Abstract
Intraperitoneal lipomas causing high-grade bowel obstruction in advanced pregnancy are rare. We report an unusual case which presented at 33 weeks with faecal vomitus and abdominal pain. Lipomas are benign adipose tissue tumours that are usually asymptomatic. The constraints of diagnosis, investigation and treatment of such tumours in pregnancy are also discussed.
Background
Intraperitoneal lipomas in pregnancy are rare. These benign tumours can present with non-specific gastrointestinal (GI) symptoms such as emesis and abdominal pain. They are generally difficult to identify clinically and harder to identify in pregnancy due to gestational, anatomical and physiological changes.
Case presentation
A 28-year-old woman attended our unit at 33 weeks of gestation with a history of vomiting, and abdominal and back pain of 1-week duration. Her antenatal history until then was unremarkable apart from having a low anterior placenta on the anomaly scan.
On admission, all her observations and examinations were normal. The abdomen was soft and non-tender with a gravid uterus appropriate for gestational age. On admission, urine dipstick analysis revealed ketones and leucocytes. Midstream urine was sent for culture and sensitivity. The full blood count, renal and liver function bloods including amylase were normal. The patient was initially managed conservatively with intravenous fluid, antiemetics and antibiotics for suspected urinary tract infection. Her symptoms improved marginally but there was persistent vomiting with mild epigastric tenderness. She continued to have normal observations.
On the third day of admission, the antibiotics were stopped as there was no growth in the urine culture. Regular antiemetics were continued with a proton pump inhibitor. An ultrasound (USS) of the upper abdomen was normal. Her vomitus was now brown in colour with specks of blood. A surgical opinion was requested due to the altered nature of the vomitus. During the day, the patient vomited 1300 mL bilious and faeculant matter. A wide bore nasogastric tube was inserted and surgical opinion requested.
Investigations
After a multidisciplinary discussion between the consultant obstetrician, surgeon and radiologist, MRI of the abdomen with gadolinium contrast was arranged. MRI of the abdomen revealed a 13.5 cm×10cm×7 cm ovoid mass thought to be an intraperitoneal lipoma occupying the superior aspect of the right paracolic gutter, abutting the undersurface of the liver (figure 1). The lesion appeared to be attached to the peritoneum along the paracolic gutter. There was marked fluid distension of the small bowel and stomach proximally, whereas the distal small bowel and colon beyond was completely collapsed due to obstruction caused by the lipoma. A laparotomy with caesarean section was planned immediately as the patient developed mild metabolic acidosis.
Figure 1.
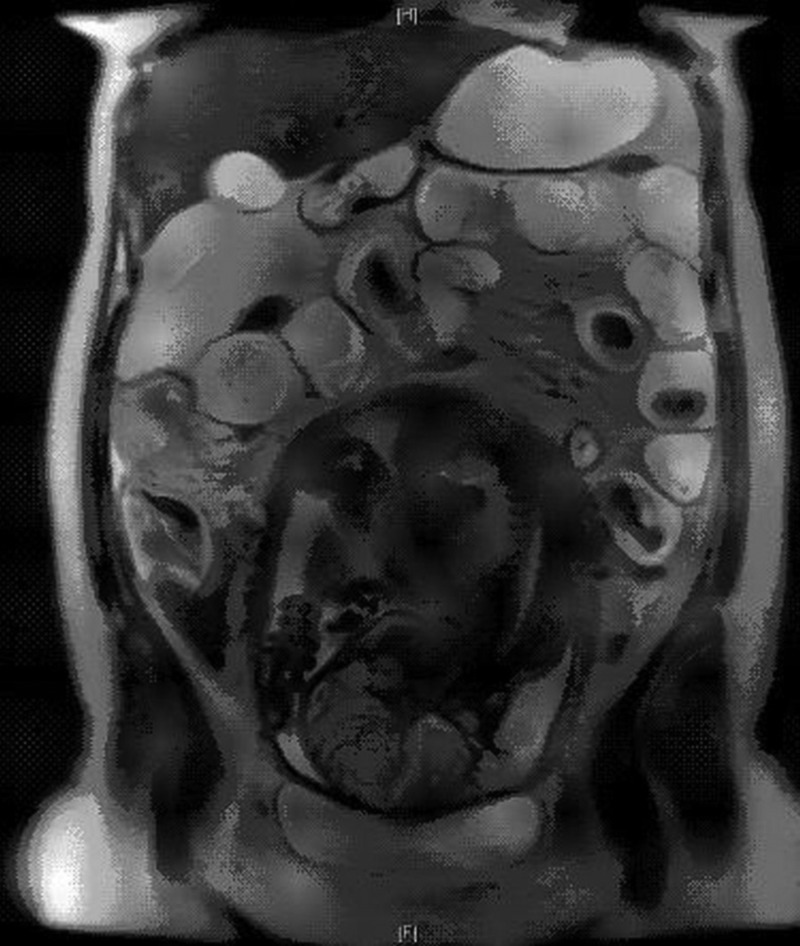
MRI of the abdomen in pregnancy. The intraperitoneal lipoma (13.5 cm×10 cm×7 cm) occupied the superior aspect of the right paracolic gutter, abutting the undersurface of the liver.
