Abstract
This study investigated maternal psychological distress, perceptions of social supports, and parenting strains after the birth of a very low birthweight (VLBW) infant. Compared to mothers of term infants, mothers of VLBW infants had significantly higher incidence of psychological distress during the neonatal period, but did not differ from mothers of term infants in their feelings of role restriction, parenting competence, or social supports. Lower general social support predicted high distress levels, but only for mothers of VLBW infants. Mothers with a low sense of parenting competence, but support from spouse/partners reported lower maternal distress.
Keywords: bronchopulmonary dysplasia, high-risk infants, parenting, psychological distress, social support
Recent attention has been focused on the impact on maternal distress of the birth of an infant whose developmental status is at risk due to extreme prematurity and/or illness. Although uncontrolled studies have suggested that mothers of preterm, very low birthweight (VLBW) infants may be at increased risk for psychological distress postpartum (Blumberg, 1980; Brooten et al., 1988; Pedersen, Bento, Chance, Evans, & Fox, 1987), controlled studies have yielded inconsistent results. For example, no differences were found when life stress, or parenting and life satisfaction, were assessed in mothers of healthy, preterm infants in comparison to mothers of healthy, term infants at one month (Crnic, Ragozin, Greenberg, Robinson, & Basham, 1983). However, mothers of VLBW infants experienced a more depressed and anxious mood at the time of infant discharge when compared to mothers of term infants (Pedersen, Bento, Chance, Evans, & Fox, 1991). Discrepancies among study results may stem from differences in the severity of health risk or prematurity in prior samples. Because smaller and sicker infants now survive premature birth as a result of medical and technological advances, the incidence of chronic, severe medical conditions has increased in preterm populations. Thus, for many parents, the birth of a VLBW infant initiates long-term adaptation to the infant’s chronic illness and/or disability, rather than the shorter term adjustment to a healthy, preterm infant’s hospitalization, transitory illness, and eventual recovery (Goldberg, Brach-field, & DiVitto, 1980; Greenberg & Crnic, 1988; Landry, Chapieski, Fletcher, & Denson, 1988).
Bronchopulmonary dysplasia (BPD) is a common and serious chronic lung disease associated with prematurity. Formerly a rare condition, BPD is now the third leading cause of lung disease in children and the leading cause of lung disease in infants in the United States, with about 7,000 new cases diagnosed yearly (Northway, 1990). Infants with BPD frequently endure long hospitalizations, many lung infections, delayed growth, and usually require oxygen therapy, multiple medications, and close medical supervision. Common respiratory illnesses can be fatal for children with BPD, thus requiring close parental monitoring of infant contact with others. Feeding difficulties, in part due to breathing problems, also require increased parental efforts to maintain normal growth (Singer et al., 1996; Singer et al., 1992).
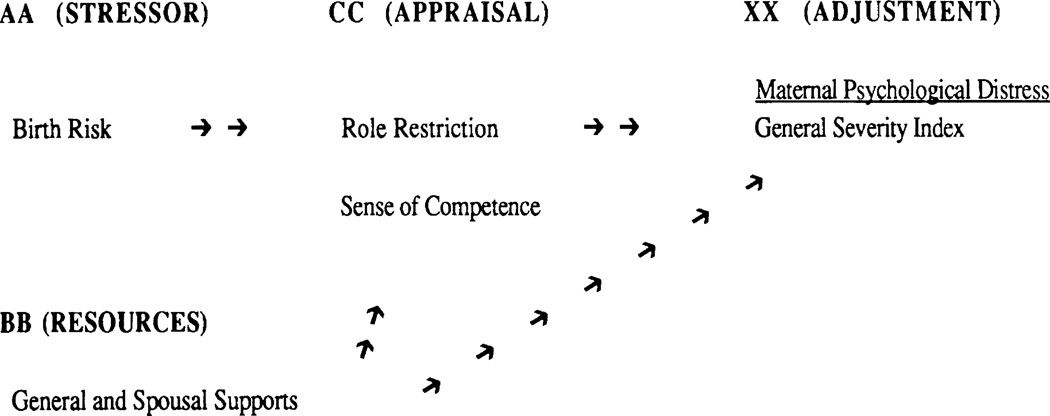
Several conceptual models have depicted child illness, or risk status, as a stressor affecting parental psychological health, family functioning, and child competence (Belsky, 1984; Crnic, Friedrich, & Greenberg, 1983; Wallander et al., 1989). One model that attempts to address how families adapt to unexpected and stressful life events, such as the birth of a very low birthweight or high-risk infant, is the Double ABCX Model of Family Adjustment and Adaptation (McCubbin & Patterson, 1983). This model focuses upon family efforts over time to recover from a crisis. The model attempts to delineate postcrisis variables that may influence the family’s ability to achieve adaptation, including critical psychological, family, and social factors that may influence adaptation; the processes engaged in to achieve satisfactory adaptation; and the outcome of these efforts. The model, in its simplest form, focuses on the stressor, family resistance resources, and family members’ appraisals of the stressor event in predicting adjustment outcome.
One outcome of interest in prior studies, because of its salience for child development, is maternal psychological distress. The impact of a child’s illness, or risk status, on maternal psychological health has been investigated in numerous studies, with mixed findings. Higher rates of depressive symptoms and feelings of increased psychological distress have been reported by mothers of children with chronic illnesses or disabling conditions in many controlled studies (Bendell, Culbertson, Shelton, & Carter, 1986; Breslau, Staruch, & Mortimer, 1982; Goldberg, Morris, Simmons, Fowler, & Levinson, 1990; Walker, Ortiz-Valdes, & Newbrough, 1989). With one exception (Goldberg et al., 1990), these studies have been cross-sectional and have confounded the factors of length of time since diagnosis and child age with illness status. BPD, as a chronic illness diagnosed neonatally, can provide a model for understanding parental adaptation to chronic illness early in infant development.
The mechanisms by which high-risk birth and infant illness might affect maternal distress levels have also not been investigated. Potential mechanisms of interest in the present study were specific aspects of maternal appraisal of her parenting role that might be affected by infant risk status and that might also relate to maternal distress (i.e., role restriction and sense of competence). Just as the birth of an infant gives increased salience to women’s roles as parents, the birth of a VLBW, high-risk infant would place greater strain on mothers’ parenting roles. Breslau, Staruch, and Mortimer (1982) found that the distress of mothers of sick children was greatest when their children were more dependent due to physical disabilities or illness. The authors attributed this distress to the greater restrictions on mothers imposed by parenting a physically dependent child. Parenting a sick, high-risk, VLBW infant may impose similar restrictions on mothers due to the greater time and worry associated with caregiving.
