Abstract
Objective
Identifying treatments to improve functioning and reduce negative symptoms in consumers with schizophrenia is of high public health significance.
Method
In this randomized clinical trial, participants with schizophrenia or schizoaffective disorder (N=149) were randomly assigned to cognitive behavioral social skills training (CBSST) or an active goal-focused supportive contact (GFSC) control condition. CBSST combined cognitive behavior therapy with social skills training and problem solving training to improve functioning and negative symptoms. GFSC was weekly supportive group therapy focused on setting and achieving functioning goals. Blind raters assessed functioning (primary outcome: Independent Living Skills Survey (ILSS)), CBSST skill knowledge, positive and negative symptoms, depression, and defeatist performance attitudes.
Results
In mixed-effects regression models in intent-to-treat analyses, CBSST skill knowledge, functioning, amotivation/asociality negative symptoms and defeatist performance attitudes improved significantly more in CBSST relative to GFSC. In both treatment groups, comparable improvements were also found for positive symptoms and a performance-based measure of social competence.
Conclusions
The results suggest CBSST is an effective treatment to improve functioning and experiential negative symptoms in consumers with schizophrenia, and both CBSST and supportive group therapy that is actively focused on setting and achieving functioning goals can improve social competence and reduce positive symptoms.
Keywords: cognitive behavioral social skills training, schizophrenia, negative symptoms, functioning, group therapy
Schizophrenia affects approximately 1% of the world population and leads to profound disability in quality of life and everyday functioning, including impairment in independent living, education, working and socializing (Harvey et al., 2012; Harvey & Strassnig, 2012). Negative symptoms of schizophrenia account for much of the poor functional outcome in schizophrenia and are an unmet treatment need in a large proportion of patients (Kirkpatrick, Fenton, Carpenter, & Marder, 2006). Over 20% of consumers with schizophrenia are estimated to have clinically-relevant persistent negative symptoms in need of treatment (Buchanan, 2007). Identifying treatments to reduce negative symptoms and improve functioning in consumers with schizophrenia is of high public health significance.
Modest improvements in functioning and negative symptoms in consumers with schizophrenia have been found in clinical trials of cognitive behavior therapy (CBT) and social skills training (SST). In a meta-analysis (Wykes, Steel, Everitt, & Tarrier, 2008) of 33 clinical trials of CBT for schizophrenia, the effect size for functioning (d=.38) and negative symptom (d=.44) outcomes were comparable to the effect size for positive symptoms (d=.37). It should be noted that these treatment effects were attenuated in trials with higher design quality (Wykes et al., 2008). Numerous clinical trials of SST have also found medium effects for community functioning (d=.52) and modest effects for negative symptoms (d=.40) (Kurtz & Mueser, 2008; Benton & Schroeder, 1990).
Given the potential efficacy of CBT and SST for schizophrenia, a group therapy intervention was developed that combined these two treatments called, Cognitive Behavioral Social Skills Training (CBSST) (Granholm, McQuaid, Auslander, & McClure, 2004; McQuaid, et al., 2000). CBSST is a recovery-oriented psychosocial rehabilitation intervention that targets functioning and negative symptoms in schizophrenia. By adding CBT to SST, SST can be used to train new skills, and thoughts that interfere with skilled performance in the real world (e.g., low self-efficacy, defeatist performance attitudes) can be addressed in cognitive therapy. Several researchers have found that defeatist attitudes (e.g., “Why try, I always fail”) are associated with poor functioning and negative symptoms, especially experiential (amotivation/asociality) negative symptoms (Grant & Beck, 2009; Green et al., 2012; Horan et al., 2010). Self-efficacy beliefs are central to motivation to engage in goal-directed activities and willingness to continue to expend effort when tasks become more difficult (Avery, Startup, & Calabria, 2009; Grant & Beck, 2009), and self-efficacy is related to negative symptoms and social functioning in consumers with schizophrenia (Cardenas et al., 2013; Hill & Startup, 2013; Yanos, Primavera & Knight, 2001). Rector and colleagues (2005) proposed that dysfunctional attitudes about the personal costs of applying energy toward goal-directed tasks could, as a defense against anticipated failure and negative evaluations by others, lead to passivity and avoidance of activities that require effort. By addressing self-efficacy and defeatist attitudes, therefore, consumers may increase motivation for social engagement and successful skill performance in the community. Consistent with this hypothesis, Grant and colleagues (2012) found that a CBT intervention designed in part to address defeatist performance attitudes in schizophrenia reduced avolition-apathy negative symptoms and improved functioning (Global Assessment of Scale) to a greater extent than standard treatment, and another open CBT trial found significant improvement in both dysfunctional attitudes and negative symptoms in a sample of consumers with psychotic disorders who had not been taking antipsychotic medication (Morrison et al., 2012).
However, some studies have not found a direct relationship between self-efficacy and functioning in schizophrenia. For example, the relationship between self-efficacy and functional outcome has been found to be mediated or moderated by other factors, such as negative symptoms (Pratt, Mueser, Smith & Lu, 2005) and illness insight (Kurtz, Olfson & Rose, 2013). In addition, the SST components of CBSST involve observational learning, practice of specific skills, reinforcement and corrective feedback. Change in functioning in CBSST may stem from behavioral activation of practiced skills, rather than change in defeatist attitudes and self-efficacy.
In a prior CBSST clinical trial (Granholm et al., 2005; Granholm et al., 2007), 76 middle-aged and older consumers (M age = 54) with schizophrenia or schizoaffective disorder were randomized to treatment as usual (TAU) or CBSST. Participants in CBSST showed significantly greater CBSST skill mastery and functioning relative to participants in TAU, and these improvements were maintained at one-year follow-up (Granholm et al., 2007). This trial showed that CBSST was more effective than TAU, but did not control for nonspecific therapist contact. In a subsequent trial (Granholm, Holden, Link, McQuaid, & Jeste, 2013), CBSST was compared with an active psychosocial control condition, goal-focused supportive contact (GFSC), in 64 middle-aged and older consumers (M age = 55) with schizophrenia or schizoaffective disorder. GFSC was an enhanced supportive contact intervention focused on helping consumers set and work toward functioning goals in a support group that provided the same amount of therapist and group contact as CBSST. Participants in CBSST showed significantly greater CBSST skill mastery and functioning relative to participants in the active GFSC control condition. Significant comparable reductions in experiential (amotivation/asociality) negative symptoms were also found in both CBSST and GFSC. Defeatist attitudes did not change significantly in treatment, but greater improvement in defeatist attitudes was associated with greater improvement in functioning in CBSST.
Both of these prior CBSST trials were focused on middle-aged and older consumers (age > 50) who had been ill for three decades on average. The efficacy of CBSST, therefore, has not been tested in a non-geriatric, more representative sample. The present study was a randomized clinical trial comparing CBSST with GFSC in consumers with schizophrenia or schizoaffective disorder age 18–65. Longer duration of illness and older age have been associated with poorer outcome in CBT for psychosis (Drury, Birchwood, Cochrane & Macmillan, 1996; Morrison et al., 2004; Morrison, et al., 2012). Similarly, in the meta-analysis by Kurtz and Mueser (2008), older samples showed less improvement on performance-based functional capacity measures, and a trend association (p < .065) was found between older age and less improvement in negative symptoms. Lower self-efficacy has also been found to be correlated with longer duration of illness and greater number of hospitalizations in consumers with schizophrenia (McDermott, 1995). Therefore, defeatist attitudes and experiential negative symptoms may be more likely to improve in the non-geriatric sample in the present trial. It was hypothesized that functional outcome, negative symptoms, and defeatist attitudes would improve to a significantly greater extent in CBSST than in GFSC.
Methods
Design
All study procedures were approved by the institutional review board of the University of California, San Diego, and VA San Diego Healthcare System. After providing informed consent and completing baseline assessments, eligible participants were randomly assigned to one of two treatment conditions: CBSST or GFSC. An independent statistician allocated participants to treatments according to a computer-generated randomization list. The study coordinator, who was not involved in any assessments or treatments, contacted the statistician to ascertain treatment assignment. Participants were then treated for 9 months and followed for 12 months after treatment, with baseline, 4.5-month (mid-treatment), 9-month (end-of-treatment), 15-month (mid-follow-up) and 21-month (one year post-treatment) follow-up assessments. Assessors were blinded to treatment allocation, and therapists and the study coordinator, who were aware of treatment allocation, did not complete any outcome assessments. Treatment took place in a separate building from assessments and participants were counseled by the study coordinator not to reveal any information about their treatment groups or the content of therapy to the assessors before each assessment visit. Participants received compensation ($50) for completing assessment visits, but not for attending treatment sessions. Transportation was provided to assessment visits, if necessary, but not to therapy sessions.
