Abstract
Objective
Psychological interventions can attenuate distress and enhance coping for those with an initial diagnosis of cancer, but there are few intervention options for individuals with cancer recurrence. To address this gap, we developed and tested a novel treatment combining Mindfulness, Hope Therapy, and biobehavioral components.
Method
An uncontrolled, repeated measures design was used. Women (N=32) with recurrent breast or gynecologic cancers were provided 20 treatment sessions in individual (n=12) or group formats (n=20). On average, participants were middle aged (M=58) and Caucasian (81%). Independent variables (i.e., hope and mindfulness) and psychological outcomes (i.e., depression, mood, worry, and symptoms of generalized anxiety disorder) were assessed pre-treatment and 2-, 4-, and 7-months later. Session-by-session therapy process (positive and negative affect, quality-of-life) and mechanism (use of intervention-specific skills) measures were also included.
Results
Distress, anxiety, and negative affect decreased, while positive affect and mental health-related quality-of-life increased over the course of treatment, as demonstrated in mixed-effects models with the intent-to-treat sample. Both hope and mindfulness increased, and use of mindfulness skills was related to decreased anxiety.
Conclusions
This treatment was feasible to deliver and acceptable to patients. The trial serves as preliminary evidence for a multi-component intervention tailored to treat difficulties specific to recurrent cancer. The blending of the components was novel as well as theoretically and practically consistent. A gap in the literature is addressed, providing directions for testing interventions designed for patients coping with the continuing stressors and challenges of cancer recurrence.
Keywords: biobehavioral, cancer, hope, mindfulness, recurrence
Introduction
Pioneers in developing psychosocial interventions, Avery Weisman and J. William Worden (1986) noted that for many, cancer recurrence is one of the most discouraging and difficult periods for an individual to face. Whenever a cancer diagnosis occurs, it is accompanied by psychological and biological stress (Andersen et al., 1998). At recurrence, prospective, controlled research shows patients' cancer-related traumatic stress symptoms are significant and when compared to their responses at their initial diagnosis, the stress is comparable (Andersen, Shapiro, Farrar, Crespin, & Wells-Di Gregorio, 2005). Controlled longitudinal data also show distress remains high for the next year (Andersen et al., 2010; Bull et al., 1999; Yang, Brothers, & Andersen, 2008). In addition, the burden of physical symptoms can be life changing. Patients experience greater fatigue and slower recovery following recurrence treatments compared to initial diagnosis (Kenne Sarenmalm, Öhlén, Odén, & Gaston-Johansson, 2008; Yang, Thornton, Shapiro, & Andersen, 2008). Both traumatic psychological and physical symptoms tax coping abilities, making it more likely for individuals to slip into troublesome strategies such as avoiding or disengaging from cancer-specific thoughts or situations (Yang, Brothers, et al., 2008).
There have been few successful trials or tests with adequate sample sizes (N>20) of interventions tailored for patients with recurrence. An exception is the three successful trials (Goodwin, Leszcz, & Ennis, 2001; Kissane et al., 2007; Spiegel, Bloom, Kraemer, & Gottheil, 1989; Spiegel et al., 2007) of supportive expressive therapy (SET) — a treatment focusing on death anxiety, isolation, responsibility, choice, and meaning. In these trials, SET effectively reduced distress and improved other outcomes such as reducing pain symptoms. However, SET is delivered to patients in groups that meet for one year or longer, a format that would be difficult to implement in many settings. Other intervention trials have had null effects on stress, negative mood, and/or depressive symptoms outcomes when testing psychoeducation (Akechi et al., 2007), peer support (Gotay et al., 2007), or expressive writing (de Moor et al., 2002; Low, Stanton, Bower, & Gyllenhammer, 2010).
Thus, the existing psychological interventions are those to ease the burden for patients with their first cancer diagnosis (Edwards, Hulbert-Williams, & Neal, 2008; Galway et al., 2012; Stanton, 2006). One such intervention, a biobehavioral one (Andersen, Golden-Kreutz, Emery, & Thiel, 2009), showed robust gains (e.g., distress, social support, physical symptoms; Andersen et al., 2007; Andersen et al., 2004). Intervention components included progressive muscle relaxation, understanding cancer stress, positive ways to cope, problem solving, and assertive communication and social support, and also strategies for improving health behaviors and compliance with cancer treatments. The appropriateness of each component for recurrence patients was considered. Several components were deemed relevant and could be delivered as manualized (e.g., social support) or easily tailored to the recurrence experience (e.g., health behaviors). A few components (e.g., disease/treatment information) seemed unnecessary for those familiar with the rigors of cancer therapies.
To identify other topics of importance, interviews with patients were undertaken (Thornton et al., 2014). Qualitative data pointed to problems unique to the recurrence experience including: chronic cancer-specific stress and a sense of foreboding; a shrinking social network; loss of intimacy with partner; and unabated physical discomfort and fatigue for which treatment options were limited. This led to integration of two additional components and, ultimately, a tailored treatment for women with recurrent cancer emerged. Thus, the research aim was to conduct a phase II trial (Campbell et al., 2000) designed to test for the treatment's feasibility, acceptability, and preliminary treatment effects. We first detail the rationale for the two new components—mindfulness and hope.
The role of mindfulness
A Mindfulness component was chosen for several reasons. In qualitative interviews, women with recurrent cancer report a multitude of thoughts and feelings related to chronic physical symptoms, repeated rounds of chemotherapy, ruminations of the past, and worries about the future (Thornton, et al., 2014). Additionally, the aforementioned thoughts and related ones were usually circumstances that could not be readily changed. An initial cancer diagnosis focuses the patient on seeking out resources, familiarizing oneself with treatments and disease, etc. Instead, the recurrence stressor requires mobilization for coping in the long term, i.e., viewing cancer as chronic condition rather than an acute one, coping with maintenance cancer therapy (i.e., continuous), or experiencing stable (or increasing) symptoms rather than a recovery trajectory. This necessitates a shift in thinking and action, requiring recognition that coping methods are not for some endpoint, but rather a process.
Mindfulness has been defined as “paying attention in a particular way: on purpose, in the present moment, and nonjudgmentally” (Kabat-Zinn, 1994, p. 4). For many with recurrence, stress (Yang, Brothers, et al., 2008), depression (Brothers & Andersen, 2009), or anxiety symptoms (Sarenmalm, Öhlén, Odén, & Gaston-Johansson, 2008) are troublesome, and to the extent they are associated with thoughts and feelings tied to the past or worries of the future, mindfulness skills should encourage focus on the present moment. To the degree circumstances cannot be imminently changed, accepting (as opposed to changing, suppressing, or avoiding) the thoughts and feelings might reduce negative sequelae associated with such thoughts.
Mindfulness interventions have been used to successfully reduce symptoms of depression and anxiety and improve mood and quality-of-life with a variety of clinical samples (Hofmann, Sawyer, Witt, & Oh, 2010), including cancer patients (Carlson et al., 2013; Hoffman et al., 2012; Shennan, Payne, & Fenlon, 2011). Consistent with previous meta-analytic reviews (e.g., Hoffmann, Sawyer, Witt, & Oh, 2010), a recent meta-analysis focused specifically on cancer patients, Piet, Wurtzen, and Zachariae (2012) found that mindfulness-based therapies resulted in significant decreases in symptoms of anxiety and depression and increases in mindfulness skills. Overall, the effect sizes associated with reductions in symptoms of anxiety and depression were .60 and .42, respectively, with the estimates from randomized controlled trials being .37 and .44, respectively. These results are comparable to results from meta-analyses examining the effect of psychological interventions on symptoms of anxiety and depression in cancer patients, with effect sizes ranging from .36 - .40 and .19 - .47, respectively (Naaman, Radwan, Fergusson, & Johnson, 2009; Sheard & Maguire, 1999). Data on other outcomes from individual studies of mindfulness-based treatments have found improvements in sleep (Andersen et al., 2013; Garland et al., 2014), fatigue (Carlson & Garland, 2005), and energy levels (Lengacher et al., 2009).
The role of hope
A theme highlighted in our qualitative study was that of recurrence hindering important goal pursuits and worries that some goals were now impossible. Evidence suggests that, compared to healthy controls, cancer patients generally report fewer achievement and leisure goals (Pinquart, Fröhlich, & Silbereisen, 2008). Schumacher (1990) found that two-thirds of cancer patients reported that physical limitations from the cancer negatively impact goal pursuits.
In Snyder's (1994) definition, hope is conceptualized as beliefs about one's ability to generate ways to reach important goals and the requisite motivation to initiate and sustain movement toward goals. Hope is operationalized as a positive motivational state based on a sense of successful agency (goal-directed energy) coupled with pathways (specific plans to meet goals; Snyder, Irving, & Anderson, 1991). More specifically, Snyder (2002) suggested that individuals reporting higher levels of hope are able to adjust their goals and redirect their energies toward important goal pursuits, such as maintaining a medical regimen (see also Gum & Snyder, 2002; Snyder, Sympson, Ybasco, Borders, Babyak, & Higgins, 1996). Cancer recurrence can change the salience of a goal and decrease hopeful thoughts of achieving the goal (Thornton, et al., 2014).
