Abstract
Rounded and velvety epidermal naevus, naevoid acanthosis nigricans, also called the acanthosis nigricans form of epidermal naevus is an extremely rare entity, with fewer than 15 cases described in the literature. We report the case of a 23-year-old woman with asymptomatic velvety verrucous plaques on her left axilla starting at the age of 14. As far as we know this is the first case of such a verrucous form with only axillar involvement of naevoid acanthosis nigricans. We report this rare case, and we make a brief review of the clinical pathophysiology and treatment of this uncommon tumour.
Background
The rounded and velvety epidermal naevus (RAVEN) is an extremely rare entity with fewer than 15 cases reported in the literature. This report contributes to a better characterisation of this entity and to clarifying that it is not usually correlated with an endocrinopathy as is apparent in acanthosis nigricans. It is also an alert towards the importance of knowing and understanding skin lesions in paediatric patients.
Case presentation
A 23-year-old woman presented with asymptomatic coalescent velvety verrucous plaques on her left axilla (figure 1). The lesion started as a velvety plaque at the age of 14. During that time and until the observation it became more verrucous and progressively spread along the axilla. She denied any previous lesion or taking any medication.
Figure 1.

Linear velvety exophytic and coalescent round-shaped plaques, distributed only in the left axila.
An examination revealed velvety exophytic and coalescent plaques located only in her left axilla. There were no other skin, scalp, nail or mucosal lesions. The remainder of her physical examination was normal. Her body mass index was 23.5 kg/m2 and she did not have any signs of thyroid disease, Cushing disease, acromegaly, diabetes mellitus, other endocrinopathy, signs of malignancy or syndromal features. Her family history was irrelevant.
Investigations
Laboratory tests (haemogram, renal and liver function, thyroid hormones, cortisol levels, insulin levels, somatotropin and blood glucose) were within normal levels. The histological examination of two biopsies of the verrucous plaques showed aspects of acanthosis nigricans as well as epidermal naevus: hyperkeratosis, marked papillomatosis, increased pigmentation of the basal cells and mild acanthosis (figures 2 and 3).
Figure 2.

Histopathological examination (H&E, ×10) showing aspects of acanthosis nigricans as well as epidermal naevus: acanthosis, marked papillomatosis and hyperkeratosis with increased pigmentation of the basal and suprabasal lamina.
Figure 3.
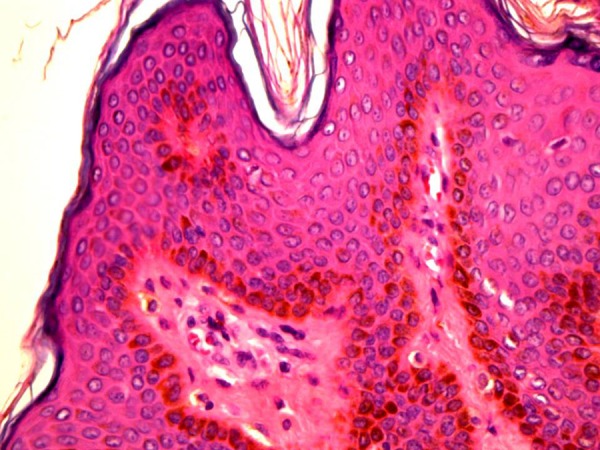
Histopathological examination (H&E, ×40) showing aspects of acanthosis nigricans as well as epidermal naevus: acanthosis, marked papillomatosis and hyperkeratosis with increased pigmentation of the basal and suprabasal lamina.
Differential diagnosis
In the differential diagnosis we have to consider other types of epidermal naevus, acanthosis nigricans and melanocytic naevus. Nevertheless the correct diagnosis could be easily ascertained combining the clinical velvety unilateral verrucous characteristics of the skin lesion, its evolution along puberty and the remarkable histopathological findings in our patient. Another important point is the fact that the plaque resulted from coalescent lesions with a rounded shape. This supports the diagnosis of RAVEN against the diagnosis of classic epidermal naevus. Acanthosis nigricans was excluded because it was a unilateral exophytic lesion, and the clinical picture and histology excluded a melanocytic lesion.
