Abstract
Pseudoaneurysm of the cystic artery is a rare cause of haemobilia resulting from either an inflammatory process in the abdomen or abdominal trauma. We report a case of a patient with chronic calculous cholecystitis associated with a pseudoaneurysm arising from an anomalous cystic artery who presented with haemobilia. The patient was managed successfully with multimodality treatment that included angioembolisation of the pseudoaneurysm and stenting of the common bile duct to relieve jaundice followed by elective open cholecystectomy.
Background
Gastrointestinal bleeding from the biliary tree (haemobilia) is an uncommon event. Previously, the most common cause of this disease was traumatic hepatobiliary injury, however, iatrogenic trauma caused by percutaneous and endoscopic hepatobiliary procedures is now the cause in two-third of haemobilia cases.1 Other causes are gallstones, inflammatory diseases, vascular malformations and neoplastic disease.1 These aneurysms can be either congenital or acquired. Pseudoaneurysms due to cholecystitis are very rare. We report a rare case of haemobilia due to a pseudoaneurysm of an anomalous cystic artery secondary to chronic calculus cholecystitis with Mirrizi's syndrome.
Case presentation
A 55-year-old man presented to the emergency department of our tertiary referral hospital with a 4-month history of repeated episodes of jaundice, right upper abdominal pain and malena. One year earlier the patient had been diagnosed with gall stones. On clinical examination the patient was pale and icteric, with no significant abdominal signs. Per rectal examination revealed malena.
Investigations
Blood investigations showed anaemia with direct hyperbilirubinaemia. Abdominal ultrasound revealed gallstones with mild central intrahepatic biliary radicle dilation.
The contrast-enhanced CT of the abdomen showed a pseudoaneurysm arising from the medial aspect of the gallbladder wall with a mass suspected to be a stone in the gallbladder (figure 1).
Figure 1.
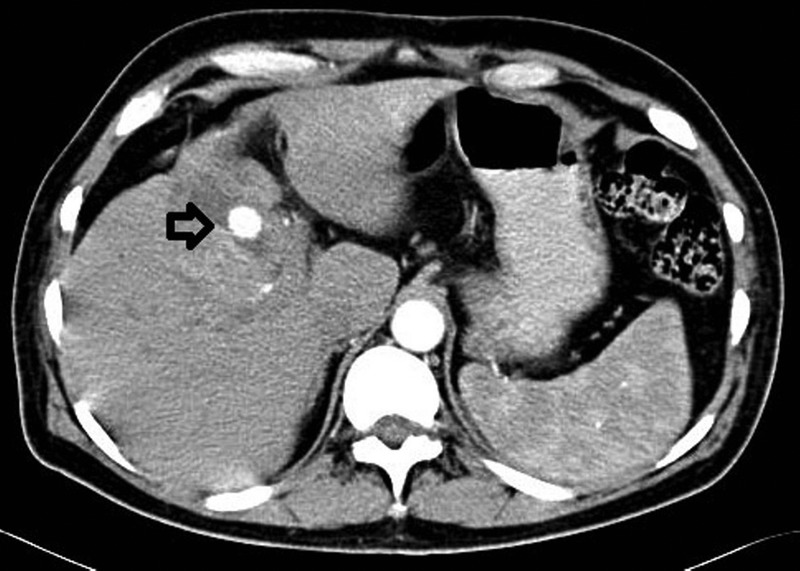
CT angiography showing cystic artery pseudoaneurysm arising from the gallbladder wall.
MR cholangiography revealed a pseudoaneurysm of the cystic artery (figure 2A,B) with blood clots, a stone within the gallbladder and type I Mirrizi’s syndrome (figure 2C). The cystic artery bearing the pseudoaneurysm was found to originate directly from the common hepatic artery on selective hepatic catheterisation (figure 3A). Early branching of the left hepatic artery from the common hepatic artery was also seen (figure 3A).
Figure 2.

MR angiography of the abdomen (A) cystic artery pseudoaneurysm on axial images, (B) cystic artery pseudoaneurysm on sagittal images, (C) MR cholangiopancreatography showing mid-common bile duct narrowing with intrahepatic biliary radical dilatations.
Figure 3.
