Abstract
Background
ERCP has a complication rate ranging between 4% and 16% such as post-ERCP pancreatitis, hemorrhage, cholangitis and perforation. Perforation rate was reported as 0.08% to 1% and mortality rate up to 1.5%. Besides, injury related death rate is 16% to 18%. In this study we aimed to present a retrospective review of our experience with post ERCP-related perforations, reveal the type of injuries and management recommendations with the minimally invasive approaches.
Methods
Medical records of 28 patients treated for ERCP-related perforations in Okmeydani Training and Research Hospital between March 2007 and March 2013 were reviewed retrospectively. Patient age, gender, comorbidities, ERCP indication, ERCP findings and details were analyzed. All previous and current clinical history, laboratory and radiological findings were used to assess the evaluation of perforations.
Results
Between March 2007 and March 2013, 2972 ERCPs were performed, 28 (0.94%) of which resulted in ERCP-related perforations. 10 of them were men (35.8%) and 18 women (64.2%). Mean age was 53.36±14.12 years with a range of 28 to 78 years. 14 (50%) patients were managed conservatively, while 14 (50%) were managed surgically. In 6 patients, laparoscopic exploration was performed due to the failure of non-surgical management. In 6 of the patients that ERCP-related perforation was suspected during or within 2 hours after ERCP, underwent to surgery primarily. There were two mortalities. The mean length of hospitalization stay was 10.46±2.83 days. The overall mortality rate was 7.1%.
Conclusion
Successful management of ERCP-related perforation requires immediate diagnosis and early decision to decide whether to manage conservatively or surgically. Although traditionally conventional surgical approaches have been suggested for the treatment of perforations, laparoscopic techniques may be used in well-chosen cases especially in type II, III and IV perforations.
Introduction
Endoscopic Retrograde Cholangiopancreatography (ERCP) which is an important diagnostic and therapeutic modality for disorders of biliary tree and pancreas, has evolved over the decades, since first introduced in 1968 by McCune et al [1]. ERCP has a complication rate ranging between 4% and 16% such as post-ERCP pancreatitis, hemorrhage, cholangitis and perforation. Perforation rate was reported as 0.08% to 1% and mortality rate up to 1.5% [2]–[6]. Besides, injury related death rate is 16% to 18% [7], [8].
Since the first endoscopic pancreatogram was obtained in 1968 and biliary sphincterotomy was first described in 1974, papillotomy for the management of choledocholithiasis have been widely used and in subsequent years, numerous endoscopic techniques evolved to address pancreaticobiliary disease [1], [9]. As the indications for ERCP have increased, a greater focus on recognizing and preventing complications has emerged [10]. ERCP has a complication rate ranging from 4% to 16% including asymptomatic hyperamylasemia, cardiopulmonary depression, hypoxia, aspiration, intestinal perforation, bleeding, cholangitis, adverse medication reactions, sepsis, acute pancreatitis and death. ERCP-related perforation is a rare but serious complication. The incidences of perforation reported by recent series were ranged from 0.3% to 1.3% [4], [6], [11]–[14].
The most important point in the management of ERCP-related perforations is the definition of the injury type. However, the unusual and unexpected complications are difficult to manage. The treatment of perforations varies from conservative management to urgent surgery according to the injury type and time of diagnosis. Majority of cases are retroperitoneal duodenal perforations usually due to papillotomy, whereas intraperitoneal perforations are less common and caused by the endoscope itself [15]. There has not been a consensus on management guidelines of ERCP related perforations, because of its low rate. There has been few case series in the literature that recommend different therapeutic modalities for ERCP-related perforation. Extensive drainage, repair with omental patch, pyloric exclusion, gastrojejunostomi, T-tube with or without cholecystectomy are surgical interventions that are used for the treatment of ERCP-related perforations [16]–[18]. Percutaneous drainage technique are generally used in the patients who managed conservatively.
Most recent studies indicate that, carefully selected patients may recover uneventfully with conservative management alone, while in the past, many authors advocated early surgical management for ERCP-related perforations [11], [19]. Many treatment guidelines have been proposed, but unfortunately there is still no consensus on it. Advances in laparoscopy and endoscopy led up to treat these unfortunate patients with minimal invasive techniques. In this study we want to present a retrospective review of our experience with post ERCP-related perforations, reveal the type of injuries and management recommendations with the minimally invasive approaches.
