Abstract
Objective
Elevation of C reactive protein (CRP) is one of the major acute-phase responses following ischaemic or haemorrhagic stroke. This study aims to investigate the associations between platelet indices, neutrophil-to-lymphocyte ratio (NLR) and erythrocyte sedimentation rate (ESR) compared with CRP in patients with cerebral infarction.
Setting
The clinical data of patients with cerebral infarction were analysed retrospectively.
Participants
We analysed, unduplicated, 516 patients with cerebral infarction (mean age 66.2±12.7, male/female=291/225).
Outcome measures
Mean platelet volume (MPV), MPV to platelet count, NLR and ESR were compared with CRP in patients with cerebral infarction in a single institute through Spearman correlation test.
Results
There were significant correlations between CRP and MPV (ρ=0.088, p=0.045), NLR (ρ=0.4, p<0.001) and ESR (ρ=0.468, p<0.001) in patients with cerebral infarction. In the male group, NLR (ρ=0.398, p<0.001) and ESR (ρ=0.502, p<0.001) showed significant correlations with CRP. In the female group, CRP showed significant correlations with MPV (ρ=0.17, p=0.011), NLR (ρ=0.392, p<0.001) and ESR (ρ=0.475, p<0.001).
Conclusions
MPV, NLR and ESR showed significant correlation with CRP in patients with cerebral infarction. MPV and NLR are cost-effective and simple parameters that can be attainable by using an automatic haematology analyser. Further well-designed and large-scale prospective studies are warranted to evaluate platelet indices or NLR for monitoring patients with cerebral infarction.
Keywords: IMMUNOLOGY, HAEMATOLOGY
Strengths and limitations of this study.
Mean platelet volume (MPV), neutrophil-to-lymphocyte ratio (NLR) and erythrocyte sedimentation rate (ESR) were positively associated with C reactive protein (CRP) in patients with cerebral infarction, especially female patients.
MPV, NLR and ESR may be useful parameters for evaluating patients with cerebral infarction compared with CRP.
MPV or NLR are cost-effective and simple parameters that can be attainable by using an automatic haematology analyser.
Further well-designed studies are warranted to understand the exact meaning of platelet indices and NLR in monitoring of patients with cerebral infarction.
Introduction
There have been many efforts to find useful diagnostic markers for monitoring patients with cerebral infarction. C reactive protein (CRP) is a marker of inflammation and a hallmark of the acute-phase response.1 Many reports suggested that CRP was associated with risk of stroke,2–4 whereas some reports did not find significant relations.5 6 Recently, Liu et al7 reported that elevated high sensitivity-CRP (hs-CRP) concentrations were associated with a higher risk of ischaemic stroke, particularly for non-fatal stroke, males and hypertensive participants but there were no significant associations between hs-CRP and intracranial haemorrhage and subarachnoid haemorrhage in a large prospective study. Also, erythrocyte sedimentation rate (ESR), a classical acute-phase marker, was often compared with CRP. Recently, there were a number of reports dealing with platelet indices such as mean platelet volume (MPV); MPV/platelet count (PC) ratios have clinical indications in various conditions such as atherosclerosis,8 9 cerebral infarction10 and active inflammatory diseases;11 12 high MPV was even associated with fractures.13 Also, the neutrophil-to-lymphocyte ratio (NLR) parameter was reported to be an important measure of systemic inflammation.14 However, platelet indices and NLR have not been fully investigated in roles as useful surrogate biomarkers of diagnosis in patients with cerebral infarction. This study aims to show any association between platelet indices, NLR and ESR compared with CRP in patients with cerebral infarction.
Methods
Data extraction
Retrospectively, we analysed, unduplicated, 516 patients with cerebral infarction (mean age 66.2±12.7 years, male-to-female ratio 1.3 (291–225)) whose MPV, MPV/PC ratio, NLR and ESR were compared with CRP from January 2010 to September 2013. All patients’ medical data were ethically protected and were solely analysed for this retrospective study. CRP levels were determined by HiSens hsCRP LTIA (HBI Co, Ltd, Anyang, Korea), latex-enhanced turbidimetric immunoassay, as read on the TBA-200FR NEO automated clinical chemistry analyser (Toshiba Medical Systems Corporation, Tochigi-ken, Japan). PC, MPV, and NLR were measured by Beckman Coulter LH 750 or 780 (Beckman Coulter, Miami, USA) haematology analysers. ESR was measured by TEST 1 (Alifax, Padova, Italy), a closed automated analyser, which determines the ESR using the aggregation capacity of red blood cells by telemetry.15
Statistical analysis
All data were confirmed by using a Kolmogorov-Smirnov test and Shapiro-Wilk test for identifying normal distribution. The correlation analysis of the two parameters was performed using Spearman correlation analysis when normal distribution was not confirmed and a Pearson correlation test was used when variables were normally distributed. A p value of less than 0.05 was considered statistically significant. Statistical analyses were performed using IBM SPSS Statistics V.20 (IBM Corporation, Armonk, New York, USA).