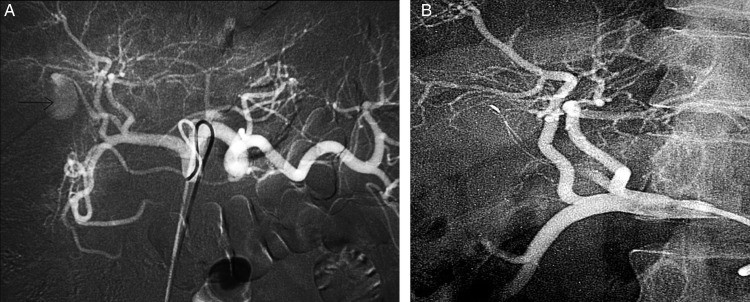
Digital subtraction angiography (A) before embolisation showing anomalous cystic artery with pseudoaneurysm at its tip, (B) after embolisation.
Differential diagnosis
Cholelithiasis with choledocholithiasis
Mirrizi's syndrome
Hepatic artery pseudoaneurysm
Treatment
Super selective catheterisation with microcoil embolisation of the anomalous cystic artery was performed resulting in occlusion of the pseudoaneurysm (figure 3B).
Endoscopic retrograde cholangiography (ERC) was performed for direct hyperbilirubinaemia. On ERC, there was passage of blood clots from the ampulla of Vater with extrinsic compression on the mid-portion of the common bile duct (CBD) without any filling defects. CBD stenting was performed to relieve jaundice.
Six days later the patient underwent elective open subtotal cholecystectomy with under-running of the cystic artery pseudoaneurysm. Intraoperatively, the gallbladder was thickened, distended and intrahepatic, and contained pus; it also contained a single large stone. There were dense adhesions in Calot's triangle. An ovoid vascular lesion was found projecting into the lumen of the gallbladder from the posterosuperior wall of its body (figure 4). The gallbladder wall around it was left behind as it was densely adhered to the liver.
Figure 4.
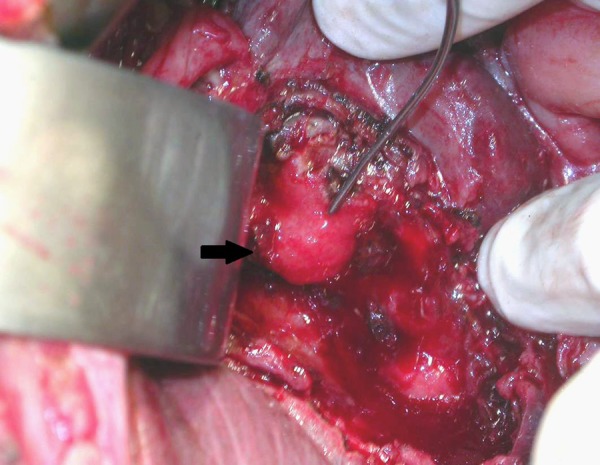
Intraoperative photograph of pseudoaneurysm during open cholecystectomy.
Outcome and follow-up
The patient had an uneventful postoperative recovery with regression of symptoms including jaundice and malena. Histopathology revealed acute on chronic cholecystitis. On follow-up after 2 years he was operated for an inguinal hernia and since then he has been asymptomatic.
Discussion
The association of upper gastrointestinal bleeding with signs of biliary disorders should suggest haemobilia. Haemobilia is usually associated with Quincke's triad of biliary colic (occurring in 70% of patients), jaundice (exhibited in 60% of cases) and gastrointestinal bleeding, which is present in all patients. The complete classic triad is found in about 22% of patients1 with acute bleeding first causing biliary colic followed by haematemesis or malena, which in turn leads to pain relief.
A cystic artery pseudoaneurysm due to an inflammatory process is a rare cause of haemobilia; an extensive search identified only 58 published cases (table 1).
Table 1.
