Abstract
Objectives
We set to measure the inter-atrial pressure gradient during simulated obstructive sleep apnea (OSA).
Background
OSA occurs when a sleeping patient attempts to inhale against an obstructed airway. How this event affects the inter-atrial pressure gradient has not been defined. We hypothesized that simulated OSA in a conscious subject (Mueller maneuver [MM], inspiration against obstruction) would promote increased right-to-left pressure gradient, and then the substrate for right-to-left atrial shunting.
Methods
Selected patients underwent simultaneous measurement of airway and atrial pressures (both left and right atrium [LA, RA]) using high-fidelity micromanometry at rest, during MM, and during VM, during right heart catheterization.
Results
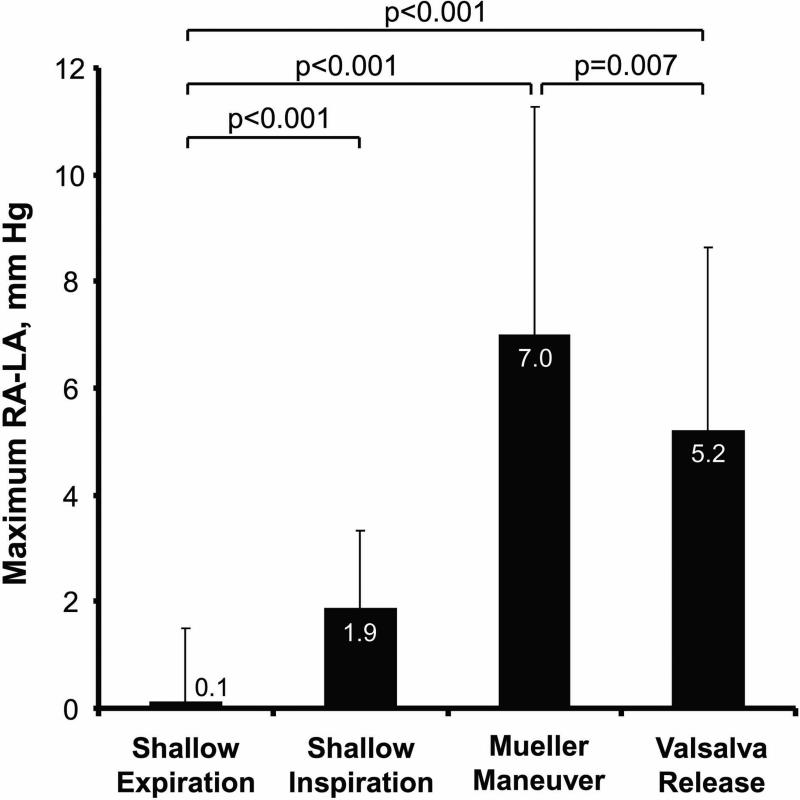
Ten patients (age 55±11 years, 2 women) were successfully studied. During the onset of MM, RA pressure transiently but consistently exceeded LA pressure in response to the steep decline in intra-thoracic pressure (maximum RA-LA pressure gradient increased from 0.1±1.4 mmHg at baseline to 7.0±4.3 mmHg during MM, p<0.001). The maximum right-to-left atrial pressure gradient during Mueller maneuver was higher than that achieved during the Valsalva maneuver release (p<0.007).
Conclusions
The onset of MM increased right-to-left pressure gradient across the atrial septum, likely as a result of greater blood return to the RA from extra-thoracic veins. The RA-LA pressure gradient achieved during MM was greater than that observed during VM. These findings delineate the hemodynamic substrate for right to left shunting during OSA.
Keywords: Foramen ovale, Sleep apnea, Mueller maneuver, Valsalva maneuver, Pressure, Gradient
Introduction
Valsalva maneuver (VM, expiration against obstruction) is commonly used as a provocative maneuver to augment right-to-left shunting through patent foramen ovale (PFO).(1) Obstructive sleep apnea (OSA) occurs when a sleeping patient attempts to inhale against an obstructed airway, and several reports suggest that OSA might also provoke right-to-left shunting. However, no previous studies explored the hemodynamic basis for this notion.(2-6) Our study was designed to document the changes in atrial hemodynamics during Mueller maneuver (MM, inspiration against obstruction) which was used to simulate OSA in an awake patient. We hypothesized that MM would lead to an increase in the right-to-left atrial (RA-LA) pressure gradient possibly comparable to the RA-LA gradient produced by VM.
Materials and Methods
A convenience sample of patients aged 18 years and above undergoing device PFO closure were prospectively studied between January 2010 and September 2011. Patients with significant myocardial, valvular, pericardial or pulmonary disease were excluded. This study was approved by the Institutional Review Board ofthe Mayo Clinic (Rochester, Minnesota), and a signed informed consent was obtained from all participants.
