptom composite and (b) clinical severity rating.
Table 2.
Estimated means and confidence intervals at each time-point for cognitive behavioral therapy (CBT), acceptance and commitment therapy (ACT), and waitlist (WL).
| CBT | ACT | WL | |
|---|---|---|---|
| SYMPTOMS | |||
| Composite Symptom Scale | |||
| Baseline | −0.1 (−0.4 to 0.3) | 0.1 (−0.3 to 0.4) | −0.1 (−0.5 to 0.2) |
| Post | −1.1 (−1.4 to −0.7) | −1.0 (−1.4 to −0.7) | −0.3 (−0.7 to 0.1) |
| 6 mo | −1.2 (−1.6 to −0.8) | −1.1 (−1.4 to −0.7) | -- |
| 12 mo | −1.4 (−1.8 to −0.9) | −1.1 (−1.5 to −0.6) | -- |
| Clinical Severity Rating | |||
| Baseline | 5.7 (5.3 to 6.0) | 5.4 (5.0 to 5.8) | 5.6 (5.2 to 6.1) |
| Post | 3.2 (2.7 to 3.8) | 3.6 (3.1 to 4.1) | 5.3 (4.7 to 5.9) |
| 6 mo | 3.2 (2.7 to 3.8) | 3.5 (3.0 to 4.0) | -- |
| 12 mo | 3.2 (2.5 to 4.0) | 3.4 (2.7 to 4.1) | -- |
| Fear & Avoidance Ratings | |||
| Baseline | 97.1 (87.8 to 106.5) | 99.2 (89.2 to 109.2) | 103.28 (92.5 to 114.0) |
| Post | 64.5 (52.0 to 77.0) | 77.4 (64.8 to 90.1) | 99.5 (86.1 to 112.9) |
| 6 mo | 63.0 (51.2 to 74.8) | 72.4 (60.6 to 84.3) | -- |
| 12 mo | 61.5 (54.2 to 80.7) | 67.4 (54.2 to 80.7) | -- |
| QUALITY OF LIFE | |||
| QOLI (weighted average) | |||
| Baseline | 0.4 (−0.2 to 1.0) | 0.5 (−0.2 to 1.1) | 0.0 (−0.7 to 0.8) |
| Post | 0.8 (0.1 to 1.5) | 0.5 (−0.2 to 1.2) | 0.1 (−0.6 to 0.8) |
| 6 mo | 0.8 (0.2 to 1.5) | 0.7 (0.1 to 1.4) | -- |
| 12 mo | 0.9 (0.2 to 1.6) | 0.9 (0.2 to 1.6) | -- |
| PUBLIC SPEAKING | |||
| SUDS during public speaking | |||
| Baseline | 60.5 (51.4 to 69.6) | 64.6 (55.2 to 74.0) | 67.8 (57.4 to 78.1) |
| Post | 34.0 (23.0 to 44.9) | 41.9 (31.5 to 52.3) | 51.4 (40.9 to 62.0) |
| 12 mo | 41.9 (29.5 to 54.2) | 31.0 (19.3 to 42.8) | -- |
Table 3.
Estimated slopes (change) from Pre to Post treatment (S1) and post to 12MFU (S2), and effect sizes (Cohen’s d) for pair-wise group slope comparisons for CBT vs. ACT, ACT vs. WL and CBT vs. WL
| CBT | ACT | WL | CBT vs. |
ACT vs. |
CBT vs. |
|
|---|---|---|---|---|---|---|
| beta (95% CI) | beta (95% CI) | beta (95% CI) | ACT d12 |
WL d |
WL d |
|
| SYMPTOMS | ||||||
| Composite Symptom Scale | ||||||
| S1 | −1.0 (−1.3 to −.7)*** | −1.1 (−1.4 to −0.8)*** | −0.2 (−0.5 to 0.1) | 0.11 | .97 | 1.02 |
| S2 | −0.1 (−0.3 to 0.0) | 0.0 (−0.2 to 0.1) | -- | 0.23 | -- | -- |
| Clinical Severity Rating | ||||||
| S1 | −2.4 (−3.0 to −1.9)*** | −1.8 (−2.4 to −1.2)*** | −0.3 (−0.9 to 0.3) | 0.62 | 1.51 | 2.19 |
| S2 | 0.0 (−0.3 to 0.4) | −0.1 (−0.4 to 0.2) | -- | 0.16 | -- | -- |
| Fear & Avoidance Ratings | ||||||
| S1 | −32.6 (−44.1 to −21.2)*** | −21.8 (−33.2 to −10.3)*** | −3.8 (−15.8 to 8.2) | .43 | .60 | 1.04 |
| S2 | −1.5 (−7.1 to 4.1) | −5.0 (−10.2 to 0.2) | -- | .31 | -- | -- |
| QUALITY OF LIFE | ||||||
| QOLI (higher numbers indicate improvement) | ||||||
| S1 | 0.4 (−0.1 to 0.9) | 0.1 (−0.4 to 0.5) | 0.1 (−0.4 to 0.6) | 0.23 | 0.00 | 0.26 |
| S2 | 0.0 (−0.2 to 0.3) | 0.2 (−0.1 to 0.5) | -- | 0.17 | -- | -- |
| PUBLIC SPEAKING | ||||||
| SUDS during speech | ||||||
| S1 | −26.6 (−38.3 to −14.8)*** | −22.7 (−33.9 to −11.6)*** | −16.3 (−27.9 to −4.8)** | 0.15 | 0.26 | 0.44 |
| S2 | 3.9 (−3.0 to 10.9) | −5.4 (−11.8 to 1.0) | -- | 0.80 | -- | -- |
Symptom outcomes
The Time × Group interaction for composite symptoms was significant for S1 (p<.001) but not for S2 (p=.318). For S1 pair-wise group slope comparisons, CBT had larger reductions in symptoms than WL (b=.80; CI=.40 to 1.2; p<.001), as did ACT (b=.88; CI=.1.3; .49 to 1.3; p<.001), whereas CBT and ACT slopes did not differ from each other (b=−.09; CI=−.49 to .32; p=.675). S1 change slopes indicated composite symptom reductions in CBT (p<.001) and ACT (p<.001), but not WL (p=.158). S2 change slopes were not significant in CBT (p=.089) or ACT (p=.736).
