Abstract
A 28-year-old woman presenting with fever was referred to our hospital and diagnosed as septic pulmonary embolism secondary to tricuspid valve endocarditis. Although antibiotic therapy was initiated, she further showed multiple complications including Janeway lesions and cerebral infarctions, suggestive of septic systemic embolism. Transoesophageal echocardiography detected a right-to-left shunt through a patent foramen ovale (PFO). The patient was successfully treated with surgical tricuspid valvuloplasty and PFO closure. Paradoxical systemic embolism may occur in patients with septic pulmonary embolism through the PFO.
Background
Paradoxical embolism may occur via interventricular, interatrial or pulmonary arteriovenous malformations. It can cause systemic embolic complications including cerebrovascular events.1 We present a rare case with right-sided infective endocarditis showing pulmonary and systemic embolism due to right-to-left shunting through the patent foramen ovale (PFO). Transoesophageal echocardiography was helpful to detect the PFO.
Case presentation
A 28-year-old woman presenting with fever, polyarthralgia and general malaise after the onset of purulent paronychia was referred to our department. The patient had no significant medical history except for subclinical hepatitis C virus infection. At the time of admission, she had a temperature of 38.8°C, sinus tachycardia (pulse rate 130 bpm) and hypoxia (oxygen saturation on room air, 86%). The physical examination was notable for hepatosplenomegaly and polyarticular tenderness. Heart and breath sounds were normal on auscultation.
Investigations
Laboratory examination revealed elevations in the white cell count (17 380/μL), C reactive protein (23.5 mg/dL) and D-dimer (53.7 μg/mL), as well as a low platelet cell count (25 000/μL). Blood cultures were positive for methicillin-sensitive Staphylococcus aureus, suggestive of sepsis with disseminated intravascular coagulation. Chest radiograph (figure 1A) and CT scan (figure 1B) revealed a right pleural effusion and multiple cavitary nodules in both lungs. Transthoracic echocardiography revealed a tricuspid valve vegetation and regurgitation (figure 1C).
Figure 1.
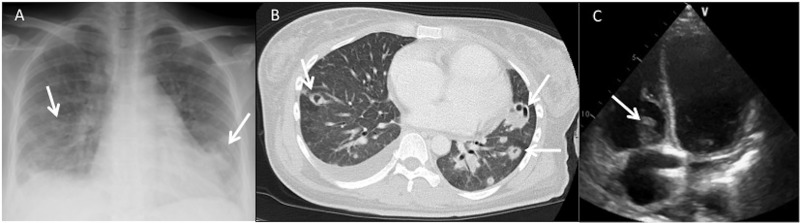
Chest radiograph (A) and CT scans (B) showing multiple bilateral cavitary lung nodules (arrows). (C) Transthoracic echocardiography demonstrating vegetation on the tricuspid valve (arrow).
Differential diagnosis
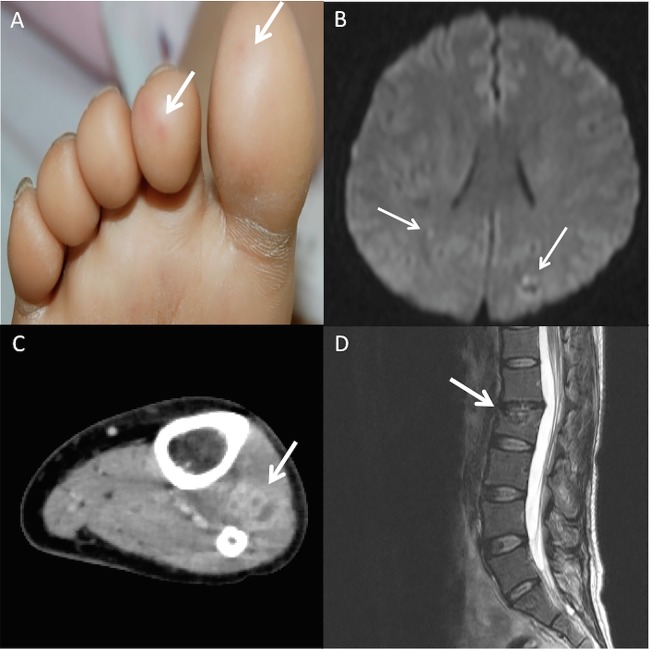
We diagnosed septic pulmonary embolism (SPE) secondary to infective endocarditis of the tricuspid valve, and initiated intravenous antibiotic therapy. However, the patient subsequently had multiple complications including Janeway lesions (figure 2A), cerebral infarctions (figure 2B), gastrocnemius muscle abscess (figure 2C) and infectious spondylitis (figure 2D), suggestive of septic systemic embolism. Transoesophageal echocardiography was then performed, and it revealed no vegetation on the mitral valve but detected a right-to-left shunt through a PFO (figure 3). The conclusive diagnosis was tricuspid endocarditis causing SPE and systemic emboli due to right-to-left shunting across the PFO.
