Abstract
Background:
The Indian population suffers with significant burden of mental illness. The prevalence rate and its association with age and other demographic indicators are needed for planning purpose.
Objective:
This study attempted to calculate age-wise prevalence of mental illness for rural and urban settings, and its association with age.
Materials and Methods:
Data published in National Sample Survey Organization (2002) report on disability is used for the analysis. Spearman correlation for strength of association, z-test for difference in prevalence, and regression statistics for predicting the prevalence rate of mental illness are used.
Result:
Overall population have 14.9/1000 prevalence of mental illness. It is higher in rural setting 17.1/1000 than urban 12.7/1000 (P < 0.001). There is a strong correlation found with age in rural (ϱ = 0.910, P = 0.001) and urban (ϱ = 0.940, P = 0.001).
Conclusion:
Results of this study confirm other epidemiological research in India. Large-population epidemiological studies are recommended.
Keywords: Age, India, mental illness, national sample survey organization report, prevalence, rural, urban
Introduction
According to the US Department of Health and Human Services, mental illness is characterized by alterations in thinking, mood or behavior associated with distress and impaired function.[1] It could refer to one or more mental disorders at a time. Mental illness is a global public health concern. According to the World Health Organization, one out of four (25%) persons is affected with some kind of mental illness.[2] The prevalence of mental disorders is higher in developed countries, but the global burden of untreated mental disease is higher in developing nations.[2,3] Eighty percent (80%) of the population suffering with mental illness lives in low-and middle-income (LAMI) countries.[2,4,5] The presence of mental illness does not affects only the individual and his personal, social, educational and occupational life, but it also makes his entire family to suffer from negative consequences.[6,7]
Considering the fact that India has 17.5% of the world's population[2] , the number of people suffering with mental illness is assumed to be huge. It is highly crucial for India to have a true estimate of the number or prevalence of mental illness in the nation. So far, several determinants of mental illness have been identified. Poverty, genetic and environmental factors: Stress and abuse in childhood stage are common associates of mental disorders in the nation.[2,8] Distribution of mental disorders also varies with age, socioeconomic status, gender and rural and urban settings.[9,10,11] Compared to urban settings, people in rural poor communities have higher accessibility and affordability challenges in receiving professional help.[12,13]
The prevalence of mental illness appears higher in children due to behavioral and emotional disorders. Those are often associated with learning difficulties, poor parenting and schooling, while age-related dementia, and other cognitive disorders increase with age.[14,15,16,17,18,19] Because mental disorders differ with age, the nature of psychiatric and psychological service requirements also vary. For the purpose of planning and provision of services, age-related prevalence of mental illnesses is very important. A high proportion of the Indian population resides in rural settings with significantly higher poverty rates than the urban setting. Because poverty is an important social determinant of mental disorders, the differences in prevalence between rural and urban settings also need to be studied for planning and development of services to the population.[11,20]
Objective
This study examines the correlation between age and prevalence of mental illness, and compares rural and urban settings.
Materials and Methods
Secondary data from the Indian National Sample Survey Organization (NSSO) 2002 are used for analysis. This report is named-NSS 58th round, report no. 485 (58/26/1), Disabled Person in India, 2002, and available in the public domain.[21] This was the first time mental illness and intellectual disability were covered by NSSO in the disability survey. Data on mental illness and intellectual disability are presented separately and in combination in this report, for planning purposes. This survey was performed by non-medical personnel. In designing the questionnaire, help from consultants with medical background was obtained with regard to diagnosis of mental illness.[21] This helped the survey personnel to identify accurately, the person with mental illness. The questionnaire was pre-tested before use. Geographically, the whole nation was covered in this survey except Leh and Kargil districts of Jammu Kashmir, interior villages of Nagaland, Andaman and Nicobar (which, together, constitute less than 1% of the total Indian population) due to challenges in accessibility. With the help of experts, multi-stage sampling was used and the sample size was calculated. The entire survey was conducted in 6 months, beginning from July to December 2002. Data in this report are presented by gender and rural or urban setting on several variables in many tables of the report and appendixes. Explanation on several variables is also offered in this report. For this research, data were taken from the text of this report, and used to develop tables for statistical analysis.
Statistical analyses
Spearman correlation (ϱ) was computed for age and prevalence, z-test between rural and urban, and least square regression model were used to determine the association of prevalence rate with age in rural and urban populations. Statistical Package for Social Sciences (SPSS) version-21, for statistical analysis was used.