Hope has been related to functioning in both physical (e.g., Berg, Snyder, & Hamilton, 2008; Snyder, Irving, & Anderson, 1991) and psychological (e.g., Feldman & Snyder, 2005; Wrobeski & Snyder, 2005) domains. When studied as an individual difference variable, women with breast cancer endorsing higher hope were more likely to use coping strategies that improved their adjustment (Stanton, Danoff-Burg, & Huggins, 2002). In lung cancer, hope was inversely related to chronic physical symptoms (e.g., pain, fatigue, coughing) and depressive symptoms (Berendes et al., 2010). Lastly, we learned previously that hopelessness at recurrence heightens risk for later depressive symptoms (Brothers & Andersen, 2009). Taken together, higher levels of hope may enable cancer patients to optimize coping strategies, leading to better psychological functioning.
Most investigations have examined hope as an individual difference variable. However, Cheavens and colleagues (2006) developed a manualized intervention to increase hope. In the initial trial, community participants receiving the hope intervention demonstrated significant increases in agency, self-esteem, and meaning in life and decreases in anxiety and depressive symptoms compared to participants in a wait-list control group. Importantly, change in hope scores was associated with pre to post-treatment reductions in depressive and anxiety symptoms, suggesting an intervention component focused on increasing hope could help patients achieve goals in the midst of coping with recurrence.
The phase II trial
Thus, a novel treatment was developed. Two elements—mindfulness and hope—were thought to be uniquely suited to the circumstances of patients with recurrence. Selected components from an efficacious biobehavioral intervention were also included to reduce stress, enhance quality-of-life, and provide domains for goal specification. Women with recurrent breast or gynecologic cancer were enrolled, and both group and individual formats were used. As this was a first test, we sought to determine feasibility of delivery and treatment acceptability.
The trial was designed using psychotherapy outcome research methodologies, which included having outcome, process, and mechanism measures and their corresponding statistical models. Regarding outcomes, we predicted significant declines in negative mood and anxious and depressive symptoms. In addition to overall change, the index proposed by Jacobson, Roberts, Berns, and McGlinchey (1999) was used to determine if reliable change occurred for individual patients, i.e., the percentage of individuals showing reliable change (improvements) on the outcome measures.
Complementary to the outcome data, treatment process measures detailed the trajectory of change, session-by-session, in patients' affect and quality-of-life. We would consider the treatment as promising if it was associated with a steady upward trajectory for patients' ratings of positive affect and emotional quality-of-life and a steady downward trajectory for negative affect. We also included a physical health quality-of-life measure, but we were unsure if any improvement would be evidenced because of the stable (or increasing) level of physical symptoms found for patients with recurrence (Sarenmalm, Öhlén, Odén, & Gaston-Johansson, 2008; Yang, Thornton, et al., 2008).
Lastly, we hypothesized that hope and/or mindfulness would be mechanism(s) for any pre/post outcome changes. After first determining if pre- to post-change in mindfulness and hope measure scores had occurred, two analytic methods were used. The first tested the relationship between pre/post change on the hope and mindfulness measures with the pre/post changes in outcomes. The second tested the relationship of patients' session-by-session usage of hope and mindfulness strategies and change in outcomes. These are complementary analyses, with the former shedding light on whether or not “global” hope/mindfulness covaried with outcomes and the latter testing whether or not “doing” hope/mindfulness occurred, and if so, whether it covaried with outcomes.
Methods
Participants
Thirty-two female patients were enrolled and initiated treatment. On average, participants were middle aged (M=58), Caucasian (81%), and living with a spouse or partner (69%). Half of the women were college educated (50%); many were working outside the home (44%) and most (69%) had a family income greater than $50,000/year. Table 1 provides disease and treatment characteristics for the initial and recurrence diagnoses.
Table 1. Disease and Cancer Treatment Characteristics for the Sample (N=32).
| Variable | Mean (SD) or % |
|---|---|
| Breast (n=18) vs. gynecologic (n=14); % breast | 56% |
| Time Since Initial Diagnosis, years | 10.07 (7.15) |
| Range (1-31) | |
| Disease Free Interval, years | 5.21 (5.62) |
| Range (.5-26) | |
| Time since first recurrence, years, breast | 6.81 (6.02) |
| Time since first recurrence, years, gynecologic | 2.36 (1.88) |
| Current extent of disease | |
| None; No evidence of disease (n=6) | 19% |
| Local or regional metastases (n=9) | 28% |
| Distant metastases (n=17) | 53% |
| Current cancer treatment | |
| None (n=7) | 22% |
| Chemotherapy (n=22) | 69% |
| Hormonal therapy (n=7) | 22% |
Procedures
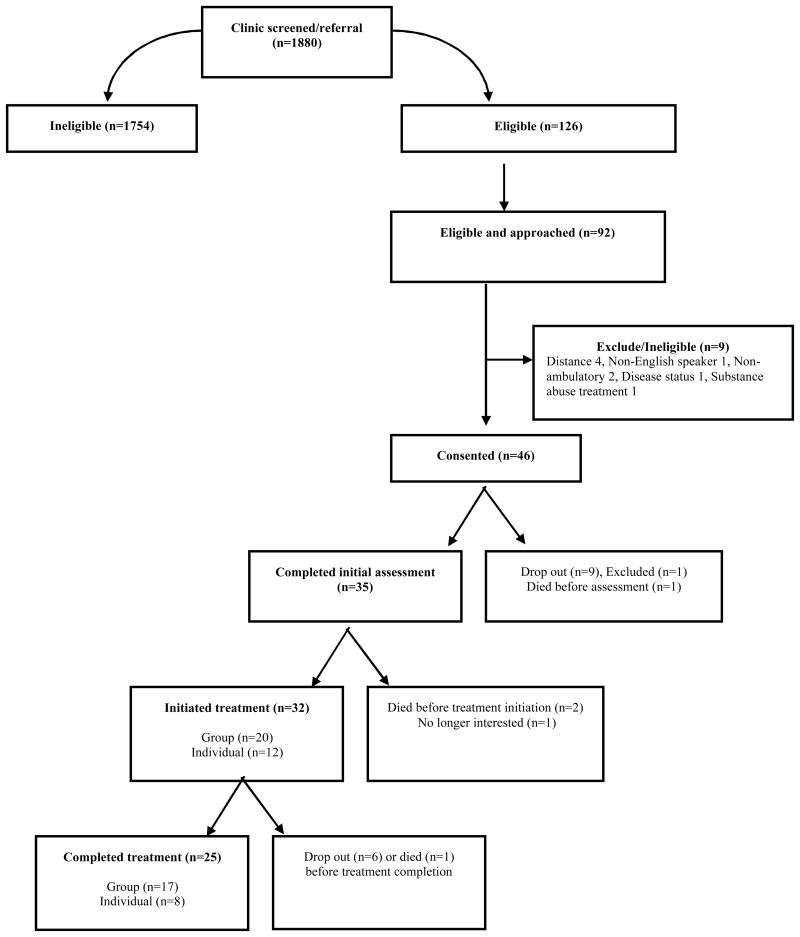
Patients with a breast or gynecologic cancer recurrence were sought from medical and gynecology oncology clinics at a university-affiliated, National Cancer Institute-designated Comprehensive Cancer Center. Eligibility criteria were as follows: diagnosis of recurrent breast or gynecologic cancer, age > 21 or < 85 years, English speaking, and residence < 70 miles from the treatment center. Exclusion criteria were previous diagnosis of intellectual or neurological condition preventing informed consent, previous diagnosis of immunologic illness/condition (e.g. arthritis), or life expectancy < 160 days. Following institutional review board approval, potentially eligible patients were identified and approached by a female research assistant who explained the study and conducted informed consent for those remaining eligible and interested. The primary reason for ineligibility was a patient not having recurrent disease. See Figure 1 for study flow.
Figure 1.
Study flow.
Following informed consent, an initial assessment of outcomes and mechanisms was conducted. Intervention sessions were delivered either individually or in a group in a Department of Psychology outpatient clinic at the University. Masters- and doctoral clinical psychologists delivered individual treatment to 12 patients and doctoral psychologists also jointly conducted two cohorts of group treatment, with 10 patients per group. The intervention was manualized, and to further standardize content and delivery, patients received a treatment guidebook consisting of overviews of in-session content, readings, worksheets, and homework assignments for each session. Group sessions lasted for 90 minutes and individual sessions lasted 50; all were audio/video taped. Twenty sessions were provided in two phases, an intensive phase of 16 weekly sessions and a maintenance phase of two biweekly and then two monthly sessions, for total treatment duration of 7 months. Prior to each therapy session patients completed the process measures of affect and quality-of-life. Treatment acceptability, outcomes, and mechanism measures were also collected at two- (mid-intensive phase), four- (post-intensive phase), and seven-months (post-maintenance phase). Patients were paid $50 for each assessment.
