Abstract
We report the case of an HIV-infected man returning from Thailand with secondary syphilis with general symptoms, hepatitis and a pulmonary mass lesion. A cerebrospinal fluid examination showed no signs of neurosyphilis. Two months after successful treatment with benzathine penicillin he presented with a mass lesion in the brain suspected to be a glioma or glioblastoma, which turned out to be a syphilitic gumma. Syphilis remains a great imitator in clinical medicine. Syphilitic brain gummata can develop within a few months.
Background
Our case shows that syphilis continues to be a great imitator, a ‘chameleon’ in clinical medicine, and should be included in the differential diagnosis of cerebral and pulmonary mass lesions and hepatitis in patients with risk of attracting sexually transmitted diseases. We were surprised, in this case, by the very short time taken to develop syphilitic brain gummata.
Case presentation
A 40-year-old man presented to the emergency department with persistent fatigue, excessive sweating and pain in the right thorax 7 weeks after a trip to Thailand. Truncal exanthema appeared after taking ibuprofen. No fever, muscle or joint pain, or other skin lesions or gastrointestinal symptoms were apparent. The patient was diagnosed with an HIV-1 infection 7 years ago. Without antiretroviral therapy the CD4 count values were between 412 and 570 cells/μL and HI-viraemia between 3600 and 25 000 copies/mL. Apart from anal condylomata acuminata, no other illnesses were noted.
Investigations
The patient was subfebrile with truncal macular skin exanthema. Laboratory testing revealed normochromic anaemia (haemoglobin 126 g/L), differentiation of leucocytes were without pathological findings. Platelets, serum glucose and renal retention values were within normal range. C reactive protein was slightly elevated (25 mg/L), transaminase levels were 2–4 fold and alkaline phosphatase level was 5-fold above upper normal limit. D dimers were severely elevated at >1000 µg/L. CT scan ruled out a pulmonary embolism. However, there was an unclear consolidation around the lingula (figure 1). An ultrasound of the abdomen revealed no pathologies. Blood and citrate blood cultures were negative. Serology tests for hepatitis A/B, Epstein-Barr virus, cytomegalovirus and Varicella-Zoster virus indicated past infection; hepatitis C virus RNA was negative. Antibodies against Brucella and Coxiella burnetii could not be found. The syphilis serology was positive with Treponema pallidum haemagglutination assay (TPHA) of 1:40 960 and venereal disease research laboratory (VDRL) 1:32, it had been negative 1 year earlier. Owing to slight paraesthesia of the right hand and the HIV infection, a lumbar puncture was performed, which revealed no evidence of neurosyphilis. The TPHA cerebrospinal fluid/serum index was negative. During treatment with benzathine penicillin 1×2.4 Mio U per week by intramuscular injection for 3 weeks, the subjective symptoms declined, the liver values returned to normal, VDRL declined and the aetiologically unclear opacity in the lingula was reduced in size (figure 2). Partner treatment for syphilis was performed.
Figure 1.

Thorax CT scan 31 May: wedge-shaped mass lesion in the lingual.
Figure 2.
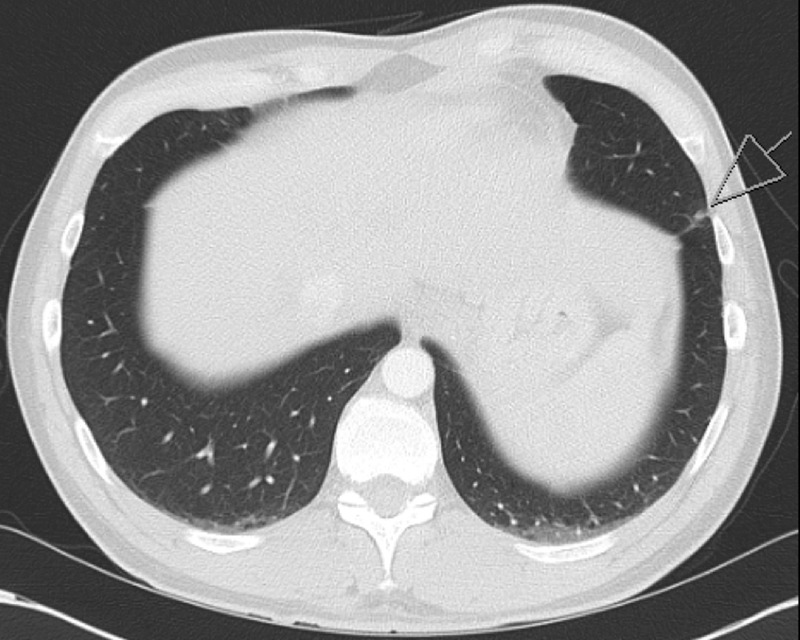
Thorax CT scan 29 September: regredient mass lesion in the lingula.