Participants
Participants were recruited through flyers and brochures posted and handed out by a study recruiter at a variety of community settings throughout San Diego County, including residential facilities (board & care/assisted living homes), clubhouses/drop-in settings, outpatient psychiatry clinics and other treatment settings in the University of California San Diego Health System, San Diego County Mental Health System, and VA San Diego Healthcare System. Inclusion criteria were: (1) Age >18, (2) diagnosis of schizophrenia (N=117) or schizoaffective disorder (N=32) based on the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID) (First, Spitzer, Gibbon, & Williams, 1996) and available medical record review, and (3) capacity to provide informed consent. At baseline, all but 4 consumers reported taking antipsychotic medications, 72 also reported antidepressant medications, and 41 reported mood-stabilizers. The minimal exclusion criteria consisted of: (1) Prior exposure to CBT or SST during the previous five years, and (2) level of care required at baseline that would interfere with participation in outpatient therapy groups or assessments (e.g., disabling medical problems, or current hospitalization for medical, psychiatric, or substance abuse problems).
Interventions
Treatment conditions were matched for amount of therapist contact and the same therapists delivered both interventions. Participants in both treatment conditions were offered a total of 36 weekly group therapy sessions (9 months) during a treatment phase, which was followed by monthly booster sessions during the follow-up period (12 sessions). In both conditions, group therapy sessions were two hours, with a lunch or snack break mid-way. Group sessions were facilitated by two masters- or doctoral-level therapists with at least two years of CBT experience. Two of us (E.G., J.M.) provided training and weekly supervision, including review of session videotapes. Participants in both treatment groups (CBSST and GFSC) were also offered individual 30–50 minute goal-setting sessions with one of their two group therapists at baseline and every three months thereafter.
Individual Goal-Setting Sessions
In these individual sessions, two recovery-oriented (living, learning, working or socializing) functioning goals were set, progress toward goal achievement was tracked, and therapists provided supportive encouragement. Functional goal achievement was the primary focus of both group interventions (CBSST and GFSC). These individual sessions were added to both treatment arms to allow additional time for personalized goal setting and breaking long-term goals down into short-term goals and specific, attainable goal steps.
Cognitive Behavioral Social Skills Training (CBSST)
CBSST (Granholm, McQuaid, McClure, Pedrelli, & Jeste, 2002; Granholm et al., 2004; Granholm et al., 2005; Granholm et al., 2007; Granholm et al., 2013; McQuaid et al., 2000), as provided in the current study, was a group therapy intervention delivered in three, six-session modules that were intended to be completed twice, for a total of 36 weekly sessions (9 months) during the treatment phase. CBSST booster sessions did not follow a manualized sequence of skill training like the treatment phase. Rather, therapists guided participants in selecting any of the skills trained during the treatment phase to address concerns and functioning goals. The CBSST treatment manual included a participant workbook that described the skills and included homework assignment forms.
The three CBSST modules were Cognitive Skills Module, Social Skills Module, and Problem-Solving Skills Module. Training thought challenging skills was the exclusive focus of the Cognitive Skills Module, but thought challenging was also used throughout the other two modules (e.g., to address defeatist attitudes and other thoughts that could be obstacles to skill learning or goal achievement). Cognitive interventions were not strongly formulation or schema based, rather cognitive therapy components focused on the practice of simplified thought challenging skills and behavioral experiment activities. Thought challenging skills were used to address symptoms and challenge defeatist beliefs that interfere with functioning behaviors, including expectancies (“It won’t be fun”), self-efficacy beliefs (“I always fail”), and anomalous/delusional beliefs (“Spirits will harm me”). Group members were introduced to the general concepts of CBT, including the relationship between thoughts, actions and feelings (generic cognitive model), automatic thoughts, thought challenging through behavioral experiments and examining evidence for beliefs, and mistakes in thinking. The primary thought challenging skill trained was the 3C’s: Catch It, Check It, Change It (“It” is an unhelpful thought).
The primary goal of the Social Skills Module was to improve communication skills through behavioral role plays, including active listening, expressing positive and negative feelings and making positive requests. Important role plays included assertive interactions with co-workers, friends and family, making new friends, and effectively interacting with case managers, doctors, and other support persons.
Basic problem-solving skills were trained in the Problem-Solving Skills Module using the acronym, SCALE – Specify the problem, Consider all possible solutions, Assess the best solution, Lay out a plan, and Execute and Evaluate the outcome. The focus was on developing specific, feasible plans to solve real-world problems, including scheduling pleasant activities, improving living situations, finances, using public transportation, finding a volunteer or paid job, and enrolling in classes.
Goal-Focused Supportive Contact (GFSC)
The GFSC intervention was an enhanced supportive contact control condition with a primary focus, like CBSST, on setting and achieving functioning goals (e.g., living, learning, working and socializing). Sessions were semi-structured and consisted of check-in about distress and potential crisis management, followed by a flexible group discussion about setting and working toward functioning goals. Sessions typically included components of psychoeducation, empathy, and non-directive reinforcement of health, coping, and symptom management behaviors, which grew out of group discussions, with minimal therapist guidance. Booster sessions employed the same approach as in the treatment phase.
Treatment Fidelity
Twenty-four randomly-selected sessions (12 from each group, stratified by module for the CBSST group) were rated for fidelity using the Cognitive Therapy Rating Scale for Psychosis (CTS-Psy; Haddock et al., 2001) and the Social Skills Group Observation Checklist (SSGOC; Bellack, Mueser, Gingerich, & Agresta, 2004). Only six items related to role play practice were rated from the SSGOC (established a rationale, discussed and modeled steps, engaged client in a role play, provided positive feedback, provided suggestions for improvement, and reinforced small steps in repeated role plays; all rated 0, absent, or 1, present), because the remaining items overlapped with nonspecific therapist items (e.g., understanding, interpersonal effectiveness) and session-structure items (e.g., agenda setting, homework) that were also rated on the CTS-Psy. The CTS-Psy total score was significantly greater in CBSST (M=40.4, SD=4.0) relative to GFSC (M=19.7, SD=1.8), t(22)=13.14, p<.001. The total CTS-Psy score for CBSST, but not for GFSC, was above the cutoff for competent CBT for psychosis (>30) used in previous clinical trials (e.g., Turkington, Kingdon, & Turner, 2002). CTS-Psy ratings of CBT-specific skills were significantly greater for CBSST than for GFSC (sum of Agenda, Feedback, Collaboration, Guided Discovery, Focus on Key Cognitions, Choices of CBT Interventions, Quality of Interventions, and Homework items: CBSST M=28.4, S.D.=3.9; GFSC M=7.9, S.D.=1.6; t(22)=13.29, p<.001), whereas ratings of nonspecific therapy skills did not differ significantly between CBSST and GFSC (sum of Understanding and Interpersonal Effectiveness items: CBSST M=11.94, S.D.=0.2; GFSC M=11.86, S.D.=0.4; t(22)=0.65, p=.52). The mean rating on the six SSGOC role play items was 4.0 (SD=1.2) for the CBSST Social Skills Module and 0.0 for the other CBSST modules and GFSC. This is not surprising, given that role play practice is only intended to be included in the CBSST Social Skills Module. Therefore, the two interventions, which were delivered by the same therapists, had similar nonspecific supportive therapy components, but high-fidelity CBT and SST interventions were only present in CBSST.
Outcome Measures
The primary outcome measure was self-reported functioning on the Independent Living Skills Survey (ILSS; Wallace, Liberman, Tauber, & Wallace, 2000). The ILSS is a 51-item, self-report measure which was administered in an interview format to assess multiple domains of functioning (appearance and clothing, personal hygiene, care of possessions and living space, food preparation, health maintenance, transportation, money management, leisure and recreational activities, job seeking, job maintenance). According to standard scoring procedures, items were scored 0 (not performed), 1 (performed), or “Not Able to Demonstrate” (e.g., for food preparation items when meals were provided by assisted living staff), and the average of available items was computed for each domain (domain scores were not computed if more than half the items were missing or scored “Not Able to Demonstrate”). Consistent with our prior study (Granholm et al., 2005), a composite score was computed as the average of scores on five relevant functional domains (appearance and clothing, personal hygiene, health maintenance, transportation, and leisure and community activities; range = 0–1). Other domain scores could not be computed due to many “not able to demonstrate” item scores for the majority of participants who were unemployed, receiving disability income that was managed by others and living in board-and-care settings where cleaning and cooking services were provided. The ILSS was administered at all assessment points.
