Abstract
In this paper, we report two cases of a 62-year-old patient presented with blurred vision and a 45-year-old male diagnosed with multiple myeloma who was referred from the Department of Oncology. Slit-lamp examination, in vivo confocal microscopy (IVCM), systemic work-up and serum protein electrophoresis were obtained. In both patients, slit-lamp findings revealed bilateral diffuse subepithelial and anterior stromal crystals and IVCM showed highly reflective deposits in the corneal epithelium and stroma. The first patient was eventually diagnosed with monoclonal gammopathy of undetermined significance following bone marrow biopsy and systemic evaluation. Unusual corneal deposits may constitute the first sign of monoclonal gammopathies. IVCM may be helpful in showing the crystalline nature of the corneal deposits and guiding the clinician to the diagnosis of gammopathies. Both ophthalmologists and oncologists should be aware that corneal deposits may herald a life-threatening hematologic disease.
Keywords: Corneal deposits, in vivo confocal microscopy, monoclonal gammopathy of undetermined significance, multiple myeloma
Corneal crystals have been recognized in association with paraproteinemias that result in excessive immunoglobulin (Ig) production such as multiple myeloma (MM), Waldenström's macroglobulinemia or benign monoclonal gammopathy.[1] In addition to the Ig deposition, corneal crystalline deposits may occur in a variety of conditions, including cystinosis, Schnyder's dystrophy, Bietti's crystalline dystrophy, tyrosinemia type II and Meesmann's dystrophy. Based on electron microscopic (EM) studies performed on involved corneas, the extent of involvement is variable; deposits may be observed only in epithelial layers, in the stroma or they could be distributed diffusely throughout the entire corneal layers.[1,2,3] In vivo confocal microscopy (IVCM) may be helpful in showing the crystalline nature of the corneal deposits and guiding the clinician to the diagnosis of gammopathies. Thus, we aimed to report the clinical and IVCM findings of corneal deposits in two patients with monoclonal gammopathy.
Case Reports
Case 1
The first case is about a 62-year-old female patient had a 3-month history of blurred vision without any systemic complaints. Her medical history was negative for any systemic disease and she was not on any medication. Her best-corrected visual acuity (BCVA) was 20/20 in both eyes. Slit-lamp examination disclosed bilateral diffuse gray-white deposits at the level of the anterior stroma [Fig. 1]. Fundus examination was within the normal limits. Corneal pachymetry disclosed central corneal thickness of 548 μm for right eye oculus dexter and 531 μm for left eye oculus sinister. IVCM (Confoscan 3.0, Nidek, Vigonza, Italy) showed highly reflective, granular and spindle-shaped crystalline deposits most densely at the level of anterior stroma [Fig. 2a and b] and with crystal density decreasing toward the posterior stroma. There was only scarce infiltration of the basal epithelium with crystals. The subbasal nerves appeared to be spared from crystal deposition. The endothelium and the predescemetic layer appeared to be uninvolved and without any deposits. The length and the diameter of the crystalline deposits ranged between 1.5-55 μm and 1-4 μm, respectively [Fig. 2]. As the corneal findings appeared consistent with those observed in gammopathy related deposits, a hematology consultation was requested. Serologic work-up revealed elevated IgA (596 mg/dL, normal range 70-400 mg/dL). The IgG level was 1210 mg/dL (normal range 700-1600 mg/dL) and the IgM level was 202 mg/dL (normal range 40-230 mg/dL). Serum immunoelectrophoresis revealed a monoclonal gammopathy involving IgA-kappa light chain. Bone marrow biopsy showed elevated plasma cell count (25%; normal range <10%) and these findings were consistent with monoclonal gammopathy of undetermined significance (MGUS). The patient was put on surveillance by the Department of Oncology and is being monitored for conversion to MM.
Figure 1.
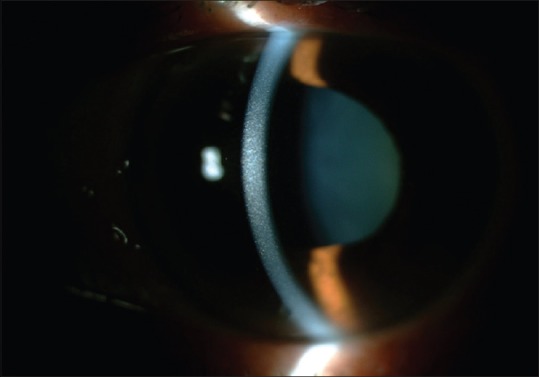
Diffuse infiltration of the central and peripheral cornea without any signs of epitheliopathy in the case with immunoglobulin A-kappa monoclonal gammopathy of unknown significance
Figure 2.