Recent studies have also suggested that maternal feelings of parenting competence are important influences on maternal distress (Teti & Gelfand, 1991). Lower maternal sense of competence has been linked to the intensity of negative emotional reactions postpartum in studies of mothers of healthy, but temperamentally difficult, infants (Cutrona & Troutman, 1986) and in studies of depressed mothers of healthy infants (Teti & Gelfand, 1991). Mothers of sick, VLBW infants may feel less competent in their parenting roles, because they must cope with infants who are more difficult, or irritable, due to prematurity and illness (Cutrona & Troutman, 1986; Goldberg et al., 1980). These appraisal factors may affect maternal adaptation through either a mediating or moderating mechanism. If these appraisal factors are mediators, they will account for the association of the stressor with the outcome of maternal distress. Alternatively, positive appraisal of her parental role, through less role restriction and better sense of competence, despite the burdens of caring for an ill or high-risk infant, could be conceptualized as a potentially moderating variable of maternal distress. In this latter case, maternal appraisal of parenting stress may differentially affect severity of psychological distress under certain conditions, such as lower social supports or greater financial burden (Baron & Kenny, 1986).
An important resistance resource for mothers of preterm, VLBW infants in their adaptation to parenting is social support. Social support has been shown to exert a significant influence on an individual’s psychological and physical health (Haggerty, 1980; Koeske & Koeske, 1990). Social support facilitates self-esteem and perceptions of self-efficacy in times of stress (Cohen & Wills, 1985; Cutrona & Troutman, 1986; Teti & Gelfand, 1991), thus reducing the intensity of negative emotional reactions. Maternal perceptions of poor social support have been linked to depressive affect in postpartum women (Cutrona & Troutman, 1986) and to higher psychological distress in mothers of sick children (Jessop, Riessman, & Stein, 1990). Social support might also affect maternal distress through its impact on parenting perceptions, such as maternal sense of competence (Belsky, 1984; Crnic, Ragozin, et al., 1983; Teti & Gelfand, 1991), or through maternal feelings of frustration with her parenting role. The "buffering" or moderating hypothesis asserts that social supports exert their most significant effects under conditions of high stress, such as the birth of a VLBW infant. Prior studies of postpartum women evaluating this hypothesis have produced mixed findings (Crnic, Ragozin, et al., 1983; Cutrona & Troutman, 1986). Based on Cohen and Wills’ (1985) theoretical framework, in order to evaluate social support as a buffer during stress, two conditions must be met: (a) the main effects of social support and the stressful event must each be significant in predicting distress, and (b) the interaction of social supports and the stressful events must be significant beyond the main effects.
The proposed model, which links infant VLBW and illness status at birth, social supports, and parenting appraisal of stressors to maternal postpartum distress, is depicted in Figure 1. The occurrence of VLBW birth is considered a stressor (AA) that can produce changes in the family system. The (BB) factor, general and spousal supports, includes resources of the family that help promote positive adjustment. Appraisal (CC) of the difficulty of the stressor (i.e., greater role restriction or lower sense of parenting competence) also affects maternal distress (XX). Review of the prior literature generated the following hypotheses:
Mothers of BPD and VLBW infants, during the neonatal period, will self-report greater psychological distress, more intense feelings of role restriction, and a lower sense of parenting competence than mothers of term infants.
Positive perceptions of spousal and general social supports will be negatively related to feelings of parental role restriction and psychological distress and positively related to sense of parenting competence for all mothers.
Positive social supports, both spousal and general supports, will differentially buffer maternal distress for mothers of BPD and VLBW infants. Maternal appraisal of role restriction and sense of parenting competence will mediate the relationship between VLBW birth and psychological distress, with greater perception of role restriction and lower sense of parenting competence related to greater psychological distress.
Figure 1.
Components of the Double ABCX Model of Family Adjustment and Adaptation.
METHOD
Sample
This investigation involved 193 mothers comprised of the following three groups: 63 mothers of VLBW infants who had developed BPD; 32 mothers of VLBW infants without BPD; and 98 mothers of healthy, term infants.
BPD infants were defined as preterm, VLBW infants who weighed <1500 grams at birth, required supplementary oxygen for more than 28 days due to lung immaturity at birth, and had radiographic evidence of chronic lung disease (Northway, Rosan, & Porter, 1967). VLBW infants were preterm infants who weighed <1,500 grams at birth and required oxygen supplementation for fewer than 14 days. Term infants had no diagnosed medical illnesses or abnormalities at birth, were >36 weeks gestational age (GA), and >2,500 grams birth weight for singleton infants.
For all groups, infants whose mothers had known psychiatric illnesses, mental retardation, or were identified as using drugs during pregnancy were excluded. The sample was recruited from the neonatal intensive care units (preterms) and newborn nurseries (full-terms) of one general and two tertiary care hospitals. There were no differences between mothers who refused to participate in the study and those who participated within any group on any of the demographic and medical variables noted.
Medical and demographic data were taken from hospital charts and maternal interviews. Infant gestational age (GA) was calculated based on combined information from infant Ballard examination (Ballard, Novak, & Driver, 1979) and maternal dates of last menstrual period and served as a measure of the degree of prematurity.
Groups did not differ with respect to socioeconomic status using the Hollingshead Scale (1957), which ranges from 1 (highest) to 5 (lowest), nor in infant race, infant gender, maternal education, and family structure (single vs. two-parent family). Proportionately, there were more firstborn infants in the BPD group than in the VLBW and term groups. Table 1 shows the demographic and medical characteristics of the three groups.
Table 1.