The Comprehensive Module Test (CMT) was used as a proximal measure of skills acquisition to assess knowledge of the specific content in the 3 CBSST modules. The CMT was included as an intervention check on whether consumers learned the CBSST skills, not a test of whether the intervention improved outcomes better than GFSC. The CMT was originally developed at UCLA for use with SST modules (Liberman, 1994). Content questions (e.g., What are the 3Cs?”) and vignettes requiring appropriate use of skills were developed to assess mastery of communication (max =11), problem-solving (max=11) and thought challenging (max=11) skills. The CMT total score (max=33) was used in analyses. The CMT was administered at all assessment points.
The Maryland Assessment of Social Competence (MASC; Bellack & Meuser, 1993; Bellack, Sayers, Mueser, & Bennett, 1994) was used as a performance-based measure of social skill capacity. The MASC is a structured behavioral role play assessment that measures the ability to resolve interpersonal problems through conversation scenarios (1 conversation initiation; 2 assertion), during which the consumer interacts with a live confederate who plays a role (e.g., boss) in a problem-oriented situation (e.g., asking for a work shift change). The measure has three parallel sets of scenarios for multiple administrations. Videotaped role plays are coded by blinded raters on dimensions of verbal content, nonverbal communication behavior, and an overall effectiveness score, which was the primary MASC variable. The MASC was not administered at mid-treatment or mid-follow-up assessments.
The PSR Toolkit (Arns, Rogers, Cook, & Mowbray, 2001) was used to collect objective functional milestone information on employment, educational activity, psychiatric hospitalizations and residential situation. This measure does not rely on self-report, because research staff obtain employment status records (e.g., time cards; pay stubs), educational transcripts, and hospital discharge summaries, and visited residential settings to determine level of services, and talk with psychiatrists, residential staff, case managers, and/or family members to obtain objective information. At each assessment point, milestone variables were coded: 1) Unemployed (=0) v. employed (any paid or unpaid job or sheltered workshop =1); 2) No education activities (=0) v. any educational engagement (=1), any psychiatric hospitalization (=1) v. none (=0), and 3) Assisted (=0) v. unassisted living (=1). The PSR Toolkit was not administered at mid-treatment or mid-follow-up assessments.
The Positive and Negative Syndrome Scale (PANSS) (Kay, Fiszbein, & Opler, 1987), Scale for the Assessment of Negative Symptoms (SANS) (Andreasen, 1982) and Beck Depression Inventory – 2nd Edition (BDI-II) (Beck, 1996) were administered to assess clinical symptoms. Based on factor analytic studies of the SANS (Blanchard & Cohen, 2006; Peralta & Cuesta, 1999; Sayers, Curran, & Mueser, 1986), two negative symptom factors were derived: Diminished Expression, defined as the average of Affective Flattening and Alogia global ratings (Items 8, 13); and Diminished Motivation, defined as the average of Avolition-Apathy and Anhedonia-Asociality global ratings (Items 17, 22). All symptom measures were administered at all assessment points.
Finally, the Defeatist Performance Attitude Scale (DPAS) is a 15-item self-report subscale derived from factor analysis of the commonly-used Dysfunctional Attitude Scale (Form A; Cane, Olinger, Gotlib, & Kuiper, 1986; Weissman & Beck, 1978; 1980). The DPAS indexes endorsement of defeatist attitudes about one’s ability to perform goal-directed tasks (e.g., “If you cannot do something well, there is little point in doing it at all”, “If I fail at my work, then I am a failure as a person,” “People will probably think less of me if I make mistakes and fail”). Items are rated on a 1–7 Likert scale and higher total scores (range = 15–105) indicate more severe defeatist performance attitudes.
Reliability
Assessors received training using videotape and practice interviews and did not complete assessments until achieving at least .80 inter-rater reliability. Inter-rater reliability (interclass correlation) was .88 for PANSS total, .87 for PANSS positive, .83 for SANS total, and .86 for the MASC effectiveness score.
Statistical Analyses
In intent-to-treat (ITT) analyses, all participants who completed baseline assessments were randomized and included in the analyses. Mixed-effects regression modeling (utilizing HLM v6.06) was used. Growth curve models predicting each level-1 outcome variable (ILSS Composite; MASC Effectiveness; SANS Diminished Motivation; SANS Diminished Expression; PANSS Positive; PANSS Total; BDI-II Total) were estimated using time (in months centered at baseline), as a level-1 predictor and group (coded CBSST = 0.5, GFSC = −0.5), number of therapy sessions attended (centered at the median), and the group X sessions interaction, as level-2 predictors of both the slope and intercept parameters. Hierarchical logistic models using a Bernoulli level-1 sampling model and Logit link function were used for PSR ToolKit binary variables. Effect sizes at end of treatment and 21-month follow-up were estimated by computing the treatment group difference for HLM model-predicted values for each outcome variable for hypothetical participants with a median number of sessions attended and dividing by the baseline assessment pooled SD for the outcome. Finally, Chi Square tests were used to examine group differences in rates of achievement of functioning milestones on binary PSR ToolKit variables.
Results
Sample
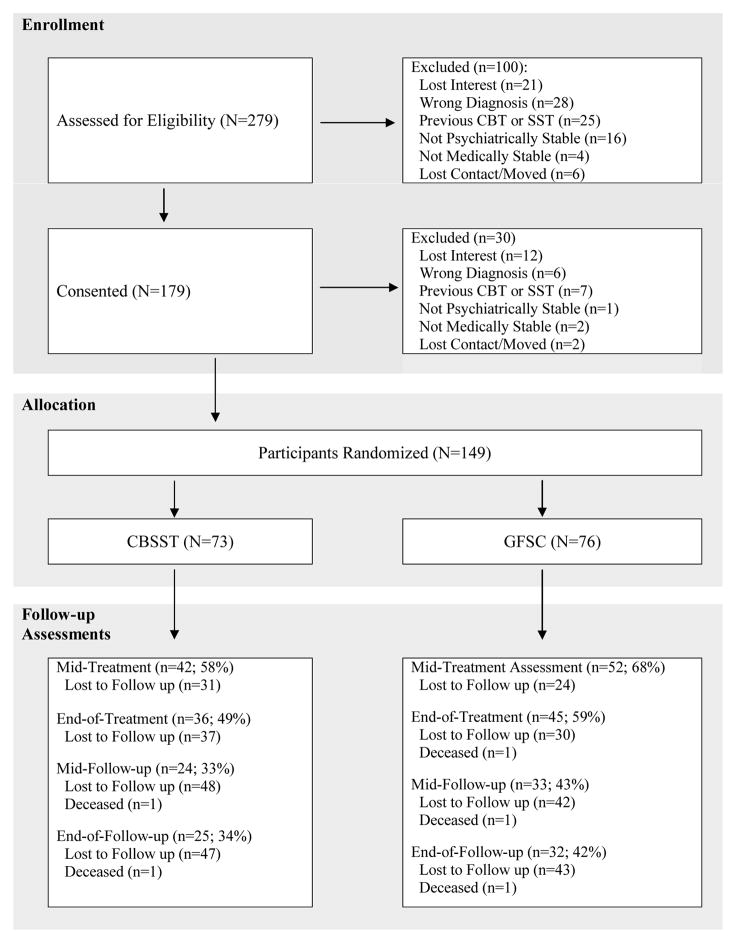
The flow of participants through the 21-month protocol is shown in Figure 1. Sixty-three percent (N=94) of participants were re-assessed at mid-treatment, 54% (N=81) at end of treatment, 38% (N=57) at mid-follow-up and 38% (N=57) at final follow-up, and 70% (N=104) of participants had more than one assessment (median = 3). The groups did not differ significantly in dropout rates at any assessment point. Dropouts at 21 months did not differ significantly from participants with a 21-month follow-up assessment on baseline ILSS (t(146)=1.28, p=.203), PANSS Positive Symptom Scale (t(146)=0.17, p=.863), SANS Diminished Motivation (t(145)=0.29, p=.771), SANS Diminished Expression (t(145)=0.76, p=.446), MASC (t(135)=0.82, p=.413), or DPAS (t(145)=0.37, p=.712) scores. The CBSST and GFSC treatment groups did not differ significantly with regard to any demographic characteristic (Table 1) or any outcome variable at baseline (Table 2).