Materials and Methods
Medical records of 28 patients treated for ERCP-related perforations in Okmeydani Training and Research Hospital between March 2007 and March 2013 were reviewed retrospectively. This study was approved by the institutional review board at our institution (Ethic Committee of Okmeydani Training and Research Hospital, Istanbul, Turkey) and informed written consent was obtained from all of the reviewed subjects for their clinical records to be used in this study.
Patient age, gender, comorbidities, ERCP indication, ERCP findings and details were analyzed. All previous and current clinical history, laboratory and radiological findings were used to assess the evaluation of perforations. Computerized tomography was planned on the onset of symptoms and repeated according the severity of the symptoms. Time between diagnosis of perforation and surgery (when used), the type of the operative intervention, the length of hospital stay, the complication rate and the ultimate patient outcome were also studied. The perforations were classified according to the site of perforation using the classification previously defined by Stapfer [11] ( Table 1 ). Institutional ethic committee approved the evaluation of human subjects and the reporting of this study.
Table 1. Classification of ERCP-Related Perforations [19].
| Type | Definition |
| 1 | Lateral or medial duodenal wall perforation (endoscope related) |
| 2 | Periampullary perforations (sphincterotomy related) |
| 3 | Ductal and duodenal perforations due to endoscopic instruments (not guide-wire) |
| 4 | Presence of retroperitoneal air due to guide-wire |
According to the management policy of our institution for ERCP-related perforations; extensive contrast extravasation on ERCP/CT, extraperitoneal or intraperitoneal fluid collection on CT with unsolved problem and severe peritonitis, duodenum lateral wall or jejunal injury and problem remaining unsolved with endoscopic procedure (retained hardware or biliary stone failed to be removed during ERCP) are candidates for urgent surgical repair. Patients without any of these conditions were managed conservatively. Conservative management consisted of close monitorisation with physical examination, nasobiliary drainage, antibiotic administration and parenteral nutritional support. All patients were monitored with white blood cell count and C-reactive protein (daily). Surgery was planned immediately when there is hypotension (systolic blood pressure ≤90 mmHg), tachycardia (heart rate ≥120/min), fever (axillary temperature ≥38°C), worsening of abdominal symptoms and signs (signs of peritonitis).
Results
Between March 2007 and March 2013, 2972 ERCPs were performed, 28 (0.94%) of which resulted in ERCP-related perforations. 10 of them were men (35.8%) and 18 women (64.2%). Mean age was 53.36±14.12 years with a range of 28 to 78 years. ERCP was performed for treatment of bile duct stones in 20 patients with additional cholangitis in 7 patients, 4 patients for cholangitis, for benign biliary stricture in 2 patients and for pancreas head cancer in 2 patients. A complete ERCP procedure includes cannulation, sphincterotomy, and basket-balloon instrumentation for stone removal or relieving the bile duct passage.
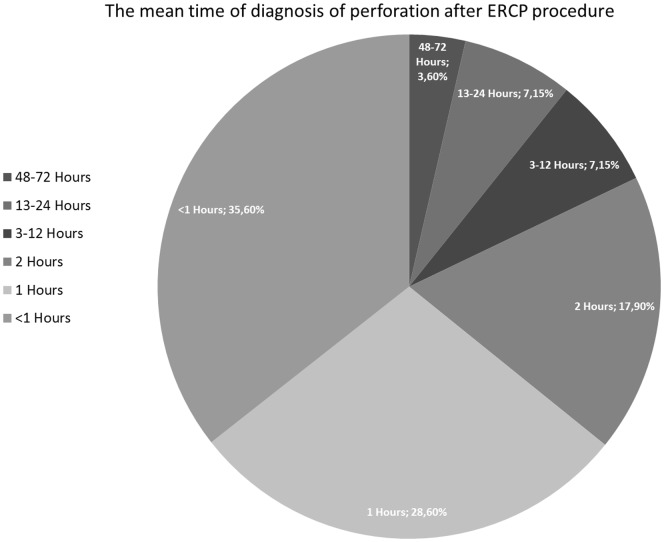
ERCP-related perforation during the intervention was suspected in 23 patients, only 10 (35.7%) of the perforations were diagnosed during ERCP whereas the remaining 18 were (64.3%) diagnosed by physical examination, trans-abdominal ultrasound, computerized tomography and abdominal radiography. Demonstration of a perforation during ERCP was accomplished by a limited contrast study through the endoscope. Severe post-procedural abdominal pain with/without pancreatitis, signs of peritonitis, fever and increased levels of CRP and white blood cells were accepted as suspected perforation. The mean time of diagnosis after ERCP procedure was 5.57 hours, ranged between 1 and 72 hours ( Figure 1 ).