The Time × Group interaction for clinical severity ratings was significant for S1 (p<.001) but not for S2 (p=.629). For S1 pair-wise group slope comparisons, CBT had larger reductions in clinical severity than WL (b=2.13; CI=−1.29 to 2.98; p<.001), as did ACT (b=1.52; CI=.68 to 2.37; p<.001), whereas CSR slopes did not differ between CBT and ACT (b=.61; CI=.20 to −1.43; p=.140). S1 change slopes indicated significant clinical severity reduction in CBT (p<.001) and ACT (p<.001), but not WL (p=.343). S2 change slopes were not significant in CBT (p=.974) or ACT (p=.501).
The Time × Group interaction for fear and avoidance ratings was significant for S1 (p=.003) but not for S2 (p=.366). For S1 pair-wise group slope comparisons, CBT showed larger reductions in fear and avoidance than WL (b=28.85; CI=12.3 to 45.4; p=.001), as did ACT (b=18.00; CI=1.4 to 34.6; p=.033), whereas the slopes did not differ between CBT and ACT (b=−10.86; CI=−27.0 to 5.3; p=.188). S1 change slopes indicated significant fear and avoidance reduction in CBT (p<.001) and ACT (p<.001), but not WL (p=.538). S2 change slopes were not significant in CBT (p=.605) or in ACT (p=.060).
Quality of life
The Time × Group interaction for quality of life was not significant for S1 (p=.539) or S2 (p=.427). S1 change slopes were not significant for CBT (p=.096) , ACT (p=.788) or WL (p=.774). S2 change slopes were not significant for CBT (p=.783) or ACT (p=.146). Because graphical inspection of means yielded a linear as opposed to piecewise change in quality of life, analyses were re-run with Time modeled as a continuous linear predictor for CBT and ACT groups. The Time × Group interaction was not significant (p=.937), but there was a main effect of Time (b=.16; CI=.03 to .28; p=.015) reflecting improvement in quality of life over the four assessment time-points regardless of treatment group.
Public speaking
The Time × Group interaction was not significant for subjective distress during public speaking for S1 (p=.469) or for S2 (p=.051). S1 change slopes indicated a significant reduction in subjective distress in CBT (p<.001), ACT (p<.001) and WL (p<.001). S2 change slopes were not significant in ACT (p=.096) or in CBT (p=.265).
Clinically Significant Improvement
Participants were classified as having achieved clinically significant improvement if (a) their clinical severity rating for social phobia was ≤ 3; and (b) they showed statistically reliable change on either of the companion scales of performance (SPS) or interactional (SIAS) anxiety. Reliable change was calculated as outlined by Jacobsen and Truax (1991) using Maasen’s (2004) more conservative denominator. Rates at Post were as follows: CBT=52.3% (n=11/21), ACT=40.9% (n=9/22), and WL=4.3% (n=1/23); χ2 (N=66, df=2)=12.93, p=.001. CBT and ACT both outperformed WL, χ2 (N=44, df=1)=12.77, p<.001 and χ2 (N=45, df=1)=8.70, p<.01, respectively, with no differences between CBT and ACT (p=.45). 6MFU rates were CBT=57.1% (n=8/14) and ACT=53.3% (n=8/15) (p=.84). 12MFU rates were CBT=40.0% (n=6/15) and ACT=41.2% (n=7/17) (p=.95). These percentages dropped slightly when carrying the last observation forward in an intent-to-treat analysis: Percentages of those achieving clinically significant change are 47.8%, 37.5%, and 4.3% for CBT, ACT, and WL, respectively, at post-treatment; 56.5% and 41.7% for CBT and ACT, respectively, at 6MFU; and 47.8% and 33.3% for CBT and ACT, respectively, at 12MFU.
Additional Psychotherapy and Medication
From Post to 12MFU, 8 stopped psychotropic medication (CBT=3, ACT=5) and 3 began medication (CBT=2, ACT=1). Over the same interval, no participant ended psychotherapy and 4 began new psychotherapy (CBT=0, ACT=4) (all between 6MFU and 12MFU).
Moderators and Predictors
Moderators and predictors were evaluated in terms of self-reported composite symptoms and independent clinician ratings of fear and avoidance. Each variable was first tested for moderation (interaction between group and moderator), and if not significant, then tested as a predictor (main effect).
Demographic
Moderator
Gender, age and ethnicity did not significantly moderate composite symptoms or fear and avoidance ratings (ps>.062).
Predictor
Gender was a significant predictor of composite symptoms (z=2.01, p=.044), with women reporting fewer symptoms than men (b=−.43; CI=−.011 to −.84), collapsed across groups and follow-up assessments. The same effect was found for fear and avoidance ratings (z=1.64 p=.024) with women rated as less fearful and avoidant than males (b=−16.60; CI=−2.13 to −31.06) collapsed across groups and follow-up assessments. Neither age nor ethnicity was a significant predictor of either outcome (ps>.230).