Figure 1.
Flow of consumers with schizophrenia through the 21-month randomized clinical trial comparing Cognitive Behavioral Social Skills Training (CBSST) with an active Goal-Focused Supportive Contact (GFSC) control treatment. Participants who attended at least one therapy session and had at least one assessment on a given outcome were included in analyses.
Table 1.
Baseline Participant Characteristics
| Variable | GFSC (N=76) | CBSST (N=73) | Statistical Analysis | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | χ2 | df | p | |
| Male | 53 | 70 | 46 | 63 | 0.76 | 1 | .385 |
| Caucasian | 44 | 58 | 41 | 56 | 0.05 | 1 | .831 |
| M | SD | M | SD | t | df | p | |
| Age (yrs.) | 41.6 | 9.2 | 41.1 | 10.4 | 0.33 | 147 | .742 |
| Education (yrs.) | 12.3 | 1.8 | 12.3 | 2.0 | 0.04 | 147 | .967 |
| Duration of Illness (yrs.) | 21.4 | 10.6 | 21.3 | 11.5 | .05 | 147 | .961 |
| PANSS Total | 73.3 | 20.0 | 71.5 | 16.6 | 0.59 | 146 | .556 |
Note: GFSC = Goal-Focused Supportive Contact; CBSST=Cognitive Behavioral Social Skills Training; PANSS=Positive and Negative Syndrome Scale.
Table 2.
Descriptive statistics for available data on all outcome measures at each assessment point for each treatment group
| Baseline | 4-months | End of Tx. | 6-month follow-up | 12-month follow-up | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | ||
| ILSS | CBSST | 72 | 0.73 (0.10) | 41 | 0.74 (0.10) | 35 | 0.72 (0.10) | 23 | 0.73 (0.12) | 24 | 0.71 (0.11) |
| GFSC | 76 | 0.70 (0.10) | 50 | 0.71 (0.11) | 44 | 0.71 (0.10) | 31 | 0.69 (0.12) | 31 | 0.69 (0.11) | |
| MASC | CBSST | 63 | 3.4 (1.0) | -- | --- | 35 | 3.8 (0.9) | -- | --- | 24 | 3.5 (0.8) |
| GFSC | 74 | 3.2 (1.2) | -- | --- | 42 | 3.4 (1.1) | -- | --- | 28 | 3.3 (1.0) | |
| CMT | CBSST | 72 | 5.8 (3.0) | 42 | 8.1 (4.4) | 36 | 10.4 (5.7) | 24 | 11.8 (5.1) | 24 | 11.1 (6.4) |
| GFSC | 76 | 5.6 (3.5) | 52 | 5.8 (4.0) | 44 | 6.5 (3.9) | 33 | 5.6 (2.8) | 31 | 5.7 (3.3) | |
| SANS Dim Mot | CBSST | 71 | 2.26 (1.11) | 39 | 2.33 (1.14) | 36 | 2.06 (1.06) | 24 | 2.02 (1.12) | 25 | 1.74 (0.81) |
| GFSC | 76 | 2.11 (1.17) | 49 | 2.11 (1.16) | 45 | 2.29 (0.91) | 33 | 2.26 (1.31) | 31 | 2.27 (1.15) | |
| SANS Dim Exp | CBSST | 71 | 1.82 (1.13) | 39 | 1.87 (1.15) | 36 | 1.92 (1.05) | 24 | 1.85 (1.03) | 25 | 1.82 (0.96) |
| GFSC | 76 | 1.80 (1.15) | 49 | 1.99 (1.04) | 45 | 1.89 (1.12) | 33 | 2.02 (1.00) | 31 | 2.00 (0.96) | |
| PANSS Positive | CBSST | 72 | 19.4 (5.5) | 42 | 19.4 (5.2) | 36 | 16.6 (4.1) | 24 | 18.4 (6.3) | 25 | 15.0 (4.7) |
| GFSC | 76 | 20.2 (6.7) | 52 | 19.8 (6.0) | 45 | 18.7 (5.8) | 33 | 18.7 (5.8) | 31 | 17.2 (5.1) | |
| BDI-II | CBSST | 72 | 17.4 (9.7) | 42 | 17.1 (11.2) | 36 | 14.0 (10.2) | 24 | 15.8 (11.0) | 25 | 12.6 (9.3) |
| GFSC | 75 | 17.2 (11.5) | 52 | 16.7 (13.6) | 45 | 13.8 (10.4) | 33 | 15.6 (15.1) | 31 | 17.3 (12.0) | |
| DPAS | CBSST | 71 | 51.1 (17.2) | 42 | 51.6 (15.7) | 36 | 49.8 (14.6) | 24 | 46.2 (16.9) | 25 | 44.2 (13.3) |
| GFSC | 76 | 56.0 (17.2) | 52 | 56.2 (19.4) | 45 | 54.1 (18.3) | 33 | 54.3 (17.9) | 32 | 54.8 (17.7) | |
Notes: CBSST=Cognitive Behavioral Social Skills Training; GFSC=Goal-Focused Supportive Contact; ILSS=Independent Living Skills Survey; MASC=Maryland Assessment of Social Competence (MASC; not administered at mid-treatment or mid-follow-up); CMT=Comprehensive Modules Test; SANS = Scale for Assessment of Negative Symptoms Diminished Motivation and Diminished Expression factors; PANSS=Positive and Negative Syndrome Scale; BDI-II=Beck Depression Inventory-II; DPAS=Defeatist Performance Attitude Scale. Groups did not differ significantly at baseline on any outcome measure.
Outcomes
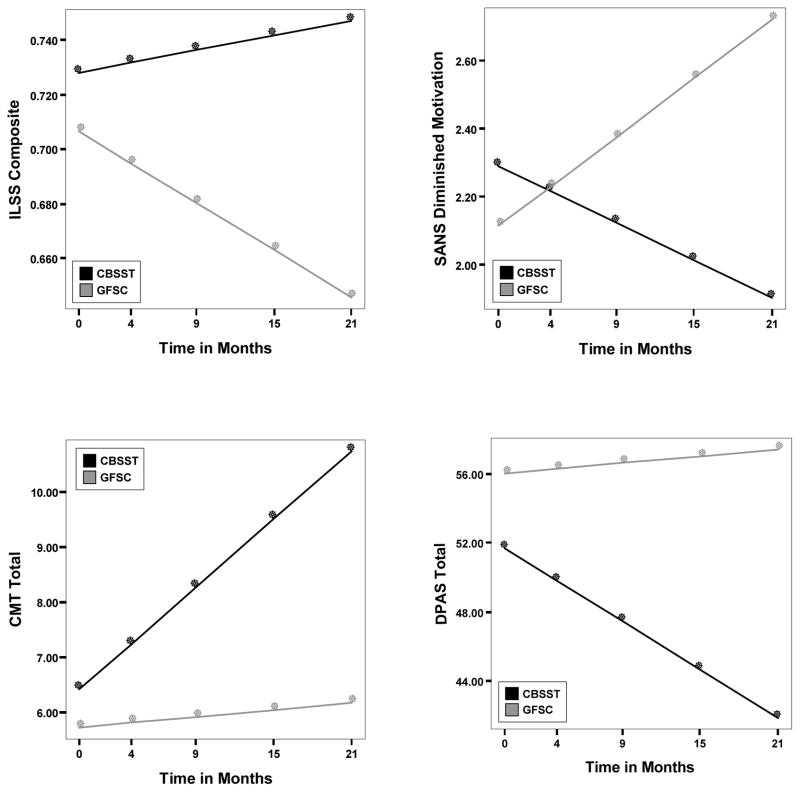
Table 2 shows descriptive statistics for each outcome variable for each treatment group at each assessment point, and results from the mixed-effects regression models are presented in Table 3. Statistically significant group X time interactions were found for the primary functioning outcome (ILSS), as well as for SANS Diminished Motivation, DPAS, and CMT, indicating significantly greater improvements over time for functioning, experiential negative symptoms, defeatist attitudes, and CBSST skill knowledge in CBSST relative to GFSC (see Figure 2). For these outcomes, effect sizes for the difference between model-estimated means of the two treatment groups at 21 months ranged from medium to very large (SANS Diminished Motivation=.52; ILSS=1.00; DPAS=.90; CMT=1.40; Table 3). The effect of time, but not the group X time interaction, was marginally significant for the MASC and significant for the PANSS Positive Subscale, indicating marginally significant improvements in social competence and significant improvement in positive symptoms over time, regardless of group membership (see Figure 3).