Figure 2.
(A) Janeway lesions on the sole of the right foot (arrows). (B) Multiple infarctions were detected on brain MRI (arrows). (C) An abscess of the gastrocnemius muscle was detected on lower extremity of CT scan (arrow). (D) MRI of the spine suggested infectious spondylitis (arrow).
Figure 3.
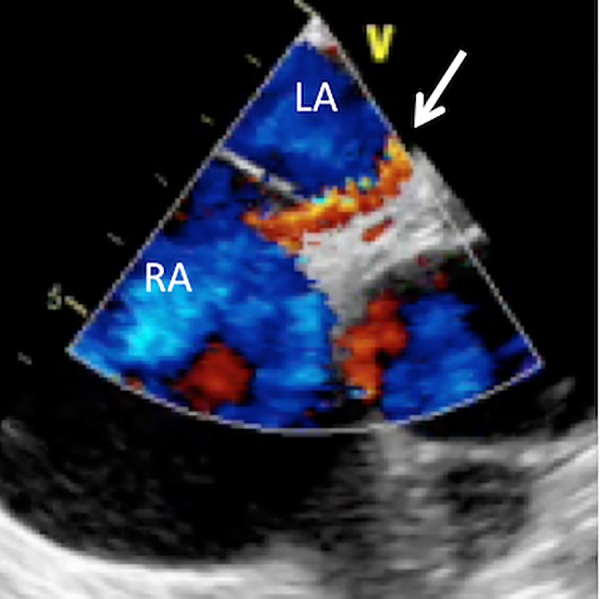
Transoesophageal colour Doppler echocardiography showing right-to-left shunting through a patent foramen ovale (arrow).
Treatment
The patient was successfully treated with continuous antibiotic therapy, surgical tricuspid valvuloplasty and PFO closure.
Outcome and follow-up
The postoperative period remained uneventful. The patient is doing well at 1-year follow-up after surgery, and showing no signs of recurrence.
Discussion
SPE is an uncommon disorder that presents with fever, respiratory symptoms and lung infiltrates. It is associated with right-sided infective endocarditis, pelvic thrombophlebitis and suppurative head and neck infections. In SPE, embolic blood clots leading to pulmonary infarction also contain microorganisms that incite a focal abscess. Microbiological studies using blood, pleural fluid and lung biopsy specimens can yield responsible pathogens; most common are staphylococcal species and Fusobacterium. Chest radiograph reveals poorly marginated peripheral lung nodules that have a tendency to cavitate, and chest CT scans are more helpful in demonstrating cavitary lesions.2
Paradoxical embolism, or venous thromboembolism transit from right-sided to left-sided cardiac chambers may occur via interventricular, interatrial or pulmonary arteriovenous malformations. It can cause systemic embolic complications including cryptogenic stroke, and sudden onset of a cryptogenic stroke during pulmonary embolism is a suspicious clue for a paradoxical embolism. The most common cause is probably a PFO. In a meta-analysis of 23 case–control studies, the OR for a PFO in patients with cryptogenic stroke compared with those with stroke from a known cause was 2.9 (95% CI 2.1 to 4.0).1 3 A PFO is a haemodynamically insignificant interatrial communication that is present in 15–35% of the adult population according to autopsy studies.4 Although transient elevations of right atrial pressure can occur during a normal cardiac cycle, more consistent elevations increase the likelihood of right-to-left shunting.5 Diagnostic techniques for PFOs are based on direct visualisation of the right-to-left shunt. Transoesophageal echocardiography has higher sensitivity than transthoracic echocardiography and is considered the gold standard for PFO detection. Its sensitivity and specificity have been reported to be essentially 100%.4 In patients with a PFO with cryptogenic stroke, anticoagulation therapy or defect closure is recommended to prevent recurrent stroke.1 However, a recent randomised trial failed to show a greater benefit of percutaneous PFO closure when compared with medical therapy alone.6
Tricuspid valve endocarditis accounts for 5–10% of infective endocarditis.7 In patients with SPE who are suspected of having tricuspid valve endocarditis, echocardiography helps to diagnose valvular infection and to detect complications such as valvular insufficiency or dehiscence, congestive heart failure and paravalvular abscesses. A transoesophageal approach again provides greater spatial resolution compared with transthoracic echocardiography, and is a superior method for the diagnosis.2 Paradoxical embolism from tricuspid endocarditis is a rare and life-threatening condition that may cause cryptogenic stroke, brain abscess and peripheral embolism.3 As far as we know, there have been only three reports of paradoxical systemic embolism associated with tricuspid endocarditis in patients with PFO. One is of an intravenous heroin abuser who showed SPE and multiple splenic infarcts, which