Sample Characteristics
| Bronchopulmonary Dysplasia (BPD) (N=63) M±SD |
Very Low Birthweight (VLBW) (N = 32) M±SD |
Full Term (T) (N=98) M±SD |
F/χ2 | |
|---|---|---|---|---|
| Infant | ||||
| Birth order | 1.6 ± 1.0 | 2.1 ± 1.0 | 2.1 ± 1.0 | 4.9b*** |
| Birthweight (grams) | 959 ± 260 | 1249 ± 192 | 3466 ± 537 | 704a***** |
| Weeks gestation | 27.2 ± 2.3 | 29.9 ± 2.2 | 39.9 ± 1.3 | 955a***** |
| Days on oxygen | 122 ± 175 | 5.4 ± 5.6 | 0 ± 0 | 28.0b***** |
| Race | ||||
| White | 54% | 48% | 52% | 1.1 |
| Black | 46% | 52% | 48% | |
| Sex | ||||
| Female | 40% | 50% | 52% | 1.4 |
| Male | 60% | 50% | 48% | |
| Multiple birth | 13% | 19% | 2% | 9.4c*** |
| Corrected age (weeks) | 3.7 ± 4.4 | 4.0 ± 5.4 | 5.3 ± 8.5 | 0.7 |
| Family | ||||
| Maternal education | 13.1 ± 1.8 | 13.0 ± 2.1 | 13.4 ± 2.4 | 0.5 |
| Maternal age (years) | 26.9 ± 5.7 | 27.6 ± 6.7 | 26.9 ± 6.0 | 0.1 |
| Socioeconomic status | 3.6 ± 1.0 | 3.6 ± 1.0 | 3.6 ± 1.0 | 0.7 |
| Percent married | 60% | 53% | 57% | 9.8 |
BPD < VLBW < T, p< .05.
BPD >/< VLBW and T, p < .05.
BPD and VLBW > T, p < .05.
p < .01.
p < .001.
Procedures
Mothers of preterm infants were approached to join the study while they were in the hospital prior to infant discharge. Mothers of term infants were left letters requesting them to volunteer for the study while in the hospital at the time of their infants’ births. Those who agreed were mailed self-report forms, which were reviewed with a research assistant during a subsequent visit. Each mother was paid $25 for participation, and transportation was provided. Mothers completed three questionnaires: the Family Inventory of Life Events and Changes, the Parenting Stress Inventory, and the Brief Symptom Inventory.
The Family Inventory of Life Events and Changes (FILE; McCubbin, Patterson, & Wilson, 1985) is a self-report instrument completed by mothers that was used to assess the family’s experience of a variety of life changes during the previous year. The inventory documents the occurrence or nonoccurrence of family life changes conceptualized as stressful in nine separate categories: intrafamily strains, marital strains, pregnancy and child bearing strains, finance/business strains, work-family transitions, illness, losses, transitions, and family legal violations. Cronbach’s alpha for the total and subscale groupings was .81 for the total, with subscale scores ranging from .30–.73. Both concurrent and predictive validity have been demonstrated by correlating the scores with other measures of family functioning and with the health status of children with cystic fibrosis (McCubbin, Patterson, & Wilson, 1985).
The Parenting Stress Index (PSI; Abidin, 1986) is a 120-item, self-report questionnaire that assesses parents’ perceptions of the degree of stress related to various dimensions of the parenting role. All items are scored on a Likert-type scale. The Social Isolation (general support) and Relationship With Spouse (spousal support) subscales were used as measures of the degree to which mothers perceived positive support from family and friends, and spouse or boyfriend, respectively. The Social Isolation sub-scale measures the degree to which the participant feels more generally supported (“I feel alone and without friends”), whereas spousal support items relate to more intimate partnering supports (“Having a child has caused more problems than I expected in my relationship with my spouse [male/female friend]”). The wording of the spousal support items allows them to be useful in both marital and single relationships. The Role Restriction subscale served as a measure of the extent to which mothers experienced their parenting role as restricting or frustrating. Typical items include, “I feel trapped by my responsibilities as a parent” and “Most of my life is spent doing things for my child.” The Sense of Competence subscale measures the extent to which a parent feels capable as a parent (“I enjoy being a parent”).
The PSI was normed on 534 families of children from 1 month to 19 years old who were seen in routine pediatric practice. Test-retest reliabilities are adequate (rs = .55 to .96), and the scales have been useful in differentiating the stressors experienced by parents of sick children from normative and comparison groups (Goldberg et al., 1990; Singer, Song, Hill, & Jaffe, 1990). In the present study, items were reverse scored on the Social Isolation subscale, which measures perceived general social supports and on the Relationship With Spouse subscale, which measures spousal or partner support, to indicate that positive relationships indicated higher supports. Internal consistency measures (Cronbach’s alpha) for the subscales in the present sample ranged from .72 to .88.
The Brief Symptom Inventory (BSI; Derogatis & Nelisaratos, 1983) is a 53-item self-report questionnaire tapping a range of psychiatric symptom patterns. It is scored and profiled on nine symptom dimensions that possess consensually established clinical significance and has acceptable reliability and validity (Derogatis & Cleary, 1977). Normative data are available on nonpatient and psychiatric populations (Derogatis, 1992). For the present study, a global measure derived from the scale, the General Severity Index (GSI), served as the dependent measure that summarized maternal self-report of psychological distress (Derogatis, 1992). Cronbach’s alpha for the present study averaged .94 for the three groups (BPD, VLBW, and term).
All mothers completed self-report forms as soon as possible after their infants reached 40 weeks corrected age (term birth). As noted in Table 1, there were no differences among groups based on corrected ages. Because infants were seen at equivalent corrected ages, groups differed on chronological age and in length of maternal experience with her infant. Because differential degree of experience might affect maternal psychological status and parenting stressors, all analyses were initially run using infant chronological age as a covariate. There were no covariate effects and chronological age was omitted from the model. Similarly, multiple birth status might also be expected to relate to degree of maternal distress, and we evaluated it as a potential covariate. Because multiple birth status was unrelated to maternal distress, it was also removed from the model.
RESULTS
Confounding Event Stressors
For the present study, the FILE served to determine whether the group differences on life stressors other than infant illness and prematurity could account for maternal psychological status. Additionally, some life stressors (e.g., financial or marital stresses) might reasonably be expected to relate to infant illness status. Thus, prior to hypothesis testing, multivariate analyses of variance were conducted on the subscales of the FILE in order to assess whether the study groups differed on other life stressors that might affect maternal distress.