Study Protocol
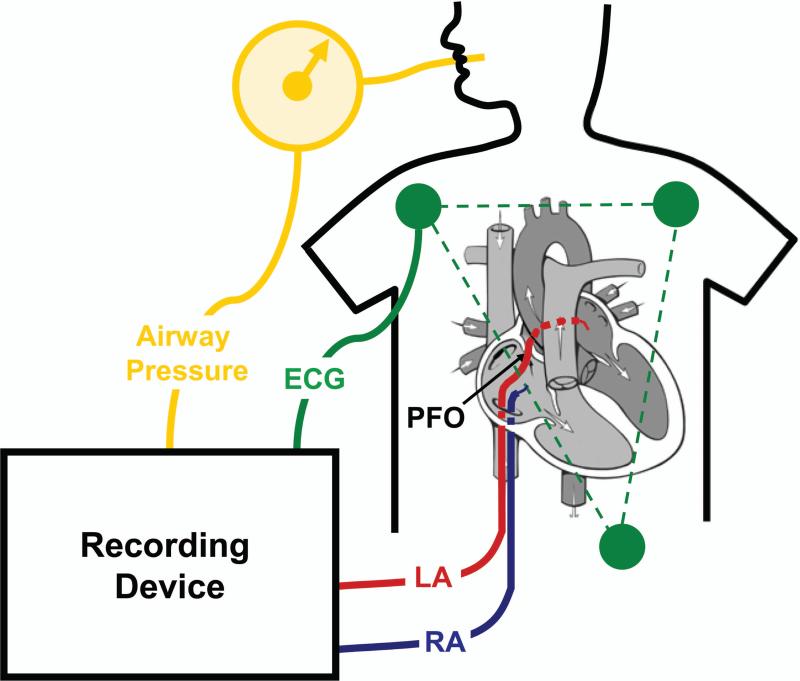
Patients were studied while taking chronic medications in the post-absorptive state and supine position during conscious sedation. Venous access was obtained in the right (9 French) and left femoral veins (9 French), and intra-cardiac echocardiography was performed to visualize the atrial septum. Pressure transducers were balanced to mid-axillary line measured manually in all patients. A 7 French fluid filled balloon wedge catheter (Arrow) was passed through the PFO into the left atrium (LA) under echocardiographic guidance. A separate fluid-filled catheter was then placed in the right atrium (RA). High fidelity micromanometer catheters (Millar Instruments) were then advanced through each fluid filled catheter into the RA and LA, respectively (Figure 1). Micromanometers were balanced against mean fluid-filled pressure in each chamber at this time and repeatedly throughout the procedure. Baseline measurements were acquired at rest at end-expiration as previously described.(7)
Figure 1.
Configuration of the recording equipment during the experiment. (PFO image source: Mayo Clinic, used with permission)
ECG = electrocardiogram; LA = left atrium; PFO = patent foramen ovale; RA = right atrium
Breathing Maneuvers
The MM and VM were rehearsed repeatedly with each patient prior to the catheterization procedure. During MM patients voluntarily inspired against a fixed resistance in an attempt to achieve negative intra-thoracic pressure; this maneuver has been previously described to simulate the airway obstruction that occurs in patients with OSA.(8-10) During VM patients voluntarily expired against fixed resistance in an attempt to achieve positive intra-thoracic pressure. A nose clip and a tight-fitting mouthpiece were placed, through which airway pressure was directly measured concurrently with LA and RA pressures. The airway pressure was projected directly and in real-time on the room monitor, allowing the patient to visualize it, and hence help maintain adequate maneuvers. The mouthpiece incorporated a small air leak through a 21-Gauge needle to help prevent complete closure of the glottis during the MM.(2)
The MM was considered satisfactory if it lasted at least 4 seconds, and the patient reached a negative airway pressure of at least -20 mmHg. The VM was considered satisfactory if the patient performed it for at least 4 seconds, and a positive airway pressure of at least +20 mmHg was reached. Patients were encouraged to maintain MM and VM for >5 seconds. A recovery period of at least 10 seconds separated each maneuver. The sequence of maneuvers was: resting baseline breathing followed by 7 MMs, then 2 VMs.