Two months later, the patient reported increasing headaches. MRI of the brain revealed a mass lesion (figure 3), and because of suspected glioma/glioblastoma the lesion was removed by osteoclastic craniotomy. The histology provided no evidence of neoplasia, but indicated an abscessed process without caseation with epithelioid cell macrophages and plasma cells without evidence of a pathogen despite processing with special dyes and immunohistochemistry. T. pallidum was established using eubacterial PCR. There was also an increase in the TPHA and VDRL. Table 1 shows the TPHA/VDRL progress with therapy details. There were no psychiatric or neurological symptoms such as insomnia, mood disorders, memory impairment, disorientation, psychosis, hearing loss or paralysis of the cranial nerves evident before, during or after treatment except a slight paraesthesia in the right hand after playing play-station for some hours.
Figure 3.
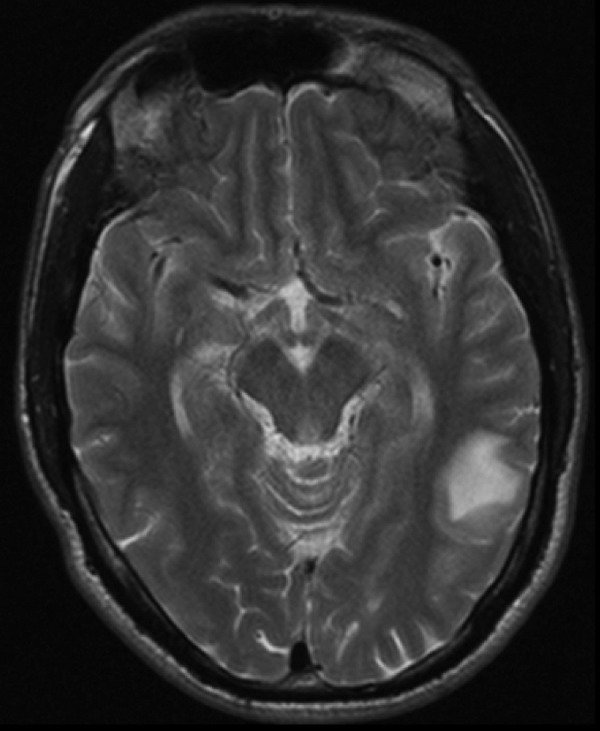
Brain MRI 1 October: mass lesion measuring 28×20×22 mm in the left parietal lobe.
Table 1.
The course of TPHA/VDRL
| 08-05-2007 | 02-06-2008 | 17-09-2008 | 10-10-2008 | 19-12-2008 | 14-07-2009 | |
|---|---|---|---|---|---|---|
| TPHA | 1:<80 | 1:20 480 | 1:640 | 1:40 960 | 1:5120 | 1:320 |
| VDRL | 1:64 | 1:2 | 1:32 | 1:4 | 1:<2 | |
| Treatment | Tardocillin by intramuscular injection | Penicillin by intravenous injection | ||||
TPHA, Treponema pallidum haemagglutination assay; VDRL, venereal disease research laboratory.
Treatment
Intravenous treatment with penicillin G 6×4 Mio U/day for 14 days was administered. The symptoms regressed completely, TPHA and VDRL titres decreased and the pulmonary and cerebral lesions could no longer be detected.