Results
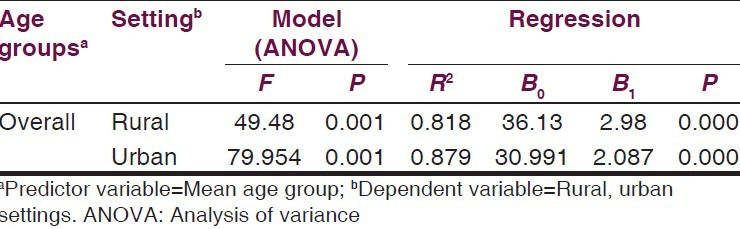
Our analysis indicated that the prevalence of mental illness was strongly correlated with the age in rural (ϱ=0.910, P = 0.001), and urban (ϱ=0.940, P = 0.001) population groups [Table 1]. However, the rural prevalence rate was significantly different from the urban population (z = 8.10, P = 0.001) [Table 2]. The estimated cumulative mean prevalence of mental illness was 1,490.5 cases/100,000 in the nation. The rural population had significantly higher rate of mental illness compared to the urban [Table 2 and Figure 1]. In the ANOVA, F = 49.486, P = 0.001 indicate a statistically significant strong association between age and mental illness in rural populations in India, where R2 = 0.81, demonstrates that 81% of the variance in prevalence of mental illness is explained by age the rural model. However, with ANOVA of F = 79.954, P = 0.001, in the urban setting, age is also strongly associate with mental illness, while an R2 = 0.87, indicates 87% of the variance in the prevalence is explained by age. In further predicting prevalence of mental illness based on age, the least-square regression equation was obtained. According to this statistical predictive model, age increase of one year predicted an increase in prevalence of 2.98 persons per 100,000 rural population. However, in the urban population, the same increase in age predicts a 2.087 persons per 100,000 thousand increase in prevalence [Table 3 and Figure 1].
Table 1.
Correlation with age separated by rural and urban setting
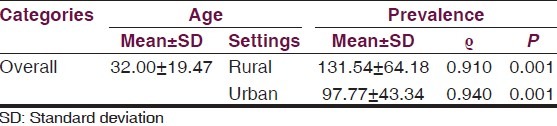
Table 2.
Prevalence of mental illness in different age groups data from NSSO report: Case per 100,000

Figure 1.
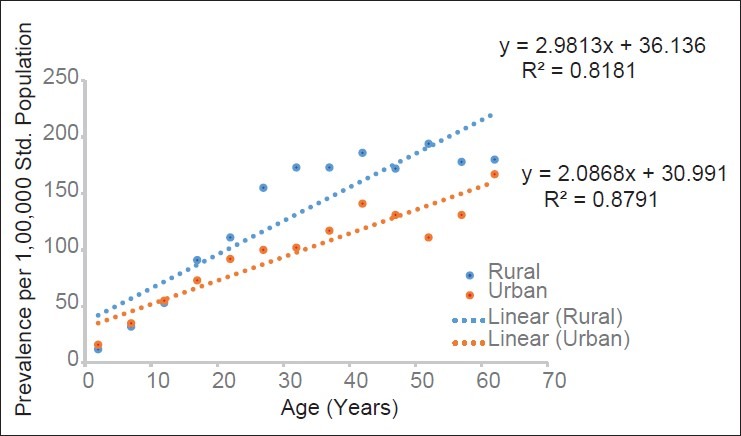
Prevalence of mental illness in rural and urban India by age (constructed from table 1)
Table 3.
Regression analysis of age with mental illness in rural and urban settings of India
Discussion
This study finds that age is an important predictor of mental illness in the population irrespective of where people live, rural or urban. Mental illness is linearly associated with age and these findings agree with prevalence studies conducted previously.[10,22] However, in another epidemiological study, the association of age with psychiatric illness among young children below the age of 3 years was found higher than for children in age range of 12-16 years.[9]
This study found that the cumulative prevalence rate in rural (17.10/1,000), urban (12.7/1,000) and in combined population in the nation was 14.90 persons per 1,000. This is also consistent with several studies.[8,9,10,14,15,19,23,24] An epidemiological review of prevalence studies of psychiatric disorders from, 1960 to 2009 conducted by Math and Srina, et al. (2010) found that the prevalence of mental illness falls in the range of 9.5-370 persons per 1000. The wide variation in prevalence rate is attributed to several factors such as diagnostic criteria, methodology adapted in survey, lower sample size, and the type of instruments used in screening.[23,25] The prevalence estimated in this study falls in the lower side of the spectrum found by Math and Srinivasaraju.[24] Only two studies have found such low prevalence rates of mental illness in India. Both were conducted in South India. Mehta, et al. (1985)[26] estimated prevalence of 14.5/1000 in rural population in Vellore; Shaji, et al. (1995)[27] also observed closely similar prevalence rate of 14.57/1000 in Ernakulum.[27] A prevalence study conducted by Surya (1964),[28] also in southern India has estimated a low prevalence of mental illness (9.5/1000) in urban population in Pondicherry.
