Abstract
Objective:
Large increases in the use of antidepressants (ADs) were reported in the past 2 decades in many countries, including Canada. Our objective was to determine whether this pattern of increasing use has continued, using data from a 2012 national mental health survey.
Method:
During the past 2 decades, a series of Canadian national health surveys have evaluated AD use in the household population. Some of these surveys have assessed past 2-day use whereas others have assessed self-reported past-month use. We applied meta-regression methods as a methodological strategy to address this heterogeneity and to examine long-term trends, incorporating 2012 data.
Results:
In keeping with prior reports, AD use rapidly increased in the 1990s and early 2000s. However, the 2012 data suggest that these increases have slowed or perhaps even stopped in recent years. A post hoc examination of longitudinal data from the National Population Health Survey reinforced the impression of a levelling off in the use of these medications.
Conclusion:
The frequency of AD use may now be stabilizing in the Canadian population. This emerging steady state may reflect a contemporary balance between the perceived need, perceived effectiveness, and acceptability of these medications in the general population.
Keywords: major depressive episode, major depression, epidemiologic studies, time trends, cross-sectional studies
Abstract
Objectif :
D’importantes augmentations de l’utilisation d’antidépresseurs (AD) ont été signalées au cours des 20 dernières années dans de nombreux pays, dont le Canada. Notre objectif était de déterminer si ce modèle d’utilisation croissante continue, à l’aide de données d’une enquête nationale de 2012 sur la santé mentale.
Méthode :
Au cours des 20 dernières années, une série d’enquêtes nationales canadiennes sur la santé ont évalué l’utilisation d’AD dans la population des ménages. Certaines de ces enquêtes ont évalué l’utilisation des 2 jours précédents alors que d’autres ont évalué l’utilisation auto-déclarée du mois précédent. Nous avons employé les méthodes de métarégression comme stratégie méthodologique pour traiter cette hétérogénéité et examiner les tendances à long terme, en incorporant les données de 2012.
Résultats :
Conformément aux études précédentes, l’utilisation des AD a augmenté en flèche dans les années 1990 et au début des années 2000. Toutefois, les données de 2012 suggèrent que ces augmentations ont ralenti ou peut-être même cessé ces dernières années. Un examen ultérieur des données longitudinales de l’Enquête nationale sur la santé de la population ont confirmé l’impression d’un ralentissement de l’utilisation de ces médicaments.
Conclusion :
La fréquence de l’utilisation des AD est peut-être en train de se stabiliser dans la population canadienne. Ce nouvel état stable peut refléter un équilibre contemporain entre le besoin perçu, l’efficacité perçue, et l’acceptabilité de ces médicaments dans la population générale.
Canadian trends in medication use are often difficult to discern from available epidemiologic data. Canadian provinces do not have universal drug coverage such that the frequency of use is not easy to determine from routinely available administrative data sources. While some provinces collect data on prescriptions filled at pharmacies, epidemiologic estimates have not often been reported from these sources. Also, such estimates reflect prescriptions filled rather than medications taken. A recent Organisation for Economic Cooperation and Development report using a defined daily dose methodology based on data from Saskatchewan and Manitoba ranked Canada third in the world in its use of ADs, behind only Iceland and Australia.1 This report documented increased use of ADs in most countries between 2000 and 2011, but did not include the United States, a country where a high frequency has previously been reported. For example, a 2011 report from the Centers for Disease Control and Prevention reported an 11% frequency of use in Americans over the age of 12.2 Various lines of evidence suggest that recent increases are due to an increased duration of use rather than an increased frequency of use.3,4 In the US study cited above,2 60% had been taking their AD for longer than 2 years.
A series of national health surveys conducted by Statistics Canada have collected data on medication use. These surveys, conducted during the past 2 decades, assessed medication use in different ways. For example, some surveys asked respondents to retrieve all of their medication containers and recorded a detailed account of all medications taken in the preceding 2 days. Other surveys merely asked respondents to report past-month use of various types of medications. Meta-regression methods provide tools for data synthesis in circumstances of study-level heterogeneity and we therefore adopted these methods to assist identification of temporal trends.