Treatment
The treatment integrated three components: Mindfulness, Hope Therapy, and Biobehavioral (see Supplementary Material). To begin, the role of each component in managing stress was discussed. It was noted that many, but not all, stressors could be managed effectively using hope building and biobehavioral components. On the other hand, problem solving might not be effective in a given moment and “fighting” or “giving up” would be similarly unhelpful. Also, a problem-solving orientation always focused on the future can detract from the joys available presently. Thus, mindfulness training was to enable patients to accept and be with the experience of the moment.
Mindfulness content was based on the Mindfulness-Based Stress Reduction (MBSR) intervention developed by Kabat-Zinn (1991) and related interventions from Stahl and Goldstein (2010). The principles of Mindfulness were introduced in the first session and discussed in sessions 2-4, with Mindfulness characterized as a way to accept “what is” in the present moment, as opposed to what “should be,” “has been,” or “might be.” All sessions started with a formal exercise (e.g., body scan, observing thoughts; see Supplemental Material). Participants were instructed to use both formal and informal mindfulness practices (i.e., paying attention while engaged in an activity not specifically designated as a mindfulness practice) each week. Goals for Mindfulness practice were to a) develop awareness (e.g., thoughts were viewed as mental events rather than “facts” to decrease their power in driving negative mood and behavior); b) cultivate acceptance; and, c) detach from negative thinking (i.e., find a non-judgmental stance). Following session one, each session began with a homework check-in and then the formal mindfulness exercise began.
As previously manualized (Cheavens, et al., 2006), the principles of Hope Therapy were highlighted in sessions 4 through 9, with goal setting continuing through the remaining ones. The focus was progress toward achieving specific, realistic, and measureable goals. Patients were asked to identify value-derived goals (i.e., goals for the most important domains of one's life) and ones sufficiently important to sustain movement toward them in the next two to four months. Also, the biobehavioral content (see below) provided domains for goal setting. Patients' discussed their goal possibilities, providing a forum to ensure that goals were manageable ones. In accordance with principles of Hope Therapy, patients learned strategies (e.g., to approach goals rather than avoid obstacles, define markers of progress, etc.) to refine their goals, generate pathways to goals, and address potential obstacles and blockages. Additionally, goals provided the context for demonstrations of agentic thinking (e.g., I will be able to do this) and interventions to increase agentic thinking. For additional description, see Cheavens et al. (2006).
The Biobehavioral Intervention (BBI; Andersen, et al., 2009) content occurred primarily in sessions 7 thru 13. In concert with Hope Therapy, the BBI content was introduced and then implemented via goal setting and identifying pathways to goals. The BBI components used were as follows: understanding one's stress response, information seeking, social support, assertive communication, sexuality, and health behaviors.
Although the trial was not designed or powered to test interactions, in developing the treatment we expected skills associated with each component to transact such that overall functioning would be improved. For example, we anticipated that mindfulness skills would be relevant for more hopeful thought in that purposeful paying of attention in the moment is likely to increase goal orientation and skillful goal pursuit. Similarly, hope skills may be used to engage in mindfulness practices such that developing plans for formal practices and identifying obstacles to maintaining mindfulness would be incorporated into goal pursuits. The biobehavioral component would provide patients with content and information relevant to identifying goals.
Therapists
A doctoral-level, lead therapist (LT) wrote both therapist and patient manuals, co-led the two treatment groups, treated some patients individually, and supervised other therapists. As expertise of mindfulness delivery is important, it is noted that the lead therapist had extensive experience, i.e., 3 years of experience in mindfulness, including personal practice, training in Mindfulness-Based Stress Reduction (8-week MBSR course, 1-week program under the direction of Dr. Jon Kabat Zinn and Dr. Saki Santorelli), and multiple retreats, including 5-7 day silent, teacher-led meditation retreats. Other investigators (BA and JC) provided expertise for manual writing and consultation in biobehavioral intervention, mindfulness, and hope therapy delivery throughout the study period.
Other therapists were post-doctoral and advanced pre-doctoral trainees who had specialty training in psycho-oncology and mindfulness. Protocol training emphasized the integration of mindfulness with the more cognitive-behavioral elements in the Hope and Biobehavioral therapies. All therapists maintained a personal mindfulness practice throughout training and intervention delivery. Use of the therapist and patient manuals ensured that the treatment content was delivered as intended/written across therapists, and hour-for-hour supervision of the therapists (done via audio/video tapes of the sessions) by senior therapists enhanced clinical skill of the intervention delivery.
Measures
Feasibility and Acceptability of Treatment
We assessed feasibility and acceptability in several ways. First, we considered treatment attrition (dropout) and session attendance rate. Additionally, patients rated the acceptability of treatment, if the treatment was ethical, how effective the treatment was thought to be, and the likelihood of negative side effects from the treatment. An item was used for each, rated on a semantic differential scale from 1-7 with relevant anchors for each item (e.g., very acceptable/unacceptable, unethical/fully ethical). Cohesion was assessed with two items (involvement in the therapy experience, felt support from therapy) using a rating scale ranging from 0 (not at all) to 10 (extremely; Andersen, Shelby, & Golden-Kreutz, 2007).
Treatment Outcomes
Anxiety related symptoms
Two measures were used. The Generalized Anxiety Disorder Questionnaire-IV (GADQ-IV; Newman et al., 2002; Rodebaugh, Holaway, & Heimberg, 2008) consists of nine items based on the DSM-IV-TR (American Psychiatric Association, 2000) criteria for Generalized Anxiety Disorder. A continuous score from 0 to 33 can be calculated by summing the items. The measure has shown adequate reliability and validity (Newman, et al., 2002). Internal consistency was .83. The Penn State Worry Questionnaire-Abbreviated (PSWQ; Hopko et al., 2003; Meyer, Miller, Metzger, Borkovec, & et al., 1990) was used to assess worry. Eight items regarding the prevalence and controllability of worry are rated from 1 (not at all) to 5 (very typical) and then summed. Scores range from 8 to 40 and higher scores indicate greater worry. The PSWQ is a valid and reliable measure for use with both older and younger adults (Crittendon & Hopko, 2006). Internal consistency at baseline was .96.
Depressive symptoms
The 20-item Center for Epidemiological Studies Depression scale (CES-D) assesses affective, cognitive, and vegetative symptoms (Comstock & Helsing, 1976; Radloff, 1977). Items (e.g., “I felt lonely”) are rated on a scale from 0 (hardly ever or never) to 3 (most of the time) as being self-descriptive in the past week. Following reverse scoring of positively worded items; items are summed, with scores ranging from 0 to 60. Higher scores reflect greater depressive symptoms. The CES-D has shown to be reliable and valid in samples of cancer patients (Hann, Winter, & Jacobson, 1999). For the present sample, internal consistency at baseline was .90.
Distress
The Profile of Mood States-short form (POMS-sf) measures six mood states (Tension-Anxiety, Depression-Dejection, Anger-Hostility, Vigor-Activity, Fatigue-Inertia, and Confusion-Bewilderment; Shacham, 1983; Curran, Andrykowski, & Studts, 1995). It has 37 items. Each is rated on a scale from 0 (not at all) to 4 (extremely) as being self-descriptive for the last 7 days. The Total Mood Disturbance (POMS-TMD) score is the sum of the Tension, Depression, Anger, Fatigue, and Confusion subscales minus the Vigor scale and can range from --22 to 300, with higher scores representing greater mood disturbance. The measure has been widely used in the cancer literature with good reliability and validity (Baker, Denniston, Zabora, Polland, & Dudley, 2002). Internal consistency at baseline was .93.
Treatment Process
Positive affect and negative affect
The short form of the Positive Affect Negative Affect Scale (PANAS-sf; Watson, Clark, & Tellegen, 1988) was used. Individuals report how often they have felt each of the 5 positive (e.g., determined) and 5 negative (e.g., upset) feelings during the previous week, including today, on a scale from 1 (not at all) to 5 (extremely). Items are summed to create positive and negative affect scales with total scores ranging from 5-25. Higher scores reflect greater positive or negative affect. In a population-based study, the PANAS-sf had adequate reliability and validity and was unaffected by age (Mackinnon, et al., 1999). Internal consistency at baseline was .84 for the positive scale and .77 for the negative scale.
Health-related quality-of-life
The Medical Outcomes Study-Short Form 12 (MOS SF-12; Ware & Sherbourne, 1992; Ware, Kosinski, & Keller, 1996; Ware, Kosinski, Turner-Bowker, & Gandek, 2002) assesses health-related quality-of-life. It includes eight subscales: physical functioning, role functioning-physical, bodily pain, general health perceptions, vitality, social functioning, role functioning-emotional, and mental health. The eight subscales are used to calculate the Physical Component Summary (PCS) and the Mental Component Summary (MCS) scores. Higher scores reflect better quality-of-life. The component score is converted to a t score, with a mean of 50 and standard deviation of 10. Extensive reliability and validity data are provided in the MOS manuals. Internal consistency at baseline was .88 for the PCS and .81 for the MCS.