The overall Wilk’s Lambda was .82, F(2, 169) = 1.9, p < 02. Group differences were then evaluated by univariate analyses of variance (ANOVAs), followed by Duncan’s multiple range post hoc analyses to determine which comparisons contributed to the overall effect. Pregnancy and illness were the only independent variables that distinguished among the groups. Mothers of both BPD and VLBW infants cited more pregnancy and illness stressors than mothers of term infants, with Ms ± SDs = 1.5 ± .8, 1.5 ± 1.0, and 1.1 ± .9, for BPD, VLBW, and term groups, respectively (F[2, 169] = 32, p < .05 for pregnancy and 1.6 ± .2, 1.3 ± 2, and .6 ± .9 for illness, F[2, 169] = 12.6, p < .001). Groups did not differ on financial stressors, life transitions, losses, or legal or work-related events that might influence maternal distress symptoms.
Maternal Distress
Because of a skewed distribution, GSI scores were normalized using square root transformations prior to analyses. A one-way ANOVA was conducted on the GSI. Duncan’s multiple range post hoc tests, which correct for the number of comparisons, were used to determine which group comparisons contributed to the overall effect.
As predicted by hypothesis 1, mothers differed in their self-reports of psychological distress by group (F[2, 190] = 5.3, p <.01). Follow-up analyses indicated that mothers of both BPD and VLBW infants did not differ from each other but reported significantly greater distress levels than mothers of healthy term infants (see Table 2). Using cut-off scores based on the nonpatient, normative data of the GSI for females, 34% of mothers of BPD infants and 31% of mothers of VLBW infants showed evidence of moderate (>84th percentile) distress as compared to 21% of mothers of healthy term infants (Zc [1, 150] = 1.8, p < .04 for BPD vs. terms and Zc [1, 121] = 1.4, p < .07 for VLBW vs. terms). Severe distress (>98th percentile) postpartum was self-reported by 13% of mothers of both BPD and VLBW infants but by only 2% of mothers of term infants (Zc [1, 150] = 2.7, p < .02 for BPD vs. term and Zc [1, 121] = 2.1, p < .02 for VLBW vs. term), indicating that mothers of both groups of VLBW infants had higher rates of clinically significant distress than mothers of term infants.
Table 2.
Comparisons by Risk/Illness Group
| Bronchopulmonary Dysplasia (BPD) |
Very Low Birthweight (VLBW) |
Term (T) |
|||||
|---|---|---|---|---|---|---|---|
| M ± SD | Range | M ± SD | Range | M ± SD | Range | F | |
| Psychological Distress | (N =63) | (N =32) | (N =98) | ||||
| General Severity Index | .62 ± .6 | 0–4 | .56 ±.6 | 0–4 | .37 ±.4 | 0–4 | 5.3a*** |
| Parenting Stressor | (N = 55) | (N = 29) | (N = 90) | ||||
| Role restriction | 18.6 ± 5 | 7–34 | 19.8 ± 6 | 8–34 | 18.4 ± 5 | 7–31 | .7 |
| Sense of competence | 28.5 ± 6 | 17–45 | 29.2 ±6 | 17–41 | 28.4 ± 7 | 15–48 | .8 |
| Social Support | (N =55) | (N =29) | (N =90) | ||||
| General support | 14.2 ±4 | 6–27 | 14.4 ± 5 | 8–26 | 13.3 ± 4 | 5–24 | .3 |
| Spousal support | 18.4 ± 5 | 7–34 | 18.6 ± 6 | 8–32 | 18.1 ± 5 | 7–31 | .9 |
BPD and VLBW > T, p < .05.
p< 0.1.
Role Restriction and Sense of Parenting Competence
To address hypothesis 1, multivariate analyses of variance (MANOVAs), with group as the independent variable, were initially conducted on the sub-scales of the PSI. Significant multivariate group differences were then evaluated by univariate analyses of variance (ANOVAs).
Contrary to hypothesis 1, groups did not differ in their perception of how restrictive they found their parental roles or in their feelings of competence as parents (see Table 2). Because these two parenting stressors were unrelated to infant illness or risk, they could not be considered mediators of maternal distress. Therefore, along with social supports, they were evaluated in their potential for moderating maternal distress.
Relationship of Parenting Stressors and Social Support to Maternal Distress
To address hypothesis 2, correlational analyses assessed the interrelationships among demographic variables, infant illness, parenting stressors, and social support factors. All correlations were first computed within each group and were reported by group if there were significant differences. If there were no differences, correlations for the combined groups were presented. For each risk group, Table 3 presents the zero-order correlations between the parenting stressor and social support variables and maternal report of distress. For all groups, greater maternal sense of competence and perception of positive spousal support were significantly related to lower distress. However, for general support, the relationship between perceived general support and maternal distress varied by group. Although higher levels of general support were related to lower distress for mothers of VLBW and BPD infants, there was no relationship between general support and distress for mothers of term infants. Similarly, relationships varied by group for the parenting stressor of role restriction and maternal distress. Greater feelings of role restriction correlated significantly with higher distress for mothers of both groups of VLBW infants; however, role restrictiveness did not significantly relate to distress in mothers of term infants.
Table 3.
Correlations of Maternal Distress (GSI) With Parenting Stressors and Social Support by Group
| General Severity Index Score |
|||
|---|---|---|---|
| Bronchopulmonary Dysplasia (N = 55) |
Very Low Birthweight (N = 29) |
Term (N = 90) |
|
| Parenting Stressor | |||
| Role restriction | .45***** | .34* | .20 |
| Sense of competence | −.46***** | −.37* | −.41***** |
| Social Support | |||
| General support | −.58***** | −.55*** | −.11 |
| Spousal support | −.35*** | −.32 | −.26** |
Note. GSI = General Severity Index.
p < .10.
p < .05.
p < .01.
p < .001.
Interrelationships Among Parenting Stressor and Support Variables
As shown in Table 4, parenting stressor and social support variables were all moderately intercorrelated, with positive supports negatively related to parenting stressors. Mothers who felt more competent in parenting and who perceived better social or spousal supports reported feeling less restricted in their parenting role. Similarly, mothers who experienced more support from spouse or friends also felt more competent.
Table 4.
Simple Correlations Among Parenting Stressors and Support Variables (N = 174)
| Sense of Competence | General Support | Spousal Support | |
|---|---|---|---|
| Parenting Stressor | |||
| Role restriction | −.42 | −.51 | −.54 |
| Sense of competence | – | .47 | .47 |
| Social Support | |||
| General support | – | .55 |
Note. All correlations were significant, p < .05.