Methods
This planned analysis for our study used cross-sectional data files collected in early cycles of the NPHS,5 the general health iterations of the CCHS,6 and 2 mental health CCHS surveys: the CCHS 1.2,7 which was conducted in 2002, and the CCHS-MH,8 conducted in 2012. The NPHS and the 2 mental health surveys recorded the use of psychotropics during the past 2 days as a component of their data collection.
Clinical Implications
Prior to 2012, most estimates suggested a lower frequency of AD use in Quebec than in the rest of Canada. The difference was no longer evident in 2012.
About 5.5% of the Canadian population took ADs in 2012, a similar proportion to an estimate from a similar survey 10 years earlier.
While substantial increases have previously been reported, these results suggest that these increases have slowed or stopped in recent years.
Limitations
The accuracy of self-reported AD use is questionable. Both false-positive and -negative self-reports may occur.
The availability of data in recent years is limited, compared with the quantity of data collected in the 1990s and early 2000s.
Evidence in support of the idea that AD use has stopped increasing depends on a single study combined with data from a longitudinal study.
The NPHS and CCHS 1.2 recorded ATC codes, whereas the CCHS-MH recorded Drug Identification Numbers. The general health iterations of the CCHS included past-month medication use as an optional component in most of its cycles, such that the data collection did not include all provinces in all years. The item was as follows:
Now I’d like to ask a few questions about your use of medications, both prescription and over-the-counter. In the past-month, that is, from [date one month ago] to yesterday, did you take antidepressants, such as Prozac, Paxil or Effexor?
The question did not change over the years, but the examples provided in it did change. The CCHS general health surveys began collecting data in 2000–2001 (CCHS 1.1) and thereafter every 2 years until 2007, at which time an annual data collection cycle was initiated. Notably, neither the 2007 survey nor any subsequent surveys recorded medication use until the 2012 CCHS-MH. In addition to the recording of past 2-day use, the NPHS included self-report items assessing past-month AD use, providing a bridge for comparison of the 2 measurement strategies.
All of these studies can support inference to the Canadian household population when the data are analyzed using appropriate sampling weights and bootstrap variance estimation procedures. In this analysis, weighted frequency estimates and 95% confidence intervals were initially examined using forest plots. We quantified heterogeneity using the I2 statistic, which represents the proportion of variability across surveys that is due to heterogeneity. Random effects meta-regression was used to quantify changes over time and to adjust for study-level covariates. Time was represented as years since 1994 so that the intercept term represented a baseline estimate and the slope term represented change per year. As recommended by Higgins and Thompson,9 permutation tests (with n = 1000 Monte Carlo trials) were used to assess P values in the meta-regression models. The analyses used Stata’s10 metan command and were conducted in the Prairie Regional Data Centre at the University of Calgary.
In view of the existing literature, there was an expectation that continued increases in AD use would be observed. When this was not observed, a post hoc analysis was conducted, after obtaining Statistics Canada approval for incorporation of data from the NPHS longitudinal file. This data source was not designed for cross-sectional inference but did provide a source of estimates during the 2002 to 2012 interval. The available data consisted of past 2-day use, recorded using ATC codes.
Results
Table 1 summarizes the number of available observations on each of the outcome variables in each survey cycle for the primary data analysis.
Table 1.
Sample size availability from NPHS and CCHS surveysa
| Survey | Past 2-day use | Past-month use | Provinces past 2-day use | Provinces past-month use |
|---|---|---|---|---|
| NPHS 1994 | 15 255 | 14 700 | All | All |
| NPHS 1996 | 73 405 | 73 140 | All | All |
| NPHS 1998 | 15 250 | 15 230 | All | All |
| CCHS 2000 | n/a | 31 130 | n/a | Ontario |
| CCHS 1.2 2002 | 36 985 | n/a | All | n/a |
| CCHS 2003 | 28 185 | 24 125 | Quebec | Ontario, Saskatchewan, British Columbia |
| CCHS 2005 | n/a | 9170 | n/a | Newfoundland and Labrador, Nova Scotia |
| CCHS-MHa | 24 960 | n/a | All | n/a |
Owing to data release restrictions, these numbers are rounded to 5.