Treatment Mechanisms
Mindfulness
The 39-item Five Facets of Mindfulness Questionnaire (FFMQ; Baer et al., 2006) assesses facets of mindfulness: observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience. Respondents rate how true or descriptive a facet is (e.g., “I watch my feelings without getting lost in them”) on a 1 (never or very rarely true) to 5 (very often or always true) scale. Items are summed for a total score, ranging from 39-195 and facet subscales can also be calculated. The FFMQ has acceptable reliability and validity in samples of both meditators and non-meditators (Christopher, Neuser, Michael, & Baitmangalkar, 2012). Internal consistency values at baseline were .89 for the total scale and ranged from .71 to .92 for the five subscales.
Hope
The 6-item State Hope Scale (SHS; Snyder, Sympson, Ybasco, Borders, Babyak, & Higgins, 1996) measures agency (belief in one's ability to reach goals) and pathways (belief in one's ability to find routes to reach goals). Individuals rate how true or false each statement (e.g., “I can think of many ways to reach my current goals.”) is for them right now on a scale of 1 (Definitely false) to 8 (Definitely true). Total scores range from 6-48 and subscale scores range from 3-24. Internal consistency values at baseline were .84 and .91 for the pathways and agency subscales, respectively and .93 for the total score, which are similar to previous studies with adult (Cheavens, et al., 2006; Snyder, et al., 1996) and cancer (Berendes, et al., 2010) samples.
Use of mindfulness and hope strategies
Starting with the two-month assessment, participants reported the frequency with which treatments strategies were used outside of therapy sessions in the past month. Specifically, one item each was used for the month's usage of mindfulness (e.g., How often have you used the formal mindfulness practice?) and hope (“How often have you used the strategies for making and following goals?”). A scale ranging from 0 (not at all) to 8 (two or more times a day/all the time) was used.
Analytic Strategy
Descriptive analyses (means and standard deviations) were used to examine feasibility and acceptability data.
Intent to treat analyses were conducted (N=32). Using all available data, mixed effects modeling (Raudenbush & Bryk, 2002) tested for change in treatment outcomes (distress, anxiety and depressive symptoms) from the initial assessment to 2-, 4-, and 7-month assessments. Unconditional growth models determined fixed and random effects for each variable of interest. Time was coded as the number of months between each assessment. The linear model was retained unless the quadratic model suggested improved fit based on examination of the difference in Bayesian Information Criterion (BIC) between the two models, as recommended by Rafferty (1995). That is, if the difference in BIC was >2 with the quadratic model exhibiting a smaller BIC, the quadratic model was retained; if the difference in BIC was <2, the linear model was retained.
Control variables and their interactions with time were entered and deleted as appropriate using a backwards elimination procedure in which non-significant terms (p>.10) were eliminated from each model. This specific procedure was used as this was an initial study and we had no theoretical reason to do otherwise. The variables considered were those for treatment format (group vs. individual treatment) and disease characteristics (site: breast vs. gynecologic; extent of current metastases: none or loco/regional vs. distant). We note, however, that control variables were not retained in the final models presented below.
In addition to the mixed effects models, effect sizes were reported along with analyses of reliable change (Jacobson, et al., 1999). Analyses of reliable change describe how much change occurred for an individual over the course of treatment and whether that change exceeds the margin of measurement error.
It was also hypothesized that the treatment would be associated with a steady upward trajectory for patients' ratings of positive affect and emotional quality-of-life and a steady downward trajectory for negative affect. To examine these hypotheses, mixed effects modeling was used to detail the trajectory of change in the session-by-session process measures using the same analytic plan as the outcome analyses (see above). Time was coded as the number of weeks between each session.
Lastly, we hypothesized that hope and/or mindfulness would be treatment mechanism(s) for any pre/post outcome change. Analyses examined mindfulness and hope using mixed effects modeling (as described above). Time was coded as the number of months between each assessment. First, pre- to post-treatment change in mindfulness and hope measure scores was determined. Second, analyses tested a) the relationship between pre/post hope and mindfulness change with the pre/post treatment outcomes; and, b) the relationship between hope and mindfulness strategy usage and change in treatment outcomes. To test the effects of mechanisms on outcomes, treatment mechanism x time effects were included in the respective models.
Results
Feasibility and Acceptability
Overall, 32 women initiated treatment (see Figure 1). The 20-session attendance rate was 79%. The mean number of sessions attended for the intensive phase was 13.1 of 16 (82%; range 2-16; SD = 4.35) and 2.75 of 4 (69%; range 0-4; SD = 1.63) for maintenance. Comparisons of women completing less than 50% of sessions were made with women who completed at least 50% of sessions. Those who attended fewer sessions (n = 5) did not differ significantly from those who attended more sessions (n = 27) on sociodemographic variables, disease free interval, current health (fatigue, pain interference, performance status), or initial values on treatment outcomes (all ps>.06). The rate of attrition (dropout) was 19%.
The patients viewed the treatment as acceptable, ethical, effective, and supportive. For all items, the general trend was a slight increase (i.e., more positive) across time, but ratings were always in the high to very high range. The grand means across time for each item using a 1-7 point scale are as follows: acceptability, 6.23 (SD= .87), ethical nature of the treatment, 6.71 (SD=. 49), effectiveness of treatment, 6.2 (SD=. 73), and likelihood of negative side effects (reversed), 1.82 (SD=1.11). Using a 0-10 point scale for cohesion, the grand means were 7.70 (SD=1.55) for involvement in the therapy experience and 8.90 (SD=1.19) for felt support.
Treatment Outcomes
Table 2 provides scores for all measures at the initial assessment. Significant linear intervention effects (improvements) over time were observed on all outcome measures (ps ≤ .01), excepting that for depressive symptoms (CES-D; p =.19). See Table 3. Regarding symptoms of anxiety, a significant fixed effect for linear slope (ps ≤ .01) indicated a reduction in anxiety symptoms for both the GADQ-IV and the PSWQ-A (e.g., see Figure 2a). In both cases, the change from baseline was a symptom decline that extended through to 7 months. There was also a significant fixed effect for linear change in the POMS-TMD (p < .01), indicating a decline in negative mood that was maintained through months 4 and 7 (see Figure 2b).
Table 2. Initial And Post-Treatment Values For Treatment Outcome, Process, and Mechanism Measures for the Sample.
| Variable | Pre-Treatment Mean (SD)/Percent (N=32) |
Post-Treatment Mean (SD)/Percent (N=24) |
Effect size (d) |
|---|---|---|---|
| Treatment Outcomes | |||
| Distress | |||
| POMS TMD | 21.72 (25.34) | 10.46 (14.41) | 0.55 |
| Anxiety-related Symptoms | |||
| GADQ-IV continuous | 8.72 (8.63) | 4.13 (4.84) | 0.64 |
| GADQ-IV % Probable GAD | 12.5% | 0% | |
| PSWQA | 18.13 (9.23) | 15.29 (5.65) | 0.37 |
| Depressive Symptoms | |||
| CES-D | 14.03 (9.25) | 12.59 (6.11) | 0.18 |
| % Moderate to Severe Symp. | 38% | 29% | |
| Treatment Process | |||
| Positive Affect | 16.79 (3.53) | 17.95 (3.26) | 0.35 |
| Negative Affect | 8.21 (3.31) | 6.50 (2.06) | 0.61 |
| Quality-of-life | |||
| MCS | 49.18 (9.12) | 55.38 (6.53) | 0.77 |
| PCS | 40.94 (12.04) | 41.82 (11.52) | 0.08 |
| Treatment Mechanisms | |||
| Mindfulness | |||
| FFMQ-Total | 136.37 (17.18) | 143.92 (17.78) | 0.44 |
| FFMQ-nonreactivity | 22.21 (4.80) | 24.67 (4.31) | 0.54 |
| FFMQ-observing | 28.13 (4.74) | 30.25 (4.01) | 0.49 |
| FFMQ-acting with awareness | 27.81 (5.92) | 28.46 (4.22) | 0.13 |
| FFMQ-describing | 28.09 (5.95) | 29.42 (5.84) | 0.23 |
| FFMQ-nonjudging | 30.13 (6.34) | 31.13 (6.37) | 0.16 |
| Hope | |||
| SHS-total | 33.16 (9.98) | 36.83 (6.10) | 0.44 |
| SHS- pathways | 17.03 (4.82) | 19.29 (2.74) | 0.57 |
| SHS-agency | 16.13 (5.51) | 17.54 (3.92) | 0.29 |
Table 3.