Differential diagnosis
The common non-obstetric causes for abdominal pain and vomiting include gastroenteritis, appendicitis, urolithiasis, biliary disease and trauma to the abdomen. Persistent vomiting inspite of antiemetics should alert the possibility of bowel obstruction.
Treatment
An uneventful lower segment caesarean section was performed through a midline incision. A live male baby weighing 2.145 kg was delivered. After closure of the uterus, inspection of the bowels by the surgeons revealed a 13×10 cm lipoma of small bowel mesentery that was found to be causing internal herniation (figure 2). The small bowel was twisted four times and dusky in colour. The lipoma was resected along with 8 cm of the small intestine and sent for histology. The histological examination revealed two serosal lipomas 14×11×8 cm and 3.5 cm with no evidence of malignancy.
Figure 2.

Lipoma of small bowel mesentry in pregnancy. The bowel was twisted four times on itself and caused internal herniation and small bowel obstruction.
Postoperative care included admission to intensive care unit to correct metabolic acidosis.
Outcome and follow-up
The patient made a good recovery postnatally with quick resolution of acidosis and was discharged on the sixth postoperative day from hospital. At the 6-week follow-up, she had no GI problems and her laparotomy wound had healed.
Discussion
Large intraperitoneal lipomas are rare and may originate from retroperitoneal adipose muscle, connective, lymphatic, nerve tissues or urogenital tract.1 The most common peritoneal lipomas occur through the intestinal tract commonly the colon, small bowel, stomach, oesophagus and pharynx.2 These benign tumours are known to attain large dimensions and have non-specific features due to their insidious growth.3
Abdominal pain and distension are the most common symptoms associated with intraperitoneal/retroperitoneal lipomas.4 Rarely symptoms of intestinal obstruction occur including vomiting and they can be mild at first. In severe cases of small bowel obstruction (SBO) as reported with our patient, the vomitus may contain faecal material because of the reversal of peristalsis and forcing of the intestinal contents back into the stomach.
In pregnancy, initial symptoms of SBO can be confused with the common symptoms of nausea, vomiting, constipation and gastro-oeophageal reflux physiological changes of the GI tract. Pregnancy has a major effect on the GI tract due to responses to increased levels of oestrogen and progesterone that cause increased bowel transit time. The mechanical displacement of bowels by the enlarging uterus decreased levels of motilin, increased colonic sodium and fluid absorption and routine iron supplementation5 are other factors contributing to symptoms similar to those of GI disorders. Owing to this, there can be a delay in diagnosis and other confounding factors include abnormal location of abdominal pain, imaging delay due to concerns of harm to the fetus.
A multidisciplinary approach to evaluation is necessary as radiological procedures and treatment measures should take into account severity of maternal symptoms, gestational age of fetus and the potential harmful effects to fetus.