Figure 1. The figure shows the mean time of diagnosis after ERCP procedure (hours).
Conservative management was successful in 14 (50%) patients ( Table 2 ), while 14 (50%) were managed surgically. In 6 patients, laparoscopic exploration was performed due to the failure of non-surgical management. Laparoscopic cholecyctectomy+Laparoscopic common bile duct exploration (LCBDE)+T-tube+drainage was performed in 5 of these patients. Although the remaining patient (63 year-old-male) underwent laparoscopic exploration on the 48th hour because of the progression of physical and laboratory findings, no sign of perforation (intra-and retroperitoneal fluid) was found. Laparoscopic cholecyctectomy+LCBDE+Stone extraction+Trans-cystic drain were successfully performed and the patient was discharged at the 12th post-operative day ( Table 3 ). In 6 of the patients that ERCP-related perforation was suspected during or within 2 hours after ERCP, underwent to surgery primarily because of the extensive contrast extravasation on ERCP/CT and extraperitoneal or intraperitoneal fluid collection on CT (also retained biliary stone failed to be removed during ERCP). LCBDE+T-Tube+Drainage were performed; additionally laparoscopic cholecystectomy was added to the surgery in non-cholecystectomized three patients ( Table 4 ). In the remaining two patients, although minimal invasive surgical approach was performed intra-abdominal abscess developed and required reoperation ( Table 5 ). One of them was 63 year-old-female patient who underwent ERCP for CBD stone. The injury was near the ampulla consequent to precut sphincterotomy, showed contrast leakage. Laparoscopic cholecyctectomy+LCBDE+Stone extraction+T-Tube+intra-and retroperitoneal drainage were performed two hours after perforation. 72 hours after ERCP, signs of peritonitis, fever, and white blood cell counts were increased. That's why the surgical team decided to re-operate the patient. Intra-abdominal abscess was seen and pyloric exclusion+T-tube revision+gastrojejunostomi was performed. She was well discharged on the 14th day. The second patient was 68 years old female with the diagnosis of pancreas head cancer and liver metastasis underwent ERCP for biliary drainage. Type III injury in the distal common bile duct secondary to wire manipulation was suspected. LCBDE+T-Tube with intra- and retroperitoneal drainage was initially performed after two hours from ERCP. She was re-operated because of the intra-abdominal abscess on the 36th hour. There were two mortalities. The first one who was in failed non-surgical treatment group and died as a result of acute myocardial infarction on the 3rd day. Other patient with the diagnosis pancreas head cancer who underwent surgery for ERCP related perforation died because of sepsis at the 10th day. The mean length of hospitalization stay was 10.46±2.83 days. The overall mortality rate was 7.1%.
Table 2. Successful Nonsurgical Management of ERCP-Related Perforations.
| Age | Gender | ERCP indication | Type of perforation | Time Between ERCP and diagnosis (hour) | Diagnosis of perforation | Radiologic Findings | LOS (day) | Outcome |
| 51 | F | CBD stones | II | 0 h | ERCP | Minimal contrast extravasation | 12 d | Survived |
| 78 | M | CBD stones | II | 1 h | CT | Retroperitoneal air | 11 d | Survived |
| 69 | F | Cholangitis | III | 2 h | CT | Intra-and retroperitoneal air | 9 d | Survived |
| 54 | F | CBD stones | II | 1 h | CT, USG | Intra-and retroperitoneal air | 14 d | Survived |
| 68 | M | Cholangitis | IV | 1 h | CT | Retroperitoneal air | 10 d | Survived |
| 66 | F | CBD Stones | III | 0 h | ERCP | Minimal contrast extravasation | 11 d | Survived |
| 57 | F | CBD stones | II | 2 h | CT | Retroperitoneal air | 11 d | Survived |
| 49 | F | Cholangitis | II | 1 h | CT | Intra-and retroperitoneal air | 9 d | Survived |
| 28 | F | CBD stones | II | 0 h | ERCP | Contrast extravasation | 12 d | Survived |
| 34 | F | CBD stones | III | 2 h | CT | Retroperitoneal air | 8 d | Survived |
| 31 | F | CBD Stones | II | 0 h | CT | Intra-and retroperitoneal air | 9 d | Survived |
| 58 | M | Benign biliary stricture | III | 1 h | CT, USG | Intra-and retroperitoneal air, fluid collection | 12 d | Survived |
| 72 | M | Pancreas Head Cancer | IV | 0 h | CT | Retroperitoneal air | 6 d | Survived |
| 68 | F | Benign biliary stricture | III | 1 h | CT | Free air, fluid collection | 11 d | Survived |
Footnotes: ERCP: Endoscopic Retrograde Cholangiopancreatography, CT: Computer Tomography, USG: Ultrasonography LOS: Length of Stay.