Interval Definitions
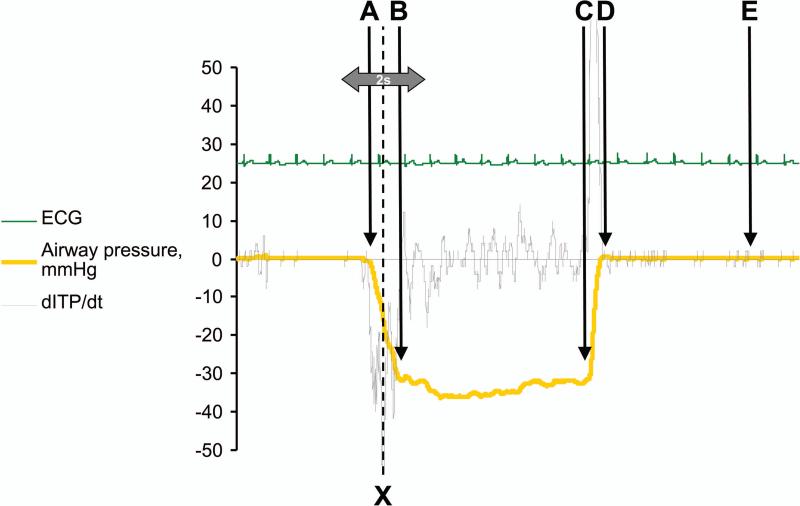
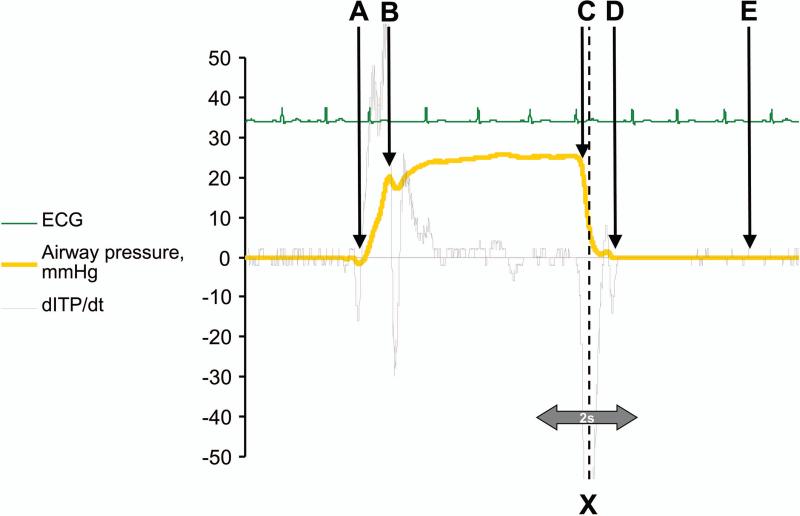
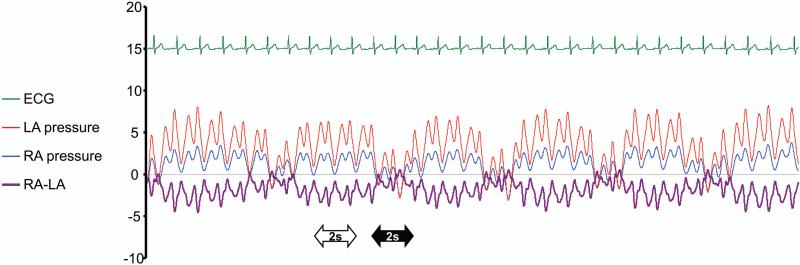
The phases of the MM were defined using the inflection points of the airway pressure curve and its first derivative with respect to time, as indicated in Figure 2. Intervals were defined for the VM as depicted in Figure 3. The latter differed from established phases in the VM.(11) For each maneuver, we defined an interval of interest (2 second duration) centered on the steepest decline in airway pressure (gray arrow around point “X”, Figures 2-3). This interval coincided with the onset of the MM and release of the VM, respectively. During baseline respiration we analyzed intervals at end-expiration (2 seconds in duration each, white arrow in Figure 4), and intervals during inspiration (2 seconds in duration each, black arrow in Figure 4).
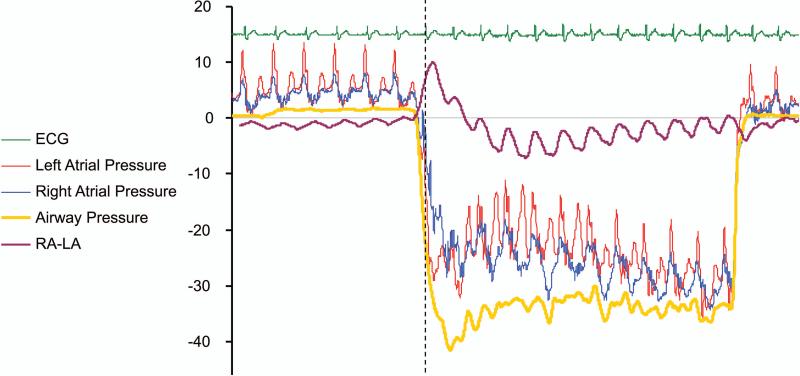
Figure 2. Intervals used in the evaluation of atrial pressures during the Mueller maneuver (MM).
