Abstract
Ciguatera fish poisoning (CFP) is a foodborne illness caused by fish containing ciguatoxin (CTX). The toxin is produced by the microalgae Gambierdiscus spp. which are then eaten by reef fish; humans contract the illness when eating either fish that have eaten the algae, or carnivorous fish that have eaten those fish. CTX is an odorless, tasteless, and colorless neurotoxin that blocks voltage-sensitive Na+ channels and accumulates in many tissues of the fish, especially the viscera. The illness is typically mild to moderate in severity with gastrointestinal (diarrhea, cramping, nausea, vomiting) and neurological (paraesthesias, cold allodynia, fatigue, pruritis) manifestations. Rarely, the disease can be more severe with significant neuropathic or cardiac effects such as bradycardia and hypotension. Endemic to Hawai‘i and islands throughout the Caribbean and Pacific, CFP incidence rates range from several to thousands of cases per 100,000 per year. Since fishing is important for local food supply, exportation, and recreation throughout the Pacific, CFP is medically and economically significant in these areas. We present a case of CFP from Hawai‘i to illustrate the disease, demonstrating that the diagnosis is primarily clinical, with confirmatory tests from fish samples available in some cases. Treatment is supportive and symptomatic with no disease specific remedy. The prognosis for most cases is good with a short duration of self-limited symptoms, but for some cases neurological sequelae can become chronic. With no effective treatment, education on which species of reef fish and which body parts to avoid eating is essential in the prevention of CFP.
Introduction
Ciguatera fish poisoning (CFP) is a foodborne illness contracted by humans eating reef fish containing ciguatoxin (CTX) and is characterized predominantly by gastrointestinal and neurological manifestations. It is the most common marine poisoning in the world1,2 and is a significant public health concern in the Caribbean, Hawai‘i, and the Pacific islands.3,4
The CTX toxin is produced by the microalgae Gambierdiscus spp., which are ingested by herbivorous reef fish that are then eaten by larger carnivorous reef fish and serve as the primary source for human illness.1,2 The toxins are lipid soluble and bioaccumulate in greater concentrations as they move up the food chain, making the larger carnivorous fish more likely to cause harm to humans.5 However, consumption of any fish in the coral reef food chain can cause disease.1 The toxin is colorless, odorless, and tasteless and is not affected by any food storage or preparation techniques.6 It is the one of the most potent Na+ channel toxins known in mammals, causing activation of voltage-sensitive Na+ channels at very small (<1 part per billion) concentrations, leading to its multiple clinical manifestations as discussed below.2 Reef fish in particular are associated with CFP, as these are the fish involved in the food chain of the Gambierdiscus spp. Reef fish commonly associated with CTX are many but include: barracudas, groupers, jacks, moray eels, snappers, parrotfish, and surgeonfish.2,6,7 Due to its lipid solubility, CTX accumulates more heavily in several places in fish including the brain, liver, and gonads. Anecdotally it has been noted that more severe cases of CFP reported to the Hawai‘i Department of Health involve consumption of the head (brain) or organs of the fish and less severe cases tend to involve consumption of only the muscle.
The manifestations of CFP are predominantly gastrointestinal and neurological, but also include other rare but potentially dangerous effects.1,2 Effects typically begin within a window of <1 to 48 hours from ingestion, with gastrointestinal symptoms occurring typically within 12 hours and neurological symptoms developing over the first 24 hours.2 Gastrointestinal effects include diarrhea, abdominal pain, nausea, and vomiting. These have the potential for significant dehydration, but are typically short-lived. Neurological effects include perioral and stocking-glove distribution paraesthesias, myalgias, numbness, cold allodynia (burning pain caused by exposure to cold temperature), fatigue, pruritis, and rarely coma.1,2 Neurological symptoms can be variable in course, with most resolving in days to weeks, though some can persist for years and are reported to recur with exposure to non-CTX containing triggers (such as consumption of chicken or alcohol).2 Rare but significant cardiovascular effects do occur, including bradycardia and hypotension.1 Typically moderate, CFP can rarely result in death.