Predictors of Maternal Psychological Distress
To address hypothesis 3, hierarchical regression analysis was used to determine the relative predictive power of infant illness (BPD) and VLBW status, parenting stressors, support factors, and their interactions for maternal distress. Control variables of race (dummy coded 0 = White; 1 = non-White) and social class (1–5) were entered first, followed at each step by individual parenting stressor and social support variables in the order noted in Table 5. Support variables were hypothesized as exogenous in our model and were entered prior to parenting stressors. Spousal support was entered first, followed by general social support, based on prior studies (Crnic, Ragozin, et al., 1983) and theorizing (Belsky, 1984) suggesting that more immediate resources from intimate relationships are most supportive of early parenting. Group (BPD, VLBW, or term) was then entered to determine the added contribution of infant VLBW and BPD to maternal distress, after accounting for factors of parenting stressors and social supports. To evaluate the role of social support as a buffer or moderator of stress, several interaction terms were entered individually and hierarchically into the regression equation. The cross-product terms of group risk status (BPD, VLBW, and term) and each of the parenting stressor and social support variables were entered into the equation individually after group (i.e., Group x Spousal Support, Group x General Social Support, Group x Role Restriction, and Group x Sense of Competence).
Table 5.
Summary of Hierarchical Multiple Regression Analysis of Maternal Distress (GSI) on Demographic Factors, Social Supports, Risk Status (Group), and Parenting Stressors (N = 193)
| Criterion: General Severity Index Score |
||||||
|---|---|---|---|---|---|---|
| Step | Predictor | B | SE B | R2 Change | R2a | Beta |
| 1 | Race | −.06 | .07 | .003 | .00 | −.06 |
| 2 | Social class | −.22 | .07 | .05 | .05 | −.22** |
| 3 | Spousal support | −.29 | .07 | .08 | .13 | −.28**** |
| 4 | General support | −.26 | .09 | .04 | .17 | −.26**** |
| 5 | Sense of competence | −.21 | .09 | .03 | .20 | −.20** |
| 6 | Role restriction | .16 | .09 | .02 | .22 | .16 |
| 7 | Group | .20 | .07 | .04 | .26 | .20** |
| 8 | Group x Spousal Support | .01 | .01 | .003 | .26 | .24 |
| 9 | Group x General Support | .08 | .02 | .05 | .31 | 1.20**** |
| 10 | Group x Sense of Competence | −.006 | .01 | .0007 | .31 | −.17 |
| 11 | Group x Role Restriction | .01 | .02 | .001 | .31 | .20 |
| 12 | Spousal x General Support | .003 | .002 | .006 | .31 | .43 |
| 13 | Spousal Support x Sense of Competence | −.008 | .002 | .05 | .36 | −2.00**** |
| 14 | Spousal Support x Role Restriction | −.0008 | .002 | .0004 | .36 | −.14 |
| 15 | General Support x Role Restriction | .001 | .004 | .0004 | .36 | −.26 |
| 16 | General Support x Sense of Competence | −.001 | .004 | .0006 | .36 | .17 |
Note. GSI = General Severity Index.
R2 values are cumulative.
p < .05.
p < .005.
Also, because parenting stressor and support variables were intercorrelated, their cross-product terms (Spousal Support x Social Support, Spousal Support x Sense of Competence, Spousal Support x Role Restriction, Social Support x Sense of Competence, Social Support x Role Restriction) were also each entered into the equation separately, after the group cross-product terms.
Significant interactions were followed by examining the distributions of interactive variables separately. The cutoff point for determining the subsample of mothers designated as high and those designated as low was the median (50th percentile) for the respective means.
Table 5 shows significant main and interaction effects that predicted maternal distress. After controlling for race and social class, both spousal and general social supports were significant predictors of maternal distress, accounting for 8% and 5% of the variance, respectively. Although general social supports remained significant in predicting distress once spousal support was accounted for, the relative effect of spousal support was somewhat weakened after general social support was controlled.
Beyond demographic and social support factors, maternal sense of competence and perception of role restriction also predicted maternal distress, with each accounting for 2% of the variance. Sense of competence remained a significant predictor of distress even when role restriction was accounted for. However, after sense of competence was considered, the effect of role restriction was weakened.
Beyond the effects of demographic, support, and parenting stressors, infant risk status (group) significantly predicted maternal distress, accounting for 4% of the variance. Further, addressing hypothesis 3, the interaction of infant risk status with social support significantly predicted maternal distress, supporting the notion of a buffering, or moderating, effect of support during times of high stress, such as the birth of a high-risk infant.
Illustrations of the moderating effect of social supports on maternal distress under conditions of high-risk infant birth are shown in Table 6. Mothers of BPD and VLBW infants who self-reported positive general social supports had levels of psychological distress equivalent to mothers of term infants. In contrast, mothers of BPD and VLBW infants who perceived themselves as having less general social support experienced higher levels of distress than mothers of term infants. Low general social supports were unrelated to distress in mothers of term infants. The moderating effect was significant for general social support, but not for spousal support, as the Group x Spousal Support interaction term did not reach significance (see Table 5).
Table 6.
Means and Standard Deviations of GSI Scores by Group and High Versus Low General Social Support
| Social Support | Term | Very Low Birthweight | Bronchopulmonary Dysplasia |
|---|---|---|---|
| High | (n = 41) .25 ± .22 | (n = 14) .25 ± .33 | (n = 17).31 ± .16 |
| Low | (n =51) .33 ± .25 | (n = 13) .59 ± .39 | (n = 39) .51 ± .33 |
Note. GSI = General Severity Index.
Although there were no other significant group interaction effects, there was a significant interaction between spousal support and maternal sense of competence that also moderated maternal distress (see Table 7), indicating that mothers with a low sense of parenting competence were buffered from distress in the context of spousal support. Alternatively, maternal sense of parenting competence predicted lower psychological distress under conditions of poor spousal supports. That is, higher partner/spousal support was related to lower distress levels in mothers, even when they were insecure about their parenting competence, and a greater sense of competence was related to better psychological status, even when spousal supports were low.
Table 7.
Means and Standard Deviations of GSI Scores by Level of Spousal Support and Sense of Competence
| Spousal Support |
||
|---|---|---|
| Sense of Competence | High | Low |
| High | (n = 54) .27 ± .22 | (n = 32) .31 ± .20 |
| Low | (n = 59) .30 ± .23 | (n = 59) .51 ± .35 |
Note. GSI = General Severity Index.