Results
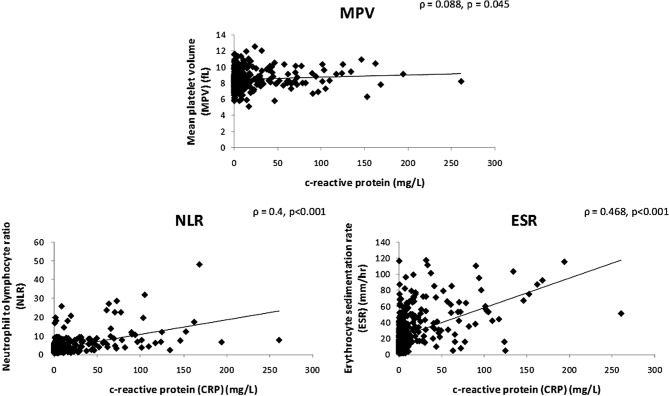
The analysed parameters were not normally distributed (p<0.05), therefore we trusted the Spearman correlation analysis. CRP showed significant correlations with MPV (ρ=0.088, p=0.045), NLR (ρ=0.4, p<0.001) and ESR (ρ=0.468, p<0.001) in patients with cerebral infarction (figure 1). However, MPV/PC (ρ=0.016, p=0.711) was not significantly correlated with CRP in patients with cerebral infarction. In the male group (n=291), CRP showed significant correlations with NLR (ρ=0.398, p<0.001), and ESR (ρ=0.502, p<0.001) in patients with cerebral infarction. However, MPV (ρ=0.008, p=0.890) and MPV/PC (ρ=−0.077, p=0.188) were not significantly correlated with CRP in the male group. In the female group (n=225), CRP showed significant correlations with MPV (ρ=0.17, p=0.011), NLR (ρ=0.392, p<0.001) and ESR (ρ=0.475, p<0.001) in patients with cerebral infarction. However, MPV/PC was not significantly correlated with CRP (ρ=0.104, p=0.121) in the female group.
Figure 1.
The correlation between mean platelet volume (MPV), neutrophil to lymphocyte ratio (NLR), erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) in cerebral infraction patients. ρ, Spearman's rank correlation coefficient.
Although the analysed parameters were not normally distributed, if the Pearson correlation test was used, CRP showed significant correlations with MPV/PC (r=0.164, p<0.001), NLR (r=0.517, p<0.001) and ESR (r=0.479, p<0.001) in patients with cerebral infarction. However, there was not a significant correlation between CRP and MPV (r=0.068, p=0.121) in patients with cerebral infarction. Also, these similar results were noted in male (n=291) or female (n=225) divided group analysis. In the male group, CRP showed significant correlations with MPV/PC (r=0.144, p=0.014), NLR (r=0.413, p<0.001) and ESR (r=0.82, p<0.001) in patients with cerebral infarction. In the female group, CRP showed significant correlations with MPV/PC (r=0.197, p=0.003), NLR (r=0.620, p<0.001) and ESR (r=0.484, p<0.001) in patients with cerebral infarction.
Discussion
There were many factors of cerebral infarction pathogenesis. We thought activated platelets could be produced in various cerebral vascular diseases and these conditions might increase MPV. The inflammation seems to be related with the pathogenesis of cerebral infarction. Inflammation is found to develop at a sufficiently early stage in progressive ischaemic brain injury.16 Besides cerebral infarction, our previous study showed a positive correlation of CRP with MPV/PC and NLR were noted in patients with pneumonia.17 Recently, there were various studies that dealt with relationships between haematological indices and cerebral infarction.18–20
Arikanoglu et al18 reported that CRP and MPV are higher in the patients with ischaemic stroke who died in comparison to those who survived. MPV is a novel index for silent cerebral infarction regardless of classical cardiovascular risk factors.19 Also, NLR predicts poor prognosis in ischaemic cerebrovascular disease.20 Although CRP level and outcome of ischaemic stroke is under debate,21 the inflammation might be related to a certain progression of cerebral infarction. Therefore, CRP is a representative inflammatory marker, and appears useful in comparing new parameters with CRP in patients with cerebral infarction.