Table 3.
Results of mixed-effects random regression modeling for all outcomes
| Outcome Measure | Predictor Variables | γ | 95% CI | t | p | d Treatment End | d 21-mo. Follow-up |
|---|---|---|---|---|---|---|---|
| ILSS (Primary Outcome) | Intercept | 0.717 | [0.702, 0.733] | 90.10 | <.001 | ||
| Group | 0.022 | [−0.009, 0.053] | 1.36 | .177 | |||
| Time | −0.001 | [−0.002, 0.000] | −1.38 | .171 | |||
| Group x Time | 0.004 | [0.002, 0.006] | 2.62 | .010 | .55 | 1.00 | |
| MASC | Intercept | 3.36 | [3.17, 3.55] | 34.92 | <.001 | ||
| Group | 0.23 | [−0.14, 0.61] | 1.21 | .229 | |||
| Time | 0.01 | [−0.00, 0.03] | 1.85 | .065 | |||
| Group x Time | −0.01 | [−0.04, 0.02] | −0.55 | .582 | .14 | .04 | |
| CMT | Intercept | 6.06 | [5.54, 6.59] | 22.72 | <.001 | ||
| Group | 0.69 | [−0.36, 1.73] | 1.29 | .201 | |||
| Time | 0.11 | [0.04, 0.19] | 2.97 | .004 | |||
| Group x Time | 0.19 | [0.04, 0.34] | 2.42 | .017 | .72 | 1.40 | |
| SANS Diminished | Intercept | 2.20 | [2.04, 2.37] | 25.96 | <.001 | ||
| Motivation | Group | 0.18 | [−0.16, 0.51] | 1.03 | .304 | ||
| Time | 0.01 | [−0.01, 0.02] | 0.53 | .596 | |||
| Group x Time | −0.05 | [−0.09, −0.01] | −2.39 | .018 | .22 | .72 | |
| SANS Diminished | Intercept | 1.82 | [1.65, 2.00] | 20.56 | <.001 | ||
| Expression | Group | 0.03 | [−0.32, 0.38] | 0.18 | .862 | ||
| Time | 0.02 | [0.00, 0.04] | 2.00 | .047 | |||
| Group x Time | −0.01 | [−0.05, 0.03] | −0.28 | .782 | .02 | .08 | |
| PANSS Positive | Intercept | 19.59 | [18.71, 20.46] | 43.74 | <.001 | ||
| Group | −0.50 | [−2.25, 1.26] | −0.56 | .578 | |||
| Time | −0.13 | [−0.21, −0.04] | −2.84 | .006 | |||
| Group x Time | −0.09 | [−0.26, 0.08] | −1.02 | .312 | .21 | .39 | |
| BDI-II | Intercept | 17.26 | [15.50, 19.03] | 19.16 | <.001 | ||
| Group | 0.06 | [−3.47, 3.60] | 0.04 | .972 | |||
| Time | −0.14 | [−0.32, 0.03] | −1.64 | .102 | |||
| Group x Time | −0.17 | [−0.51, 0.17] | −0.97 | .332 | .14 | .33 | |
| DPAS | Intercept | 53.85 | [51.28, 56.41] | 41.19 | <.001 | ||
| Group | −4.34 | [−9.46, 0.79] | −1.66 | .099 | |||
| Time | −0.20 | [−0.42, 0.02] | −1.82 | .070 | |||
| Group x Time | −0.54 | [−0.97, −0.10] | −2.42 | .017 | .53 | .90 |
Notes: CBSST=Cognitive Behavioral Social Skills Training; GFSC=Goal Focused Supportive Contact; ILSS=Independent Living Skills Survey; CMT=Comprehensive Modules Test; SANS = Scale for Assessment of Negative Symptoms; PANSS=Positive and Negative Syndrome Scale; BDI-II=Beck Depression Inventory-II; DPAS=Defeatist Performance Attitude Scale. All models included number of sessions attended (plus all two-way interactions with group and time and the three-way interaction) as a predictor of outcome, but all effects involving number of sessions were non-significant, except the group X session X time interaction in the ILSS model, γ = −0.0003, t = −3.806, p<.001 and the effect of number of sessions attended in the CMT model: γ=0.05, t=2.12, p=.036. Effect sizes (d) were estimated by computing the treatment group difference for HLM model-predicted values for each outcome variable for hypothetical participants with a median number of sessions attended and dividing by the baseline assessment pooled SD.
Figure 2.
Trajectories across assessment points from baseline to 21-month follow-up are shown for hypothetical participants with a median number (14.5) of therapy sessions attended in Cognitive Behavioral Social Skills Training (CBSST) and Goal-Focused Supportive Contact (GFSC). Trajectories were estimated from mixed-effects regression models that showed significant group X time interactions for functioning (Independent Living Skills Survey (ILSS), p=.010), negative symptoms (Scale for Assessment of Negative Symptoms (SANS) Diminished Motivation Factor, p=.018), dysfunctional attitudes (Defeatist Performance Attitude Scale (DPAS), p=.017) and CBSST skills acquisition (Comprehensive Modules Test (CMT), p=.017). Improvement is indicated by increasing scores for ILSS and CMT, and decreasing scores for the DPAS and SANS.
Figure 3.
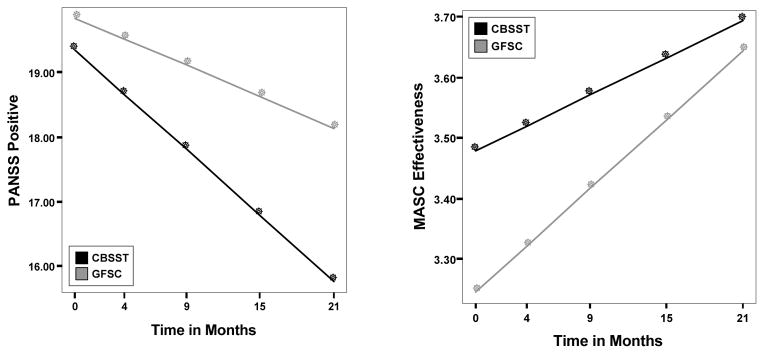
Trajectories across assessment points from baseline to 21-month follow-up are shown for hypothetical participants with a median number (14.5) of therapy sessions attended in Cognitive Behavioral Social Skills Training (CBSST) and Goal-Focused Supportive Contact (GFSC). Trajectories were estimated from mixed-effects regression models that showed a significant time effect for positive symptoms (Positive and Negative Syndrome Scale (PANSS) Positive Subscale, p=.006) and a marginally significant time effect for social competence (Maryland Assessment of Social Competence (MASC), p=.065). Improvement is indicated by decreasing scores for the PANSS and increasing scores for the MASC.
Given our hypothesis that duration of illness might impact defeatist belief severity, duration of illness was included as a covariate in the mixed-effects regression model for DPAS, but was not a significant predictor of the intercept (γ= 0.09, t=0.79, p=.430, 95% CI [−0.14, 0.32] or slope (γ= −0.01, t=−1.38, p=.170, 95% CI [−0.02, 0.00]. The number of older patients was very small (N=11 over age 55; N=0 over 65) in this sample, however, so this may not be an adequate test of the potential impact of duration of illness.
Objective Functioning Milestones
Hierarchical logistic regression models showed a statistically significant group X time interaction for education (γ= 0.17, t=2.06, p=.041, OR=1.18, 95% CI [1.01, 1.38]), indicating significantly greater engagement in educational activities over time in CBSST than in GFSC, but not for living situation (γ= −0.01, t=−0.27, p=.786, OR=0.99, 95% CI [0.91, 1.08]), employment (γ= 0.001, t=0.03, p=.977, OR=1.00, 95% CI [0.92, 1.10]), or psychiatric hospitalizations (γ= 0.03, t=0.58, p=.562, OR=1.03, 95% CI [0.93, 1.13]). A significantly greater proportion of participants were engaged in educational activities at end of treatment in CBSST relative to GFSC (CBSST=21%; GFSC=5%; X2=4.67, p=.031), but the proportion of participants living independently (CBSST=35%; GFSC=26%; X2=0.86, p=.355), working in paid or volunteer jobs (CBSST=38%; GFSC=23%; X2=2.03, p=.154), and hospitalized (CBSST=23%; GFSC=26%; X2(1)=0.043, p=.836) did not differ significantly between the treatment groups. Groups did not differ significantly at baseline on any of these milestones.