Table 3. Failed Non-Surgical Management of ERCP-Related Perforations.
| Age | Gender | ERCP indication | Type of perforations | Time between ERCP and diagnosis (hour) | Time between ERCP and Operation (hour) | Type of Operation | LOS (day) | Outcome |
| 54 | F | Cholangitis+CBD stone | II | 0 h | 24 h | Laparoscopic cholecyctectomy+LCBDE+T-Tube+drainage | 18 d | Survived |
| 45 | M | CBD stones | II | 12 h | 36 h | Laparoscopic cholecyctectomy+LCBDE+Stoneextraction+T-Tube+drainage | 3 d | Ex (AMI) |
| 54 | F | Cholangitis+CBD stone | II | 72 h | 108 h | Laparoscopic cholecyctectomy+LCBDE+drainage | 10 d | Survived |
| 57 | F | CBD stones | III | 24 h | 96 h | Laparoscopic cholecyctectomy+Stone extraction+LCBDE+T-Tube | 11 d | Survived |
| 71 | F | CBD stones | II | 18 h | 48 h | Laparoscopic cholecyctectomy+LCBDE+T-Tube+drainage | 12 d | Survived |
| 63 | M | Cholangitis+CBD stone | III | 12 h | 48 h | Laparoscopic cholecyctectomy+LCBDE+Trans-Cystic drain | 12 d | Survived |
Footnotes: ERCP: Endoscopic Retrograde Cholangiopancreatography, LOS: Length of Stay, AMI: Acute Myocardia Infarcts, Ex:Exitus, LCBDE: Laparoscopic common bile duct exploration.
Table 4. Primary Minimal Invasive Surgical Management of ERCP-Related Perforations.
| Age | Gender | ERCP indication | Type of Perforation | Time Between ERCP and diagnosis (hour) | Time between ERCP and Operation (hour) | Type of Operation | LOS (day) | Outcome |
| 42 | M | Cholangitis+CBD Stones | II | 0 h | 1 h | LCBDE+T-Tube+drainage | 10 d | Survived |
| 37 | F | Cholangitis+CBD Stones | II | 0 h | 1 h | Laparoscopic cholecyctectomy+LCBDE+Trans-cytic drain+drainage | 7 d | Survived |
| 39 | M | Cholangitis+CBD Stones | III | 2 h | 3 h | LCBDE+T-Tube | 8 d | Survived |
| 40 | M | Cholangitis+CBD Stones | II | 1 h | 2 h | LCBDE+T-Tube+drainage | 8 d | Survived |
| 43 | M | Cholangitis+CBD Stones | II | 0 h | 1 h | Laparoscopic cholecyctectomy+LCBDE+T-Tube+drainage | 13 d | Survived |
| 35 | F | Cholangitis | II | 2 h | 3 h | Laparoscopic cholecyctectomy+LCBDE+T-Tube+drainage | 4 d | Survived |
Footnotes: ERCP: Endoscopic Retrograde Cholangiopancreatography, LOS: Length of Stay, LCBDE: Laparoscopic common bile duct exploration.
Table 5. Failed primary minimal invasive surgical management of ERCP-related perforations.
| Age | Gender | ERCP indication | Type of Perforation | Time Between ERCP and diagnosis (hour) | Time between ERCP and Operation (hour) | Type of Operation | LOS (day) | Outcome |
| 63 | F | CBD stones | II | 0 h | 1-) 2 h 2-) 72 h | Laparoscopic cholecyctectomy+LCBDE+Stone extraction+T-Tube+drainage Re-operation: Pyloric exclusion+T-Tube revision+gastrojejunostomy | 14 d | Survived |
| 68 | F | Pancreas head cancer+liver metastasis | III | 1 h | 1-) 2 h 2-) 36 h | LCBDE+T-Tube+drainage Re-operation: explorative laparotomy+intra-abdominal abscess+drainage | 10 d | Ex (Sepsis) |
Footnotes: ERCP: Endoscopic Retrograde Cholangiopancreatography, LOS: Length of Stay, LCBDE: Laparoscopic common bile duct exploration.