Summary of cases of cystic artery pseudoaneurysm secondary to inflammation reported in literature
| Serial number | Author | Year | Journal | Aetiology | Presentation | Management |
|---|---|---|---|---|---|---|
| 1 | Glaysher et al | 2014 | International Journal of Surgery Case Reports | Calculous cholecystitis with cholecystoenteric fistula | Jaundice+pain+malena | Open subtotal cholecystectomy |
| 2 | Suzuki et al | 2013 | Clinical Journal of Gastroenterology | Acute calculous cholecystitis | Epigastric pain+jaundice | Open cholecystectomy |
| 3 | Nana et al | 2013 | International Journal of Surgery Case Reports | Acute cholecystitis | Quinke triad | TAE+lap cholecystectomy |
| Acute cholecystitis | Haemobilia+pain | TAE | ||||
| 4 | Fung et al | 2013 | Scottish Medical Journal | Acute cholecystitis | Haemobilia | – |
| 5 | Dewachter et al | 2012 | Journal Belge de Radiologie - Belgisch Tijdschrift voor Radiologi | Acute calculous cholecystitis | Epigastric pain+nausea | Lap cholecystectomy+resection of pseudoaneurysm |
| 6 | Chong et al | 2012 | Canadian Association of Radiologists Journal | – | Fever+epigastric pain+vomiting | – |
| 7 | Komatsu et al | 2011 | Journal of Medical Cases | Acute calculous cholecystitis | Epigastic pain+haematemesis+malena | TAE |
| 8 | Anand et al | 2011 | Annals of Gastroenterology | Idiopathic | RUQ pain+haematemesis+malena | Cholecystectomy |
| 9 | Nkwam et al | 2010 | Journal of Surgical Case Reports | Acute calculous cholecystitis | RHC pain | TAE |
| 10 | Desai et al | 2010 | Radiology Case | Chronic calculous cholecystitis | Epigastic pain+malena | TAE |
| 11 | Ahmed et al | 2010 | The British Journal of Radiology | Xanthogranulomatous cholecystitis | RHC pain+lump | TAE+open cholecystectomy |
| 12 | Leung et al | 2010 | Hong Kong Medical Journal | Acute cholecystitis | Haematochezia | TAE |
| 13 | Hague et al | 2010 | CardioVascular and Interventional Radiology | Acute calculous cholecystitis | RHC pain | TAE |
| Acute calculous cholecystitis | RHC pain | TAE | ||||
| – | Epigastric pain+malena | TAE | ||||
| 14 | Siddique et al | 2011 | BMJ Case Reports | Acute xanthogranulomatous cholecystitis | Epigastric pain+fever | TAE+elective open cholecystectomy |
| 15 | Mullen et al | 2009 | CardioVascular and Interventional Radiology | Acute calculous cholecystitis | RHC pain+malena | TAE |
| Acute calculous cholecystitis | RHC pain | TAE | ||||
| 16 | Sousa et al | 2009 | Gastroentérologie Clinique et Biologique | Acute calculous cholecystitis | Epigastric pain+haematemesis | Cholecystectomy |
| 17 | Radouane et al | 2008 | Journal of Radiology | Calculous cholecystitis | Not known | |
| 18 | Machida et al | 2008 | Radiation Medicine | Acute calculus cholecystitis | RUQ pain | Cholecystectomy |
| 19 | Al’ Aref et al | 2008 | Hepatobiliary & Pancreatic Diseases International | Idiopathic | RUQ pain+malena | TAE |
| 20 | Shimada et al | 2008 | Digestive Surgery | Xanthogranulomatous cholecystitis | Jaundice | TAE—extended right hepatectomy |
| 21 | Ghoz et al | 2007 | Hepatobiliary & Pancreatic Diseases International | Acute on chronic cholecystitis | Abdominal pain+haematemesis | TAE+cholecystectomy |
| 22 | Akatsu et al | 2007 | Surgery Today | Acute cholecystitis | RUQ pain+jaundice | Cholecystectomy |
| 23 | Saluja et al | 2007 | BMC Gastroenterology | Acute calculus cholecystitis | Haematemesis+Malena | TAE+partial cholecystectomy |
| 24 | Chun-Jung Lin et al | 2007 | Chinese Journal of Radiology | Acalculous cholecystitis | Joundice+abdominal pain | TAE+cholecystectomy |
| 25 | Pérez-Castrillón et al | 2006 | Endoscopy | Acute cholecystitis | Abdominal pain+anaemia | TAE |
