Abstract
A 6-year-old Thai girl presented with itching, redness and copious discharge in both eyes. Slit-lamp biomicroscopy of the left eye revealed cobblestone papillae with marked ptosis while in the right eye only small papillae were observed. Punctuate epithelial keratitis was noted only in the left eye. There were no associated factors for giant papillary conjunctivitis (ie, suture or contact lens). The cobblestone papillae in the left eye persisted after maximal topical and oral antiallergic medications. Two doses of supratarsal corticosteroid (20 mg of triamcinolone acetonide) injection without any topical or oral antiallergic medications were undertaken in the left eye 1 month apart. Cobblestone papillae and punctate epithelial erosion (including allergic symptoms) were completely recovered. There was no recurrence after 18 months of follow-up. This case report indicates that using supratarsal corticosteroid injection by itself in recalcitrant vernal keratoconjunctivitis provides promising results.
Background
Vernal keratoconjunctivitis (VKC) is a chronic conjunctival inflammatory condition predisposed to atopic disease. Generally, most cases are bilateral with symmetrical involvement.1 Asymmetrical involvement can, however, be found and unilateral cases are uncommon.1 2 3
Giant papillae or ‘cobblestone’ papillae at the upper tarsal conjunctiva is one of the most common findings in VKC. Treatments of choice for reducing papillae include topical medications (ie, antihistamines, mast cell stabilisers, corticosteroids, cyclosporine A and tacrolimus) and/or oral medications (ie, antihistamines and corticosteroids) as well as immunotherapy for recalcitrant cases.1 In case of failure to respond to these medications, supratarsal corticosteroid injection has been reported. Partial improvement with possible recurrence was observed. We report a paediatric patient with asymmetrical VKC successfully treated with two doses of supratarsal corticosteroid injection after failure of topical as well as oral medications.1–3
Case presentation
A 6-year-old Thai girl presented after 2 months of itching, foreign body sensation, copious discharge and ptosis in the left eye. Her best corrected visual acuity was 20/20 in the right eye and 20/40 in the left. Slit-lamp biomicroscopy of the left eye revealed bulbar conjunctival redness, mucous discharge and giant (cobblestone) papillae at the upper tarsal conjunctiva with superficial punctuate keratitis (figure 1A). There was a mild papillary reaction without corneal involvement in the right eye (figure 1B). She had no history of wearing contact lenses, having an ocular prosthesis or undergoing ocular surgery (eg, glaucoma filtering surgery or sclera buckles).
Figure 1.
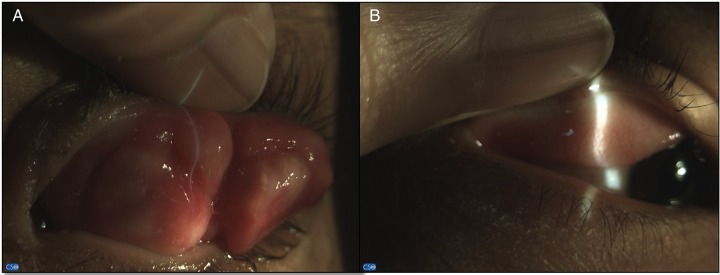
Slit-lamp photograph of eyelids with eversion showing cobblestone papillae in the left eye (A) and fine papillae in the right eye (B).
Investigations
Since the papillae were relatively large and recalcitrant to all medications, incisional biopsy of the tarsal conjunctiva was undertaken to rule out a conjunctival tumour. The pathological examination revealed fibrovascular tissue with infiltration of eosinophils and other chronic inflammatory cells.
Treatment
For the first 2 months, both eyes were treated four times a day with topical mast cell stabiliser (sodium cromoglycate) and the left eye was additionally treated with a potent topical corticosteroid (prednisolone acetate 1%) four times a day. The symptoms as well as the papillary reaction in the right eye improved markedly; however, the cobblestone papillae and punctate corneal erosion (including ocular itching in the left eye) persisted. The ketotifen fumarate 0.025% eye drops were therefore prescribed instead of the sodium cromoglycate and the frequency of topical prednisolone acetate was increased to six times a day. The symptoms, however, worsened.