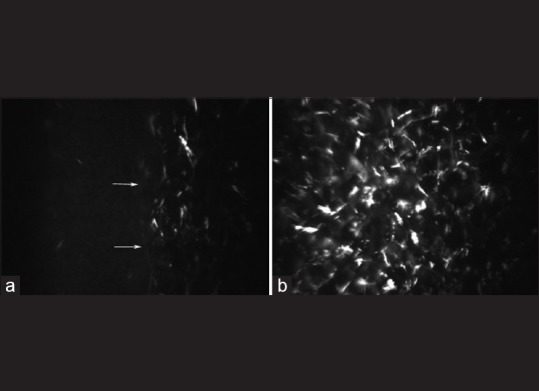
In vivo confocal microscopy images of case number 1. (a) Immunoprotein deposition at the level of anterior stroma with sparing of the epithelium. The epithelium-stromal junction is highlighted with arrows. (b) Presence of both granular and spindle-like hyperintense deposits in the corneal stroma
Case 2
The second case is a 45-year-old male was diagnosed with IgG-kappa type MM 6-month prior to his initial eye examination. His bone marrow biopsy had revealed abnormal plasmoid cells [Fig. 3a], which stained positively with the CD-138 (Syndecan-1), a diagnostic marker for plasma and MM cells [Fig. 3b]. On his follow-up visits, the patient was referred for burning sensation in both eyes. On examination, his BCVA was 20/20 in both eyes. Slit-lamp examination revealed superficially located diffuse corneal crystalline deposits without any signs of overt epitheliopathy. Fundus examination was normal. IVCM demonstrated numerous discrete, partially hyper-reflective linear crystalline deposits at the level of the corneal epithelium [Fig. 4a]. No deposits were detected in stromal layers or the endothelium [Fig. 4b and c]. These crystals were observed as having a tubular morphology with a central hollow lumen, length ranges between 30 and 40 μm and thickness ranges between 2 and 10 μm in diameter. The patient had been diagnosed with bone plasmacytoma and spinal metastasis at the time of his initial eye examination. The patient succumbed to the complications of MM 6-month later.
Figure 3.
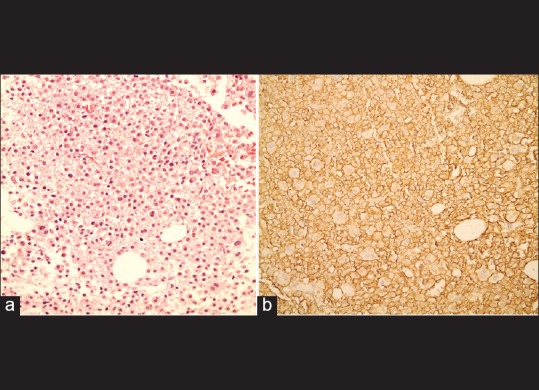
(a) Depiction of the abnormal plasma cells in the bone marrow biopsy of the patient with immunoglobulin G-kappa multiple myeloma. (b) Diffuse staining of the bone marrow with CD-138 marker
Figure 4.

In vivo confocal microscopy images of case number 2. (a) Dense infiltration of the corneal epithelium with typical centrally hypointense slender crystalline deposits. (b) An oblique section at the epithelium-cornea junction depicting the localization of the immunoprotein deposits to the epithelial layer with uninvolved stromal appearance. The characteristic morphology of the immunoprotein deposit with a central hypointense lumen and hyperintense borders is depicted with arrows. (c) The endothelium appeared to be devoid of crystalline infiltration and of normal cellular morphology
Discussion
Immunoprotein crystals are characterized by the presence of parallel, banded crystalloid or granular deposits, which are sometimes observed to have hexagonal cross-sectional appearances.[1] In 2002, Buerk and Tu published the first report of corneal Ig crystals in a case of IgG-kappa gammaglobulinemia as imaged with IVCM.[4] They observed discrete, hyper-reflective globular structures in the epithelium and anterior stroma.[4] Although the status of the endothelium was not reported, a decrease in the extent of crystal deposition following systemic chemotherapy was noted. In a more recent report by Steinberg et al.,[5] spindle-shaped diffusely infiltrating crystalline structures were observed throughout the entire cornea using laser IVCM in a case of IgG-kappa producing MM. The endothelium appeared normal in that case. To the best of our knowledge, our report is the third one in the literature to detail the in vivo ultrastructural characteristics of crystalline keratopathy associated with gammopathies using IVCM. Our findings are significant in certain aspects. In case number 2 with IgG-kappa MM, IVCM revealed hollow tubular structures with hypointense central lumen and a relatively more hyperintense outer wall [Fig 2]. This appearance of the IgG-kappa crystals was noted to closely replicate their EM appearance.[1,2,3,4,5,6] In an EM study by Henderson et al.,[6] crystals-related to IgG-kappa gammopathies appeared as thick-walled deposits 40 nm in diameter resembling “hollow rods” with a diameter of 30 nm and exhibiting a central lucent core. As such, the IVCM features of the immunoprotein deposits may assist in the differential diagnosis of crystalline keratopathies by pointing out to the Ig origin thus ensuring earlier work-up and treatment of a potentially fatal plasma cell disorder. A second important finding is the almost purely epithelial involvement in case number 2 with a demarcation zone at the level of Bowman's membrane lending support to the tear route of entry of the deposits into the cornea. Steuhl et al.[7] and Cherry et al.[2] had demonstrated the presence of Igs in the ocular tears of an IgG-kappa monoclonal gammopathy patient who had deposits limited to the corneal epithelium. Both the epithelium and stromal layers have been shown to be infiltrated in the setting of IgG-kappa gammopathy; however biopsy proven epithelium-only crystal deposition has been demonstrated in a limited number of reports.[8] The findings of case number 2 shows that corneal deposits related to IgG-kappa gammopathy could be found exclusively limited to the epithelium. In contrast, the Ig deposits in case number 1 diagnosed with MGUS associated IgA-gammopathy involved the anterior and midstroma with sparing of the epithelium and endothelial layers.