CCHS = Canadian Community Health Survey; CCHS 1.2 = Canadian Community Health Survey: Mental Health and Well-Being (2002); CCHS-MH = Canadian Community Health Survey—Mental Health (2012); n/a = not applicable; NPHS = National Population Health Survey
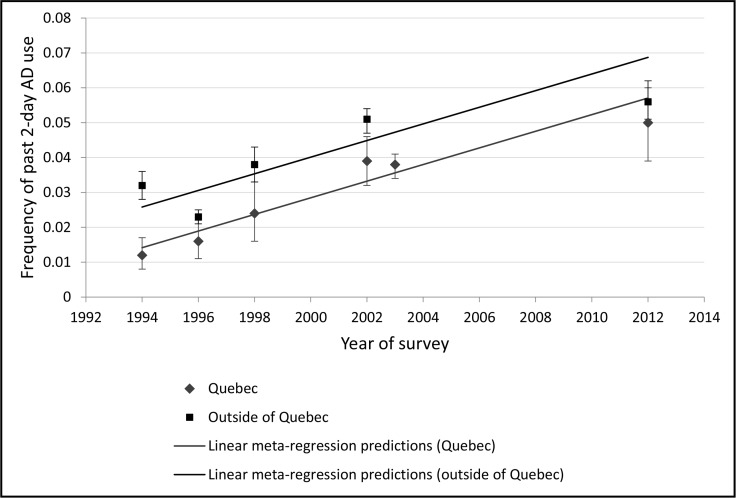
A preliminary examination of forest plots provided a visual impression of an overall increase in use during the early surveys, as expected. Also, predictably, the frequency of use was lower in surveys that assessed past 2-day use as compared with those that assessed past-month use. However, with stratification by province, there was also the suggestion of a lower frequency of use in Quebec. As a result, an indicator variable for Quebec residence was included in a meta-regression analysis along with the indicators of measurement strategy and time. The resulting model had significant terms for all of these variables (all P values < 0.02); however, the resulting linear regression equation underestimated the 2012 data by a substantial margin (Figure 1).
Figure 1.
Past 2-day AD use in Canada, by year, with population-weighted estimates and a linear meta-regression model
AD = antidepressant
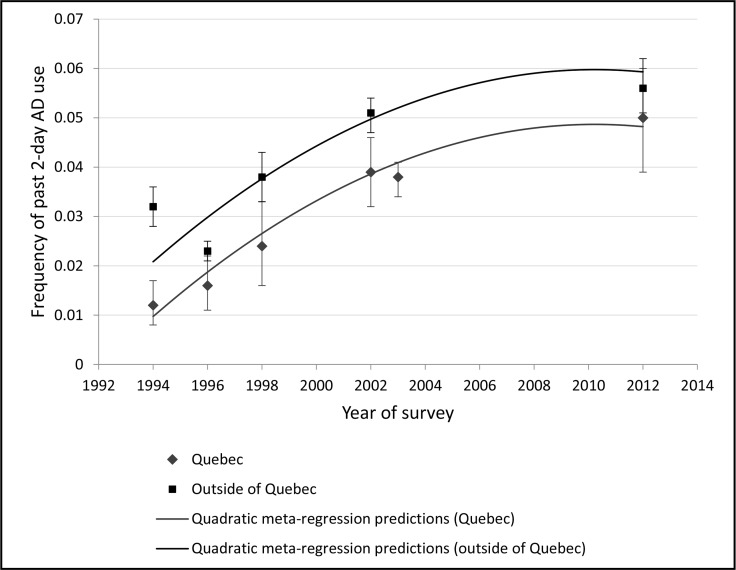
The linear meta-regression model presented in Figure 1 predicted a 6.9% frequency of use outside of Quebec and a 5.7% frequency of use in Quebec by 2012, whereas the actual estimates were 5.6% and 5.0%, respectively. Indeed, the 2012 estimates were similar to those collected 10 years earlier, an unexpected result given the world literature. The I2 from the linear model depicted in Figure 1 was 87%. Addition of a time squared term to the model (this model is subsequently referred to as a quadratic model) resulted in improved fit (Figure 2) and produced a slightly lower I2 at 80%. Both time (β = 0.005, t = 7.50, df = 15, P < 0.001) and time-squared (β = −0.0015, t = 3.98, df = 15, P = 0.001) were statistically significant in this model, as was Quebec residence (β = −0.011, t = 4.69, df = 15, P < 0.001) and measurement strategy (2-days as opposed to past-month) measurement (β = −0.0078, t = 3.20, df = 15, P = 0.006). Figure 2 presents population-weighted estimates and fitted values from this quadratic meta-regression model for past 2-day use. Using the permutation test, all of these effects remained statistically significant (all P < 0.02).