Fixed Effects From Unconditional Growth Models for Treatment Outcomes, Process Variables, and Mechanisms and Use of Treatment Strategies.
| Variable | Estimate | 95% CI | T-statistic | P-value | |
|---|---|---|---|---|---|
| Treatment Outcomes | |||||
|
| |||||
| GADQ-IV | Intercept | 8.260 | 6.023, 10.498 | 7.402 | <.001 |
| Linear | -.628 | -1.022, -.233 | -3.211 | .003 | |
| PSWQ-A | Intercept | 17.403 | 14.644, 20.162 | 12.828 | <.001 |
| Linear | -.279 | -.485, -.072 | -2.733 | .010 | |
| CES-D | Intercept | 13.493 | 10.639, 16.347 | 9.582 | <.001 |
| Linear | -.196 | -.498, .105 | -1.333 | .193 | |
| POMS-TMD | Intercept | 19.145 | 12.287, 26.003 | 5.639 | <.001 |
| Linear | -1.378 | -2.317, -.439 | -2.964 | .005 | |
|
| |||||
| Treatment Process | |||||
|
| |||||
| Positive Affect | Intercept | 16.03 | 15.001, 17.059 | 31.492 | <.001 |
| Linear | .047 | .007, .088 | 2.314 | .022 | |
| Negative Affect | Intercept | 8.243 | 7.368, 9.117 | 19.186 | <.001 |
| Linear | -.056 | -.086, -.026 | -3.682 | <.001 | |
| SF-12 MCS | Intercept | 49.437 | 46.961, 51.913 | 40.501 | <.001 |
| Linear | .196 | .096, .295 | 3.888 | <.001 | |
| SF-12 PCS | Intercept | 41.702 | 38.187, 45.217 | 24.047 | <.001 |
| Linear | .009 | -.092, .110 | .175 | .861 | |
|
| |||||
| Treatment Mechanisms | |||||
|
| |||||
| Hope (SHS total) | Intercept | 33.764 | 30.914, 36.615 | 24.023 | <.001 |
| Linear | .335 | .048, .623 | 2.388 | .024 | |
| Mindfulness (FFMQ) | Intercept | 137.357 | 131.702, 143.013 | 49.062 | <.001 |
| Linear | .992 | .353, 1.630 | 3.160 | .003 | |
|
| |||||
| Usage of Mindfulness and Hope Strategies | |||||
|
| |||||
| Formal Mindfulness | Intercept | 4.604 | 3.567, 5.642 | 8.937 | <.001 |
| Linear | -.169 | -.342, .005 | -2.012 | .056 | |
| Informal Mindfulness | Intercept | 5.209 | 4.360, 6.057 | 12.348 | <.001 |
| Linear | .015 | -.089, .119 | .298 | .768 | |
| Goal strategies | Intercept | 4.077 | 3.066, 5.089 | 8.092 | <.001 |
| Linear | -.080 | -.225, .065 | -1.124 | .270 | |
All Effects Show Linear Change (N=32).
Figure 2.
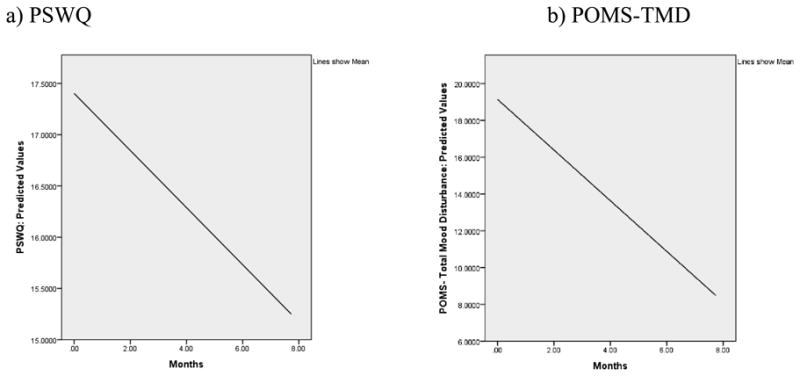
Graphs showing significant linear effects (ps≤.01) for anxiety symptoms (PSWQ-A; Fig. 2a) and emotional distress (POMS; Fig.2b) from pre to post treatment. In both cases, the change was a symptom decline from baseline that was maintained through months 4 and 7.
We also determined whether reliable change had been achieved for each patient. In addition to the index of Jacobson and colleagues (1999), there are other indices from which to choose (e.g., Jacobson & Traux, 1991) and different confidence intervals (CIs) can be chosen for the test. Here, both the 95 and 90% CIs are provided. Using a 95% CI and considering patients who completed both the baseline and 7-month assessments (n=24), reliable change was experienced for 25% of participants for the PSWQ (6/24), 17% for the GADQ (4/24), 17% for the CES-D (4/24), and 25% for the POMS-TMD (6/24). Using a 90% CI, reliable change was experienced for 42% for the PSWQ (10/24), 25% for the GADQ (6/24), 29% for the CES-D (7/24), and 42% for the POMS-TMD (10/24).
Treatment Process
Using session-by-session data, the linear change models exhibited better fit than the quadratic. See Table 3. There was a significant fixed effect for changes over time in positive (p < .05) and negative affect (p < .001) on the PANAS-sf (see Figures 3a and 3b) and the SF-12 mental health component summary (p < .001), though not the physical health component summary (p = .86). These results show that increases (i.e., improvements) were seen in positive affect and mental health-related quality-of-life from baseline that were maintained through months 4 and 7, while negative affect decreased over the same period, as predicted.
Figure 3.
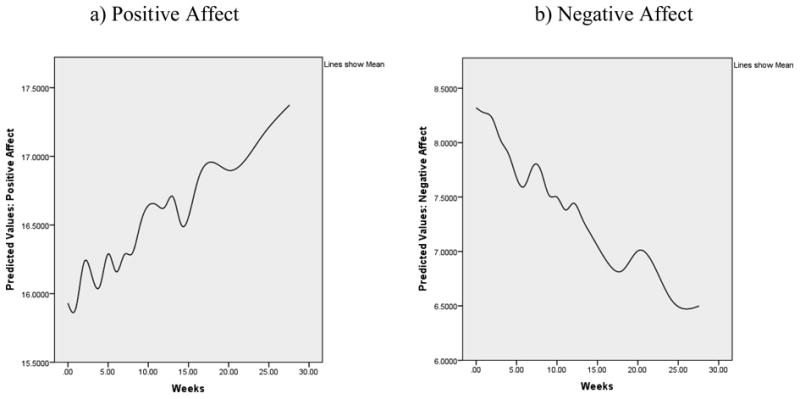
Graphs showing significant linear effects for session-by-session change, with a significant increase in positive affect (p = .02; Fig. 3a) and a significant decline in negative affect (p<.001; Fig 3b).
Treatment Mechanisms
Mindfulness and Hope scores
As predicted, analyses showed significant fixed effects for linear slope (ps < .03), indicating significant increases in both mindfulness (FFMQ Total) and hope (SHS Total) from baseline to 7 months. See Table 3. Considering these effects, exploratory analyses were conducted to learn more about the specific changes within each measure by testing for change on the subscales of each. For the FFMQ, the analyses for the Non-reacting, Observing, and Describing facets showed significant linear gains by 4 months, which were maintained through 7 months (all ps < .02). The Acting with Awareness and Non-judgment facets of the FFMQ did not significantly change (ps > .2). Analyses for the SHS showed that, for the Pathways subscale, significant fixed effects for both linear (p < .001) and quadratic (p< .01) changes indicated improvements over the first 4 months and gains maintained through the next 3 months. The SHS-Agency scores did not significantly change (p = .17).
The primary analyses tested if scores on the measures of mindfulness or hope covaried with treatment outcome change. Mindfulness (FFMQ total) was negatively related to all outcome variables at pretreatment (i.e., significant intercept effects, ps<. 05). More important, there was a significant interaction of FFMQ total with linear change over time for all outcomes: GADQ-IV (β = .03, p = .02), PSWQA (β =.01, p =.05), CES-D (β =.02, p = .05), and POMS-TMD (β=.06, p = .02). Women with higher mindfulness scores had consistently lower levels of symptoms of generalized anxiety disorder, worry, depressive symptoms, and total mood disturbance over the course of treatment with less change over time. Women with lower mindfulness scores experienced a greater decrease in depressive symptoms, worry, and total mood disturbance over the study than did those reporting initially higher levels of mindfulness.
Similar analyses using patients' reports of hope (SHS total) were conducted. The SHS total score also was negatively related to all outcome measures of distress (all ps < .05 for intercept effects). However, the SHS total score was not related to linear slope (change over time) of the outcomes.