Using the airway pressure (AP, yellow) and its first derivative (dAP/dt, grey) the following time points were identified as follows: “A” constitutes the beginning of the MM when patient is starting to inspire against an obstructed airway (AP decreases to at least to -5 mmHg, and dAPp/dt turns negative). “B” occurs when inspiratory efforts level off as the patient maintains stable negative intra-thoracic pressure (AP curve stops decreasing, and dAP/dt starts turning positive). “C” constitutes the end of breath as the patient expires with an open airway (AP curve increases by 5 mmHg or more from the maximum negative value; dAP/dt values are positive). “D” defines the end of the MM, when intra-thoracic pressure values return to baseline. “E” stands for the end of one breathing experiment, and was set at 3-5 seconds after point “D.” The interval of interest for the main analysis is depicted as a gray arrow.
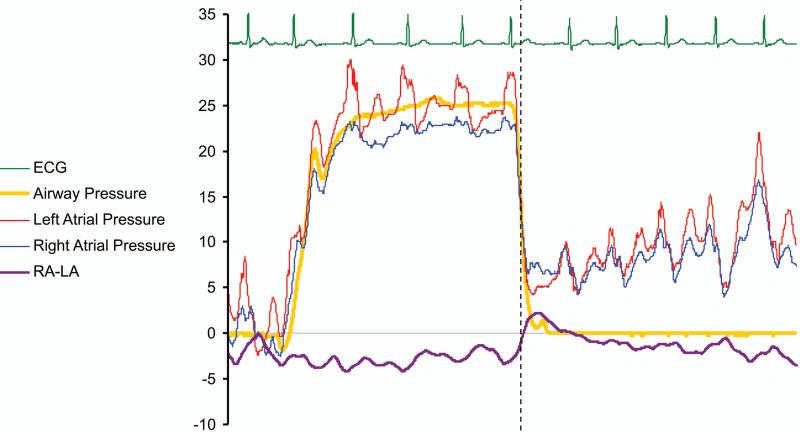
Figure 3. Intervals used in the evaluation of the Valsalva maneuver (VM).
Using the airway pressure (AP, yellow) and its first derivative (dAP/dt, grey) the following time points are defined during the VM: “A” corresponds to the onset of VM strain (AP increases to ≥5 mmHg, and dAP/dt becomes positive). “B” expiratory effort levels with stable positive intra-thoracic pressure (AP curve stops increasing, and dAP/dt ceases being positive). “C” corresponds to VM release (AP curve decreases by 5 mmHg or more from the maximum value; dAP/dt values are negative). “D” defines the end of VM: a moment, when intra-thoracic pressure values return to baseline. “E” stands for the end of one breathing experiment, and was set at 3-5 seconds after point “D.” The interval of interest for the main analysis is depicted as a gray arrow.
Figure 4. Atrial pressures during shallow respiration.
(Pressures on the Y-axis are recorded in mmHg) The right atrial (RA, blue) pressure rises above the left atrial (LA, red) pressure very transiently during the onset of inspiration (black arrow). This is indicated by the RA-LA (purple) tracing exceeding zero at these times. White arrow represents one of the 2 second end-expiratory intervals which were used to define baseline.
The instantaneous RA-LA pressure gradient curve was determined by subtracting the LA pressure from the RA pressure and plotting against time. Maximal RA-LA pressure gradient for each of the above defined intervals of interest was identified.
For the analysis of baseline respiration we utilized 3 intervals of shallow expiration and 3 intervals of shallow inspiration from each patient. The measurements were averaged for a given patient and maneuver (shallow expiration, shallow inspiration, MM, VM).
Statistical Analysis
Continuous variables are presented as mean ± standard deviation or numbers (percentages). Baseline and respiratory maneuver measurements were compared by paired t-test, and linear correlation was used to relate maximum RA-LA pressure gradient to the maximum change in airway pressure. P-values <0.05 were considered significant. All analyses were performed using JMP version 9.0.
Results
Patient Characteristics
Study subjects (N = 10) were individuals with previously documented PFO who had no evidence of organic heart disease otherwise (Table 1). Atrial shunting was detected by TEE in all patients prior to the catheterization procedure. A total of 21 patients were approached regarding the study participation, and from these 10 patients were able and willing to perform adequate breathing maneuvers for analysis, 3 patients could not undergo sufficient practice of the breathing maneuvers prior to the catheterization, 4 patients were not able to perform these maneuvers when lying down in the catheterization laboratory, tracings from 2 patients could not be analyzed due to recording errors, and 2 patients chose not to participate in this study.
Table I.