were resistant to antibiotic therapy. A PFO was detected during surgery, and was closed by direct suture.8 The second is a patient with systemic lupus erythematosus with Libman-Sacks endocarditis who developed splenic and cerebral infarctions. Transoesophageal echocardiography suggested the presence of a PFO, and the patient was successfully treated with transcatheter PFO closure and anticoagulation therapy.9 The third patient had a brain abscess, and transoesophageal echocardiography detected infective tricuspid endocarditis and PFO. This patient had a complete clinical recovery with brain surgery and intravenous antibiotic therapy.7 Similarly to the reported cases, transoesophageal colour Doppler echocardiography was helpful to detect the PFO, and successful treatment was achieved through PFO closure in our patient. In these patients, tricuspid regurgitation or pulmonary hypertension secondary to pulmonary embolism may have increased right atrial pressure, which promoted right-to-left shunting through the PFO.5 10 11 It remains uncertain if patients with tricuspid valve endocarditis and PFOs would benefit from defect closure, although it would prevent further embolic events and seeding. A randomised trial would be difficult due to the rarity of the condition in clinical practice.7
Learning points.
Paradoxical systemic embolism may occur in patients with septic pulmonary embolism (SPE) due to right-to-left shunting through a patent foramen ovale (PFO).
PFOs are present in 15–35% of the adult population, and transoesophageal echocardiography is the gold standard for PFO detection.
In patients with SPE complicated by systemic embolism, transoesophageal echocardiography should be performed to evaluate for a PFO.
Footnotes
Contributors: TN, HY and TO were involved in acquisition, analysis and interpretation of clinical information and data. IT prepared the manuscript and approved the final version.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Maron BA, Shekar PS, Goldhaber SZ. Paradoxical embolism. Circulation 2010;122:1968–72. [DOI] [PubMed] [Google Scholar]
- 2.Cook RJ, Ashton RW, Aughenbaugh GL et al. Septic pulmonary embolism: presenting features and clinical course of 14 patients. Chest 2005;128:162–6. [DOI] [PubMed] [Google Scholar]
- 3.Costa F, Carerj S, Cammaroto S et al. Concurrent pulmonary and cerebral embolism: is tricuspid valve endocarditis the culprit? Int J Cardiovasc Res 2013;2:2. [Google Scholar]
- 4.Homma S, Di Tullio MR. Patent foramen ovale and stroke. J Cardiol 2010;56:134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Homma S, Sacco RL. Patent foramen ovale and stroke. Circulation 2005;112:1063–72. [DOI] [PubMed] [Google Scholar]
- 6.Furlan AJ, Reisman M, Massaro J et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med 2012;366:991–9. [DOI] [PubMed] [Google Scholar]
- 7.Suero G, Varghese R, Shah M et al. Embolic brain abscess in a patient with tricuspid valve endocarditis and a patent foramen ovale. J Neurol Res 2012;2:123–6. [Google Scholar]
- 8.Caleb M, Shanker S, Agasthian T et al. Tricuspid endocarditis and paradoxical embolism. Asian Cardiovasc Thorac Ann 2001;9:132–4. [Google Scholar]
- 9.Zurick AO III, Yang EH, Chang PP et al. A 38-year-old Hispanic woman with paradoxical embolism and Libman-Sacks endocarditis involving the tricuspid valve. J Am Soc Echocardiogr 2007;20:1316 e5–7. [DOI] [PubMed] [Google Scholar]
- 10.Bier A, Jones J, Lazar E et al. Endocarditis of a tricuspid prosthesis causing valvular stenosis and shunting through a patent foramen ovale. Chest 1986;90:293–5. [DOI] [PubMed] [Google Scholar]
- 11.Johri AM, Kovacs KA, Kafka H. An unusual case of infective endocarditis: extension of a tricuspid valve vegetation into the left atrium through a patent foramen ovale. Can J Cardiol 2009;25:429–31. [DOI] [PMC free article] [PubMed] [Google Scholar]