DISCUSSION
Results from the present study support the premise that infant risk status, as measured through maternal experiences of very low birthweight birth and infant illness, is a stressor that places the mother at increased likelihood for psychological distress neonatally (Pedersen et al., 1987). From a clinical risk perspective, moderately severe symptoms of distress were self-reported by about one third of postpartum mothers of VLBW infants in this sample. Moreover, significantly more mothers of VLBW infants in comparison to mothers of term infants had clinically high levels of symptoms of severe overall distress. As similar distress levels in mothers have been linked to their decreased sensitivity and greater punitiveness to their infants, as well as to altered feeding interactions for VLBW infants (Cohn & Tronick, 1983; Field, Healy, Goldstein, & Guthertz, 1990; Singer et al., 1996), identification of and intervention for mothers of VLBW infants at greater risk for distress might enhance dyadic interactions and later outcome for high-risk infants.
The present data provide support for the importance of the role of family resource and resistance factors denoted in the Double ABCX Model in affecting maternal psychological adjustment. Both general and more intimate spousal supports were found to have significant impact as moderators of maternal psychological distress. Neither role restriction nor sense of competence, the stressor appraisal variables, were mediators of maternal distress. Sense of parenting competence, however, was a significant moderator of distress under conditions of low spousal support.
Results of this study reinforce the contextual importance of social supports to maternal psychological well-being early in adapting to parenting a high-risk infant. Perceived social supports, rather than infant risk status per se, were most critical in predicting mothers’ distress, as mothers of VLBW infants who felt positively supported did not experience increased distress symptoms. Some other studies have not found variation in the effects of social support as a function of stress level in mothers of young preterm infants (Crnic, Ragozin, et al., 1983; Cutrona & Troutman, 1986). However, their samples of healthy term and preterm, but not VLBW, infants, whose families had low life stress, were different from ours in which infant risk status was high and life stressors varied significantly.
Consistent with the buffering hypothesis (Cohen & Wills, 1985), social support was most salient under the most stressful conditions. Mothers’ distress was greater when infant illness or VLBW was accompanied by perceived low social support. Conversely, low social support was not related to maternal distress for mothers of term infants. Results from the present study indicate that the perceived availability of support plays a protective role in preventing the pathologic effects of negative life events. The powerful impact of the role of social support in conjunction with life events was likely enhanced in this study by the comparison of VLBW birth, as a stressful life event, with the birth of a healthy term infant, typically perceived as a joyful life event. The finding of the lack of relationship between general social support and distress in mothers of term infants suggests that positive life events may also function as a stress buffer under conditions of low social support (Cohen & Hoberman, 1983).
Perception of positive support from a spousal or intimate relationship also was a uniquely important moderating factor under certain conditions, in that high spousal or partner support mitigated maternal psychological distress for mothers with a lower sense of parenting competence. The importance of marital supports on maternal self-efficacy, life satisfaction, and parenting behavior has been demonstrated in prior studies of young parents (Crnic, Ragozin, et al., 1983; Teti & Gelfand, 1991). The present study suggests that, for mothers whose sense of competence around caring for a young infant is poor, positive intimate support reduces the psychological distress usually associated with lower sense of competence.
Surprisingly, mothers of VLBW infants, despite their differences in distress, did not differ from mothers of term infants in terms of perception of their experiences of role restriction or in sense of competence in parenting. Prior studies of older infants with a variety of illnesses or risk conditions have been inconsistent in findings related to these parenting stressors (Bendell et al., 1986; Goldberg et al., 1990; Kazak, Reber, & Snitzer, 1988). In the present study, mothers were seen relatively early in the neonatal period, and the cumulative strains of caring for a high-risk infant may not have yet affected their experiences of competence or restriction in parenting. Because all young infants require substantial caregiving efforts neonatally, differences among groups might not have been discernible yet.
Limitations of the study include the fact that the absence of a pre- and post-delivery research design does not allow causal inferences to be made about the impact of the birth of a VLBW infant on maternal psychological status. However, the independent measurement of infant risk status and the fact that groups were carefully balanced for other factors known to relate to psychological distress and health status suggest a legitimate means of evaluating the postpartum relationships between infant VLBW birth, risk status, and maternal psychological distress. Moreover, there were no differences among groups in their experience of a variety of life stressors other than the pregnancy and illness variables of interest.
Another concern is that maternal self-report was used to obtain information regarding mothers’ psychological distress, social supports, and parenting perceptions. However, multiple regression analyses established the relative and independent contributions of infant risk status, social supports, and maternal parenting perceptions to maternal distress. Results were reported conservatively, only after controlling for all other factors in the model. Additionally, univariate correlations yielded only low to moderate correlations among the parameters measured, which indicates that multi-collinearity was not a problem.
Similar levels of distress symptoms have been related to impairments in caregiving and affective interactions in studies of healthy term infants (Cohn & Tronick, 1983; Crnic, Ragozin, et al., 1983; Field et al., 1990; Gelfand & Teti, 1990), and the present study suggests that maternal distress is a potential factor in the differences in caregiving behaviors noted in other studies of preterm infants. Supporting this hypothesis, in another study of this population that evaluated feeding interactions, mothers of VLBW infants who were more depressed were less responsive to their infants (Singer et al., 1996).
Future studies should evaluate the specific clinical dimensions of, and the types and severity of, maternal distress in VLBW populations, as well as assess whether maternal distress has an impact on the long term outcomes of VLBW infants. Although sample size limitations did not allow its use in the current study, path or structural equation analysis would be optimal in developing models relevant to parental adaptation to the care of preterm infants.
CLINICAL IMPLICATIONS
Findings from this study indicate that the birth of a very low birthweight infant evokes considerable psychological distress, primarily for mothers who also perceive themselves as lacking social supports. Given that one third of all mothers of preterm infants had clinically discernible levels of distress, these data suggest that the neonatal period may be an optimal time period for identification of those mothers who are most at risk. Although this study did not elaborate on the specific nature of maternal symptoms, other studies have implicated depression, anxiety, and hostility (Brooten et al., 1988; Singer et al., 1996) as contributors to parental distress. Especially for infants who are ill, such as those with BPD, grief reactions similar to those of parents whose infants have died have been reported (Benfield, Leib, & Neuber, 1976).