Clinical and Echocardiographic Characteristics of the Patients Included in This Study PFO = patent foramen ovale; TEE = trans-esophageal echocardiography
| Variable | Value (N = 10) |
|---|---|
| Age (years) | 55 ± 11 |
| Gender (women) | 2 (20%) |
| Height (cm) | 173 ± 9 |
| Weight (kg) | 85 ± 15 |
| Body mass index (kg/m2) | 29 ± 6 |
| History of stroke | 10 (100%) |
| History of hypertension | 2 (20%) |
| History of hyperlipidemia | 6 (60%) |
| Coronary artery disease | 0 (0%) |
| Active smoking | 1 (10%) |
| PFO detected via TEE | 10 (100%) |
| Right to left shunt detected at rest on TEE | 7 (70%) |
| Right to left shunt detected with Valsalva on TEE | 10 (100%) |
| Right to left shunt at rest on intracardiac echocardiography (by bubble study and by color Doppler) | 10 (100%) |
| Left ventricular ejection fraction on echocardiography (%) | 61 ± 4 |
Shallow Respiration
During shallow respiration RA pressure was predominantly less than LA pressure, as documented by persistently negative values of the RA-LA pressure gradient (purple tracing in Figure 4). A transient rise in RA pressure relative to LA pressure occurred during inspiration (black arrow in Figure 4), so that the maximum RA-LA pressure gradient observed during inspiration was higher than that observed during expiration (1.9±1.4 mmHg vs. 0.1±1.4 mmHg; p<0.001). Simultaneous color Doppler echocardiography revealed transient right to left shunting coincident with shallow inspiration in some patients.
Changes with Mueller Maneuver
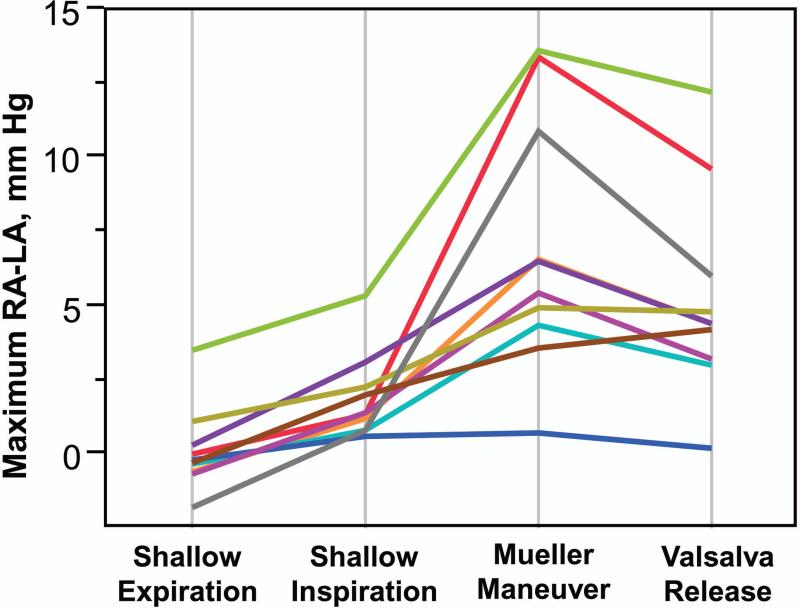
The mean duration of MM sustained by patients in this study was 6.7±1.7 seconds. Figure 5A depicts a recording during MM: Airway pressure initially drops to -42 mm Hg (yellow color), and then remains below -20mm Hg for 8 seconds. The RA-LA pressure gradient prior to MM was mildly negative (purple) as LA pressure (red) slightly exceeded RA (blue). Shortly after the airway pressure drops (drop in yellow tracing = onset of MM) there was a rise in the RA-LA pressure gradient, such that RA pressure transiently exceeded LA pressure. The RA-LA pressure gradient rose during MM in 9 of 10 patients, increasing from 0.1±1.4 mmHg at baseline to 7.0±4.3 mmHg during the initial phase of the MM (p<0.001, Figure 6). Table 2 depicts the mean of all the maximum RA-LA pressure gradients achieved by each patient. The intra-personal standard deviation of the maximum RA-LA pressure gradient was 2.0 mm Hg (intra-personal variance = 4.2 mm Hg), and the inter-personal standard deviation of the maximum RA-LA pressure gradient was 4.3 mm Hg (inter-personal variance = 18.5 mm Hg). The magnitude of the maximum airway pressure change during the Mueller maneuvers was only modestly correlated with the maximum RA-LA pressure gradient (R = 0.27; p = 0.02).
Figure 5.
Panel A: Sample recording from a patient performing a Mueller maneuver. (Pressures on the Y-axis are recorded in mmHg)
Panel B: Sample recording from a patient performing maneuver of a Valsalva maneuver. (Pressures on the Y-axis are recorded in mmHg)
RA = right atrial pressure; LA = left atrial pressure
Figure 6.
Panel A: The maximum right to left atrial (RA-LA) pressure gradient observed during baseline respiration, Mueller maneuver, and Valsalva release.
Panel B: Parallel plots of the matched pairs depicting the changes in the maximum RA-LA pressure gradient during baseline respiration, Mueller maneuver, and during Valsalva release. The measurements from each one patient were averaged for all of his/her attempts at a given maneuver, i.e. each line represents averages for one patient.
Table II.