Mindfulness and Hope strategy usage
Next, we tested whether patients' reports of usage of assigned mindfulness and hope-related strategies covaried with changes in treatment outcomes. For these analyses, the first time point (intercept) was two months as that was the first assessment of strategy usage. Descriptively, at two months patients reported, on average, engaging in formal mindfulness practices and using strategies for making and following goals 2-3 times per week over the course of the previous month; on average, patients reported engaging in informal mindfulness practices 4 times per week. Individuals engaging in formal mindfulness practices more often had lower levels of worry (PSWQA; β = -.94, p = .02) at two months. Further, use of mindfulness practices significantly interacted with linear time to influence worry (PSWQA; β = .22, p = .02). That is, individuals using the mindfulness practice more often in the previous month had consistently lower levels of worry over the course of treatment. Finally, use of strategies for making and following goals was not related to linear change in treatment outcomes.
Discussion
An uncontrolled, repeated measures design was used to test a novel combination of treatment components that were used as originally designed (Mindfulness, Hope) or tailored to address the specific concerns of women with cancer recurrence (Biobehavioral Intervention). Multiple measures at multiple time points were used for mixed effects modeling with the intent-to-treat sample. Firstly, negative mood and symptoms of anxiety showed significant improvement. Unlike the significance tests, effect sizes are independent of sample size, and they ranged from .37 (low medium) to .64 (medium-large), with the largest effect sizes found for the declines in anxiety (.64) and negative mood (.55) (see Table 2). According to some, effect sizes can be viewed as indicative of clinically meaningful change (Evans, Margison, & Barkham, 1998). Secondly, roughly one third of the patients achieved reliable change. This estimate of change is regarded as satisfactory considering the intent of the trial was to demonstrate if the treatment had any effect. Thirdly, the process data revealed the trajectory of change. As the treatment unfolded (from mindfulness, through hope with specific goal setting) negative affect was decreasing and positive affect and mental health quality-of-life increasing. Albeit not definitive, this methodology and resultant analyses provide convergent, positive evidence for the promise of the treatment.
Feasibility and acceptability data were obtained and in both cases the data were positive. Session attendance rate was 79% and treatment drop-out was low, 19%, similar to that of other trials (e.g., Akechi et al., 2007; Andersen et al., 2004; de Moor et al., 2002; Gotay et al., 2007). Even with difficult physical symptoms and the majority (69%) receiving chemotherapy, patients made attendance and staying with treatment a priority. So too the treatment was acceptable, with ratings being high to very high across all time points. Similarly, the patients reported high felt support throughout the intervention, with ratings ranging from 8.5 to 9 points on a 10-point scale.
Evidence was provided for the specific utility of both mindfulness and hope elements of the treatment. In terms of mindfulness, the subscales of Observe, Describe, and Non-reactivity significantly increased over the course of treatment. This may be related to the particular focus on these three skills in the formal mindfulness exercises that were conducted at the beginning of each session. Regarding hope, the pathways subscale (but not the agency subscale) of the SHS increased significantly from baseline to 7 months. Taken together, there is evidence that the intervention increased both mindfulness and hopeful thought. We were most interested, however, in the relationship between these hypothesized mechanisms and outcomes. Two analytic methods were used.
The first tested the relationship between scores on the mindfulness and hope measures with the outcome change. Mindfulness scores at baseline predicted rates of change in symptoms of depression, anxiety, worry, and total distress. There were greater decreases in these symptoms at lower levels of pre-treatment mindfulness and the changes for those starting at higher levels of mindfulness were more modest. If replicated, this finding would suggest that the intervention might be particularly useful for those with low mindfulness at baseline. Regarding hope, pre-treatment levels did not predict the rate of change in the outcome variables. This suggests that the treatment was equally efficacious across all levels of hope.
The second method tested the relationship of change in patients' usage of mindfulness and hope strategies across sessions and change in outcomes. Use of mindfulness skills was, according to some measures, related to decreased anxiety-related worry. It is possible that targeting the use of both formal and informal mindfulness skills (and, in turn, potentially increasing a stance of acceptance) may help to cope with worry and anxiety, much like it has for patients with anxiety disorders (Evans et al., 2008). The use of hope strategies outside of session was not related to change in outcome. There are two potential explanations for this. First, mindfulness practices were conducted in every session and were assigned as homework every week, with the focus on goal-setting and other hope skills being more circumscribed. As such, less time focusing on in vivo use of hope strategies may have prevented the translation of in-session practice to use in patients' everyday lives (e.g., 2 to 3 times per week may not be adequate to optimally utilize hope skills). Second, this sample had relatively high hope scores at baseline (M = 33 of 46); it is possible that patients were less likely to practice skills with which they were already facile. It is of note that the pre-treatment hope score of this sample is equivalent to the post-treatment hope scores found in the initial Hope Therapy paper (Cheavens, et al., 2006).
Significant changes in symptoms of depression or in reports of physical health quality-of-life were not found. Overall, there was less than a two-point decrease in mean CES-D scores. Regarding the percent of patients having at least a moderate level of symptoms on the CES-D, it was 39 percent at pretreatment and declined to 28 percent at post treatment. Upon accrual, the mental health characteristics of this sample were similar (Andersen, et al., 2005; Yang, Brothers, et al., 2008) or slightly more distressed (e.g., Devine, Parker, Fouladi, & Cohen, 2003; Palesh et al., 2007) than seen in other studies of patients with recurrence. Generally, changes in anxiety-related symptoms are easier to detect (or of greater magnitude) than changes in depressive symptoms in psychological interventions for cancer patients (e.g., Meyer & Mark, 1995). Regardless, in subsequent tests of the intervention, we would want to produce reductions in depressive symptoms for patients entering treatment with moderate to severe symptoms. Regarding physical health quality-of-life, the finding of stable levels over the course of a psychosocial intervention is consistent with longitudinal studies of patients coping with recurrence (e.g., Brothers, et al., 2011; Hersch, Juraskova, Price, & Mullan, 2009). That there was stability in this domain, however, lends support to the contention that changes in indices of psychological health were not dependent on improvements in physical states.
In considering the context of the study, with a phase II pre-experimental design cause (treatment) and effect (outcome) statements cannot be made. The significant pre/post changes on the outcomes for the group data are supplemented with the reliable change data for individuals. Relatedly, the session-by-session process data document the trajectory of change in both positive and negative affect between the pre, mid-, and post assessments. A strength of the intervention is its tailoring to the circumstances of recurrence, but as currently designed, it requires therapist expertise in three stress reduction modalities, although any one component can be trained within a reasonable time frame. For reasons of generalizability and cost, we chose therapists with less clinical experience (i.e., pre and post doctoral trainees), and all were not equally versed in all treatment models. The net effect of this was likely a limiting of treatment dose and, in turn, a lowering of effectiveness. A more powerful delivery of the intervention would necessitate experienced therapists having equivalent multi-model expertise. So to, the sample size may have resulted in inadequate power for some of the outcomes. Finally, our sample was homogeneous, including only breast and gynecologic patients and the majority being Caucasian. We designed the treatment to be gender and disease site neutral and anticipate that it would be similarly effective, but currently its generalizability to other racial/ethnic groups and cancer sites is unknown.
In conclusion, the findings are encouraging and suggest that there are feasible ways to study and help a cancer population that has received limited attention. Though there is some overlap with the difficulties experienced by all cancer patients, patients with recurrence have unique problems and illness trajectories. For many today, recurrence diagnosis does not signal imminent death but the beginning of coping with a chronic illness—one characterized by diminished but relatively stable health and, for many, continuous cancer therapy. This study provides suggestive evidence for a tailored treatment capable of reducing worries and anxiety and improving quality-of-life for women with these diagnoses. With the paucity of interventions specific to the experience of recurrent cancer, the present feasibility study provides support for a randomized study incorporating mindfulness, hope, and biobehavioral strategies.
Supplementary Material
Acknowledgments
We thank the patients for their kind participation and therapist, Eleshia Morrison, Ph.D. This research was supported by grants from the National Institutes of Health/National Cancer Institute (R21 CA135005 and K05 CA098133).
Footnotes
All authors declare that there are no conflicts of interest.
The manuscript contains original unpublished work. It has not appeared or been described in any context; it is not being submitted for publication elsewhere.