Figure 2.
Past 2-day AD use in Canada, by year. Population weighted estimates and a meta-regression model including a time squared term.
AD = antidepressant
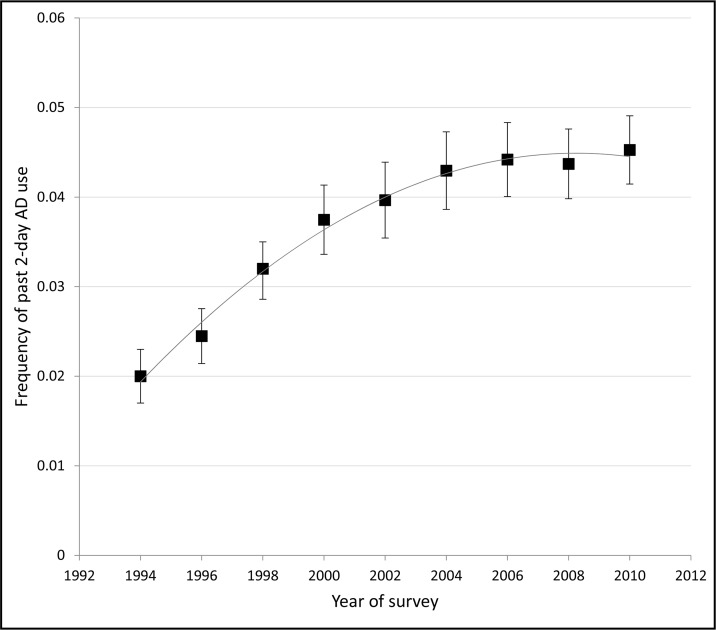
While the estimates reported above were suggestive of a nonlinear pattern, the availability of data between 2002 and 2012 was limited. Past-month, self-reported use was assessed in the 2003 CCHS 2.1 for the provinces of Ontario, Saskatchewan, and British Columbia, where the overall frequency was 6.3% (95% CI 5.9% to 6.8%) and in the 2005 CCHS in Newfoundland and Nova Scotia (frequency of use 6.7%, 95% CI 5.9% to 7.4%). Notably, these estimates are expected (see above) to be slightly less than 1% higher than the past 2-day estimates as they reflect past-month use. In view of the lack of data, estimates were also derived from the longitudinal file of the NPHS for all years for which they were possible. These estimates were based on the longitudinal file from the same survey that produced the cross-sectional estimates from the first 3 cycles, used in the primary analysis (see above). However, the longitudinal file was subject to attrition. In the NPHS, 69.7% of respondents were successfully followed either to the end of the study in 2010 or to when they left the sampling frame owing to death or institutionalization. The pattern is presented in Figure 3 and corroborates the idea that the frequency of use has levelled off.
Figure 3.
Estimates of past 2-day AD use from the 1994–2010 National Population Health Survey Longitudinal Filea
a Error bars represent 95% confidence intervals. The line is a trend line based on least squares fit of a model including a year-squared term. It does not derive from a meta-regression model.
AD = antidepressant
Discussion
A surprising result from the 2012 CCHS-MH was that the frequency of AD use in Canada did not increase to an appreciable extent from the CCHS 1.2 survey conducted 10 years earlier. The slope term from the linear model presented in Figure 1 was 0.24%, suggesting ongoing increases of about 1% every 4 years and of more than 2% over 10 years, but the actual change between 2002 and 2012 was only 0.5% (5.1% to 5.6%) outside of Quebec and 1.1% (3.9% to 5.0%) in Quebec. This modest increase was surprising as most countries are believed to have experienced large increases over the decade 2000–2011.1 Increases were also apparent in Canada up to 2002 (figures 1 to 3), but the 2012 estimate is too low to be consistent with a continued linear increase. Future estimates will be helpful to confirm the tentative conclusion that the rate of increase has slowed or stopped. The results of the 2012 survey may indicate that a steady state has emerged with the use of these medications.