Theoretically relevant
Moderator
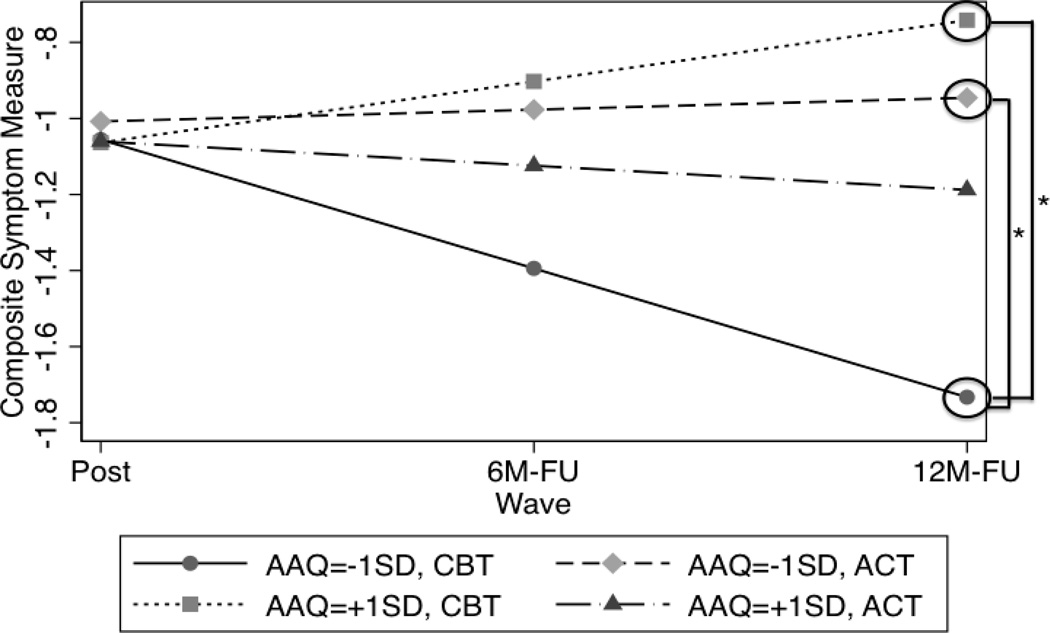
The linear experiential avoidance (AAQ) term interacted with Group and Time to moderate composite symptoms χ2 (N=44, df=1)=4.04, p=.044. As shown in Figure 3, tests of simple effects revealed a significant interaction at 12MFU. For participants 1 SD below the mean on AAQ (higher experiential avoidance), CBT showed greater symptom reduction than ACT (b=1.03; CI=.055 to 2.01; p=.038). In addition, within CBT, participants 1 SD below the mean on AAQ (higher experiential avoidance) showed greater symptom reduction than those 1 SD above the mean (b=1.49; CI=.034 to 2.95, p=.045). Experiential avoidance did not moderate fear and avoidance ratings (ps>.510).
Figure 3.
Group × Time moderation of cognitive behavioral therapy (CBT) and acceptance and commitment therapy (ACT) by experiential avoidance (Acceptance and Action Questionnaire; AAQ) on social anxiety symptom composite
Note. * p<.05; −1SD=1 standard deviation below the mean on AAQ; +1SD=1 standard deviation above the mean on AAQ
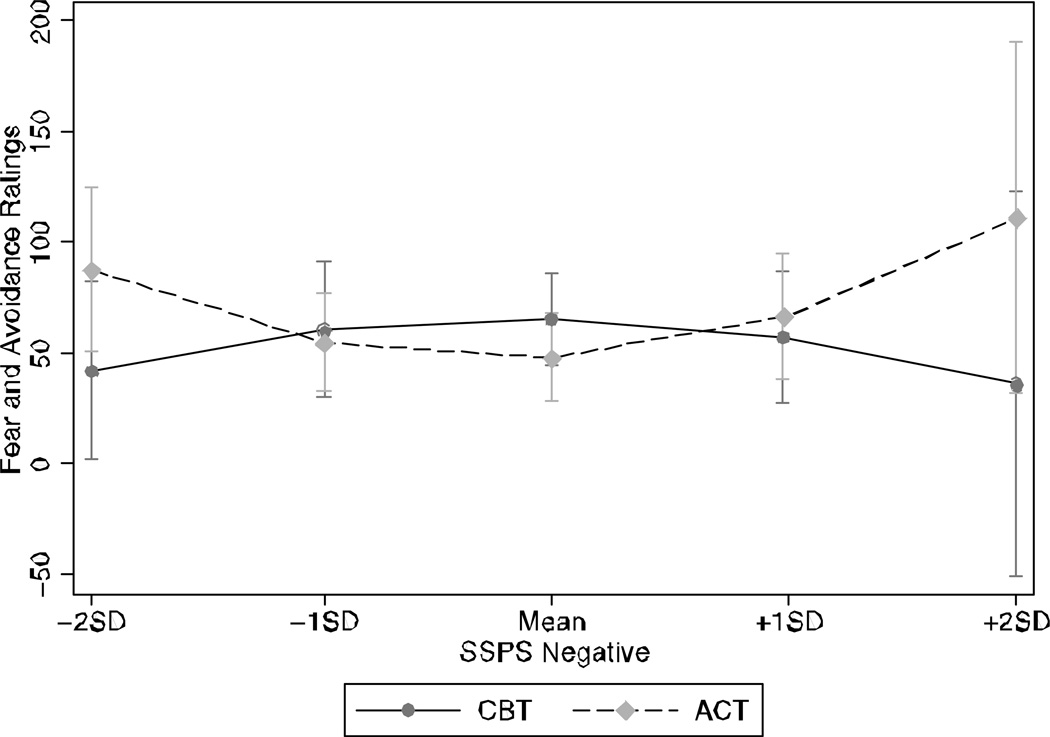
The quadratic fear of negative evaluation (SSPS) term significantly interacted with Group and Time to moderate fear and avoidance ratings χ2 (N=50, df=1)=7.48, p =.01. However, tests of simple effects revealed that the groups did not significantly differ from one another at any value of SSPS from 2 standard deviations below to 2 standard deviations above the mean at Post, 6 or 12MFU (ps>.102). Although no significant simple effects were found, the groups showed inverse curvilinear relationships between fear of negative evaluation and outcomes (see Figure 4). Fear of negative evaluation did not moderate composite symptoms (ps>.223).