The high volume, short-term, acute care characteristics of modern hospitals do not lend themselves well to the provision of social supports for families. Although most major medical centers now have follow-up programs for preterm infants, these visits tend to occur infrequently and are focused on the medical and developmental outcomes of the infant rather than on family processes. In an innovative study of parent-initiated telephone calls, Brooten and colleagues (1988) found that, over the first 18 months of life, mothers called a hotline most frequently in the first 3 months after childbirth. Mothers initiated contact primarily to seek reassurance about the infant’s physical conditions and behavior, but also for personal concerns regarding relationships, return to school or work, frustrations related to medical care, and financial problems. Out of 36 families, only two fathers initiated calls, suggesting that mothers continue to have primary responsibility for the infant’s care. The authors concluded that a telephone hotline provided important supports for mothers of preterm infants in a cost-effective manner.
The layering of social and psychological services onto standard follow-up care for premature infants and their parents, whether it be through telephone services, a discharge assessment with a mental health professional, or parent support groups (Baley, Hancharik, & Rivers, 1988), seems warranted given data from the present study that indicate high rates of initial maternal distress and the powerful positive impact of social supports during stress. Insofar as such services can identify those mothers with symptoms of clinical distress for referral to more formal intervention or alleviate distress during the postpartum period, they may prevent the development of more severe symptoms that are likely to interfere with effective parenting (Cohn & Tronick, 1983; Field et al., 1990).
The present data also suggest the importance of evaluating other family factors, particularly maternal perception of spousal supports. Positive perception of spousal supports moderated distress symptoms for mothers who felt less competent in their caregiving abilities. Fathers are less likely to have contact with health care providers (McKeever, 1981), despite their importance in facilitating maternal adaptation in this and other studies (Crnic, Ragozin, et al., 1983; Friedrich, 1979; Stoneman, Brody, & Burke, 1989). These data suggest that every effort must be made to engage fathers in child care. Inquiry about paternal involvement by health care providers and attempts to accommodate support services to their needs may have a positive impact on maternal distress.
Footnotes
This research was supported by grants NIH-HL 38193 and Maternal and Child Health Services MCJ 390592. We thank our consultant, Dr. Tiffany Field, and the mothers, the hospitals, and the nursing staff who participated in this project, especially Barb Cavender, R.N., and Drs. Jill Baley, Mark Collin, John Moore, and Lawrence Lilien. We also thank Terri Lotz-Ganley for manuscript preparation and Bridgett Davis, Roger Bielefeld, Ehat Ercanli, and Lori Zrimsek for data collection and analyses. Portions of this article were presented at the International Conference on Infant Studies, Miami, FL, May, 1992, and at the Society for Pediatric Research Meetings, Seattle, WA, May, 1994.
Contributor Information
Lynn T. Singer, Rainbow Babies and Childrens Hospital, 11100 Euclid Avenue, Mail Stop 6019, Cleveland, OH 44106.
Marilyn Davillier, Department of Pediatrics, Case Western Reserve University School of Medicine, Cleveland, OH.
Peggy Bruening, Department of Pediatrics, Case Western Reserve University School of Medicine, Cleveland, OH.
Suzanne Hawkins, Department of Pediatrics, Case Western Reserve University School of Medicine, Cleveland, OH.
Toyoko S. Yamashita, Department of Epidemiology and Biostatistics, Case Western Reserve University School of Medicine, Cleveland, OH.
REFERENCES
- Abidin RR. Parenting Stress Index. 2nd ed. Charlottesville, VA: Pediatric Psychology Press; 1986. [DOI] [PubMed] [Google Scholar]
- Baley J, Hancharik S, Rivers A. Observations of a support group for parents with infants with severe bronchopulmonary dysplasia. Journal of Developmental and Behavioral Pediatrics. 1988;9:19–24. [PubMed] [Google Scholar]
- Ballard J, Novak K, Driver M. A simplified score for assessment of fetal malnutrition of newly born infants. Journal of Pediatrics. 1979;95:769–774. doi: 10.1016/s0022-3476(79)80734-9. [DOI] [PubMed] [Google Scholar]
- Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual strategies and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Bendell D, Culbertson J, Shelton T, Carter B. Interrupted infantile apnea: Impact on early development, temperament, and maternal stress. Journal of Clinical Child Psychology. 1986;15:304–310. [Google Scholar]
- Benfield D, Leib S, Neuber J. The response of parents to the birth of a critically ill newborn in a regional center. New England Journal of Medicine. 1976;294:975–978. doi: 10.1056/NEJM197604292941803. [DOI] [PubMed] [Google Scholar]
- Blumberg NL. Effects of neonatal risk, maternal attitude, and cognitive style on early postpartum adjustment. Journal of Abnormal Psychology. 1980;89:139–150. doi: 10.1037//0021-843x.89.2.139. [DOI] [PubMed] [Google Scholar]
- Breslau N, Staruch K, Mortimer E. Psychological distress in mothers of disabled children. American Journal of Diseases of Children. 1982;136:682–686. doi: 10.1001/archpedi.1982.03970440026007. [DOI] [PubMed] [Google Scholar]
- Brooten D, Gennaro S, Brown L, Britts P, Gibbons A, Babenwill-Sachs S, Kumar S. Anxiety, depression and hostility in mothers of preterm infants. Nursing Research. 1988;37:213–216. [PubMed] [Google Scholar]
- Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Cohen S, Wills T. Stress, social support and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Cohn J, Tronick E. Three month old infants’ reaction to simulated maternal depression. Child Development. 1983;54:185–193. [PubMed] [Google Scholar]
- Crnic K, Friedrich W, Greenberg M. Adaptation of families with mentally retarded children: A model of stress, coping, and family ecology. American Journal of Mental Deficiency. 1983;88:125–138. [PubMed] [Google Scholar]
- Crnic K, Ragozin A, Greenberg M, Robinson N, Basham R. Social interaction and developmental competence of preterm and full-term infants during the first year of life. Child Development. 1983;54:1199–1210. [PubMed] [Google Scholar]