Maximum right-to-left atrial pressure gradient during the four respiratory maneuvers as recorded in each patient.
| Patient (#) | Maximum RA-LA Pressure Gradient (mm Hg) | |||
|---|---|---|---|---|
| Shallow Expiration | Shallow Inspiration | Mueller Maneuver | Valsalva Release | |
| 1 | 0 | 1.2 | 13.4 | 9.6 |
| 2 | −0.6 | 0.6 | 6.6 | 4.4 |
| 3 | 3.6 | 5.4 | 13.6 | 12.2 |
| 4 | −0.6 | 0.6 | 4.3 | 3.0 |
| 5 | −0.4 | 0.2 | 0.7 | 0.2 |
| 6 | 0.4 | 3.4 | 6.5 | 4.4 |
| 7 | −0.8 | 1.4 | 5.4 | 3.2 |
| 8 | 1 | 2.2 | 4.9 | 4.8 |
| 9 | −1.8 | 0.6 | 10.9 | 6.0 |
| 10 | −0.2 | 3.4 | 3.6 | 4.2 |
| Mean ± SD | 0.1 ± 1.4 | 1.9 ± 1.7 | 7.0 ± 4.3 | 5.2 ± 3.4 |
SD = standard deviation
Changes with Valsalva Maneuver
The mean duration of sustained VM was 7.1±1.3 seconds. A typical VM is shown in Figure 5B. The maximum RA-LA pressure gradient during VM release was significantly higher compared to baseline (5.2±3.4 mmHg vs. 0.1±1.4 mmHg; p<0.001; Figure 6). The RA-LA maximum pressure gradient was greater during MM onset compared to VM release (7.0±4.3 mmHg during MM vs. 5.2±3.4 mmHg during VM, p=0.007; Figure 6). The magnitude of the maximum airway pressure change during the Valsalva maneuvers was moderately correlated with the maximum RA-LA pressure gradient (R = 0.53; p = 0.03).
Intra-Cardiac Echocardiography
Intra-cardiac echocardiography was utilized for the visualization of the atrial septum and for the positioning of the LA catheters. The imaging probe was then withdrawn to allow for simultaneous access for the placement of the RA catheters, and therefore, we did not image the PFO during MM or VM. However, during one of the procedures the patient fell asleep and started snoring while the intra-cardiac imaging was present and the PFO visualized (each snort represents a partial airway obstruction). On the echo-Doppler imaging we noted a transient right to left shunt which temporally coincided with the onset of each snort (attached Video file includes both the audio and video tracings).
Discussion
In this study we document the consequences of sudden intra-thoracic pressure changes occurring with MM and VM on the right-to-left atrial pressure gradient. The MM can produce significant increase in RA pressure relative to LA pressure, though the window during which RA exceeds LA is short and limited to the initial onset of negative intra-thoracic pressure. Increased RA-LA pressure gradient was also noted with the Valsalva release, a well-established maneuver for provoking right-to-left shunts. In our patients, the maximum RA-LA pressure gradient measured during MM were greater than that observed during VM. The Mueller maneuver, therefore, produces the substrate for right-to-left shunting, and to an extent similar to the Valsalva maneuver.
Mechanism of Pressure Changes
The MM increases right-sided venous return by enhancing the pressure gradient from extra-thoracic to intra-thoracic veins during inspiration. Negative intra-thoracic pressure is created as the diaphragm descends while abdominal pressure may increase slightly, favoring increased venous return to the right heart. Because the left atrium and pulmonary veins both reside within the thorax, there is no enhancement of pulmonary venous return to the left heart during inspiration. This explains the increase in right-to-left pressure gradient that transiently occurs with inspiration. Further, when inspiration is more forced, the pressure gradient favoring right heart filling is greatly enhanced, favoring more robust right-to-left pressure gradient.
These phenomena may have been previously under-appreciated because of their very transient nature. This is particularly true with regards to the sudden intra-thoracic pressure drop at initiation of the MM which could not be reliably imaged via intra-cardiac or trans-thoracic echocardiography. Indeed, even prior invasive studies focused on the steady state interval that follows the transient drop in airway pressure (interval “BC” in Figure 2 of the current study).(12) Our data show that during this interval yet another steady state is achieved wherein the RA to LA gradient remains negative (i.e. LA exceeds RA). To test our hypothesis regarding pressure gradients during the MM it was necessary to precisely measure both LA and RA pressures during the complete maneuver, and particularly during the sudden drop in airway pressure at the onset of the MM. Our findings are consistent with previous studies showing that MM leads to transient decrease in LA volume,(2) and we also confirm that the MM leads to a fall in intravascular central venous pressure.(8) Future imaging based studies (possibly utilizing magnetic resonance imaging techniques) could further our understanding of how the timing of PFO valve opening is related to the inter-atrial pressure gradient change, particularly during the sudden airway pressure drop of the MM initiation.