We did not find any sign of endothelial involvement in our cases. This is in agreement with the reports of Buerk and Tu[4] and Steinberg et al.[5] in which the endothelium was uninvolved in their cases with IgG-kappa gammopathy as images with IVCM. There are only scattered reports describing endothelial involvement; in the majority of biopsy proven cases, the deposits have been found to be localized to the epithelium and or stroma.[7,9] It may be difficult to differentiate direct endothelial from predescemetic localization using light to electron microscopy and IVCM may contribute in identifying endothelial involvement in paraproteinemias.[10]
Conclusion
In vivo confocal microscopy is a valuable diagnostic tool that can assist in the identification of immunoprotein deposits as well as determination of the extent of corneal involvement in gammopathies. Untreated, paraproteinemias may cause a progressive visual loss and more importantly, life-threatening systemic involvement. The ophthalmologist may be the initial physician to evaluate such a patient with undiagnosed paraproteinemia and in that setting, IVCM may have a role in identifying the presence and hinting to the nature of the corneal deposits.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Garibaldi DC, Gottsch J, de la Cruz Z, Haas M, Green WR. Immunotactoid keratopathy: A clinicopathologic case report and a review of reports of corneal involvement in systemic paraproteinemias. Surv Ophthalmol. 2005;50:61–80. doi: 10.1016/j.survophthal.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Cherry PM, Kraft S, McGowan H, Ghosh M, Shenken E. Corneal and conjunctival deposits in monoclonal gammopathy. Can J Ophthalmol. 1983;18:143–9. [PubMed] [Google Scholar]
- 3.Kawamura H, Seo T, Watanabe I, Ito I, Shirasawa H, Muranaka Y. A case of corneal crystalline deposits associated with multiple myeloma. Nihon Ganka Gakkai Zasshi. 1988;92:1473–8. [PubMed] [Google Scholar]
- 4.Buerk BM, Tu E. Confocal microscopy in multiple myeloma crystalline keratopathy. Cornea. 2002;21:619–20. doi: 10.1097/00003226-200208000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Steinberg J, Eddy MT, Katz T, Matthiessen E, Fricke OH, Richard G, et al. Bilateral crystalline corneal deposits as first clinical manifestation of monoclonal gammopathy: A case report. Case Rep Ophthalmol. 2011;2:222–7. doi: 10.1159/000330334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henderson DW, Stirling JW, Lipsett J, Rozenbilds MA, Roberts-Thomson PJ, Coster DJ. Paraproteinemic crystalloidal keratopathy: An ultrastructural study of two cases, including immunoelectron microscopy. Ultrastruct Pathol. 1993;17:643–68. doi: 10.3109/01913129309027800. [DOI] [PubMed] [Google Scholar]
- 7.Steuhl KP, Knorr M, Rohrbach JM, Lisch W, Kaiserling E, Thiel HJ. Paraproteinemic corneal deposits in plasma cell myeloma. Am J Ophthalmol. 1991;111:312–8. doi: 10.1016/s0002-9394(14)72315-3. [DOI] [PubMed] [Google Scholar]
- 8.Perry HD, Donnenfeld ED, Font RL. Intraepithelial corneal immunoglobulin crystals in IgG-kappa multiple myeloma. Cornea. 1993;12:448–50. doi: 10.1097/00003226-199309000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto T, Hishida A, Honda N, Ito I, Shirasawa H, Nagase M. Crystal-storing histiocytosis and crystalline tissue deposition in multiple myeloma. Arch Pathol Lab Med. 1991;115:351–4. [PubMed] [Google Scholar]
- 10.Font RL, Matoba AY, Prabhakaran VC. IgG-kappa immunoglobulin deposits involving the predescemetic region in a patient with multiple myeloma. Cornea. 2006;25:1237–9. doi: 10.1097/01.ico.0000240094.78095.f5. [DOI] [PubMed] [Google Scholar]