Figure 4.
Moderation of cognitive behavioral therapy (CBT) and acceptance and commitment therapy (ACT) by fear of negative evaluation (Self Statements During Public Speaking (Negative); SSPS) at 12-Month Follow-up
Predictor
Experiential avoidance did not predict fear and avoidance ratings (p>.212) and fear of negative evaluation did not predict composite symptoms (p>.456).
Comorbidity, personality and perceived control
Moderator
Comorbid depression, extroversion, perceived control, comorbid anxiety and neuroticism did not significantly moderate composite symptoms or fear and avoidance ratings (ps>.065).
Predictor
Comorbid depression significantly predicted fear and avoidance ratings (z=2.28, p=.023), with patients with comorbid depression rated as more fearful and avoidant (b=23.8; CI=3.33 to 44.33). Extroversion was a significant linear predictor of composite symptoms (z=1.96, p=.05). Participants higher in extroversion reported significantly fewer symptoms (b=−.08; CI=0 to −.16), collapsed across groups and follow-up assessments. The same direction of effect was found for fear and avoidance ratings (z=2.16 p=.031), with those higher in extraversion rated as less fearful and avoidant (b=−.272; CI=−.25 to −5.20). Perceived control was a significant predictor of fear and avoidance ratings (z=2.00 p=.045), with patients higher in perceived control reporting lower fear and avoidance (b=−.73; CI=−.016 to −1.44), collapsed across group and follow-up assessments. Neither comorbid depression nor perceived control predicted composite symptoms (ps=.067), and neither comorbid anxiety nor neuroticism significantly predicted either outcome (ps>.186).
Discussion
The goals of this study were to compare the efficacy of CBT and ACT for social phobia, and to assess which variables at baseline functioned as indicators of participants who did best with either treatment approach. Broadly speaking, the two treatments did not differ from each other in terms of self-report, independent clinician, or public speaking outcomes, with each treatment superior to the wait-list control on the majority of measures. CBT fared better than ACT in individuals with higher experiential avoidance, and there were trends for superior outcomes from CBT and inferior outcomes from ACT at the extreme ends of fear of negative evaluation. Also, individuals without comorbid depression or who were higher in extraversion or perceived control fared better than their counterparts with either treatment approach.
We measured treatment outcome using self-report measures of symptoms and quality of life, independent clinician ratings of fear and avoidance of social situations and overall clinical severity, and anxiety during a public speaking task. These measures were repeated at pre-treatment, post-treatment, and six months and twelve months following pre-treatment (excepting absence of the public speaking task from the six-month assessment). The outcomes from CBT and ACT were remarkably consistent across measurement modality and across timing of assessment. One exception was a trend for ACT to show greater reductions in anxiety during public speaking from post to the 12-month follow-up than CBT. The results are generally consistent with a prior study (Arch et al., 2012), where few differences were found in outcomes between the two treatments for a mixed anxiety disorder sample, excepting greater improvements from post to follow-up on clinical severity ratings for ACT than CBT. In the current study, ACT and CBT produced similar rates of clinically significant improvement, that were comparable to published mean response rates for CBT for social phobia: 46% at post-treatment (12 studies, 29 data points) and 52.9% at follow-up (3 studies, 10 data points) (Chen et al., 2007; Davidson et al., 2004; Olivares et al., 2002; Piet, Hougaard, Hecksher, & Rosenberg, 2010; Spence, Donovan, & Brechman-Toussaint, 2000; Stangier, Heidenreich, Peitz, Lauterbach, & Clark, 2003; Tillfors et al., 2008). Very few studies have used reliable change index methods to compute treatment response rates but the few that have (Stangier et al., 2003; Tillfors et al., 2008) evidence response rates comparable to those in the present study.
The lack of differences between CBT and ACT is not due to lack of effectiveness, since the two treatment conditions yielded superior outcomes to a wait-list comparison on most outcomes. That being said, clinically significant improvement rates in the active treatment conditions of 40% to 57% beg the question of what can be done to improve outcomes. The search for moderators aims to improve outcomes. There were two measures on which differences from the wait-list control were not observed, the first being the self-report measure of quality of life, on which no group improved significantly by post-treatment. Yet, quality of life did significantly improve over the full 12-month period in treated participants. These data suggest that changes in quality of life may take longer than symptom changes, which is consistent with prior evidence for changes in quality of life by the 12 month follow-up, albeit more so following CBT than ACT (Arch et al., 2012). It is also possible that larger treatment effects, and even differences between ACT and CBT, would have been observed with more sensitive and multiple measures of quality of life. The second measure was anxiety during public speaking, on which all groups, including the wait-list group, improved significantly from pre to post. These data suggest that repetition of the public speaking task was alone sufficient to yield significant improvements in anxiety, although improvements that did not generalize to other measures of social anxiety severity. The findings raise concerns about the value of such public speaking tasks as a measure of treatment effectiveness in the absence of controls for repeated assessment.