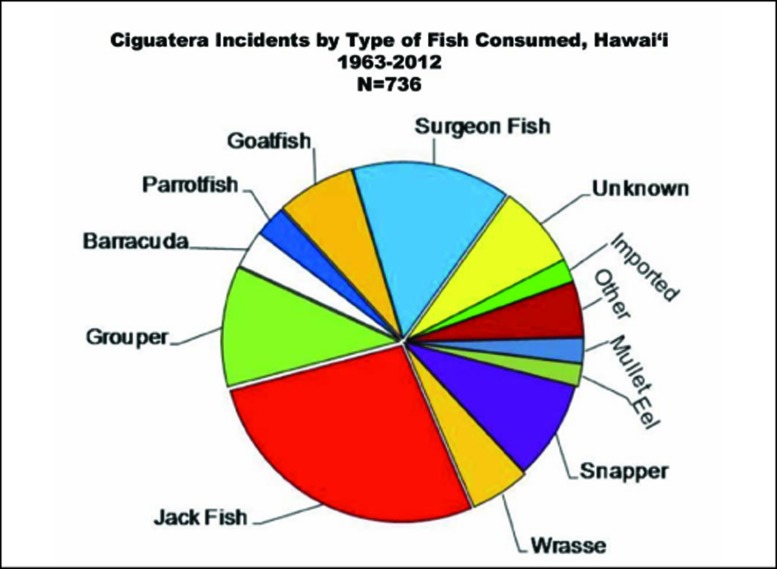
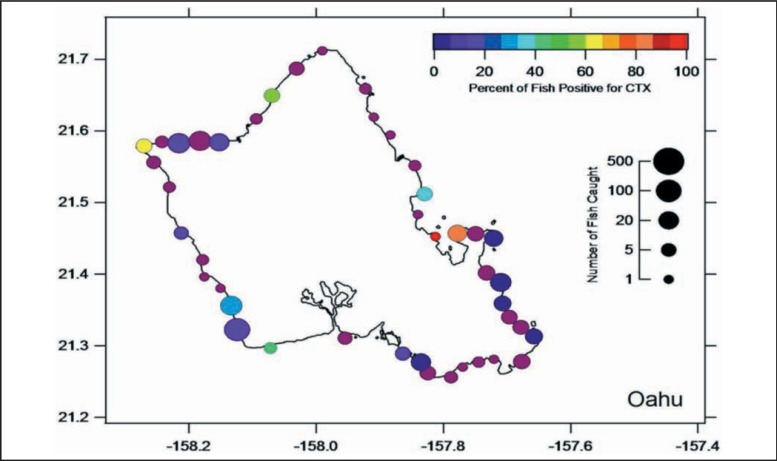
An endemic problem in Hawai‘i and many of the Pacific Islands,3,4 cases of CFP are reported to the Hawai‘i Department of Health, with a total of 3 to 69 cases per year in the state, averaging 28.5 total cases per year from 2002–2011.4 With underreporting of milder cases, it is likely that the actual local incidence is anywhere from 10 to 20 times higher than reported. There have been two reported deaths from CFP in Hawai‘i occurring in 1964 after eating broiled reef fish including their viscera.8 There is a broad range of incidence across the Pacific islands, with Samoa at about 1.6 cases per 100,000 per year and the Cook Islands at nearly 1,500 cases per 100,000 per year.3 Fish are an important natural resource throughout the Pacific and fishing is a very common means of subsistence, putting many people at risk for CFP. Reef fishing also represents a common sport in Hawai‘i, endangering both visitors and the local population. Based on data from the Hawai‘i Department of Health, the five most common fish associated with cases of CFP in the state from 1963 to 2012 are jack (ulua, kahala, or papio), surgeon fish (kole), groupers (roi or hapu ‘u), snappers (lehi, onaga, taape, or waha-nui), and wrasses (Figure 1; Hawai‘i State Department of Health, unpublished data, Oct 2013). There are many local myths about how to determine which fish are safe, including avoiding fish from the leeward side of the island. From 2008 to 2012 researchers from the University of Hawai‘i cooperated with local fishermen to conduct surveillance studies of roi caught across the state of Hawai‘i, testing the fish for the presence of CTX. The map in Figure 2 represents the cumulative data from the island of O‘ahu.9 The study shows that no coast of any Hawaiian Island is free from CTX-positive fish and it is speculated that any relationship to the leeward side of an island is more likely due to which coast is more commonly fished rather than the presence or absence of CTX positive fish.10
Figure 1.