| 26 | Lee | 2006 | Clinical Radiology | Chronic cholecystitis | Lower GI bleed | Not known |
| 27 | Sibulesky et al | 2006 | American Journal of Surgery | Calculous cholecystitis | RHC pain+malena | Open cholecystectomy |
| 28 | Joyce et al | 2006 | Irish Journal of Medical Sciences | Acute on chronic cholecystitis | Haemobilia | Cholecystectomy |
| 29 | Oueslati et al | 2005 | Journal de Chirurgie | Idiopathic | Haemobilia | Cholecystectomy |
| 30 | Morioka et al | 2004 | Journal of Gastroenterology & Hepatology | Chronic calculus cholecystitis | Haemobilia | Cholecystectomy |
| 31 | Gutierrez et al | 2004 | American Journal of Surgery | Acute calculus cholecystitis | RHC pain+malena | TAE failed f/b open cholecystectomy |
| 32 | Hiroshi et al | 2002 | Journal of Biliary Tract Pancreas | Dyspnoea+malena | TAE | |
| 33 | Maeda et al | 2002 | Journal of Hepato-Biliary-Pancreatic Surgery | Calculous cholecystitis | Epigastric pain+jaundice | TAE+elective open cholecystectomy |
| 34 | AA Palejwala et al | 2000 | CME Journal Gastroenterology, Hepatology and Nutrition | Acute cholecystits | RUQ pain+haematemesis+jaundice | Cholecystectomy |
| 35 | Delgadillo et al | 1999 | Journal of Vascular & Interventional Radiology | Acute pancreatitis | Haemobilia | TAE |
| 36 | dePerrot et al | 1999 | The British Journal of Surgery | Pancreatitis | Epigastric pain | Surgery |
| 37 | Kaman et al | 1998 | American Journal of Gastroenterology | Acute calculous cholecystitis | Haemobilia | Cholecystectomy with ligation of pseudoaneurysm |
| 38 | Kirchgatterer et al | 1998 | Wiener Klinische Wochenschrift | Chronic calculous cholecystitis | Haemobilia | Cholecystectomy |
| 39 | England et al | 1998 | Clinical Radiology | Acute calculous cholecystitis | Haemobilia | Open cholecystectomy f/b TAE |
| 40 | Miura et al | 1998 | Nippon Shokakibyo Gakkai Zasshi | – | Haemobilia | – |
| 41 | Ritz et al | 1997 | Journal de Chirurgie | Acute calculous cholecystitis | Haemobilia | Cholecystectomy |
| 42 | Matsuba et al | 1996 | Japanese Journal of Gastroenterology Surgery | Cholecystitis | RUQ pain | Cholecystectomy |
| 43 | Nakajima et al | 1996 | Journal of Gastroenterology | Acute calculous cholecystitis | Haemobilia | Cholecystectomy |
| 44 | Barba et al | 1994 | Canadian Journal of Surgery | Cholecystitis | Haemobilia | Cholecystectomy with ligation of pseudoaneurysm |
| 45 | Read et al | 1991 | ANZ Journal of Surgery | Cholecystitis | Haemobilia | Cholecystectomy |
| 46 | Strickland et al | 1991 | CardioVascular and Interventional Radiology | Calculous cholecystitis | Haemobilia | – |
| 47 | Smague et al | 1990 | Journal de Chirurgie | Acute cholecystits | Upper abdominal pain+haematemesis | Cholecystectomy |
| 48 | Read et al | 1990 | ANZ Journal of Surgery | Chronic calculous cholecystitis | Haemobilia | Cholecystectomy |
| 49 | Wu et al | 1988 | Acta Chirurgica Scandinavica | Acute cholecystitis | – | Surgery |
| 50 | Rhee JW et al | 1987 | New York State Journal of Medicine | Acute calculous cholecystitis | RUQ pain+fever | Cholecystectomy |
| 51 | Reddy et al | 1983 | Southern Medical Journal | Cholecystitis | Haemobilia | Cholecystectomy |
| 52 | Glazer et al | 1980 | Journal of Radiology | Postcholecystectomy | UGI bleed | – |
| 53 | Hakami et al | 1976 | American Journal of Proctology | ? Cholecystitis | Haemobilia | Cholecystectomy |
| 54 | Devin et al | 1971 | Journal de Chirurgie | Acute pancreatitis | Epigastric pain, jaundice, malena | Partial cholecystectomy |
?, suspected; f/b, followed by; GI, gastrointestinal; RHC, right hypochondrium; RUQ, right upper quadrant; TAE, transarterial embolisation; UGI, upper GI.