A 20 mg injection of supratarsal triamcinolone acetonide was scheduled for the left eye. Supratarsal injections in small children are difficult to administer without sedation and thus general anaesthesia was chosen in this patient. After the injection, the size of the cobblestone papillae significantly decreased. Since some residual papillae remained, a further supratarsal steroid injection was performed.
Outcome and follow-up
Two months later, the cobblestone papillae and punctate epithelial erosion (including allergic symptoms) were completely alleviated (figure 2). There was no further recurrence during 18 months of follow-up. The intraocular pressures—measured by Goldmann tonometry—were not elevated; and no other ocular side effects were detected. After the supratarsal steroid injection, only antibiotics without any antiallergic eye-drops were prescribed and used for 1 week.
Figure 2.
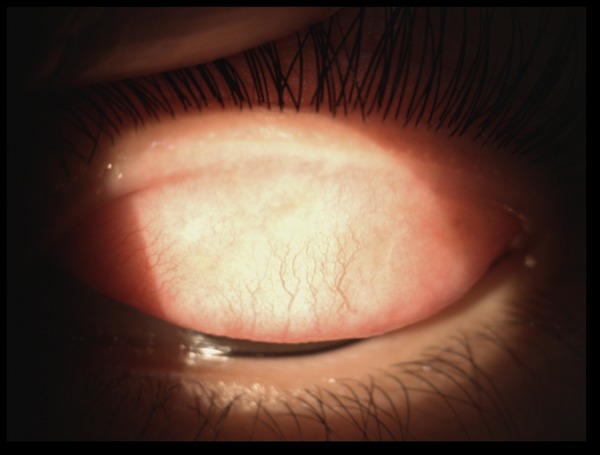
Slit-lamp photograph of eyelid with eversion showing complete recovery in the left eye.
Discussion
Generally, VKC is a chronic bilateral and symmetrical disease. Since asymmetrical involvement is rare, giant papillary conjunctivitis (GPC), which induces similar conjunctival changes as VKC, should be excluded.4 GPC is not a true ocular allergy; instead, the main cause is a consequence of repetitive microtrauma or irritative event(s) (ie, from sutures, contact lenses or ocular prostheses).4 5 Owing to the extremely large, giant (cobblestone-like) papillae we found, and significant corneal involvement with no history of irritative stimuli, VKC was the most likely cause in our patient.
Conjunctival tumours can simulate allergic conjunctivitis. Lymphoid tissue from conjunctival lymphoma may sometimes be misdiagnosed as giant papillae.6 7 Should the condition be unresponsive to antiallergic drugs and if the papillae are relatively large, a conjunctival tumour should be included in the differential diagnosis. Incisional biopsy was, therefore, undertaken in our case but was negative and allergic conjunctivitis was approved as the diagnosis.
Pharmacological therapy is the main treatment of all types of allergic conjunctivitis. For VKC, such therapy can be palliative but may not eliminate the disease. Recurrence can occur when the medications are withdrawn.1 4 In severe cases with giant papillae unresponsive to medical therapy, surgical management (ie, excision of the papillae or cryotherapy) often gives only a transient response,8–10 but if combined with amniotic membrane transplantation, better results have been reported.11
Supratarsal corticosteroid injection has been found to be an effective and relatively safe treatment for refractory VKC.12–15 Either short-acting dexamethasone or intermediate-acting triamcinolone are equally effective with a low risk of increased intraocular pressure.12 13 In support of such an approach, previous studies have reported a ≥50% decrease in papillae size with complete healing of a shield ulcer.12 15 Injections are repeated when the disease recurs or is recalcitrant.15 In our patient, after two injected doses, there was a 100% decrease in papillae and the corneal erosion was totally healed. Most antiallergic drugs were maintained after surgery, as in prior reports; however, other medications may not be required after the two doses of injection as in our case. Furthermore, most studies proposed partial response and recurrence after injection.13–15 In the present observation, there was a complete recovery without recurrence after two doses of injection.
Supratarsal corticosteroid injection is an effective choice of treatment for refractory VKC. Significant improvement without any long-term medications has been observed.