Ciguatera incidents by type of fish consumed, Hawai`i (1963–2012) (image courtesy Hawai‘i State Department of Health)
Figure 2.
Percent of groupers (roi) positive for CTX on the coasts of O‘ahu (image courtesy of Dr. P.K. Bienfang)
Example Case
In 2009 the Honolulu Advertiser reported a case of a previously healthy 53-year-old man who developed a severe case of confirmed CFP after consuming a reef fish caught in Hawai‘i.11 The man and his wife both consumed a knifejaw fish that the man had caught while spear fishing in a reef off Kaua‘i. Both he and his wife had onset of typical ciguatera symptoms, including gastrointestinal upset and paraesthesias, within a few hours of consuming the fish. His wife's case was relatively mild and short in duration, but he progressed to develop more severe neurological manifestations including severe neuropathy. He was unable to walk, speak, or feed himself and was hospitalized for more than 2 months. Remnants of the fish that the patient ate were tested by the Department of Health and found to be positive for CTX.
Discussion
A diagnosis of CFP is clinically based on the presence of typical gastrointestinal and neurological symptoms and history of ingestion of a likely CTX containing fish. There are currently no blood tests available to confirm poisoning with CTX.1,2 The current gold standard for confirming the diagnosis is the testing of fish remnants for CTX (when they are available), as illustrated in the case above.1 Treatment of CFP is supportive, with symptomatic treatment of gastrointestinal manifestations and supportive care in more severe cases with bradycardia and hypotension.2 There are no proven treatments for neurological manifestations. Mannitol has shown promise in ameliorating the neurological sequelae, but the only double-blind, randomized controlled trial to date showed no difference when compared to normal saline and highlighted concerns for hypotension caused by mannitol.2,6 Some limited data suggest that neuromodulating medications such as amitriptyline may be beneficial, but controlled trials are lacking.2 While no specific remedies are available in austere environments to prevent or treat CFP, there are many local remedies throughout the Pacific Islands such as plant extracts that are unproven by research.1,7 One common traditional remedy employed stems from the tree heliotrope, which is found in Hawai‘i and throughout the Pacific Islands; no studies confirming its efficacy have been published.
Most cases do not cause long term effects; however, there are some patients that will have persistent neurological symptoms, including neuropathy, fatigue, or pruritis chronically. There is also evidence of sensitization, with affected individuals having more rapid onset of symptoms upon subsequent exposure to the toxin.2
With no specific treatment available for CFP, prevention is a key component to the management of this disease, especially in endemic areas such as Hawai‘i and the Pacific islands. The most effective approach to preventing CFP is to avoid reef fish which are more likely to contain CTX. Fish containing CTX cannot be reliably distinguished from safe fish based on appearance, taste, or smell. Some traditional methods exist in Hawai‘i and the Pacific Islands for determining which fish may be at risk for causing ciguatera, including feeding it first to the family pet or the oldest member of the family, or avoiding fish that flies avoid, but these methods cannot be recommended as they are neither safe nor reliable. There is a common belief that people should avoid larger individual fish of a given species, but any size of fish can potentially harbor sufficient amounts of CTX to elicit symptoms.10 In the past commercially-produced, portable CTX detection kits were available to test fish prior to eating, but their production has been discontinued due to a significant number of false negative tests.12 People should avoid consumption of the liver, brain, or gonads of reef fish, as these tissues sequester much higher levels of CTX than the muscle tissue. The key to prevention is educating the populace about the risks of eating reef fish in endemic areas. In cases where this is not feasible, such as in areas where reef fish are a primary source of subsistence, education about avoiding consumption of the viscera (which have a higher concentration of the toxin) is also important.