For the first time, this study showed MPV and NLR as expected ESR could be statistically correlated with CRP in a moderate number of patients with cerebral infarction. We identified that MPV was correlated with CRP overall and in the female group, but was not correlated in the male group. A report suggested that in Korea, women had a higher median PC than men.22 A few studies suggested that men had slightly higher MPV than women.23 24 Only female MPV showed significant correlation with CRP. The exact causes of gender difference were not uncovered, but it might owe to a difference of PC or hormonal differences between women and men. In the Pearson correlation analysis, CRP showed significant correlations with MPV/PC (r=0.164, p<0.001), NLR (r=0.517, p<0.001) and ESR (r=0.479, p<0.001) in patients with cerebral infarction. However, as all analysed parameters were not normally distributed, we considered it proper to interpret data by the Spearman correlation test. Both NLR and ESR were positively correlated with CRP in Pearson or Spearman correlation tests.
This study might support further related studies dealing with an association between cerebral infarction and inflammation. Also, MPV, NLR and ESR should be further investigated for their ability to find the clinical impact of disease progression and expectation of mortality in patients with cerebral infarction. Up to date, the consensus diagnostic cut-off ranges of MPV and NLR have not been established for evaluation of cerebral infarction. Furthermore, platelet indices measure the femtolitre (10–15 L) levels and still have not been standardised; the results also vary from device to device.25 This study has some limitations such as the participants were retrospectively analysed for quite a long time (3 years and 8 months). We did not categorise specific cerebral infarction types and did not strictly exclude patients with additional disorders such as diabetes, cardiovascular diseases and malignant diseases, which might impact the level of enrolled parameters. In addition, MPV can be influenced by the time interval between sampling and analysis.26 MPV results become increasingly unreliable after 4 h.27 Complete blood count analysis in our laboratory has almost proceeded within 4 h from sampling start.
In conclusion, we suggest the novel possibility that MPV and NLR may be useful parameters for evaluating patients with cerebral infarction compared with CRP. Characteristically, MPV or NLR are inexpensive and simple parameters that can be attainable by using an automatic haematology analyser. Therefore, further well-designed and large-scale prospective studies are warranted to evaluate platelet indices or NLR for monitoring patients with cerebral infarction.
Supplementary Material
Footnotes
Contributors: J-HL designed and participated in all stages of the study. K-YK consulted diagnosis of patients. S-YY, H-SK and CSL helped with consultations for this study.
Funding: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (No. 2008-0061891).
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Di Napoli M, Elkind MS, Godoy DA et al. Role of C-reactive protein in cerebrovascular disease: a critical review. Expert Rev Cardiovasc Ther 2011;9:1565–84. [DOI] [PubMed] [Google Scholar]
- 2.Cao JJ, Thach C, Manolio TA et al. C-reactive protein, carotid intima-media thickness, and incidence of ischemic stroke in the elderly: the Cardiovascular Health Study. Circulation 2003;108:166–70. [DOI] [PubMed] [Google Scholar]
- 3.Di Napoli M, Papa F, Bocola V. C-reactive protein in ischemic stroke: an independent prognostic factor. Stroke 2001;32:917–24. [DOI] [PubMed] [Google Scholar]
- 4.Rost NS, Wolf PA, Kase CS et al. Plasma concentration of C-reactive protein and risk of ischemic stroke and transient ischemic attack: the Framingham study. Stroke 2001;32:2575–9. [DOI] [PubMed] [Google Scholar]
- 5.Bos MJ, Schipper CM, Koudstaal PJ et al. High serum C-reactive protein level is not an independent predictor for stroke: the Rotterdam Study. Circulation 2006;114:1591–8. [DOI] [PubMed] [Google Scholar]
- 6.Wilson PW, Nam BH, Pencina M et al. C-reactive protein and risk of cardiovascular disease in men and women from the Framingham Heart Study. Arch Intern Med 2005;165:2473–8. [DOI] [PubMed] [Google Scholar]