Treatment Adherence
The treatment groups did not differ significantly with regard to the mean number of sessions attended (36 possible) during the treatment phase (CBSST M= 12.2, SD= 10.6, range =0–34; GFSC: M=15.6, SD=12.9, range =0–36; t(147)=1.74, p =.083). Participants generally did not take advantage of booster sessions (64% did not attend any of the 12 sessions), but groups did not differ significantly with regard to the mean number of booster sessions attended (CBSST M= 2.2, SD= 3.7, range =0–12; GFSC: M=2.8, SD=4.5, range=0–12; t(147)=0.86, p =.392).
To examine the effects of treatment engagement and dose of intervention, all statistical models reported above included number of sessions attended (plus two-way interactions with group and time, and the three-way interaction) as a predictor of outcome. All of these effects involving number of sessions were non-significant except for the effect of number of sessions attended on the CMT outcome (γ =0.05, t=2.12, p=.036), and in model with ILSS as the outcome, the group X number of sessions X time interaction was significant (γ =−0.0003, t=−3.80, p<.001). The correlation between number of sessions attended and ILSS trajectory (slope across assessment points) was significant for GFSC (r=.27, p=.046), but not for CBSST (r=−.14, p=.356), with greater attendance associated with greater improvement in functioning in GFSC, but not in CBSST. In addition, general hypothesis testing in HLM was used to compare ILSS scores of participants with low attendance (8 sessions) and high attendance (24 sessions). At 21 months, model-estimated ILSS scores for participants in CBSST with low (.753) and high (.728) session attendance did not differ significantly (χ2(1) = 1.23, p = .267, d=−.25), but did differ significantly between participants with low (.631) and high (.690) session attendance in GFSC (χ2(1) = 10.39, p = .002, d=.58). In addition, the effect size for the treatment group difference (CBSST v. GFSC) in model-estimated ILSS scores was small to medium and not significant for participants with high attendance (χ2(1) = 2.57, p = .105, d=.38), but was large and significant for participants with low attendance, (χ2(1) = 17.26, p < .001, d=1.21).
Discussion
The results indicated that CBSST is an effective psychosocial intervention to improve functioning in consumers with schizophrenia. Functioning trajectories over time were significantly more positive in CBSST than in GFSC. Rates of achieving functioning milestones, which are very difficult to impact through available treatments, were also better in CBSST, especially for educational engagement. These findings replicated the results of two prior CBSST clinical trials with older adults (Granholm et al., 2005; Granholm et al., 2007; Granholm et al., 2013) and extended the evidence for better functional outcome to a more representative sample of consumers with schizophrenia. These benefits of CBSST cannot be attributed to nonspecific therapist factors, alone. Functioning outcomes improved to a greater extent in CBSST than in GFSC, suggesting specific CBT and SST interventions were more potent interventions than goal-setting and supportive contact, alone. Taken together, the findings from three CBSST clinical trials suggest that CBSST should be offered over supportive goal-setting interventions to geriatric and non-geriatric consumers with schizophrenia.
Experiential negative symptoms and defeatist performance attitudes also improved to a significantly greater extent in CBSST relative to GFSC. These findings are consistent with another open CBT trial that found significant improvement in both dysfunctional attitudes and negative symptoms in a sample of consumers with psychotic disorders who had not been taking antipsychotic medication (Morrison et al., 2012). Granholm et al. (2013) also found that participants with more severe defeatist attitudes at baseline were more likely to show improved functioning, and that change in defeatist attitudes during treatment predicted better functional outcome nine months after treatment. Given that defeatist performance attitudes have been associated with functional outcome and experiential negative symptoms (Grant & Beck, 2009; Horan et al., 2012; Green et al., 2012), it is possible that reductions in defeatist attitudes in CBT interventions contributed to improvements in these outcomes. However, this is only the first clinical trial to demonstrate significantly greater improvement in experiential negative symptoms in CBSST relative to an active control condition, so it may be premature to recommend CBSST for negative symptoms, until this finding is replicated.
Unlike the present clinical trial, a previous trial of CBSST for older consumers with schizophrenia (Granholm et al., 2013), did not find significantly greater improvement in negative symptoms or defeatist attitudes in CBSST relative to GFSC. Several factors may have contributed to these conflicting findings. First, experiential negative symptoms and defeatist attitudes may be more rigid and resistant to change in older consumers who have experienced decades of illness-related failures, stigma, and negative evaluations by others. In support of this possibility, longer duration of illness and older age have been associated with poorer outcome in CBT for psychosis trials (Drury et al., 1996; Morrison et al., 2004; Morrison et al., 2012), and longer duration of illness was associated with lower self-efficacy in one study (McDermott, 1995). However, the present sample had been ill for two decades on average, so consumers in this study had significant exposure to factors that might impact severity of defeatist attitudes, and we did not find significant associations between duration of illness and severity of defeatist attitudes in the present sample. Second, a factor analytic study of the Dysfunctional Attitudes Scale (DAS Form A) in older (age > 60) adults with nonpsychotic depression did not find strong support for a similar defeatist performance attitude (or “perfectionism”) factor of the DAS in these older consumers, suggesting questionable validity of the DPAS measure in older psychiatric samples (Floyd, Scogin & Chaplin, 2004). A DPAS measure with items more relevant to older consumers (e.g., items on health and loss of independence, rather than achievement) may be needed to adequately test cognitive mediation in CBT studies with older consumers. Finally, it is possible that the SST components and improvement in social skills in CBSST contributed to improvements in functioning and negative symptoms to a greater extent than reduction in defeatist beliefs. Self-efficacy and self-defeatist beliefs might be modified in CBSST, but may not be necessary to improve outcome. Improvements may stem from behavioral activation of practiced skills.
Thus, there is some evidence that functioning and negative symptom outcomes in CBT are mediated by reduction in defeatist attitudes, but this will require further study with larger samples (perhaps combining samples from multiple trials) to increase power to examine defeatist beliefs in the context of other potential mediators and moderators (e.g., age, duration of illness, gender, insight, neurocognitive impairment). Nonetheless, the findings of this study and other recent research (Grant & Beck, 2009; Horan et al., 2012; Granholm et al., 2013; Green et al., 2012), suggest that cognitive therapy interventions targeting defeatist beliefs may help improve functioning and negative symptom outcomes in some consumers with schizophrenia.
It is notable that both treatments showed similar improvements in social competence and positive symptoms. This suggests that an active psychosocial intervention that includes at least supportive contact and systematic recovery-oriented goal setting can be beneficial to consumers with schizophrenia for reducing positive symptom distress and increasing competence in social interactions to some extent (e.g., through interactions with peers in group). Other researchers have pointed out the benefits of supportive contact interventions to consumers with schizophrenia (Penn et al., 2004). Despite the benefits found for GFSC, it is important to note that functioning, negative symptoms, and defeatist attitudes all improved to a greater extent in CBSST than in GFSC, suggesting the specific CBT and SST interventions were more potent than supportive goal-setting interventions to improve these outcomes.
Given the cost and burden of delivering psychosocial interventions, it is important to identify the minimal therapy dosage needed to improve outcomes. On average, participants received only 12 of the 36 CBSST sessions offered and did not actively engage in booster sessions. Nonetheless, negative symptom and functioning outcomes were still superior in CBSST relative to GFSC, and the number of sessions attended was not significantly associated with outcome in CBSST, suggesting additional exposure may not result in additional gains. Morrison and colleagues (2004) also found that the number of sessions delivered was not associated with symptom outcome in a CBT for psychosis effectiveness trial conducted in a community mental health setting. These findings may indicate that less exposure to the CBSST content is a sufficient dosage for benefit. However, additional research is needed to determine the adequate dosage of treatment, because participants were not randomized to longer and shorter treatments, so participant characteristics (e.g., motivation, neurocognitive impairment, illness severity) may have contributed to number of sessions delivered. It will be important to randomize participants to high and low intensity interventions in future trials to identify the optimal number of sessions needed to impact functional outcome in psychosocial rehabilitation interventions.