The lack of outcome differences between ACT and CBT is also not due to confounding by baseline severity, acceptability of treatment, or delivery of treatment. That is, individuals assigned to ACT or CBT did not differ on baseline demographic or clinical variables. Nor did they differ in their rate of attrition or their perceived credibility in the treatment. Also, the two treatments were delivered with equivalent competency, as judged by an independent rater. Confounding influences from therapist allegiance were deemed unlikely given the junior status of the therapists. Rates of removal and addition of pharmacotherapy were equivalent across the two active treatment groups. Notably, whereas four participants in ACT added a new psychotherapy (although none achieved clinically reliable change despite additional therapy), none did so in CBT. Similarly, in the prior study, significantly more ACT participants continued or began new psychotherapy compared to CBT participants (Arch et al., 2012),. It is unclear why ACT would increase or sustain involvement in psychotherapies.
Although involvement in alternative psychotherapy clouds the group comparison, the results indicate that individuals with social phobia will, on average, respond as well to ACT as they do to CBT. The results may derive from procedures and processes that are shared in common between these approaches. Similarities between ACT and CBT are discussed elsewhere (Arch & Craske, 2008). These include exposure to, rather than suppression of, anxious thoughts; active effort to deal with anxious thoughts; and attainment of strategic control over emotions albeit via different paths. The results may also derive from the common element of exposure therapy. As was the case in the earlier comparison of ACT and CBT for a mixed anxiety sample (Arch et al., 2012), the two treatments in the current study were structured to be equated on the amount of exposure to feared situations, albeit presented with different rationales (i.e., to gain control over fear responding in CBT and to achieve actions consistent with life values in ACT). Given the potency of exposure for anxiety disorders (e.g. Norton & Price, 2007), it is conceivable that the shared component of exposure overrode other differences between the two treatments, and thereby equated their effects. Overall, the current findings add to the growing body of literature supporting the efficacy of acceptance-based approaches as a viable alternative to cognitive behavioral therapies that aim to regulate internal (somatic and cognitive) state, at least given equivalent amounts of exposure to feared situations.
Our second goal was to discover whether certain subgroups of individuals would respond more positively to either treatment approach. Based on the prior study with a mixed anxiety disorder sample (Wolitzky-Taylor et al., 2012), we hypothesized that CBT would outperform ACT in those with moderate levels of fear of negative evaluation, without comorbid depression, and higher experiential avoidance, whereas ACT would outperform CBT in those with comorbid depression and lower experiential avoidance. Individuals with higher experiential avoidance fared better in terms of self-reported symptoms with CBT than ACT by the 12-month follow-up assessment; psychological flexibility had no bearing on response to ACT. Superior CBT outcomes as a function of higher experiential avoidance mirrors trends in the prior study (Wolitzky-Taylor et al., 2012). Theoretically, one might assume that those with the highest levels of experiential avoidance would respond best to a treatment designed to decrease such avoidance by increasing psychological flexibility (i.e., ACT). However, the current results suggest that high levels of experiential avoidance are a better match with the tenants of CBT. As discussed in Wolitzky-Taylor et al. (2012), perhaps those in CBT with high levels of experiential avoidance were more motivated to practice CBT skills in an effort to decrease negative affect. Given that this moderating effect occurred during the follow-up period, it is also possible that for those who began treatment with more experiential avoidance, CBT increased psychological flexibility more than did ACT, thereby leading to more engagement in self-directed exposure during the follow-up period for those who had received CBT. Another possibility is that lower levels of adherence to exposure in ACT were particularly detrimental to those with more avoidance at baseline, although the same reasoning cannot be applied to the earlier study (Wolitzky-Taylor et al., 2012) where ACT and CBT did not differ in terms of exposure adherence. Finally, results should be interpreted cautiously given that the moderating effect of experiential avoidance was found only for self-reported symptoms and not for fear and avoidance ratings.
Over and above symptom severity, our measure of fear of negative evaluation, the SSPS, significantly moderated clinician-rated outcome, although interpretation is tempered by lack of significant simple effects. Visual inspection revealed inverse curvilinear relationships, with individuals scoring either the highest or the lowest on fears of negative evaluation tending to fare better with CBT and worse with ACT. Thus, the current results contrast with the prior report in which moderate levels of anxiety sensitivity led to better outcomes from CBT whereas they did not affect ACT (Wolitzky-Taylor et al., 2012), and with the report by Meuret et al. (2010) where higher levels of anxiety sensitivity led to poorer response to cognitive therapy and greater response to capnometry assisted respiratory training. Conceivably, fear of negative evaluation for social anxiety does not function in the same way as anxiety sensitivity for panic disorder or for mixed anxiety disorders. As the moderating effect of fear of negative evaluation was found only for clinician-rated outcomes and not for self-reported symptoms, and was not supported by significant simple effects analyses, it should be interpreted cautiously.