- 7.Liu Y, Wang J, Zhang L et al. Relationship between C-reactive protein and stroke: a large prospective community based study. PLoS ONE 2014;9:e107017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murat SN, Duran M, Kalay N et al. Relation between mean platelet volume and severity of atherosclerosis in patients with acute coronary syndromes. Angiology 2013;64:131–6. [DOI] [PubMed] [Google Scholar]
- 9.Ozkan B, Uysal OK, Duran M et al. Relationship between mean platelet volume and atherosclerosis in young patients with ST elevation myocardial infarction. Angiology 2013;64:371–4. [DOI] [PubMed] [Google Scholar]
- 10.Tang WB, Li MX, Li GQ et al. [Changes of mean platelet volume, fibrinogen content and blood rheology in peripheral blood of youth patients with cerebral infarction]. Zhongguo Shi Yan Xue Ye Xue Za Zhi 2012;20:390–3. [PubMed] [Google Scholar]
- 11.Canpolat F, Akpinar H, Eskioglu F. Mean platelet volume in psoriasis and psoriatic arthritis. Clin Rheumatol 2010;29:325–8. [DOI] [PubMed] [Google Scholar]
- 12.Yazici S, Yazici M, Erer B et al. The platelet indices in patients with rheumatoid arthritis: mean platelet volume reflects disease activity. Platelets 2010;21:122–5. [DOI] [PubMed] [Google Scholar]
- 13.Cure E, Balik MS, Cumhur Cure M et al. Is the mean platelet volume predictive of hip fractures in the elderly? Ann Lab Med 2013;33:367–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Imtiaz F, Shafique K, Mirza SS et al. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med 2012;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cha CH, Park CJ, Cha YJ et al. Erythrocyte sedimentation rate measurements by TEST 1 better reflect inflammation than do those by the Westergren method in patients with malignancy, autoimmune disease, or infection. Am J Clin Pathol 2009;131:189–4. [DOI] [PubMed] [Google Scholar]
- 16.Hallenbeck JM. Significance of the inflammatory response in brain ischemia. Acta Neurochir Suppl 1996;66:27–31. [DOI] [PubMed] [Google Scholar]
- 17.Lee JH, Yoon SY, Kim HS et al. Characteristics of the mean platelet volume, neutrophil to lymphocyte ratio, and C-reactive protein compared to the procalcitonin level in pneumonia patients. Platelets 2014. [DOI] [PubMed] [Google Scholar]
- 18.Arikanoglu A, Yucel Y, Acar A et al. The relationship of the mean platelet volume and C-reactive protein levels with mortality in ischemic stroke patients. Eur Rev Med Pharmacol Sci 2013;17:1774–7. [PubMed] [Google Scholar]
- 19.Li B, Liu X, Cao ZG et al. Elevated mean platelet volume is associated with silent cerebral infarction. Intern Med J 2014;44:653–7. [DOI] [PubMed] [Google Scholar]
- 20.Celikbilek A, Ismailogullari S, Zararsiz G. Neutrophil to lymphocyte ratio predicts poor prognosis in ischemic cerebrovascular disease. J Clin Lab Anal 2014;28:27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taheraghdam A, Aminnejad S, Pashapour A et al. Is there a correlation between hs-CRP levels and functional outcome of Ischemic Stroke? Pak J Med Sci 2013;29:166–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim MJ, Park PW, Seo YH et al. Reference intervals for platelet parameters in Korean adults using ADVIA 2120. Ann Lab Med 2013;33:364–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bain BJ. Platelet count and platelet size in males and females. Scand J Haematol 1985;35:77–9. [DOI] [PubMed] [Google Scholar]
- 24.Butkiewicz AM, Kemona H, Dymicka-Piekarska V et al. Platelet count, mean platelet volume and thrombocytopoietic indices in healthy women and men. Thromb Res 2006;118:199–204. [DOI] [PubMed] [Google Scholar]
- 25.Beyan C. Is mean platelet volume a predictive marker in patients with venous thrombosis? Clin Appl Thromb Hemost 2012;18: 670–1. [DOI] [PubMed] [Google Scholar]
- 26.Machin SJ, Briggs C. Mean platelet volume: a quick, easy determinant of thrombotic risk? J Thromb Haemost 2010;8:146–7. [DOI] [PubMed] [Google Scholar]
- 27.Brummitt DR, Barker HF. The determination of a reference range for new platelet parameters produced by the Bayer ADVIA120 full blood count analyser. Clin Lab Haematol 2000;22:103–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.