Learning points.
The associated risk factors for giant papillary conjunctivitis should be excluded before diagnosis of vernal keratoconjunctivitis (VKC).
Although the adverse effects of corticosteroid were not detected in the present study, they should be monitored for meticulously.
This case shows the benefits of supratarsal corticosteroid injection for refractory VKC without any other medications.
Acknowledgments
The authors thank the patient for her permission; the Department of Ophthalmology and the Faculty of Medicine for their support and Mr Bryan Roderick Hamman and Mrs Janice Loewen-Hamman for assistance with the English-language presentation of the manuscript.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kumar S. Vernal keratoconjunctivitis: a major review. Acta Ophthalmol 2009;87:133–47. [DOI] [PubMed] [Google Scholar]
- 2.Keklikci U, Soker SI, Soker Cakmak S et al. Unilateral vernal keratoconjunctivitis: a case report. Eur J Ophthalmol 2007;17:973–5. [DOI] [PubMed] [Google Scholar]
- 3.Awwad ST, Najjar DM, Arlette A et al. Vernal keratoconjunctivitis presenting unilaterally. J Pediatr Ophthalmol Strabismus 2006;43:179–80. [DOI] [PubMed] [Google Scholar]
- 4.Friedlaender MH. Ocular allergy. Curr Opin Allergy Clin Immunol 2011;11: 477–82. [DOI] [PubMed] [Google Scholar]
- 5.La Rosa M, Lionetti E, Reibaldi M et al. Allergic conjunctivitis: a comprehensive review of the literature. Ital J Pediatr 2013;39:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee DH, Sohn HW, Park SH et al. Bilateral conjunctival mucosa-associated lymphoid tissue lymphoma misdiagnosed as allergic conjunctivitis. Cornea 2001;20:427–9. [DOI] [PubMed] [Google Scholar]
- 7.Strauss EC, Warren JF, Margolis TP et al. Diagnosis of conjunctival B-cell lymphoma by polymerase chain reaction heteroduplex analysis. Am J Ophthalmol 2003;136:207–9. [DOI] [PubMed] [Google Scholar]
- 8.Diallo JS. Tropical endemic limboconjunctivitis. Rev Int Trach Pathol Ocul Trop Subtrop 1976;53:71–80. [PubMed] [Google Scholar]
- 9.Khan MD, Kundi N, Saeed N. A study of 530 cases of vernal conjunctivitis from the North Western Frontier Province of Pakistan. Pak J Ophthalmol 1986;2:111–14. [Google Scholar]
- 10.Resnikoff S, Cornand G, Filliard G et al. Limbal vernal keratoconjunctivitis in the tropics. Rev Int Trach Pathol Ocul Trop Subtrop Sante Publique 1988;65:21–72. [PubMed] [Google Scholar]
- 11.Guo P, Kheirkhah A, Zhou WW et al. Surgical resection and amniotic membrane transplantation for treatment of refractory giant papillae in vernal keratoconjunctivitis. Cornea 2013;32:816–20. [DOI] [PubMed] [Google Scholar]
- 12.Saini JS, Gupta A, Pandey SK et al. Efficacy of supratarsal dexamethasone versus triamcinolone injection in recalcitrant vernal keratoconjunctivitis. Acta Ophthalmol Scand 1999;77:515–18. [DOI] [PubMed] [Google Scholar]
- 13.Holsclaw DS, Whitcher JP, Wong IG et al. Supratarsal injection of corticosteroid in the treatment of refractory vernal keratoconjunctivitis. Am J Ophthalmol 1996;121:243–9. [DOI] [PubMed] [Google Scholar]
- 14.Singh S, Pal V, Dhull CS. Supratarsal injection of corticosteroids in the treatment of refractory vernal keratoconjunctivitis. Indian J Ophthalmol 2001;49:241–5. [PubMed] [Google Scholar]
- 15.Zaouali S, Kahloun R, Attia S et al. Supratarsal injection of triamcinolone acetonide and childhood allergic keratoconjunctivitis. Int Ophthalmol 2012;32:99–106. [DOI] [PubMed] [Google Scholar]