Several predictors of overall treatment outcome were identified. Female gender was associated with greater improvement across treatment groups. Gender was not a predictor of CBT outcomes in prior studies, including for social phobia (Schuurmans et al., 2009; Watanabe et al., 2010), and it was neither a predictor nor a moderator of outcome in the previous study of a mixed anxiety disorder sample (Wolitzky-Taylor et al., 2012). The gender effect may reflect selection bias rather than a replicable finding. Higher extraversion was also associated with greater improvement. To our knowledge, only one other study examined extraversion as a predictor of behavioral treatment in a social phobia sample, with null results (Chen et al., 2007). Depression was predictive of poorer outcome across both treatment conditions in the current study. It was previously found that comorbid depression led to greater improvement in ACT (Wolitzky-Taylor et al., 2012) and for CBT, depression either led to poorer outcome (Chambless, Tran, & Glass, 1997; Steketee, Chambless, & Tran, 2001) or had no association with outcome (Kampman, Keijsers, Hoogduin, & Hendriks, 2008; Schuurmans et al., 2009). Finally, higher levels of perceived control were predictive of better outcomes. Meuret et al. (2010) found that lower perceived control was associated with greater improvement in cognitive therapy for panic disorder. Thus, in all cases, the role of predictors of exposure-based treatment, whether cognitively based or acceptance based, is in need of further replication.
Despite the many strengths of the study, there are some limitations. Most notably, the sample size was relatively small, which may have led to insufficient power to detect differences between two active treatments, and failure to replicate all findings from our prior study (Arch et al., 2012). Given our sample size, we had sufficient power (80%) to detect only large effects for the treatment group effects (Cohen’s d = .85) and moderator analyses (Cohen’s f2 = .45). Power to detect moderate and small effects for both analyses was 40% and 20%, respectively. Thus, future studies with larger samples should attempt to replicate these findings before definitive prescriptive recommendations are made. Still, the fact that the current results mirrored our prior findings in terms of similarity in outcomes across CBT and ACT and trends for the positive predictive value of high experiential avoidance for CBT outcomes (Arch et al., 2012; Wolitzky-Taylor et al., 2012) suggests some degree of replicability and consistency across samples. Second, treatment was delivered by relatively inexperienced graduate students. Although this is common to many clinical trials and expert supervision was provided, the findings may have differed with more experienced clinicians. We failed to measure therapy allegiance of our therapists, although we presume that allegiance was a less significant factor than might otherwise be the case with highly experienced therapists. Also, we had a high level of treatment attrition (nearly 50% by 12 month follow-up), which may have reduced power and affected our ability to observe continued change over the follow-up period. Although multi-level modeling can produce less biased estimates when data are missing, we do not know whether lower attrition would have influenced findings for the follow-up time points. Finally, some participants in ACT received additional treatment during the follow-up period, and we did not assess what type of treatment or the number of sessions they received. However, none of these four participants achieved reliable change criteria by the 12-month follow-up, suggesting that the findings were unlikely to be influenced by the additional treatment.
In sum, this study adds to the small but growing body of evidence indicating that CBT and ACT perform equally well for the treatment of social phobia, and significantly outperform waitlist controls. As it becomes clear that ACT is a viable alternative to CBT, for whom each treatment works best becomes a question of central importance. This study also replicated a moderator finding from a previous comparison of CBT and ACT, showing that individuals with lower psychological flexibility respond more favorably to CBT.
Acknowledgments
Research Coordinators: Natasha Mehta, Jenny Czarlinski, Amy McGranahan, Bita Mesri, Natalie Arbid
Therapists: Aaron Baker, Natalie Castriotta, Maria Jalbrzikowski, Jon Schettino, Chris Conway, Barbara Depreeuw, Joe Trombello, Amy Jimenez, Sarah Sullivan, Erica Simon, Lily Brown, Laurie Brenner, Caitlin Ferriter, Emmanuel Espejo, Katie Williams, Lisa Christensen, Joanna Arch, Meghan McGinn, Najwa Culver, Richard LeBeau, Shaina Katz, Lynette Schumann, Michael Redding, Daniel Glenn, Betty Liao, Cameron Sepah
Supervisors: Jennifer Plumb, Raphael Rose
Consultants: Steven Hayes, Kathleen McGraugh
Statistical Guidance: Philip Ender and UCLA Statistical Consulting
This project was funded by the National Institutes of Mental Health 1 R21 MH081299 (PIs: Craske, Lieberman and Taylor)
Footnotes
These studies establish the effects of coping skill training; it is conceivable that implementation of cognitive and somatic skills during exposure augments outcomes from exposure therapy but very few studies have evaluated this question (Meuret, Wolitzky-Taylor, Twohig, & Craske, 2012)
One patient was diagnosed with a neurological condition, one patient began a new medication during treatment, and one patient was advised by a physician not to participate due to medical concerns.
Medical exclusions were based on participant report of a medical condition diagnosed by a physician; in the case of uncertainty, clarification was obtained directly from physicians. However, participants were not excluded if certain medical conditions were well controlled (e.g., elevated blood pressure, hypothyroidism).
See author for a copy of the CBT treatment manual; the ACT manual is published (Eifert & Forsyth, 2005).
Creative hopeless was moved from session 1 to session 2
Therapists who provided CBT and ACT had experience in both treatments.
UCLA supervisors observed but did not participate in ACT supervision sessions.
Given the mixed anxiety disorder sample and subsequently low n per disorder, ICCs for individual disorders should be interpreted cautiously.
Results did not differ between winsorized/corrected and uncorrected data
Although multiple imputation can be used to estimate missing data, simulation studies suggest that with large amounts of missing data on the dependent variable (10–20%), multiple imputation can inflate standard errors, and should not be used (Von Hippel, 2007).