- Cutrona C, Troutman B. Social support, infant temperament, and parenting self-efficacy: A mediational model of postpartum depression. Child Development. 1986;57:1507–1518. [PubMed] [Google Scholar]
- Derogatis LR. The Brief Symptom Inventory manual. Baltimore, MD: Clinical Psychometric Research; 1992. [Google Scholar]
- Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90. Journal of Clinical Psychology. 1977;33:981–989. [Google Scholar]
- Derogatis LR, Nelisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Field TM, Healy B, Goldstein S, Guthertz M. Behavior-state matching and synchrony in mother-infant interactions of non-depressed versus depressed dyads. Developmental Psychology. 1990;26:7–14. [Google Scholar]
- Friedrich WN. Predictors of coping behavior of mothers of handicapped children. Journal of Consulting and Clinical Psychology. 1979;47:1140–1141. doi: 10.1037//0022-006x.47.6.1140. [DOI] [PubMed] [Google Scholar]
- Gelfand DM, Teti D. The effects of maternal depression on children. Clinical Psychology Review. 1990;10:329–353. [Google Scholar]
- Goldberg S, Brachfield S, DiVitto B. Feeding, fussing, and play: Parent-infant interaction in the first year as a function of prematurity and perinatal medical problems. In: Field T, editor. High-risk infants and children: Adult and peer interactions. New York: Academic Press; 1980. pp. 133–154. [Google Scholar]
- Goldberg S, Morris P, Simmons R, Fowler R, Levinson J. Chronic illness in infancy and parenting stress: A comparison of three groups of parents. Journal of Pediatric Psychology. 1990;15:347–358. doi: 10.1093/jpepsy/15.3.347. [DOI] [PubMed] [Google Scholar]
- Greenberg M, Crnic K. Longitudinal predictors of developmental status and social interaction in premature and full-term infants at age two. Child Development. 1988;59:554–570. doi: 10.1111/j.1467-8624.1988.tb03216.x. [DOI] [PubMed] [Google Scholar]
- Haggerty RJ. Life stress, illness, and social support. Developmental Medicine and Child Neurology. 1980;22:391–400. doi: 10.1111/j.1469-8749.1980.tb03723.x. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Two factor index of social position. New Haven, CT: Yale University Press; 1957. [Google Scholar]
- Jessop D, Riessman C, Stein R. Chronic childhood illness and maternal mental health. Developmental and Behavioral Pediatrics. 1990;9:147–156. [PubMed] [Google Scholar]
- Kazak A, Reber M, Snitzer L. Childhood chronic illness and family functioning: A study of phenylketonuria. Pediatrics. 1988;81:224–230. [PubMed] [Google Scholar]
- Koeske G, Koeske R. The buffering effect of social support on parental stress. American Journal of Orthopsychiatry. 1990;60:440–451. doi: 10.1037/h0079164. [DOI] [PubMed] [Google Scholar]
- Landry S, Chapieski L, Fletcher J, Denson S. Three year outcomes for low birth weight infants: Differential effects of early medical complications. Journal of Pediatric Psychology. 1988;13:317–327. doi: 10.1093/jpepsy/13.3.317. [DOI] [PubMed] [Google Scholar]
- McCubbin HI, Patterson JM. The Double ABCX Model of adjustment and adaptation. In: McCubbin H, Sussman M, Patterson J, editors. Advances and developments in family stress theory and research. New York: Haworth Press; 1981. pp. 95–106. [Google Scholar]
- McCubbin HI, Patterson JM, Wilson LR. FILE: Family Inventory of Life Events and Changes. In: McCubbin HI, Thompson A, editors. Family assessment: Inventories for research and practice. Madison, WI: University of Wisconsin; 1985. pp. 81–100. [Google Scholar]
- McKeever PT. Fathering the chronically ill child. American Journal of Maternal Child Nursing. 1981;6:124–128. doi: 10.1097/00005721-198103000-00014. [DOI] [PubMed] [Google Scholar]
- Northway W. Bronchopulmonary dysplasia: Then and now. Archives of Diseases of Childhood. 1990;65:1076–1081. doi: 10.1136/adc.65.10_spec_no.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northway WH, Rosan R, Porter DY. Pulmonary disease following respiratory therapy of hyaline membrane disease. New England Journal of Medicine. 1967;276:357–359. doi: 10.1056/NEJM196702162760701. [DOI] [PubMed] [Google Scholar]
- Pedersen D, Bento S, Chance G, Evans B, Fox A. Maternal emotional responses to preterm birth; Paper presented at the bi-annual meeting of the Society for Research in Child Development; Seattle, WA. 1991. Apr, [Google Scholar]
- Pedersen DR, Bento S, Chance G, Evans B, Fox A. Maternal emotional response to preterm birth. American Journal of Orthopsychiatry. 1987;57:15–21. doi: 10.1111/j.1939-0025.1987.tb03504.x. [DOI] [PubMed] [Google Scholar]
- Singer L, Davillier M, Preuss L, Szekely L, Hawkins S, Yamashita T, Baley J. Feeding interactions in infants with very low birthweight and bronchopulmonary dysplasia. Journal of Developmental and Behavioral Pediatrics. 1996;17(2):69–76. [PMC free article] [PubMed] [Google Scholar]
- Singer L, Martin R, Hawkins S, Benson-Szekely L, Yamashita T, Carlo W. Oxygen desaturation complicates feeding of bronchopulmonary dysplasia infants in the home environment. Pediatrics. 1992;90:380–384. [PMC free article] [PubMed] [Google Scholar]
- Singer L, Song L, Hill B, Jaffe A. Stress and depression in mothers of failure-to-thrive children. Journal of Pediatric Psychology. 1990;15:6–10. doi: 10.1093/jpepsy/15.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoneman Z, Brody G, Burke M. Marital quality, depression and inconsistent parenting: Relationship with observed mother-child conflict. American Journal of Orthopsychiatry. 1989;59:105–117. doi: 10.1111/j.1939-0025.1989.tb01639.x. [DOI] [PubMed] [Google Scholar]
- Teti D, Gelfand DM. Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development. 1991;62:918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x. [DOI] [PubMed] [Google Scholar]
- Walker L, Ortiz-Valdes F, Newbrough JR. The role of maternal employment and depression in the psychological adjustment of chronically ill, mentally retarded, and well children. Journal of Pediatric Psychology. 1989;14:357–370. doi: 10.1093/jpepsy/14.3.357. [DOI] [PubMed] [Google Scholar]
- Wallander J, Varni J, Batani L, Harris HT, De Hahn C, Wilcox KT. Disability parameters, chronic strain, and adaptation of physically handicapped children and their mothers. Journal of Pediatric Psychology. 1989;14:32–42. doi: 10.1093/jpepsy/14.1.23. [DOI] [PubMed] [Google Scholar]