Compared to urban population in India, this study found significantly higher prevalence of mental illness in rural population. Considering the fact that larger proportions of the rural population live in poverty, poverty may be a significant determinant of mental illness. The findings of this study can be supported with other studies conducted in low and middle income countries.[11,29,30,31,32] However, the difference in prevalence rate based on rural and urban settings is not well supported in many Indian epidemiological studies,[23,25,33] except one, that estimated psychiatric morbidity in children and adolescents.[9]
The findings of this study agree with other studies. Researchers have reported that the prevalence rate of psychiatric disorders is underreported in India as compared to the developed nations.[25] Until now, most of the prevalence studies are conducted with the average population of 5,000 or less,[23] with many of the southern states of India, overrepresented in survey than any other study in the nation. Under this survey, 45,571 households, in 4637 randomly selected villages, and 24,731 in urban blocks were interviewed for mental illness. Random selection of villages and urban blocks in different states of the country makes the research data and its findings, representative of the different socioeconomic groups, and caste. Despite the fact that this survey is much more representative of the entire population of the country, its findings have limited scope in representing true estimation of prevalence rate, association with the age, and difference in two settings, because of the limitations of the survey itself.
The NSSO report, on which this study is based, does not provide information on which ICD standards definitions were used, how surveyors were prepared for survey, what were their trainings and how mental disorders were confirmed. What instruments were used, and what was the reliability of those instruments. Case definition used in the survey was also vague, which might have covered few persons with intellectual disabilities by chance or excluded mentally ill people mistakenly, considering them intellectually disabled. To keep balance, this survey identified more people with severe mental illness, while people with mild mental illness might have remained unidentified and uncounted.
Conclusion
Despite its limitations, the findings of this study identified high prevalence rates of mental illness in India and its association with age and rural settings. Compared to other studies, this study is based on larger sample size. In future, large epidemiological population studies are suggested to identify psychosocial determinants of mental illness more precisely.
Acknowledgement
Authors sincerely thank all anonymous researchers and surveyor of the NSSO report.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services; Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. U.S. Department of Health and Human Services; pp. 1–25. [Google Scholar]
- 2.World Health Organization (WHO) ECOSOC Meeting, Addressing non-communicable diseases and mental health: Major challenges to sustainable development in the 21st century, Discussion Paper: Mental health, poverty and development. [Online] 2009. [Last accessed on 2014 June 17]. Available from: http://www.who.int/nmh/publications/discussion_paper_en.pdf .
- 3.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Boer HM, Mula M, Sander JW. The global burden and stigma of epilepsy. Epilepsy Behav. 2008;12:540–6. doi: 10.1016/j.yebeh.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 5.Bertolote JM, Fleischmann A, De Leo D, Wasserman D. Psychiatric diagnoses and suicide: Revisiting the evidence. Crisis. 2004;25:147–55. doi: 10.1027/0227-5910.25.4.147. [DOI] [PubMed] [Google Scholar]
- 6.Walton-Moss B, Gerson L, Rose L. Effects of mental illness on family quality of life. Issues Ment Health Nurs. 2005;26:627–42. doi: 10.1080/01612840590959506. [DOI] [PubMed] [Google Scholar]
- 7.Tsang HW, Tam PK, Chan F, Cheung WM. Sources of burdens on families of individuals with mental illness. Int J Rehabil Res. 2003;26:123–30. doi: 10.1097/00004356-200306000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Havenaar JM, Geerlings MI, Vivian L, Collinson M, Robertson B. Common mental health problems in historically disadvantaged urban and rural communities in South Africa: Prevalence and risk factors. Soc Psychiatry Psychiatr Epidemiol. 2008;43:209–15. doi: 10.1007/s00127-007-0294-9. [DOI] [PubMed] [Google Scholar]
- 9.Srinath S, Girimaji SC, Gururaj G, Seshadri S, Subbakrishna DK, Bhola P, et al. Epidemiological study of child and adolescent psychiatric disorders in urban and rural areas of Bangalore, India. Indian J Med Res. 2005;122:67–79. [PubMed] [Google Scholar]