The most common modalities used to diagnose GI disorders outside pregnancy are abdominal X-ray, USS, CT or MRI. In pregnancy, imaging with USS is the first line as it is non-invasive and free from ionising radiation.6 The radiation exposure from an abdominal/pelvis CT is 300 mrad which is below the cut-off of 50 rad, the level for concern of teratogenesis.7 MRI in pregnancy has gained popularity in the last decade as it is not known to have adverse effects on fetal health.7 8
The treatment of intraperitoneal/retroperitoneal lipomas is mostly surgical.9 10 The capsule that surrounds the lipoma usually presents a clear cleavage plane with neighbouring structures which allows easy surgical resection. A complete resection is sufficient to prevent further recurrences. The recurrence rate of all lipomas is usually less than 5% and is usually due to incomplete resection.11
Bowel obstruction is an unusual complication in pregnancy. In one series of case studies of nine cases of SBO in pregnancy, 80–89% of the patients had primary symptoms of abdominal pain, vomiting and constipation.12 Previous abdominal surgery was documented in 90% of patients. There were three fetal deaths in this cohort at 22, 23 and 30 weeks.
Learning points.
Intraperitoneal lipomas as a cause of bowel obstruction are rare.
Bowel obstruction is associated with increased maternal morbidity during pregnancy.
Symptoms associated with bowel obstruction are similar to physiological gestational symptoms such as vomiting and abdominal pain.
Clinical suspicion of bowel obstruction should be increased when pregnant patients do not respond to antiemetics and intravenous fluids.
Footnotes
Contributors: SM drafted the report. SA and CN were involved in the management of the case and contributed to minor revisions of the draft.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Martinez CA, Palma RT, Waisberg J. Giant retroperitoneal lipoma: a case report. Arq Gastroenterol 2003;40:251–5. [DOI] [PubMed] [Google Scholar]
- 2.Taylor AJ, Stewart ET, Dodds WJ. Gastrointestinal lipomas: a radiologic and pathologic review. AJR Am J Roentgenol 1990;155:1205–10. [DOI] [PubMed] [Google Scholar]
- 3.Cavazza A, Guinta A, Pedrazzoli C et al. [Extrarenal retroperitoneal angiomyolipoma: description of a case and review of the literature]. Pathologica 2001;93:44–9. [PubMed] [Google Scholar]
- 4.Barut I, Trahan OR, Terhi C et al. Lipoma of the parietal peritoneum: an unusual cause of abdominal pain. Ann Saudi Med 2006;26:388–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singer AJ, Brandt LJ. Pathophysiology of the gastrointestinal tract during pregnancy. Am J Gastroenterol 1991;86:1695–712. [PubMed] [Google Scholar]
- 6.Temperton DH. Pregnancy and work in diagnostic imaging departments. British Institute of Radiology, 2009. [Google Scholar]
- 7.Mole RH. Irradiation of the embryo and fetus. Br J Radiol 1987;60:17–31. [DOI] [PubMed] [Google Scholar]
- 8.Baker PN, Johnson IR, Harvey PR et al. A three-year follow-up of children imaged in utero with echo-planar magnetic resonance. Am J Obstet Gynecol 1994;170(1 Pt 1):32–3. [DOI] [PubMed] [Google Scholar]
- 9.Arribas D, Kay A, Latorre A et al. Retroperitoneal mucinous cystadenoma. Arch Gynecol Obstet 2004;270:292–3. [DOI] [PubMed] [Google Scholar]
- 10.Lai EC, Chung KM, Lau WY. Primary retroperitoneal mucinous cystadenoma. ANZ J Surg 2006;76:537. [DOI] [PubMed] [Google Scholar]
- 11.Luo X, Gao W, Zhan J. Giant omental lipoma in children. J Pediatr Surg 2005;40:734–6. [DOI] [PubMed] [Google Scholar]
- 12.Meyerson S, Holtz T, Ehrinpreis M et al. Small bowel obstruction in pregnancy. Am J Gastroenterol 1995;90:299–302. [PubMed] [Google Scholar]