Our findings may be altered by patho-physiologic states in which the balance between the right and left intra-cardiac pressures is changed. In patients with elevated right sided pressures (such as in pulmonary embolism, severe tricuspid regurgitation, or primary pulmonary hypertension), the baseline right-to-left pressure balance is shifted to favor the right side, and further studies would be needed to investigate whether such substrate could predispose to even more pronounced RA-LA pressure gradients during MM and OSA. Recent pilot data support this notion.(13) In patients with diastolic dysfunction involving primarily LV filling, the amount of right-to-left shunting may be diminished.
Limitations
Our study may underestimate the pressure differences in actual OSA. The decreases in intrathoracic pressure achieved by patients during actual OSAs can be substantially more dramatic than those pressure changes documented during the MMs in our study. Such wider intra-thoracic pressure swings could create even more profound increases in RA to LA gradient than we demonstrated. However, the invasive nature of the precise measurement of RA and LA pressure would be prohibitive to performing this study safely on sleeping subjects outside of the catheterization laboratory. Convincing data from previous studies suggest that MM is a valid and reproducible simulation of the true hemodynamic changes occurring in authentic OSA episodes.(8) While we were able to accurately measure pressure differences, the very small and transient amount of shunting precludes precise volume measurement. We did not observe any transient desaturation on pulse oximetry during the maneuvers.
The positioning of the LA catheter through the PFO could have theoretically led to an increase in the PFO patency; however, intra-cardiac echocardiography did not reveal a significant change in the shunted blood signal via Doppler imaging before and after the placement of the LA catheter during resting respiration. Additionally, if such increased left-to-right shunting had occurred it would have likely lead to a more prompt equalization of pressures between RA and LA, and consequent under-estimation of the RA-LA pressure gradient.
Clinical Implications
A growing body of evidence supports the notion that obstructive apneas can lead to shunting across a PFO,(3-6,14) and given that apneas may occur hundreds of times per night in patients with severe OSA, they may significantly increase the possibility of paradoxical embolus and stroke, especially since patients with OSA also have an altered hemostatic milieu with higher propensity to clot formation. (15,16) This theory is supported by the fact that OSA is independently associated with stroke. (5,17) However, our present study does not provide evidence regarding these epidemiological observations; rather it delineates the hemodynamic basis for the plausibility of this theory.
Conclusion
The MM is a useful intervention to approximate physiologic changes seen in patients with OSA. The onset of MM increased right-to-left pressure gradient across the atrial septum, likely as a result of greater blood return to the RA from extra-thoracic veins. The RA-LA pressure gradient achieved during MM was greater than that observed during VM. These findings delineate the hemodynamic substrate for right to left shunting during OSA.
Supplementary Material
Video with Audio
Intra-cardiac Doppler echocardiography showing a transient right to left shunt in a snoring patient (each snort represents a likely inspiratory obstruction).
Acknowledgments
This project was supported in part by grants from the Mayo Foundation, National Institutes of Health (NIH HL65176), National Center for Advancing Translational Sciences (NCATS; UL1 TR000135), and the Czech ministry of education (Human Bridge Grant, CZ.1.07/2.3.00/20.0022), and grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. This study was in part supported by European Regional Development Fund - Project FNUSA-ICRC (No. CZ.1.05/1.1.00/02.0123), by European Social Fund within the project Young Talent Incubator (reg. no. CZ.1.07/2.3.00/20.0022).
Abbreviations
- LA
Left atrium
- LV
Left ventricle
- MM
Mueller maneuver
- OSA
Obstructive sleep apnea
- PFO
Patent foramen ovale
- RA
Right atrium
- TEE
Trans-esophageal echocardiogram
- VM
Valsalva maneuver
Footnotes
Disclosures and Conflicts of Interest:
VKS received a gift to Mayo Foundation from Phillips Respironics Foundation, has served as a consultant for Merck, Johnson and Johnson, Respicardia, ResMed, Sova Pharmaceuticals, and Apnex Medical, and is working with Mayo Health Solutions and their industry partners on intellectual property related to sleep and cardiovascular disease. GSP has received a research grant from the Respironics Foundation. TK, BAB, VKS and GSR have submitted a disclosure relevant to these data to the Mayo Office of Intellectual Property.