Conclusion
Ciguatera fish poisoning is an important fish-borne disease in Hawai‘i and the Pacific islands. Though most cases have mild to moderate gastrointestinal and neurological symptoms, the potential for more severe and even life-threatening illness exists. There is significant variation in the incidence of the disease depending on location and it is important for travelers to these areas to be familiar with the local risk of CFP and to make decisions about eating reef fish accordingly. Diagnosis is clinical, with confirmatory fish tissue sampling. Treatment is supportive and symptomatic with no disease-specific remedy proven. Due to the lack of treatment options, prevention via avoidance of likely CTX containing fish is essential, or at a very minimum avoiding the head and viscera of reef fish.
Acknowledgment
The authors would like to thank the Hawai‘i Department of Health's Disease Investigation Branch for providing data on the incidence of ciguatera by type of fish consumed and the graph used in Figure 1.
Disclosures
The authors report no financial conflicts of interest.
Disclaimer
The views expressed in the manuscript are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense or United States Government.
References
- 1.Dickey RW, Plakas SM. Ciguatera: A public health perspective. Toxicon. 2010;56(2):123–136. doi: 10.1016/j.toxicon.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Isbister GK, Kiernan MC. Neurotoxic marine poisoning. Lancet Neurol. 2005;4(4):219–228. doi: 10.1016/S1474-4422(05)70041-7. [DOI] [PubMed] [Google Scholar]
- 3.Skinner MP, Brewer TD, Johnston R, Fleming LE, Lewis RJ. Ciguatera fish poisoning in the Pacific islands (1998 to 2008) PLoS Negl Trop Dis. 2011;5(12):e1416. doi: 10.1371/journal.pntd.0001416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.State of Hawaii Department of Health, author. 10-Year Summary of Reported Cases of Notifiable Diseases Hawai‘i 2002–2011. [September 3, 2013]. http://hawaii.gov/health/about/about/pr/New%20Disease%20Template%20for%20WEB%20publish2002_2011.html.
- 5.Bienfang PK, Trapido-Rosenthal H, Lows EA. Magnification of risks: Bioaccumulation/biomagnifications in food chains. In: Meyers RA, editor. Encyclopedia of Sustainability Science and Technology. New York, NY: Springer; 2012. [Google Scholar]
- 6.Centers for Disease Control and Prevention, author. Ciguatera fish poisoning--New York City, 2010–2011. MMWR Morb Mortal Wkly Rep. 2013;62(4):61–65. [PMC free article] [PubMed] [Google Scholar]
- 7.Bienfang PK, Parsons ML, Bidigare RR, Laws EA, Moeller PDR. Ciguatera fish poisoning: A synopsis from ecology to toxicity. In: Walsh PJ, Smith SL, Fleming LE, Solo-Gabriele HM, Gerwick WH, editors. Oceans and Human Health: Risks and Remedies from the Sea. New York, NY: Elsevier Science Publishers; 2008. pp. 257–270. [Google Scholar]
- 8.Anderson BS, Sims JK, Wiebenga NH, Sugi M. The epidemiology of ciguatera fish poisoning in Hawaii, 1975–1981. Hawaii Med J. 1983;42(10):326–334. [PubMed] [Google Scholar]
- 9.Oahu roi results. Dr. P.K. Bienfang's website on ciguatera testing in roi (peacock groupers) [September 3, 2013]. http://www.fish4science.com/Oahu_map_of_Roi.html.
- 10.Bienfang P, DeFelice S, Laws E, Wallsgrove N, Caldwell P. Ciguatoxicity in the main Hawaiian Islands: special and temporal variability in the introduced reef carnivore Cephalopholis argus. J Res Environ Sci Toxicol. 2012;1(4):47–57. [Google Scholar]
- 11.Diana L. Isle man's case shows ciguatera's risk. Honolulu Advertiser. [September 3, 2013]. http://the.honoluluadvertiser.com/article/2009/Nov/09/ln/hawaii911090324.html.
- 12.Bienfang P, DeFelice S, Dowling A. Quantitative evaluation of commercially available test kit for ciguatera in fish. Food and Nutrition Sciences. 2011;2(6):594–598. doi: 10.4236/fns.2011.26083. [DOI] [Google Scholar]