References
- Akechi T, Taniguchi K, Suzuki S, Okamura M, Minami H, Okuyama T, Uchitomi Y. Multifaceted psychosocial intervention program for breast cancer patients after first recurrence: Feasibility study. Psycho-Oncology. 2007;16(6):517–524. doi: 10.1002/pon.1101. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th. Washington, DC: American Psychiatric Association; 2000. text revision ed. [Google Scholar]
- Andersen, Farrar WB, Golden-Kreutz DM, Glaser R, Emery CF, Crespin TR, Carson WE. Psychological, behavioral, and immune changes after a psychological intervention: A clinical trial. Journal of Clinical Oncology. 2004;22(17):3570–3580. doi: 10.1200/JCO.2004.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Farrar WB, Golden-Kreutz D, Kutz LA, MacCallum R, Courtney ME, Glaser R. Stress and immune responses after surgical treatment for regional breast cancer. Journal of the National Cancer Institute. 1998;90(1):30–36. doi: 10.1093/jnci/90.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Farrar WB, Golden-Kreutz DM, Emery CF, Glaser R, Crespin TR, Carson WE. Distress reduction from a psychological intervention contributes to improved health for cancer patients. Brain, Behavior, and Immunity. 2007;21(7):953–961. doi: 10.1016/j.bbi.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Golden-Kreutz DM, Emery CF, Thiel DL. Biobehavioral intervention for cancer stress: Conceptualization, components, and intervention strategies. Cognitive and Behavioral Practice. 2009:253–265. doi: 10.106/j.cbpra.2008.11.002. [DOI] [Google Scholar]
- Andersen BL, Shapiro CL, Farrar WB, Crespin TR, Wells-Di Gregorio SM. Psychological responses to cancer recurrence: A controlled prospective study. Cancer. 2005;104:1540–1547. doi: 10.1002/cncr.21309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Shelby RA, Golden-Kreutz DM. RCT of a psychological intervention for patients with cancer: I. Mechanisms of change. Journal of Consulting and Clinical Psychology. 2007;75(6):927–938. doi: 10.1037/0022-006X.75.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Thornton LM, Shapiro CL, Farrar WB, Mundy BL, Yang HC, Carson WE., 3rd Biobehavioral, immune, and health benefits following recurrence for psychological intervention participants. Clinical Cancer Research. 2010;16(12):3270–3278. doi: 10.1158/1078-0432.CCR-10-0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen SR, Wurtzen H, Steding-Jessen M, Christensen J, Andersen KK, Flyger H, Dalton SO. Effect of mindfulness-based stress reduction on sleep quality: Results of a randomized trial among Danish breast cancer patients. Acta Oncologica. 2013;52(2):336–344. doi: 10.3109/0284186X.2012.745948. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baker F, Denniston M, Zabora J, Polland A, Dudley WN. A POMS short form for cancer patients: Psychometric and structural evaluation. Psycho-Oncology. 2002;11(4):273–281. doi: 10.1002/pon.564. [DOI] [PubMed] [Google Scholar]
- Berendes D, Keefe FJ, Somers TJ, Kothadia SM, Porter LS, Cheavens JS. Hope in the context of lung cancer: Relationships of hope to symptoms and psychological distress. Journal of Pain and Symptom Management. 2010;40(2):174–182. doi: 10.1016/j.jpainsymman.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CJ, Snyder CR, Hamilton N. The effectiveness of a hope intervention in coping with cold pressor pain. Journal of Health Psychology. 2008;13(6):804–809. doi: 10.1177/1359105308093864. [DOI] [PubMed] [Google Scholar]
- Brothers BM, Andersen BL. Hopelessness as a predictor of depressive symptoms for cancer patients coping with recurrence. Psycho-Oncology. 2009;18:267–275. doi: 10.1002/pon.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brothers BM, Yang HC, Strunk DR, Andersen BL. Cancer patients with major depressive disorder: Testing a biobehavioral/cognitive behavior intervention. Journal of Consulting and Clinical Psychology. 2011;79(2):253–260. doi: 10.1037/a0022566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull AA, Meyerowitz BE, Hart S, Mosconi P, Apolone G, Liberati A. Quality of life in women with recurrent breast cancer. Breast Cancer Research and Treatment. 1999;54(1):47–57. doi: 10.1023/a:1006172024218. [DOI] [PubMed] [Google Scholar]
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, Tyrer P. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321(7262):694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson LE, Doll R, Stephen J, Faris P, Tamagawa R, Drysdale E, Speca M. Randomized controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer. Journal of Clinical Oncology. 2013;31(25):3119–3126. doi: 10.1200/JCO.2012.47.5210. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. International Journal of Behavioral Medicine. 2005;12(4):278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- Cheavens JS, Feldman DB, Gum A, Michael ST, Snyder CR. Hope therapy in a community sample: A pilot investigation. Social Indicators Research. 2006;77(1):61–78. doi: 10.1007/s11205-005-5553-0. [DOI] [Google Scholar]
- Christopher MS, Neuser NJ, Michael PG, Baitmangalkar A. Exploring the psychometric properties of the five facet mindfulness questionnaire. Mindfulness. 2012;3(2):124–131. doi: 10.1007/s12671-011-0086-x. [DOI] [Google Scholar]
- Comstock GW, Helsing KJ. Symptoms of depression in two communities. Psychological Medicine. 1976;6(4):551–563. doi: 10.1017/s0033291700018171. [DOI] [PubMed] [Google Scholar]
- Crittendon J, Hopko DR. Assessing worry in older and younger adults: Psychometric properties of an abbreviated Penn State Worry Questionnaire (PSWQ-A) Journal of Anxiety Disorders. 2006;20(8):1036–1054. doi: 10.1016/j.janxdis.2005.11.006. [DOI] [PubMed] [Google Scholar]
- Curran SL, Andrykowski KJ, Studts JL. Short form of the Profile of Mood States (POMS-SF): Psychometric information. Psychological Assessment. 1995;7(1):80–83. doi: 10.1037/1040-3590.7.1.80. [DOI] [Google Scholar]
- de Moor C, Sterner J, Hall M, Warneke C, Gilani Z, Amato R, Cohen L. A pilot study of the effects of expressive writing on psychological and behavioral adjustment in patients enrolled in a phase II trial of vaccine therapy for metastatic renal cell carcinoma. Health Psychology. 2002;21(6):615–619. doi: 10.1037/0278-6133.21.6.615. [DOI] [PubMed] [Google Scholar]
- Devine D, Parker PA, Fouladi RT, Cohen L. The association between social support, intrusive thoughts, avoidance, and adjustment following an experimental cancer treatment. Psycho-Oncology. 2003;12(5):453–462. doi: 10.1002/pon.656. [DOI] [PubMed] [Google Scholar]
- Devins GM, Orme CM, Costello CG. Measuring depressive symptoms in illness populations: Psychometric properties of the Center for Epidemiologic Studies Depression (CES-D) scale. Psychology and Health. 1988;2:139–156. doi: 10.1080/08870448808400349. [DOI] [Google Scholar]
- Edwards AG, Hulbert-Williams N, Neal RD. Psychological interventions for women with metastatic breast cancer. Cochrane Database of Systematic Reviews. 2008;(3):CD004253. doi: 10.1002/14651858.CD004253.pub3. [DOI] [PubMed] [Google Scholar]
- Evans C, Margison F, Barkham M. The contribution of reliable and clinically significant change methods to evidence-based mental health. Evidence Based Mental Health. 1998;1(3):70–72. doi: 10.1136/ebmh.1.3.70. [DOI] [Google Scholar]
- Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness-based cognitive therapy for generalized anxiety disorder. Journal of Anxiety Disorders. 2008;22(4):716–721. doi: 10.1016/j.anxdis.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Feldman DB, Snyder CR. Hope and meaningful life: Theoretical and empirical associations between goal-directed thinking and life meaning. Journal of Social and Clinical Psychology. 2005;24:401–421. doi: 10.1521/jscp.24.3.401.65616. [DOI] [Google Scholar]
- Galway K, Black A, Cantwell M, Cardwell CR, Mills M, Donnelly M. Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients. Cochrane Database of Systematic Reviews. 2012;11:CD007064. doi: 10.1002/14651858.CD007064.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland SN, Carlson LE, Stephens AJ, Antle MC, Samuels C, Campbell TS. Mindfulness-based stress reduction compared with cognitive behavioral therapy for the treatment of insomnia comorbid with cancer: A randomized, partially blinded, noninferiority trial. Journal of Clinical Oncology. 2014;32(5):449–457. doi: 10.1200/JCO.2012.47.7265. [DOI] [PubMed] [Google Scholar]
- Goodwin PJ, Leszcz M, Ennis M. The effect of group psychosocial support on survival in metastatic breast cancer. New England Journal of Medicine. 2001;345(24):1719–1726. doi: 10.1056/NEJMoa011871. [DOI] [PubMed] [Google Scholar]
- Gotay CC, Moinpour CM, Unger JM, Jiang CS, Coleman D, Martino S, Albain KS. Impact of a peer-delivered telephone intervention for women experiencing a breast cancer recurrence. Journal of Clinical Oncology. 2007;25(15):2093–2099. doi: 10.1200/JCO.2006.07.4674. [DOI] [PubMed] [Google Scholar]
- Gum A, Snyder CR. Coping with terminal illness: The role of hopeful thinking. Journal of Palliative Medicine. 2002;5(6):883–894. doi: 10.1089/10966210260499078. [DOI] [PubMed] [Google Scholar]