References
- 1.Beelke M, Angeli S, Del Sette M, Gandolfo C, Cabano ME, Canovaro P, Nobili L, Ferrillo F. Prevalence of patent foramen ovale in subjects with obstructive sleep apnea: a transcranial Doppler ultrasound study. Sleep Med. 2003;4(3):219–23. doi: 10.1016/s1389-9457(02)00256-3. [DOI] [PubMed] [Google Scholar]
- 2.Orban M, Bruce CJ, Pressman GS, Leinveber P, Romero-Corral A, Korinek J, Konecny T, Villarraga HR, Kara T, Caples SM. Dynamic changes of left ventricular performance and left atrial volume induced by the mueller maneuver in healthy young adults and implications for obstructive sleep apnea, atrial fibrillation, and heart failure. The American journal of cardiology. 2008;102(11):1557–61. doi: 10.1016/j.amjcard.2008.07.050. others. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beelke M, Angeli S, Del Sette M, De Carli F, Canovaro P, Nobili L, Ferrillo F. Obstructive sleep apnea can be provocative for right-to-left shunting through a patent foramen ovale. Sleep. 2002;25(8):856–62. [PubMed] [Google Scholar]
- 4.Shiomi T, Guilleminault C, Stoohs R, Schnittger I. Leftward shift of the interventricular septum and pulsus paradoxus in obstructive sleep apnea syndrome. Chest. 1991;100(4):894–902. doi: 10.1378/chest.100.4.894. [DOI] [PubMed] [Google Scholar]
- 5.Pellaton C, Heinzer R, Michel P, Eeckhout E. Patent foramen ovale and obstructive sleep apnoea: from pathophysiology to diagnosis of a potentially dangerous association. Archives of cardiovascular diseases. 2011;104(4):242–51. doi: 10.1016/j.acvd.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Angeli S, Del Sette M, Beelke M, Anzola GP, Zanette E. Transcranial Doppler in the diagnosis of cardiac patent foramen ovale. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2001;22(5):353–6. doi: 10.1007/s100720100064. [DOI] [PubMed] [Google Scholar]
- 7.Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circulation. Heart failure. 2010;3(5):588–95. doi: 10.1161/CIRCHEARTFAILURE.109.930701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Somers VK, Dyken ME, Skinner JL. Autonomic and hemodynamic responses and interactions during the Mueller maneuver in humans. Journal of the autonomic nervous system. 1993;44(2-3):253–9. doi: 10.1016/0165-1838(93)90038-v. [DOI] [PubMed] [Google Scholar]
- 9.Hanly PJ, George CF, Millar TW, Kryger MH. Heart rate response to breath-hold, valsalva and Mueller maneuvers in obstructive sleep apnea. Chest. 1989;95(4):735–9. doi: 10.1378/chest.95.4.735. [DOI] [PubMed] [Google Scholar]
- 10.Bradley TD, Tkacova R, Hall MJ, Ando S, Floras JS. Augmented sympathetic neural response to simulated obstructive apnoea in human heart failure. Clinical science. 2003;104(3):231–8. doi: 10.1042/CS20020157. [DOI] [PubMed] [Google Scholar]
- 11.Nishimura RA, Holmes DR., Jr. Clinical practice. Hypertrophic obstructive cardiomyopathy. N Engl J Med. 2004;350(13):1320–7. doi: 10.1056/NEJMcp030779. [DOI] [PubMed] [Google Scholar]
- 12.Condos WR, Jr., Latham RD, Hoadley SD, Pasipoularides A. Hemodynamics of the Mueller maneuver in man: right and left heart micromanometry and Doppler echocardiography. Circulation. 1987;76(5):1020–8. doi: 10.1161/01.cir.76.5.1020. [DOI] [PubMed] [Google Scholar]
- 13.Huang J, Bouvette MJ. Occluding the pulmonary artery to improve detection of patent foramen ovale during ventricular assist device placement. Annals of cardiac anaesthesia. 2012;15(2):118–21. doi: 10.4103/0971-9784.95074. [DOI] [PubMed] [Google Scholar]
- 14.Shanoudy H, Soliman A, Raggi P, Liu JW, Russell DC, Jarmukli NF. Prevalence of patent foramen ovale and its contribution to hypoxemia in patients with obstructive sleep apnea. Chest. 1998;113(1):91–6. doi: 10.1378/chest.113.1.91. [DOI] [PubMed] [Google Scholar]
- 15.Nobili L, Schiavi G, Bozano E, De Carli F, Ferrillo F, Nobili F. Morning increase of whole blood viscosity in obstructive sleep apnea syndrome. Clin Hemorheol Microcirc. 2000;22(1):21–7. [PubMed] [Google Scholar]
- 16.Wedzicha JA, Syndercombe-Court D, Tan KC. Increased platelet aggregate formation in patients with chronic airflow obstruction and hypoxaemia. Thorax. 1991;46(7):504–7. doi: 10.1136/thx.46.7.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dyken ME, Somers VK, Yamada T, Ren ZY, Zimmerman MB. Investigating the relationship between stroke and obstructive sleep apnea. Stroke; a journal of cerebral circulation. 1996;27(3):401–7. doi: 10.1161/01.str.27.3.401. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video with Audio
Intra-cardiac Doppler echocardiography showing a transient right to left shunt in a snoring patient (each snort represents a likely inspiratory obstruction).