Abstract
An unusual extensive bilateral macular oedema (MO) with spontaneous resolution occurred following a car crash accident. Qualitative and quantitative analysis of the macular region using spectral domain optical coherence tomography (SD-OCT) and multifocal electroretinogram (mfERG) was performed daily during the first 7 days, as well as at 3 and 6 months following the accident. SD-OCT examination demonstrated extensive MO accompanied by neurosensory detachment and subretinal fluid. During the 7 days following the accident there was gradual resolution of the oedema accompanied by visual recovery. One year later no anatomical changes were observed, the mfERG showed complete recovery and visual acuity returned to normal level. Although whiplash is a common injury in motor vehicle accidents, whiplash maculopathy (WMP) is rarely reported, most likely due to underdiagnosis. Here we describe the spontaneous resolution of a severe MO after whiplash injury in a car crash accident.
Background
Whiplash maculopathy (WMP) is an unusual finding associated with a localised retinal concussion after car accident. Only a few cases have been described, most likely due to underdiagnosis.1–3 Here we report on the spontaneous resolution of an unusual macular oedema (MO) with extensive neurosensory detachment after a car crash accident. Although benign the physicians should be alert in similar situations on patient history and complaints as differential diagnosis is extensive and long term complications cannot be excluded.
Case presentation
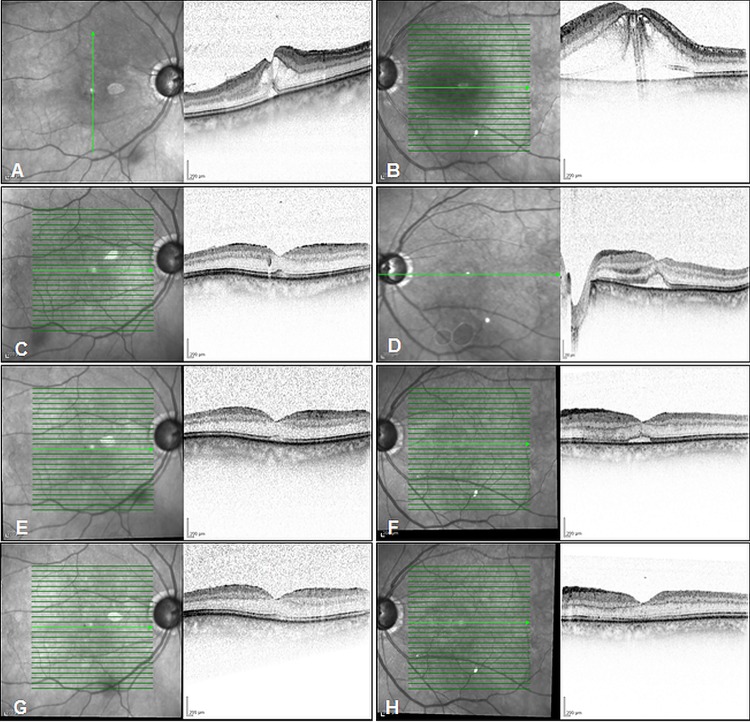
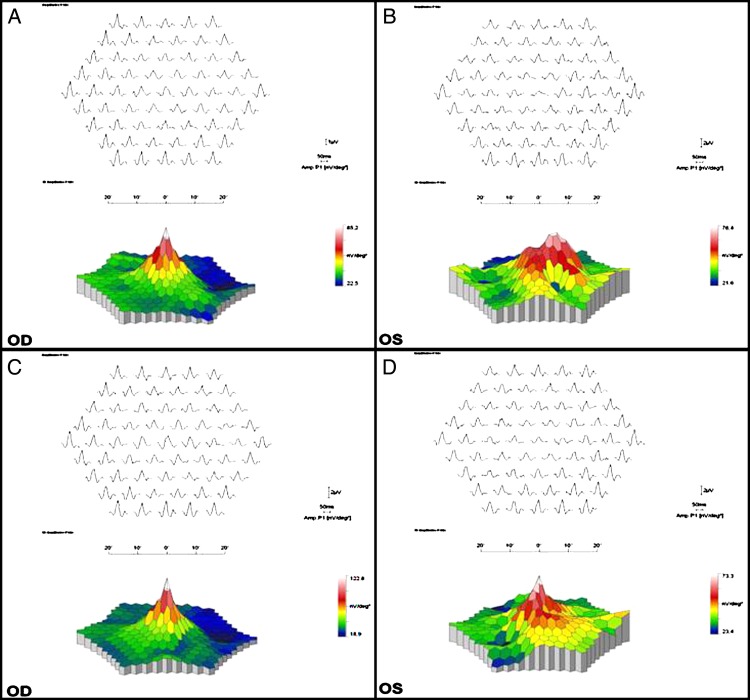
A 77-year-old woman involved in a car crash accident at a speed of 50 km/h (31 mph) was examined immediately after the accident because of blurred near vision. At the moment of impact neither the seat belt nor the airbag deployed resulting in a mild bruise on the chest from the impact on the driving wheel. There were no further signs of facial or orbital trauma. Blood tests as well as neuroimaging were normal. The examination revealed bilateral multifocal lenses, normal anterior chamber and intraocular pressure. Best corrected visual acuity (VA) was 6/19, Nieden (Nd) VI right eye (OD) and 3/60, Nd IV left eye (OS) with brief episodes of Charles Bonnet symptoms. Funduscopy revealed a yellow-greyish discoloration of the macula but no haemorrhages or cotton wool spots. Optical coherence tomography (OCT) examination demonstrated an extensive MO complicated by neurosensory detachment and subretinal fluid (figure 1A, B). The patient was examined daily and a gradual improvement was noted. On day 3 the retina showed signs of recovery as evidenced by subretinal fluid decrease (figure 1C, D). The multifocal electroretinogram (mfERG) responses of the OD were normal (figure 2A) the OS demonstrated mild central depression (figure 2B). On day 7 VA had improved to 6/6, Nd III OD and 6/15, Nd V OS with complete oedema resolution and preservation of the inner/outer segment (IS/OS) junction (figure 1E, F). Follow-up examination at 3 months showed improved VA (6/6 Nd I, OD; 6/7.5 Nd II OS), normal macular anatomy (figure 1G, H) and normal/near normal mfERG on both eyes (figure 2C, D). On the last examination at 6 months the VA was normal for far and near (6/6 OD, 6/7.5 OS, Nd I-II), the macular anatomy was restored with an intact IS/OS junction and only subtle signs of an epiretinal membrane on the left eye could be observed.