- Hann D, Winter K, Jacobson P. Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) Journal of Psychosomatic Research. 1999;46(5):437–443. doi: 10.106/S0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- Hersch J, Juraskova I, Price M, Mullan B. Psychosocial interventions and quality of life in gynaecological cancer patients: A systematic review. Psycho-Oncology. 2009;18(8):795–810. doi: 10.1002/pon.1443. [DOI] [PubMed] [Google Scholar]
- Hoffman CJ, Ersser SJ, Hopkinson JB, Nicholls PG, Harrington JE, Thomas PW. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: A randomized, controlled trial. Journal of Clinical Oncology. 2012;30(12):1335–1342. doi: 10.1200/JCO.2010.34.0331. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopko DR, Stanley MA, Reas DL, Wetherell JL, Beck JG, Novy DM, Averill PM. Assessing worry in older adults: Confirmatory factor analysis of the Penn State Worry Questionnaire and psychometric properties of an abbreviated model. Psychological Assessment. 2003;15(2):173. doi: 10.1037/1040-3590.15.2.173. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Roberts LJ, Berns SB, McGlinchey JB. Methods for defining and determining the clinical significance of treatment effects: Description, application, and alternatives. Journal of Consulting and Clinical Psychology. 1999;67(3):300–307. doi: 10.1037/0022-006X.67.3.300. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037/0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. illustrated. New York: Delta Trade Paperbacks; 1991. reprint. [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness meditation in everyday life. 1st. New York: Hyperion; 1994. [Google Scholar]
- Kenne Sarenmalm E, Öhlén J, Odén A, Gaston-Johansson F. Experience and predictors of symptoms, distress and health-related quality of life over time in postmenopausal women with recurrent breast cancer. Psycho-Oncology. 2008;17(5):497–505. doi: 10.1002/pon.1258. [DOI] [PubMed] [Google Scholar]
- Kissane DW, Grabsch B, Clarke DM, Smith GC, Love AW, Bloch S, Li Y. Supportive-expressive group therapy for women with metastatic breast cancer: Survival and psychosocial outcome from a randomized controlled trial. Psycho-Oncology. 2007;16(4):277. doi: 10.1002/pon.1185. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Johnson-Mallard V, Post-White J, Moscoso MS, Jacobsen PB, Klein TW, Kip KE. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology. 2009;18(12):1261–1272. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- Low CA, Stanton AL, Bower JE, Gyllenhammer L. A randomized controlled trial of emotionally expressive writing for women with metastatic breast cancer. Health Psychology. 2010;29(4):460–466. doi: 10.1037/a0020153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon A, Jorm AF, Christensen H, Korten AE, Jacomb PA, Rodgers B. A short form of the Positive and Negative Affect Schedule: Evaluation of factorial validity and invariance across demographic variables in a community sample. Personality and Individual Differences. 1999;27(3):405–416. doi: 10.1016/S0191-8869(98)00251-7. [DOI] [Google Scholar]
- Meyer T, Mark M. Effects of psychosocial interventions with adult cancer patients: A meta-analysis of randomized experiments. Health Psychology. 1995;14:101–108. doi: 10.1037/0278-6133.14.2.101. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD, et al. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Naaman SC, Radwan K, Fergusson D, Johnson S. Status of psychological trials in breast cancer patients: A report of three meta-analyses. Psychiatry. 2009;72(1):50–69. doi: 10.1521/psyc.2009.72.1.50. [DOI] [PubMed] [Google Scholar]
- Newman MG, Zuellig AR, Kachin KE, Constantino MJ, Przeworski A, Erickson T, Cashman-McGrath L. Preliminary reliability and validity of the Generalized Anxiety Disorder Questionnaire-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy. 2002;33(2):215–233. doi: 10.1016/S0005-7894(02)80026-0. [DOI] [Google Scholar]
- Palesh OG, Collie K, Batiuchok D, Tilston J, Koopman C, Perlis ML, Spiegel D. A longitudinal study of depression, pain, and stress as predictors of sleep disturbance among women with metastatic breast cancer. Biological Psychology. 2007;75(1):37–44. doi: 10.1016/j.biopsycho.2006.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piet J, Wurtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80(6):1007–1020. doi: 10.1037/a0028329. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Fröhlich C, Silbereisen RK. Testing models of change in life goals after a cancer diagnosis. Journal of Loss and Trauma. 2008;13(4):330–351. doi: 10.1080/15325020701742052. [DOI] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–164. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models. Newbury Park, CA: Sage; 2002. [Google Scholar]
- Rodebaugh TL, Holaway RM, Heimberg RG. The factor structure and dimensional scoring of the generalized anxiety disorder questionnaire for DSM-IV. Assessment. 2008;15(3):343–350. doi: 10.1177/1073191107312547. [DOI] [PubMed] [Google Scholar]
- Sarenmalm EK, Öhlén J, Odén A, Gaston-Johansson F. Experience and predictors of symptoms, distress and health-related quality of life over time in postmenopausal women with recurrent breast cancer. Psycho-Oncology. 2008;17(5):497–505. doi: 10.1002/pon.1258. [DOI] [PubMed] [Google Scholar]
- Schumacher A. Sinnfindung bei Brustkrebspatientinnen. Frankfurt: Lang; 1990. Meaning finding in breast cancer patients. [Google Scholar]
- Shacham S. A shortened version of the Profile of Mood States. Journal of Personality Assesment. 1983;47(3):305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- Sheard T, Maguire P. The effect of psychological interventions on anxiety and depression in cancer patients: Results of two meta-analyses. British Journal of Cancer. 1999;80(11):1770–1780. doi: 10.1038/sj.bjc.6690596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shennan C, Payne S, Fenlon D. What is the evidence for the use of mindfulness-based interventions in cancer care? A review. Psycho-Oncology. 2011;20(7):681–697. doi: 10.1002/pon.1819. [DOI] [PubMed] [Google Scholar]
- Snyder CR. The psychology of hope: You can get there from here. New York, NY: Free Press; 1994. [Google Scholar]
- Snyder CR, Irving L, Anderson JR. Hope and health: Measuring the will and the ways. In: Snyder C, Forsyth DR, editors. Handbook of social and clinical psychology: The health perspective. New York: Pergamon Press; 1991. pp. 285–305. [Google Scholar]
- Snyder CR, Rand KL, King EA, Feldman DB, Woodward JT. “False” hope. Journal of Clinical Psychology. 2002;58(9):1003–1022. doi: 10.1002/jclp.10096. [DOI] [PubMed] [Google Scholar]
- Snyder CR, Sympson SC, Ybasco FC, Borders TF, Babyak MA, Higgins RL. Development and validation of the State Hope Scale. Journal of Personality and Social Psychology. 1996;(70):321–335. doi: 10.1037/0022-3514.70.2.321. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2(8668):888–891. doi: 10.1016/S0140-6736(89)91551-1. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Butler LD, Giese-Davis J, Koopman C, Miller E, DiMiceli S, Kraemer HC. Effects of supportive-expressive group therapy on survival of patients with metastatic breast cancer: A randomized prospective trial. Cancer. 2007;110(5):1130–1138. doi: 10.1002/cncr.22890. [DOI] [PubMed] [Google Scholar]
- Stahl B, Goldstein E. A mindfulness-based stress reduction workbook. Oakland, CA: New Harbinger Publications; 2010. [Google Scholar]
- Stanton AL. Psychosocial concerns and interventions for cancer survivors. Journal of Clinical Oncology. 2006;24:5132–5137. doi: 10.1200/JCO.2006.06.8775. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Danoff-Burg S, Huggins ME. The first year after breast cancer diagnosis: Hope and coping strategies as predictors of adjustment. Psycho-Oncology. 2002;11(2):93–102. doi: 10.1002/pon.574. [DOI] [PubMed] [Google Scholar]
- Thornton LM, Levin AO, Dorfman CS, Godiwala N, Heitzmann C, Andersen BL. Emotions and social relationships for breast and gynecologic patients: A qualitative study of coping with recurrence. Psycho-oncology. 2014;23(4):382–389. doi: 10.1002/pon.3429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J, Jr, Kosinski M, Keller SD. A 12-Item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. SF-12v2: How to score version 2 of the SF-12 health survey. Lincoln, RI: QualityMetric Inc.; 2002. [Google Scholar]
- Ware JE, Sherbourne CD. The MOS-36 Short-Form Health Survey (SF-36) Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weisman AD, Worden JW. The emotional impact of recurrent cancer. Journal of Psychosocial Onocology. 1986;3(4):5–16. [Google Scholar]
- Wrobleski KK, Snyder CR. Hopeful thinking in older adults: Back to the future. Experimental Aging Research. 2005;31(2):217–233. doi: 10.1080/03610730590915452. [DOI] [PubMed] [Google Scholar]
- Yang HC, Brothers BM, Andersen BL. Stress and quality of life in breast cancer recurrence: Moderation or mediation of coping? Annals of Behavioral Medicine. 2008;35(2):188–197. doi: 10.1007/s12160-008-9016-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang HC, Thornton LM, Shapiro CL, Andersen BL. Surviving recurrence: Psychological and quality of life recovery. Cancer. 2008;112(5):1178–1187. doi: 10.1002/cncr.23272. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.