Treatment
The patient was referred for treatment with CO2 LASER as reported in other cases because of the patient's phototype VI and the exophytic character of the lesion. She underwent one session of CO2 LASER in a test area of 5 cm2, with good cosmetic and functional result. However, further follow-up and treatment were not possible because the patient abandoned the treatment sessions.
Discussion
The first reported case of a probable RAVEN was made by Curth.1 Attending the histogenesis of this lesion it is thought that a postzygotic mosaicism of the fibroblast growth factor receptor three gene is involved, although this is an extrapolated hypothesis from previous epidermal naevi studies.2 RAVEN can appear at birth, childhood, puberty or in middle-aged adults.
We report our case because, as far as we know, this is the first case with only axillary involvement of such an exophytic growth. Previous published cases have not shown this type of exophytic growth (except a case reported by Waal et al,3 in which the axillary lesion of the patient also had a slightly marked exophytic growth); but in our patient the clinical evolution and histological examination support the hypothesis of RAVEN. There are fewer than 15 cases published of this entity; the majority of them are of lighter skin phototypes and midline localisation. We can hypothesise that the reason for such an exophytic growth could be because it is located in the axilla or may be because of the long evolution of the lesion (almost 10 years without treatment).
The diagnosis of this entity is based on clinical and histological findings. In opposition to acanthosis nigricans, RAVEN does not have a predilection for intertrigenous areas.4 In the literature RAVEN is not associated with endocrinopathy, with the exception of two cases (Hashimoto's thyroiditis and obesity).5 The clinical course is unpredictable. Several locations have been reported: face, scalp, chest, abdomen, periumbilical area, back and thigh.
RAVEN is a benign naevus but early diagnosis and intervention may be important in selected patients for a better cosmetic outcome. Owing to its rarity there are no any guidelines for treatment. Topical tretinoin cream,6 5-fluorouracil cream, cryosurgery, LASER and surgery have been tried. Several sessions of CO2 LASER are the most common reported treatment in the literature for RAVEN. New molecules inhibiting fibroblast growth factor receptor three are being investigated for other disorders such as acute myeloid leukaemia and may in the future prove useful for these benign lesions.3
Learning points.
Rounded and velvety epidermal naevus (RAVEN) can be only located to the axilla and have a marked exophytic growth.
Correct clinical and histological correlation is needed to make the differential diagnosis with the more common acanthosis nigricans and classical epidermal naevus.
In almost every case reported, RAVEN has not been associated with any endocrinopathy.
Early diagnosis and intervention may be important for a better cosmetic outcome.
Footnotes
Contributors: TM contributed to conception, design, analysis and interpretation of data, drafting of the manuscript and gave the final approval; CA contributed to acquisition of the data, analysis and interpretation of the data, and gave the final approval; RC contributed to critical revision of the manuscript and gave the final approval.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Curth HO. Unilateral epidermal naevus resembling acanthosis nigricans. Br J Dermatol 1976;95:433–6. [DOI] [PubMed] [Google Scholar]
- 2.Petit A, Lemarchand-Venencie F, Pinquier L et al. Nevoid acanthosis nigricans or RAVEN (rounded and velvety epidermal nevus): three cases. Ann Dermatol Venereol 2012;139:183–8. [DOI] [PubMed] [Google Scholar]
- 3.Waal AC, van Rossum MM, Bovenschen HJ. Extensive segmental acanthosis nigricans form of epidermal nevus. Dermatol Online J 2010;16:7. [PubMed] [Google Scholar]
- 4.Ersoy-Evans S, Sahin S, Mancini AJ et al. The acanthosis nigricans form of epidermal nevus. J Am Acad Dermatol 2006;55:696–8. [DOI] [PubMed] [Google Scholar]
- 5.Jeong JS, Lee JY, Yoon TY. Unilateral nevoid acanthosis nigricans with a submammary location. Ann Dermatol 2011;23:95–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishnaram AS. Unilateral nevoid acanthosis nigricans and neurofibromatosis 1: an unusual association. Indian J Dermatol Venereol Leprol 2010;76:715–17. [DOI] [PubMed] [Google Scholar]