Discussion
To the best of our knowledge, this is one of the first reported episodes of secondary syphilis with skin exanthema affecting the lungs and liver. Secondary syphilis affecting the liver is present in about 25% of patients. Involvement of the lungs is recorded very rarely. In recent years, only nine cases have been recorded in the literature between 1965 and 2006.1 Pulmonary lesions can appear as bilateral infiltrates, solitary or multiple subpleural nodules, pleural effusion or lymphadenopathy.1 For the diagnosis, Coleman et al2 propose the following clinical criteria: (1) historical and physical findings typical of secondary syphilis; (2) serological test results positive for syphilis; (3) pulmonary abnormalities seen radiographically with or without associated symptoms or signs; (4) exclusion of other forms of pulmonary disease, when possible, according to findings of serological tests, sputum smears and cultures, and cytological examination of sputum; and (5) response to antisyphilis therapy of signs found by radiological examination. In our case all points except the exclusion of other forms of pulmonary disease were positive. Owing to the HIV infection, a more aggressive diagnostic method could have been performed by examination of the sputum, bronchoalveolar lavage and lung biopsy to rule out other infection due to Mycobacterium spp, Nocardia, Aspergillus and Pneumocystis jirovecii, and to exclude tumour and systemic diseases. It appears that pulmonary syphilis is often associated with other extracutaneous localisations and hepatic involvement, as was seen in our patient. A good clinical and radiological response to penicillin therapy relies on its narrow spectrum and is an important diagnostic tool.2
Cerebral syphilitic gummata are rare manifestations of tertiary syphilis. Cases of cerebral gummata are declining considerably due to improved diagnostics leading to earlier treatment compared with the 19th and 20th centuries. Fargen et al3 describe in their review how, in a series of 4000 test cases with syphilis in the 19th century, the incidence was so high that patients with symptoms of an intracranial tumour were first treated for syphilis and a brain tumour was only assumed after there was no response to this treatment.4 The proportion of syphilitic gummata among operated brain tumours in the last published series by Oblu et al5 in 1970 was only 0.1%. Syphilitic gummata are granulomatous lesions that can form in any organ. Central nervous gummata are predominantly located in the convex portion of the human brain.3 Usually, a cerebral gumma occurs on average 15 years after the primary infection. The time frame of less than half a year in the case of our patient was exceptionally short. It is suggested in the review of Lynn and Lightman6 that HIV accelerates and changes the clinical course of neurosyphilis and that co-infection with HIV increases the incidence of neurological complications of syphilis. Aggressive neurosyphilis can occur with either high or low CD4+ lymphocyte counts, because intact cell-mediated immune response is probably critical for the control of T. pallidum infection. Subtle functional T cell deficits are seen even in early HIV infection. This may be one of the reasons for the atypical presentation in our patient.
As in our case, TPHA and VDRL titres in the serum are usually positive at the time of diagnosis of cerebral syphilitic gummata, but often negative in the cerebrospinal fluid.
It is not possible, even today, to diagnose a cerebral syphilitic gumma non-invasively; empiric “ex juvantibus” treatment against syphilis in the face of a cerebral tumour is not indicated nowadays given the rarity of this clinical manifestation. Our case shows that syphilis continues to be the great imitator, the ‘chameleon’ in clinical medicine, and should be included in the differential diagnosis of cerebral and pulmonary mass lesions and hepatitis in patients with risk of attracting sexually transmitted diseases.
Learning points.
Syphilis continues to be the great imitator, the ‘chameleon’ in clinical medicine.
Syphilis should be included in the differential diagnosis of hepatitis, cerebral and pulmonary mass lesions, and in patients with risk of attracting sexually transmitted diseases.
Treponema pallidum haemagglutination assay and venereal disease research laboratory titres in the serum are usually positive at the time of diagnosis of cerebral syphilitic gummata, but often negative in the cerebrospinal fluid.
Syphilitic brain gummata can develop within a few months.
Footnotes
Contributors: Authors KS and HF have both substantially contributed to the conception of the work and the acquisition and interpretation of data. KS has drafted the work and HF has revised it critically. KS and HF approved the final version to be published.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.David G, Perpoint T, Boibieux A et al. Secondary pulmonary syphilis: report of a likely case and literature review. Clin Infect Dis 2006;42:e11–15. [DOI] [PubMed] [Google Scholar]
- 2.Coleman DL, Mcphee SJ, Ross TF et al. Secondary syphilis with pulmonary involvement. West J Med 1983;138:875–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Fargen KM, Alvernia JE, Lin CS et al. Cerebral syphilitic gummata: a case presentation and analysis of 156 reported cases. Neurosurgery 2009;64:568–75. [DOI] [PubMed] [Google Scholar]
- 4.Merritt HH, Adams RD, Solomon HC. Neurosyphilis. New York: Oxford University Press, 1946. [Google Scholar]
- 5.Oblu N, Stanciu A, Sandulescu G et al. Cerebral syphilitic gumma. 3 cases reports. Neurochirurgie 1970;16:249–58. [PubMed] [Google Scholar]
- 6.Lynn WA, Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis 2004;4:456–6. [DOI] [PubMed] [Google Scholar]