Figure 1.
Optical coherence tomography (OCT) imaging. On presentation OCT demonstrates extensive macular oedema with subretinal fluid accumulation (A and B). On day 3 the retina showed signs of recovery with reduction of oedema (C and D) and by day 7 there was almost complete recovery of the macular anatomy (E and F).Three months after first presentation the macular anatomy was completely restored (G and H).
Figure 2.
Multifocal electroretinogram. The evoked potentials of the right eye at day 3 after first presentation are normal whereas the evoked potentials of the left eye still show some central alteration. Three months after first presentation the evoked potentials of both eyes have reached normal levels, however subtle areas of distortion remain in the left eye, probably due to internal limiting membrane traction.
Investigations
Spectral domain optical coherence tomography (SD-OCT)
mfERG
Differential diagnosis
Toxic maculopathies, shaken baby syndrome, valsalva retinopathy and Purtscher's retinopathy
Treatment
Observational approach.
Outcome and follow-up
During the first 7 days the patient was followed on a daily basis, further examinations were performed at 3, 6 and 12 months after the accident. During the first 7 days there was a gradual resolution of the oedema accompanied by visual recovery. One year later no anatomical changes could be observed, the mfERG showed complete recovery and visual acuity returned to normal level.
Discussion
Since the first description on WMP1 only sporadic cases have been reported, most likely due to underdiagnosis. In particular serous retinopathy associated with neurosensory detachment is a rare occurrence.4 5 Although the neurosensory detachment in our case was extensive, the anatomy of the inner retina and particularly the IS/OS junction was preserved, which is consistent with the rapid improvement of VA and mfERG activity. MfERG alterations have been previously studied in traumatic maculopathy cases6 and can persist up to 6 months.7 In the absence of a direct ocular force we hypothesise a rapid anteroposterior stress of the vitreous followed by rapid deceleration leading to retinal traction, capillary breaks, fluid extravasation and MO. The lack of a native lens, which provides resistance to stress on the vitreous, may have further contributed to the development the MO and neurosensory detachment.
In conclusion, the natural history of WMP is characterised by a blurring of vision accompanied by a central scotoma but the visual acuity recovers usually within days. The differential diagnosis is extensive and includes toxic maculopathies, shaken baby syndrome, valsalva retinopathy and Purtscher's retinopathy. Much attention should be given to the patient’s history as well as visual symptoms and a careful slit-lamp examination as well as OCT should be able to define the characteristic pathology. Although benign physicians should be alert in similar situations as long-term complications cannot be excluded.
Learning points.
Whiplash injury is frequent in car crash accidents.
Whiplash maculopathy is an unusual finding associated with a localised retinal concussion.
To define the characteristic pathology much attention should be paid to patients history and symptoms.
Examination should include careful slit-lamp examination assisted by optical coherence tomography in uncertain cases.
Observational approach is sufficient as spontaneous improvement is frequent.
Acknowledgments
The authors thank Ms Karin Ehrenberg and Ms Elke Cropp for their valuable technical assistance.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Narasaki S, Matsuzaki H, Obayashi K. [Ophthalmic disturbance in whiplash injury]. Nihon Ganka Gakkai Zasshi 1968;72:1694–703. [PubMed] [Google Scholar]
- 2.Mavrakanas N, Dreifuss S, Safran AB. OCT III imaging of whiplash maculopathy. Eye (Lond) 2008;22:860–1. [DOI] [PubMed] [Google Scholar]
- 3.McCannel CA. OCT III imaging of whiplash maculopathy. Eye (Lond) 2011;25:531–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pham TQ, Chua B, Gorbatov M et al. Optical coherence tomography findings of acute traumatic maculopathy following motor vehicle accident. Am J Ophthalmol 2007;143:348–50. [DOI] [PubMed] [Google Scholar]
- 5.Kung J, Leung LS, Leng T et al. Traumatic airbag maculopathy. JAMA Ophthalmol 2013;131:685–7. [DOI] [PubMed] [Google Scholar]
- 6.Purvin V, Maturi R, Vaphiades MS. Sprint car visual loss. Surv Ophthalmol 2004;49:90–5. [DOI] [PubMed] [Google Scholar]
- 7.Saleh M, Letsch J, Bourcier T et al. Long-term outcomes of acute traumatic maculopathy. Retina 2011;31:2037–43. [DOI] [PubMed] [Google Scholar]