Effect sizes are calculated based on the method described by Feingold (2009) that produces estimates analogous to Cohen’s d for growth curve models in randomized clinical trials
Effect sizes are calculated using pooled standard deviations from the two groups included in the comparison at baseline for S1 and at post for S2
References
- Arch JJ, Craske MG. Acceptance and commitment therapy and cognitive behavioral therapy for anxiety disorders: Different treatments, similar mechanisms? Clinical Psychology: Science and Practice. 2008;15(4):263–279. [Google Scholar]
- Arch JJ, Eifert GH, Davies C, Vilardaga JCP, Rose RD, Craske MG. Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. Journal of Consulting and Clinical Psychology. 2012;80(5):750–765. doi: 10.1037/a0028310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond FW, Bunce D. Mediators of change in emotion-focused and problem-focused worksite stress management interventions. Journal of Occupational Health Psychology. 2000;5(1):156–163. doi: 10.1037//1076-8998.5.1.156. [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KC, Guenole N, Orcutt HK, … Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological flexibility and acceptance. Behavior Therapy. 2011;42:676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3(4):257–260. [Google Scholar]
- Brown TA, Di Nardo PA, Barlow DH. The Anxiety Disorders Interview Schedule for DSM IV (ADIS IV) San Antonio, TX: Psychological Corporation/Graywind Publications Inc; 1994. [Google Scholar]
- Brown TA, White KS, Forsyth JP, Barlow DH. The structure of perceived emotional control: Psychometric properties of a revised anxiety control questionnaire. Behavior Therapy. 2004;35(1):75–99. [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26(1):17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH, Brown TA, Hofmann SG. Effects of suppression and acceptance on emotional responses of individuals with anxiety and mood disorders. Behaviour Research and Therapy. 2006;44(9):1251–1263. doi: 10.1016/j.brat.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Tran GQ, Glass CR. Predictors of response to cognitive-behavioral group therapy for social phobia. Journal of Anxiety Disorders. 1997;11(3):221–240. doi: 10.1016/s0887-6185(97)00008-x. [DOI] [PubMed] [Google Scholar]
- Chen J, Nakano Y, Ietzugu T, Ogawa S, Funayama T, Watanabe N, … Furukawa TA. Group cognitive behavior therapy for Japanese patients with social anxiety disorder: Preliminary outcomes and their predictors. BMC Psychiatry. 2007;7(1):69. doi: 10.1186/1471-244X-7-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Stein MB, Sullivan G, Sherbourne C, Bystritsky A, Rose RD, … Golinelli D. Disorder-specific impact of coordinated anxiety learning and management treatment for anxiety disorders in primary care. Archives of General Psychiatry. 2011;68(4):378–388. doi: 10.1001/archgenpsychiatry.2011.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalrymple KL, Herbert JD. Acceptance and Commitment Therapy for generalized social anxiety disorder. Behavior Modification. 2007;31(5):543–568. doi: 10.1177/0145445507302037. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Foa EB, Huppert JD, Keefe FJ, Franklin ME, Compton JS, … Gadde KM. Fluoxetine, comprehensive cognitive behavioral therapy, and placebo in generalized social phobia. Archives of General Psychiatry. 2004;61(10):1005. doi: 10.1001/archpsyc.61.10.1005. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, … Jacobson NS. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74(4):658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Eifert GH, Forsyth JP. Acceptance and commitment therapy for anxiety disorders: A practioner’s treatment guide to using mindfulness, acceptance, and values-based behavior change strategies. Oakland, CA: New Harbinger Publications, Inc; 2005. [Google Scholar]
- Eysenck HJ, Eysenck SBG. Manual of the Eysenck Personality Questionnaire. London: Hodder and Stoughton; 1975. [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14(1):43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Leibowitz MR, Hami S, Stein MB, Goetz D. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31(6):1025–1035. doi: 10.1017/s0033291701004056. [DOI] [PubMed] [Google Scholar]
- Frisch MB. Manual and treatment guide for the Quality of Life Inventory. Minneapolis, MN: National Computer Systems; 1994. [Google Scholar]
- Frisch MB, Clark MP, Rouse SV, Rudd MD, Paweleck JK, Greenstone A, Kopplin DA. Predictive and treatment validity of life satisfaction and the Quality of Life Inventory. Assessment. 2005;12(1):66–78. doi: 10.1177/1073191104268006. [DOI] [PubMed] [Google Scholar]
- Guttman I. Care and handling of univariate or multivariate outliers in detecting spuriosity: A bayesian approach. Technometrics. 1973:723–738. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: The Guilford Press; 1999. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG, Bissett RT, Pistorello J, Toarmino D, … McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54(4):553–578. [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal data analysis. Hoboken, New Jersey: John Wiley & Sons, Inc; 2006. [Google Scholar]
- Hofmann SG, DiBartolo PM. An instrument to assess self-statements during public speaking: Scale development and preliminary psychometric properties. Behavior Therapy. 2000;31(3):499–515. doi: 10.1016/s0005-7894(00)80027-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope DA, Heimberg RG, Juster HA, Turk CL. Managing social anxiety: A cognitive-behavioral therapy approach client workbook. New York, NY: Oxford University Press; 2000. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kampman M, Keijsers GPJ, Hoogduin CAL, Hendriks G-J. Outcome prediction of cognitive behaviour therapy for panic disorder: Initial symptom severity is predictive for treatment outcome, comorbid anxiety or depressive disorder, cluster C personality disorders and initial motivation are not. Behavioural and Cognitive Psychotherapy. 2008;36(01):99–112. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline P, Barrett P. The factors in personality questionnaires among normal subjects. Advances in Behaviour Research and Therapy. 1983;5(3–4):141–202. [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Levitt JT, Brown TA, Orsillo SM, Barlow DH. The effects of acceptance versus suppression of emotion on subjective and psychophysiological response to carbon dioxide challenge in patients with panic disorder. Behavior Therapy. 2004;35(4):747–766. [Google Scholar]