The exact cause of association between pseudoaneurysms and inflammation is not clear but it has been hypothesised that the inflammatory process leads to ulceration of the gallbladder wall and partial erosion of the elastic and muscular components of the vascular wall, leading to the development and rupture of the pseudoaneurysm.2 Despite cholecystitis being common, the rarity of cystic artery pseudoaneurysms can be explained by early thrombosis of the cystic artery due to inflammation.3
Cystic artery pseudoaneurysms can rupture in the biliary tree4 or rarely into the peritoneum.5 A high index of suspicion is required for diagnosis. Abdominal colour Doppler ultrasound can be an effective initial diagnostic tool but lacks high sensitivity.4 Endoscopy is helpful in diagnosing haemobilia in a patient with upper gastrointestinal bleeding. MRI and CT scan can identify the underlying pathology such as stones, cholecystitis, neoplasms and vascular abnormalities. However, selective hepatic angiography is the technique of choice in the management of haemobilia of any cause and for suspected pseudoaneurysms in particular, due to its high diagnostic accuracy and therapeutic potential.1 6 It is useful especially in elderly, haemodynamically unstable patients unfit for surgery, in stopping the active bleeding. Nevertheless, angiography has certain diagnostic limitations for the variable flow rate and intermittent bleeding, and also when there are hepatic artery abnormalities or when there has been previous manipulation. Despite there being reports of gallbladder infarction after hepatic artery embolisation with occlusion of the cystic artery, there has been no report of gallbladder gangrene, to date, after embolisation of the cystic artery pseudoaneurysm, probably due to collateral blood supply from the epicholedochal artery.7
In our patient, the cystic and left hepatic arteries were arising from the common hepatic artery. These anomalies have been described in the literature but are very uncommon.8 9
Haemobilia is known to cause biliary obstruction due to blood clots leading to jaundice, as seen in our case, which can be relieved by endoscopic drainage with stenting or nasobiliary drainage.10
Maeda et al5 were the first to report successful management of a cystic artery aneurysm by a combined approach: embolisation of the cystic artery to stabilise the patient, followed by cholecystectomy at a later, safer time. It seems a logical combination as the cause of inflammation, the stone, needs to be treated as well. Our case was also managed similarly with success.
Learning points.
In patients with gallstone disease, presence of malena should raise suspicion of a pseudoaneurysm.
A cystic artery pseudoaneurysm can be successfully managed by angioembolisation and open total/subtotal cholecystectomy.
Patients with a cystic artery pseudoaneurysm not fit for surgical intervention can be managed by embolisation alone.
Footnotes
Contributors: VK contributed to editing and approval of manuscript. HD contributed to revision and approval of manuscript. RG contributed to writing, editing and approval of manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Green MH, Duell RM, Johnson CD et al. Hemobilia. Br J Surg 2001;88:773–86. [DOI] [PubMed] [Google Scholar]
- 2.Akatsu T, Tanabe M, Shimizu T et al. Pseudoaneurysm of the cystic artery secondary to cholecystitis as a cause of hemobilia: report of a case .Surg Today 2007;37:412–17. [DOI] [PubMed] [Google Scholar]
- 3.Desai AU, Saunders MP, Anderson HJ et al. Successful transcatheter arterial embolisation of a cystic artery pseudoaneurysm secondary to calculus cholecystitis: a case report. Radiol Case 2010;4:18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakajima M, Hoshino H, Hayashi E et al. Pseudoaneurysm of the cystic artery associated with upper gastrointestinal bleeding .J Gastroenterol 1996;31:750–4. [DOI] [PubMed] [Google Scholar]
- 5.Ghoz A, Kheir E, Kotru A et al. Hemoperitoneum secondary to rupture of cystic artery pseudoaneurysm. Hepatobiliary Pancreat Dis Int 2007;6:321–3. [PubMed] [Google Scholar]
- 6.Maeda A, Kunou T, Saeki S et al. Pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization and elective cholecystectomy. J Hepatobiliary Pancreat Surg 2002;9:755–8. [DOI] [PubMed] [Google Scholar]
- 7.Takayasu K, Moriyama N, Muramatsu Y et al. Gallbladder infarction after hepatic artery embolization .AJR Am J Roentgenol 1985;144:135–8. [DOI] [PubMed] [Google Scholar]
- 8.Sureka B, Mittal MK, Mittal A et al. Variations of celiac axis, common hepatic artery and its branches in 600 patients. Indian J Radiol Imaging 2013;23:223–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patil SJ, Pakhiddey R, Rana K et al. Anomalous origin of cystic artery from common hepatic artery—a case report. J Morphol Sci 2013;30:198–9. [Google Scholar]
- 10.Wang CC, Liu CJ, Chen C et al. Hemobilia associated with acute calculus cholecystitis successfully treated with endoscopic naso-biliary drainage and laparoscopic cholecystectomy—a case report. Tzu Chi Med J 2006;18:137–40. [Google Scholar]