In contrast to CBSST, in GFSC, additional treatment was significantly associated with better outcome. This difference in dose effects between conditions might be related to the skills training approach of CBSST. In skills-based interventions, participants learn and use skills that can be applied in the absence of a therapist, but when skills are not trained, extended contact with a supportive therapist may be required for meaningful gains. Once consumers learn skills in CBSST, they can continue to use them to work on functioning goals, even if they drop out of treatment. In contrast, once consumers drop out of GFSC, they no longer have the support of the therapist to work on goals. The skills are the active ingredients in CBSST, whereas the therapist and other group members are the primary active ingredients in GFSC. A greater dose of treatment, therefore, leads to greater exposure to the active ingredient in GFSC, but even if consumers dropout in CBSST, they can continue to use the skills they learned to improve functioning and negative symptoms.
Retention in this trial (54%) was much lower than in previous CBSST trials (75–86%; Granholm et al., 2005; Granholm et al., 2013). It is possible that sampling differences contributed to the high dropout rate; in that, the lengthy, repeating nature of the CBSST modules might be more appropriate for an older more chronic population and disliked by non-geriatric consumers, leading to dropout. Dropout rates, however, did not differ significantly between GFSC and CBSST, so repeating the CBSST modules may not be the cause of dropout in this non-geriatric sample. It is possible that challenges related to the limited public transportation system and long travel distances in San Diego County contributed to differences in dropout rates between CBSST clinical trials, because transportation was provided to therapy in previous trials with good retention, but not in the present trial. Mueser and colleagues (2010) also suggested that transportation challenges impacted attendance in a multi-site trial of SST for consumers with serious mental illness, because they found greater attendance (90% v. 66%) at sites with better access to transportation. In future research, modifications like using a shorter, less-redundant intervention and providing transportation might help engage and retain consumers in interventions like CBSST, especially in areas with limited public transportation.
This study had several limitations. As noted above, this clinical trial had a high dropout rate, which limits interpretation of results, because group differences found might reflect a selective bias in who remained in the study. Several steps were taken to address this and increase confidence in the results. First, the mixed-effects regression analyses used, do not require complete data and allow for a larger number of participants to be included than would be possible with traditional ANOVA-based designs, which increases both power and generalizability. Second, several analyses were conducted to identify possible biases introduced by drop-out rates. The two treatment groups did not differ significantly in drop-out rates, and participants who dropped out did not differ significantly from those retained on any of the key outcome variables at baseline. These analyses provided no evidence that drop-out rates introduced a systematic bias into the sample.
Another important limitation was that the primary outcome measure was a self-report measure of functioning, and the validity of patient-reported outcomes has been questioned in this population (Bowie et al., 2007; Sabbag et al., 2012). However, significant change was also found on at least one objective functioning milestone (educational activities), which provided some additional support for greater improvement in functioning in CBSST. The study also cannot answer the question of whether CBSST should be offered over CBT or SST. The relative efficacy these interventions bundled into CBSST is an area requiring additional research. Finally, the present trial did not inform which patients should be offered CBSST. More research is needed to identify which consumers are more likely to benefit.
Despite these limitations, identifying treatments to improve functioning and reduce negative symptoms in consumers with schizophrenia is of high public health significance, and the results of this randomized clinical trial indicated that CBSST is an effective psychosocial intervention to improve these outcomes in some consumers with schizophrenia.
Acknowledgments
We thank the participants who volunteered for this study. Research reported in this publication was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Rehabilitation Research and Development Service, and the National Institute of Mental Health of the National Institutes of Health (RO1MH071410 and P30MH66248).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Andreasen NC. Negative symptoms in schizophrenia: Definition and reliability. Archives of General Psychiatry. 1982;39:784–788. doi: 10.1001/archpsyc.1982.04290070020005. [DOI] [PubMed] [Google Scholar]
- Arns P, Rogers ES, Cook J, Mowbray C. The IAPSRS toolkit: Development, utility, and relation to other performance measurement systems. Psychiatric Rehabilitation Journal. 2001;25:43–52. doi: 10.1037/h0095051. [DOI] [PubMed] [Google Scholar]
- Avery R, Startup M, Calabria K. The role of effort, cognitive expectancy appraisals and coping style in the maintenance of the negative symptoms of schizophrenia. Psychiatry Research. 2009;167:36–46. doi: 10.1016/j.psychres.2008.04.016. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Mueser KT, Forester BP, Wolfe R, Cather C, Xie H, McHugo GJ, Bird B, Aschbrenner KA, Naslund JA, Feldman J. Long-Term Outcomes of a Randomized Trial of Integrated Skills Training and Preventive Healthcare for Older Adults with Serious Mental Illness. American Journal of Geriatric Psychiatry. 2013 doi: 10.1016/j.jagp.2013.04.013. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Bellack AS, Mueser KT, Gingerich S, Agresta J. Social Skills Training for Schizophrenia: A Step-by-Step Guide. 2. New York: Guilford Press; 2004. [Google Scholar]
- Bellack AS, Mueser KT. Psychosocial treatment for schizophrenia. Schizophrenia Bulletin. 1993;19:317–336. doi: 10.1093/schbul/19.2.317. [DOI] [PubMed] [Google Scholar]
- Bellack AS, Sayers M, Mueser KT, Bennett M. Evaluation of social problem solving in schizophrenia. Journal of Abnormal Psychology. 1994;103:371–378. doi: 10.1037//0021-843x.103.2.371. [DOI] [PubMed] [Google Scholar]
- Benton MK, Schroeder HE. Social skills training with schizophrenics: A meta-analytic evaluation. Journal of Consulting and Clinical Psychology. 1990;58:741–747. doi: 10.1037//0022-006x.58.6.741. [DOI] [PubMed] [Google Scholar]
- Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophrenia Bulletin. 2006;32:238–245. doi: 10.1093/schbul/sbj013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie CR, Twamley EW, Anderson H, Halpern B, Patterson TL, Harvey PD. Self-assessment of functional status in schizophrenia. Journal of Psychiatric Research. 2007;41:1012–1018. doi: 10.1016/j.jpsychires.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan RW. Persistent negative symptoms in schizophrenia: An Overview. Schizophrenia Bulletin. 2007;33:1013–1022. doi: 10.1093/schbul/sbl057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cane DB, Olinger LJ, Gotlib IH, Kuiper NA. Factor structure of the dysfunctional attitude scale in a student population. Journal of Clinical Psychology. 1986;42:307–309. [Google Scholar]
- Cardenas V, Abel S, Bowie CR, Tiznado D, Depp CA, Patterson TL, Jeste DV, Mausbach BT. When functional capacity and real-world functioning converge: the role of self-efficacy. Schizophrenia Bulletin. 2013;39:908–916. doi: 10.1093/schbul/sbs004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drury V, Birchwood M, Cochrane R, Macmillan F. Cognitive therapy and recovery from acute psychosis: A controlled trial. II. Impact on recovery time. British Journal of Psychiatry. 1996;169:602–607. doi: 10.1192/bjp.169.5.602. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders, clinician version (SCID-CV) Washington, D.C: American Psychiatric Press, Inc; 1996. [Google Scholar]
- Floyd M, Scogin F, Chaplin WF. The Dysfunctional Attitudes Scale: factor structure, reliability, and validity with older adults. Aging and Mental Health. 2004;8:153–160. doi: 10.1080/13607860410001649572. [DOI] [PubMed] [Google Scholar]
- Granholm E, McQuaid JR, Auslander L, McClure FS. Group cognitive-behavioral social skills training for older outpatients with chronic schizophrenia. Journal of Cognitive Psychotherapy. 2004;18:266–279. [Google Scholar]