- Liebowitz MR. Social phobia. Modern problems of pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Loerinc A, Meuret A, Twohig M, Rosenfield D, Craske MG. Response rates in CBT for anxiety disorders: Measurement matters. (submitted for publication) [Google Scholar]
- Maassen GH. The standard error in the Jacobson and Truax Reliable Change Index: The classical approach to the assessment of reliable change. Journal of the International Neuropsychological Society. 2004;10(6):888–893. doi: 10.1017/s1355617704106097. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36(4):455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- McGrath KB, Forman EM, Herbert JD. Development and validation of the ACT/CT adherence and competence rating scale. (in preparation) [Google Scholar]
- Meuret AE, Hofmann SG, Rosenfield D. Catastrophic appraisal and perceived control as moderators of treatment response in panic disorder. International Journal of Cognitive Therapy. 2010;3:262–277. doi: 10.1521/ijct.2010.3.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Twohig M, Rosenfield D, Hayes S, Craske MG. Brief acceptance and exposure therapy for panic disorder: A pilot study. Cognitive and Behavioral Practice. 2012;19:606–618. [Google Scholar]
- Meuret AE, Wolitzky-Taylor KB, Twohig MP, Craske MG. Coping skills and exposure therapy in panic disorder and agoraphobia: latest advances and future directions. Behavior Therapy. 2012;43(2):271–284. doi: 10.1016/j.beth.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ, Price EC. A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. The Journal of Nervous and Mental Disease. 2007;195:521–531. doi: 10.1097/01.nmd.0000253843.70149.9a. [DOI] [PubMed] [Google Scholar]
- Olivares J, García-López L-J, Beidel DC, Turner SM, Albano AM, Hidalgo M-D. Results at long-term among three psychological treatments for adolescents with generalized social phobia (I): Statistical significance. Psicología Conductual. 2002;10(1):147–166. [Google Scholar]
- Piet J, Hougaard E, Hecksher MS, Rosenberg NK. A randomized pilot study of mindfulness-based cognitive therapy and group cognitive-behavioral therapy for young adults with social phobia. Scandinavian Journal of Psychology. 2010;51(5):403–410. doi: 10.1111/j.1467-9450.2009.00801.x. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Craske MG, Brown TA, Barlow DH. Measurement of perceived control over anxiety-related events. Behavior Therapy. 1996;27(2):279–293. [Google Scholar]
- Roy-Byrne PP, Craske MG, Stein MB, Sullivan G, Bystritsky A, Katon W, … Sherbourne CD. A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry. 2005;62(3):290–298. doi: 10.1001/archpsyc.62.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuurmans J, Comijs H, Emmelkamp PMG, Weijnen IJC, van den Hout M, van Dyck R. Long-term effectiveness and prediction of treatment outcome in cognitive behavioral therapy and sertraline for late-life anxiety disorders. International Psychogeriatrics / IPA. 2009;21(6):1148–1159. doi: 10.1017/S1041610209990536. [DOI] [PubMed] [Google Scholar]
- Spence SH, Donovan C, Brechman-Toussaint M. The treatment of childhood social phobia: The effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. Journal of Child Psychology and Psychiatry. 2000;41(6):713–726. [PubMed] [Google Scholar]
- Stangier U, Heidenreich T, Peitz M, Lauterbach W, Clark DM. Cognitive therapy for social phobia: Individual versus group treatment. Behaviour Research and Therapy. 2003;41(9):991–1007. doi: 10.1016/s0005-7967(02)00176-6. [DOI] [PubMed] [Google Scholar]
- Steketee G, Chambless DL, Tran GQ. Effects of axis I and II comorbidity on behavior therapy outcome for obsessive-compulsive disorder and agoraphobia. Comprehensive Psychiatry. 2001;42(1):76–86. doi: 10.1053/comp.2001.19746. [DOI] [PubMed] [Google Scholar]
- Tillfors M, Carlbring P, Furmark T, Lewenhaupt S, Spak M, Eriksson A, … Andersson G. Treating university students with social phobia and public speaking fears: Internet delivered self-help with or without live group exposure sessions. Depression and Anxiety. 2008;25(8):708–717. doi: 10.1002/da.20416. [DOI] [PubMed] [Google Scholar]
- Tolin DF. Is cognitive-behavioral therapy more effective than other therapies? A meta-analytic review. Clinical Psychology Review. 2010;30(6):710–720. doi: 10.1016/j.cpr.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Von Hippel PT. Regression with missing Ys: An improved strategy for analyzing multiply imputed data. Sociological Methodology. 2007;37(1):83–117. [Google Scholar]
- Watanabe N, Furukawa TA, Chen J, Kinoshita Y, Nakano Y, Ogawa S, … Noda Y. Change in quality of life and their predictors in the long-term follow-up after group cognitive behavioral therapy for social anxiety disorder: a prospective cohort study. BMC Psychiatry. 2010;10(1):81. doi: 10.1186/1471-244X-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor KB, Arch JJ, Rosenfield D, Craske MG. Moderators and non-specific predictors of treatment outcome for anxiety disorders: A comparison of cognitive behavioral therapy to acceptance and commitment therapy. Journal of Consulting and Clinical Psychology. 2012;80(5) doi: 10.1037/a0029418. [DOI] [PubMed] [Google Scholar]