The frequency of use of a medication in the population is related to the incidence of new use and the duration of use, the prevalence of use being about the product of the rate of new use multiplied by the average duration of use. As such, there are several theoretical interpretations for the apparent levelling off in the frequency: the rate of new use and (or) the mean duration of use may have stopped increasing. As noted above, available evidence suggests that the rate of new use stopped increasing some time ago.3,4 In the past, increasing AD use has elicited conflicting claims either of continued under-treatment or of excessive or inappropriate treatment. It is conceivable that the emergence of a steady state in the population reflects a summation of real-world utilitarian decisions concerning the actual tolerability and perceived benefits of these medications, with such factors probably having an effect primarily on the duration of use.
There are several limitations of the analysis reported here. First, the emphasis on synthesis of study-based estimates precludes consideration of individual-level determinants of AD use. Second, some of the changes over time may reflect demographic changes in the underlying population, as the sampling weights are designed to produce representative estimates in the year in which the data were collected. Also, the data from the NPHS longitudinal file are not weighted for cross-sectional estimation. Owing to attrition, the longitudinal NPHS sample may have become less representative of the household population over time. The slightly lower frequency of use in the 2010 NPHS (Figure 3), as opposed to the meta-regression model depicted in Figure 2, may reflect an impact of depression on the attrition from the longitudinal cohort.
Conclusions
After 2 decades of increasing use, the frequency of use of ADs appears to have levelled off in Canada.
Acknowledgments
Dr Patten is a Senior Health Scholar with Alberta Innovates, Health Solutions (AIHS). Dr Fiest was supported by a PhD Studentship from AIHS during the study period. The estimates reported in our paper derive used data collected by Statistics Canada, but the analysis and results are the sole responsibility of the authors and do not reflect the views of Statistics Canada. This work was supported by an operating grant from the Canadian Institutes of Health Research (MOP-130415).
Abbreviations
- AD
antidepressant
- ATC
Anatomical Therapeutic Chemical Classification System
- CCHS
Canadian Community Health Survey
- CCHS 1.2
Canadian Community Health Survey Mental Health and Well-being (2002)
- CCHS-MH
Canadian Community Health Survey—Mental Health (2012)
- NPHS
National Population Health Survey
References
- 1.Organisation for Economic Cooperation and Development (OECD) Health at a glance 2013: OECD indicators [Internet] Paris (FR): OECD; 2013. [cited 2014 May 2]. Available from: http://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2013_health_glance-2013-en. [Google Scholar]
- 2.Pratt LA, Brody DJ, Gu Q. Antidepressant use in persons aged 12 and over: United States, 2005–2008 [Internet] Atlanta (GA): Centers for Disease Control and Prevention; 2011. [cited 2014 May 2]. Available from: http://www.cdc.gov/nchs/data/databriefs/db76.htm. [Google Scholar]
- 3.Patten SB, Wang JL, Williams JV, et al. Frequency of antidepressant use in relation to recent and past major depressive episodes. Can J Psychiatry. 2010;55(8):532–535. doi: 10.1177/070674371005500808. [DOI] [PubMed] [Google Scholar]
- 4.Moore M, Yuen HM, Dunn N, et al. Explaining the rise in antidepressant prescribing: a descriptive study using the general practice research database. BMJ. 2009;339:b3999. doi: 10.1136/bmj.b3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Statistics Canada . National Population Health Survey—household component—cross-sectional (NPHS) [Internet] Ottawa (ON): Statistics Canada; 2007. [cited 2014 May 2]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3236&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 6.Statistics Canada . Canadian Community Health Survey—annual component [Internet] Ottawa (ON): Statistics Canada; 2013. [cited 2014 May 2]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 7.Gravel R, Béland Y. The Canadian Community Health Survey: mental health and wellbeing. Can J Psychiatry. 2005;50:573–579. doi: 10.1177/070674370505001002. [DOI] [PubMed] [Google Scholar]
- 8.Statistics Canada . Canadian Community Health Survey—mental health and wellbeing [Internet] Ottawa (ON): Statistics Canada; 2013. [cited 2014 May 2]. Available from: http://www23.statcan.gc.ca:81/imdb/p2SV.pl?Function=getSurvey&SDDS=5015&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 9.Higgins JP, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med. 2004;23(11):1663–1682. doi: 10.1002/sim.1752. [DOI] [PubMed] [Google Scholar]
- 10.StataCorp . Stata user’s guide: version 13 College. Station (TX): Stata Corporation; 2013. [Google Scholar]