Discussion
Although many patients with ERCP-related perforations can be managed expectantly, there is a dilemma for whom urgent operative intervention is necessary. In previous years some authors have suggested early operation for all endoscopic sphincterotomy perforations. However, with increasing experience with this rare but potentially lethal complication, there is increasing evidence that most perforations may be managed without surgery [20]–[23]. Early diagnosis of post-ERCP perforations is critical for successful management. Besides, the timing of operation is also important. The initial management is determined by the type and mechanism of injury. Progression of the symptoms and laboratory tests should be warning the surgeon for immediate surgical management. The key point is to decide who can be conservatively managed and who should be promptly operated.
Although several researches have classified ERCP-related perforations according to the location or mechanism of injury and have recommended various treatments, the most popular of these classifications was presented by Stapfer et al [11], [13], [14]. Stapfer et al classified perforations into four types according to the location and the mechanism of injury ( Table 1 ) [11]. Type I perforations occur on the medial or lateral wall far from the ampulla and are caused by the endoscope itself or by the stent. Type II perforations are generally retroperitoneal, are classified as peri-vaterian, occur during sphincterotomy. Type III perforations are due to wire manipulation or basket instrumentation during stone retrieval and occur in the distal common bile duct. Type IV perforations are tiny retroperitoneal perforations caused by the use of compressed air during endoscopy. Another classification was suggested by Howard et al. includes three groups; group I: guidewire perforations, group II: periampullary perforations, group III: duodenal perforations [13]. Another frequently used classification was presented by Enns et al; group I: esophageal, gastric and duodenal perforations, group II: sphincterotomy-related perforations, group III: guidewire-related perforations [14]. There were 17 type-II perforations, 9 type-III perforations and 2 type-IV perforations in our case series according to the classification system of Stapfer et al. No type-I injury was observed.
The initial clinical presentation of patients with ERCP-related perforation is non-specific. The classic presentation of perforation, with severe epigastric pain, vomiting and epigastric tenderness progressing to generalized rigidity is only seen in the minority of cases. Moreover, the diagnosis is likely to be delayed if the patient has elevated amylase levels and the clinical presentation is attributed to post-ERCP pancreatitis. The most accurate diagnose can be made when the rupture is seen during the procedure. When there is a suspected duodenal perforation, an ultrasound or CT scan is a sensitive method to judge the existence of peritoneal, retroperitoneal emphysema or fluid collection [24], [25]. Genzlinger et al suggested that with routine post-ERCP computerized tomography in 13% to 33% of patients small amounts of retroperitoneal air may be detected, probably as a result of a post-procedural but non-significant micro-perforations [26]. Leukocytosis and fever that usually occur in the early phase are useful parameters for determining the management approach. Retroperitoneal nature of the injuries may mask severity; therefore, negative abdominal findings should not exclude surgery. Additionally, Mao et al suggested that subcutaneous emphysema is a sensitive physical sign that can be regarded as an effective parameter for an early diagnosis of perforation besides other radiologic examinations [16]. In our case series, perforation was suspected during the procedure in 23 (82%) patients and only in 8 (28.5%) of them it was diagnosed. Computerized tomography was performed within initial hours in 15 patients with suspected perforation to verify the diagnosis. These ratios are similar with other studies [3], [11], [13].
Most authors suggested to determine the type and mechanism of the perforation before selecting the optimal treatment method. Many studies reported that around 70% of patients with ERCP-related perforation could be managed conservatively [11], [17], [18]. Although, Stapfer et al reported that Type I injuries required prompt surgical interventions, recent studies recommended successful endoscopic treatments with endoscopic clippings, endo-loop applications and endoscopic closure devices [27]. Additionally, Stapfer suggested conservative treatment strategy for type II and III injuries (periampullary and bile duct injuries). In the presence of significant peritoneal findings, type II and III perforations should be treated by surgery. Furthermore, type IV (retroperitoneal air alone) perforations are not regarded as real perforations and should be treated conservatively. The rate of conservative management may vary depending on the management policies of the institutions. Our conservative treatment rate was 50% which is low compared to the other series. This is because these patients underwent surgery not only for the injury but also for the underlying disease, which could not be treated by ERCP.