- Granholm E, McQuaid JR, McClure FS, Auslander LA, Perivoliotis D, Pedrelli P, Jeste DV. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. American Journal of Psychiatry. 2005;162:520–529. doi: 10.1176/appi.ajp.162.3.520. [DOI] [PubMed] [Google Scholar]
- Granholm E, McQuaid JR, McClure FS, Link PC, Perivoliotis D, Gottlieb JD, Jeste DV. Randomized controlled trial of cognitive behavioral social skills training for older people with schizophrenia: 12-month follow-up. Journal of Clinical Psychiatry. 2007;68:730–737. doi: 10.4088/jcp.v68n0510. [DOI] [PubMed] [Google Scholar]
- Granholm E, Holden J, Link PC, McQuaid JR, Jeste DV. Randomized controlled trial of cognitive behavioral social skills training for older consumers with schizophrenia: Defeatist performance attitudes and functional outcome. American Journal of Geriatric Psychiatry. 2013;21:251–262. doi: 10.1016/j.jagp.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophrenia Bulletin. 2009;35:798–806. doi: 10.1093/schbul/sbn008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant PM, Huh GA, Perivoliotis D, Beck AT. Randomized trial to evaluate the efficacy of cognitive therapy for low-functioning patients with schizophrenia. Archives of General Psychiatry. 2012;69:121–127. doi: 10.1001/archgenpsychiatry.2011.129. [DOI] [PubMed] [Google Scholar]
- Green MF, Hellemann G, Horan WP, Lee J, Wynn JK. From perception to functional outcome in schizophrenia: modeling the role of ability and motivation. Archives of Generiatric Psychiatry. 2012;69:1216–1224. doi: 10.1001/archgenpsychiatry.2012.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock G, Devane S, Bradshaw T, McGovern J, Tarrier N, Kinderman P, Harris N. An investigation into the psychometric properties of the Cognitive Therapy Scale for Psychosis (CTS-Psy) Behavioural & Cognitive Psychotherapy. 2001;29:221–233. [Google Scholar]
- Harvey PD, Heaton RK, Carpenter WT, Jr, Green MF, Gold JM, Schoenbaum M. Functional impairment in people with schizophrenia: Focus on employability and eligibility for disability compensation. Schizophrenia Research. 2012;140:1–8. doi: 10.1016/j.schres.2012.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PD, Strassnig M. Predicting the severity of everyday functional disability in people with schizophrenia: Cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry. 2012;11:73–79. doi: 10.1016/j.wpsyc.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill K, Startup M. The relationship between internalized stigma, negative symptoms and social functioning in schizophrenia: the mediating role of self-efficacy. Psychiatry Research. 2013;30:151–157. doi: 10.1016/j.psychres.2012.09.056. [DOI] [PubMed] [Google Scholar]
- Horan WP, Rassovsky Y, Kern RS, Lee J, Wynn JK, Green MF. Further support for the role of dysfunctional attitudes in models of real-world functioning in schizophrenia. Journal of Psychiatric Research. 2010;44:499–505. doi: 10.1016/j.jpsychires.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick B, Fenton W, Carpenter WT, Marder SR. The NIMH-MATRICS consensus statement on negative symtoms. Schizophrenia Bulletin. 2006;32:214–219. doi: 10.1093/schbul/sbj053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klingberg S, Wölwer W, Engel C, Wittorf A, Herrlich J, Meisner C, Buchkremer G, Wiedemann G. Negative symptoms of schizophrenia as primary target of cognitive behavioral therapy: results of the randomized clinical TONES study. Schizophrenia Bulletin. 2011;37:98–110. doi: 10.1093/schbul/sbr073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB. The schizophrenia patient outcomes research team (PORT): Updated treatment recommendations 2009. Schizophrenia Bulletin. 2010;36:94–103. doi: 10.1093/schbul/sbp130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz MM, Mueser KT. A meta-analysis of controlled research on social skills training for schizophrenia. Journal of Consulting Clinical Psychology. 2008;76:491–504. doi: 10.1037/0022-006X.76.3.491. [DOI] [PubMed] [Google Scholar]
- Kurtz MM, Olfson RH, Rose J. Self-efficacy and functional status in schizophrenia: relationship to insight, cognition and negative symptoms. Schizophrenia Research. 2013;145:69–74. doi: 10.1016/j.schres.2012.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberman RP. Psychosocial treatments for schizophrenia. Psychiatry. 1994;57:104–114. doi: 10.1080/00332747.1994.11024674. [DOI] [PubMed] [Google Scholar]
- McDermott BE. Development of an instrument for assessing self-efficacy in schizophrenic spectrum disorders. Journal of Clinical Psychology. 1995;51:320–331. [PubMed] [Google Scholar]
- McQuaid JR, Granholm E, McClure FS, Roepke S, Pedrelli P, Patterson TL, Jeste DV. Development of an integrated cognitive-behavioral and social skills training intervention for older patients with schizophrenia. Journal of Psychotherapy Practice and Research. 2000;9:149–156. [PMC free article] [PubMed] [Google Scholar]
- Morrison AP, Turkington E, Wardle M, Spencer H, Barratt S, Dudley R, Brabban A, Hutton P. A preliminary exploration of predictors of outcome and cognitive mechanisms of change in cognitive behavior therapy for psychosis in people not taking antipsychotic medication. Behaviour Research and Therapy. 2012;50:163–167. doi: 10.1016/j.brat.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Morrison AP, Renton JC, Williams S, Dunn H, Knight A, Kreutz M, Nothard S, Patel U, Dunn G. Delivering cognitive therapy to people with psychosis in a community mental health setting: An effectiveness study. Acta Psychiatrica Scandinavica. 2004;110:36–44. doi: 10.1111/j.1600-0447.2004.00299.x. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Pratt SI, Bartels SJ, Swain K, Forester B, Cather C, Feldman J. Randomized trial of social rehabilitation and integrated health care for older people with severe mental illness. Journal of Consulting Clinical Psychology. 2010;78:561–573. doi: 10.1037/a0019629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penn DL, Mueser KT, Tarrier N, Gloege A, Corrine C, Serrano D, Otto MW. Supportive therapy for schizophrenia: Possible mechanisms and implications for adjunctive psychosocial treatments. Schizophrenia Bulletin. 2004;30:101–112. doi: 10.1093/oxfordjournals.schbul.a007055. [DOI] [PubMed] [Google Scholar]
- Peralta V, Cuesta MJ. Dimensional structure of psychotic symptoms: An item-level analysis of SAPS and SANS symptoms in psychotic disorders. Schizophrenia Research. 1999;38:13–26. doi: 10.1016/s0920-9964(99)00003-1. [DOI] [PubMed] [Google Scholar]
- Pratt SI, Mueser KT, Smith TE, Lu W. Self-efficacy and psychosocial functioning in schizophrenia: a mediational analysis. Schizophrenia Research. 2005;78:187–197. doi: 10.1016/j.schres.2005.02.014. [DOI] [PubMed] [Google Scholar]
- Rector NA, Beck AT, Stolar N. The negative symptoms of schizophrenia: A cognitive perspective. Canadian Journal of Psychiatry. 2005;50:247–257. doi: 10.1177/070674370505000503. [DOI] [PubMed] [Google Scholar]
- Sabbag S, Twamley EW, Vella L, Heaton RK, Patterson TL, Harvey PD. Predictors of the accuracy of self assessment of everyday functioning in people with schizophrenia. Schizophrenia Research. 2012;137:190–195. doi: 10.1016/j.schres.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayers SL, Curran PJ, Mueser KT. Factor structure and construct validity of the scale for the assessment of negative symptoms. Psychological Assessment. 1996;8:269–280. [Google Scholar]
- Turkington D, Kingdon D, Turner T. Effectiveness of a brief cognitive-behavioural therapy intervention in the treatment of schizophrenia. British Journal of Psychiatry. 2002;180:523–527. doi: 10.1192/bjp.180.6.523. [DOI] [PubMed] [Google Scholar]
- Wallace CJ, Liberman RP, Tauber R, Wallace J. The independent living skills survey: A comprehensive measure of the community functioning of severely and persistently mentally ill individuals. Schizophrenia Bulletin. 2000;26:631–658. doi: 10.1093/oxfordjournals.schbul.a033483. [DOI] [PubMed] [Google Scholar]
- Weissman AN, Beck AT. Development and validation of the dysfunctional attitude scale: A preliminary investigation. Paper presented at the Annual Meeting of the American Educational Research Association; Toronto, CA. 1978. [Google Scholar]
- Weissman AN. Assessing depressogenic attitudes: A validation study. Paper presented at the 51st annual meeting of the Eastern Psychological Association; Hartford, CT. 1980. [Google Scholar]
- Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: Effect sizes, clinical models, and methodological rigor. Schizophrenia Bulletin. 2008;34:523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanos PT, Primavera LH, Knight EL. Consumer-run service participation, recovery of social functioning, and the mediating role of psychological factors. Psychiatric Services. 2001;52:493–500. doi: 10.1176/appi.ps.52.4.493. [DOI] [PubMed] [Google Scholar]