- 10.Ghosh AB, Banerjee G, Biswas D. Psychiatric morbidity in a sub-Himalayan tribal community: An epidemiological study. Indian J Psychiatry. 2004;46:324–32. [PMC free article] [PubMed] [Google Scholar]
- 11.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81:609–15. [PMC free article] [PubMed] [Google Scholar]
- 12.Srinivasa Murthy R, Kishore Kumar KV, Chisholm D, Thomas T, Sekar K, Chandrashekari CR. Community outreach for untreated schizophrenia in rural India: A follow-up study of symptoms, disability, family burden and costs. Psychol Med. 2005;35:341–51. doi: 10.1017/s0033291704003551. [DOI] [PubMed] [Google Scholar]
- 13.Chatterjee S, Patel V, Chatterjee A, Weiss HA. Evaluation of a community-based rehabilitation model for chronic schizophrenia in rural India. Br J Psychiatry. 2003;182:57–62. doi: 10.1192/bjp.182.1.57. [DOI] [PubMed] [Google Scholar]
- 14.Emerson E. Prevalence of psychiatric disorders in children and adolescents with and without intellectual disability. J Intellect Disabil Res. 2003;47:51–8. doi: 10.1046/j.1365-2788.2003.00464.x. [DOI] [PubMed] [Google Scholar]
- 15.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–44. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 16.Lavigne JV, Gibbons RD, Christoffel KK, Arend R, Rosenbaum D, Binns H, et al. Prevalence rates and correlates of psychiatric disorders among preschool children. J Am Acad Child Adolesc Psychiatry. 1996;35:204–14. doi: 10.1097/00004583-199602000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Graham JE, Rockwood K, Beattie BL, Eastwood R, Gauthier S, Tuokko H, et al. Prevalence and severity of cognitive impairment with and without dementia in an elderly population. Lancet. 1997;349:1793–6. doi: 10.1016/S0140-6736(97)01007-6. [DOI] [PubMed] [Google Scholar]
- 18.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: A global public-health challenge. Lancet. 2007;369:1302–13. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 19.Shaji S, Bose S, Verghese A. Prevalence of dementia in an urban population in Kerala, India. Br J Psychiatry. 2005;186:136–40. doi: 10.1192/bjp.186.2.136. [DOI] [PubMed] [Google Scholar]
- 20.Thara R, Padmavati R, Srinivasan TN. Focus on psychiatry in India. Br J Psychiatry. 2004;184:366–73. doi: 10.1192/bjp.184.4.366. [DOI] [PubMed] [Google Scholar]
- 21.National Sample Survey Organization (NSSO) Ministry of Statistics and Programme Implementation Government of India. Disabled Persons in India, NSS 58th round (July - December 2002) Report No. 485 (58/26/1) December 2003, New Delhi. [Online] 2003. [Last accessed on 2014 Jun 18]. Available from: http://www.domain.b.com/economy/general/2005/pdf/Disability_in_India.pdf .
- 22.Nandi DN, Mukherjee SP, Boral GC, Banerjee G, Ghosh A, Ajmany S, et al. Prevalence of Psychiatric morbidity in two tribal communities in certain villages of West Bengal: A cross cultural study. Indian J Psychiatry. 1977;19:2–12. [Google Scholar]
- 23.Math SB, Chandrashekar CR, Bhugra D. Psychiatric epidemiology in India. Indian J Med Res. 2007;126:183–92. [PubMed] [Google Scholar]
- 24.Math SB, Srinivasaraju R. Indian Psychiatric epidemiological studies: Learning from the past. Indian J Psychiatry. 2010;52(Suppl 1):S95–S103. doi: 10.4103/0019-5545.69220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhola P, Kapur M. Child and adolescent psychiatric epidemiology in India. Indian J Psychiatry. 2003;45:208–17. [PMC free article] [PubMed] [Google Scholar]
- 26.Mehta P, Joseph A, Verghese A. An epidemiological study of psychiatric disorders in a rural area in Tamil Nadu. Indian J Psychiatry. 1985;27:153–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Shaji S, Verghese A, Promodu K, George B, Shibu VP. Prevalence of priority psychiatric disorders in a rural area of Kerala. Indian J Psychiatry. 1995;37:91–6. [PMC free article] [PubMed] [Google Scholar]
- 28.Surya NC. Mental morbidity in Pondicherry. Transaction-4, Bangalore: All India Institute of Mental Health. 1964:50–61. [Google Scholar]
- 29.Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, et al. Poverty and common mental disorders in low and middle income countries: A systematic review. Soc Sci Med. 2010;71:517–28. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhide S, Mehta AK. Chronic Poverty in Rural India: Issues and findings from panel data. J Hum Dev Capab. 2004;5:195–209. [Google Scholar]
- 31.Meenakshi JV, Ray R. Impact of household size and family composition on poverty in rural India. J Policy Model. 2002;24:539–59. [Google Scholar]
- 32.Murthy RS, Lakshminarayana R. Is it possible to carry out high-quality epidemiological research in psychiatry with limited resources? Curr Opin Psychiatry. 2005;18:565–71. doi: 10.1097/01.yco.0000179499.23311.f3. [DOI] [PubMed] [Google Scholar]
- 33.Ganguli HC. Epidemiological findings on prevalence of mental disorders in India. Indian J Psychiatry. 2000;42:14–20. [PMC free article] [PubMed] [Google Scholar]