The extent of surgery was proportional to the degree of injury, and the intraabdominal contamination. The basic principles of surgical therapy are repair of the leakage with diversion of the gastric contents and control for the source of the sepsis by means of external drainage [28]. Generally, surgical interventions that are used for the treatment of ERCP-related perforations are as follows; extensive drainage, repair with omental patch, pyloric exclusion, gastrojejunostomi, T-tube with or without cholecystectomy [16]–[18]. Sarli et al reported a wide range of operative procedures for the treatment of ERCP-related perforations, including simple retroperitoneal drainage, duodenal repair around a T-tube inserted into the perforation, common bile duct exploration+T-tube placement, duodenal diversion by antrectomy+gastrojejunostomy or gastrojejunostomy with pyloric exclusion and pancreaticoduodenectomy [29]. No article was found in the literature about the laparoscopic management of ERCP-related perforations. In a study about the comparison of LCBDE and ERCP for the treatment of common bile duct stones, it was pointed that in experienced hands LCBDE is a safe and feasible option with the advantages of minimal access [30].
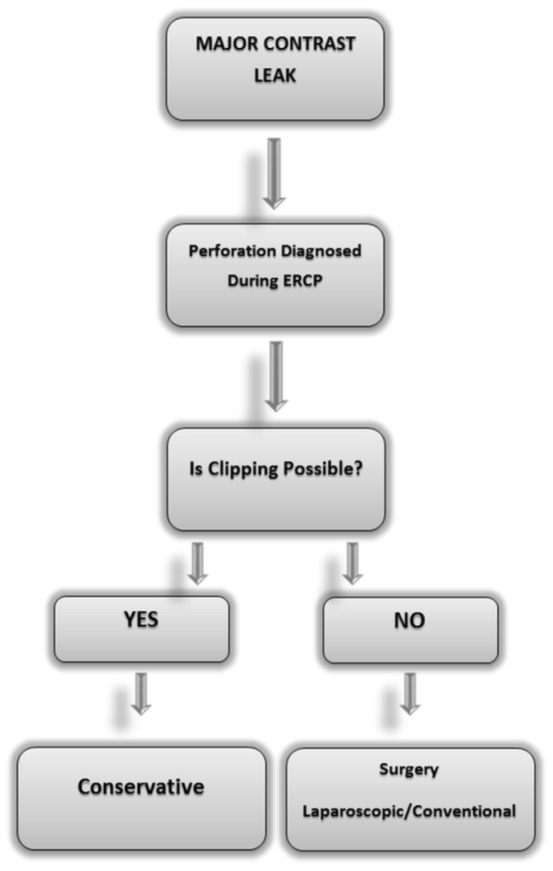
To summarize, we performed LC+LCBDE+T-tube+intra-or/and retroperitoneal drainage in 6 patients due to the failure of non-surgical management and LCBDE+with or without LC+T-tube+intra-or/and retroperitoneal drainage for 8 patients as a primary management. This approach failed in 2 (14%) patients, and our surgical mortality rate was 7.1%. These rates were similar to literature ( Table 6 ). In this technique we can solve the injury and also the underlying disease (extraction of bile duct stones) in the same intervention. The most important limitation of our study was lack of type I injuries. It should be kept in mind that minimally invasive management (endoclipping) could be attempted if the perforation is diagnosed during ERCP. We suggest that, in patients with cholelitiasis and choledocholithiasis if type II and III perforation occurs during ERCP, CBDE+LC+T-tube+drainage with nasogastric suction can be performed as primary treatment or when conservative treatment fails. Based on our findings, we propose a simple management algorithm which can be readily and easily used ( Figure 2 ). To design a prospective study about laparoscopic approach is not possible due to major ethical issues. That's why the evaluation of this approach can only be made by retrospective case series. The source of severe sepsis and peritonitis may not be revealed objectively by laparoscopy laparoscopy which is a serious problem that needs to be resolved.
Table 6. Reported perforation rates with ERCP.
| Study | Length of Study | Number of ERCP's | Perforations | Operations | Mortality | Year |
| Chaudhary and Aranya [31] | 10 years | 750 | 10(1.3) | 10(100%) | 2(20%) | 1996 |
| Loperfido et al [6] | 2 years | 3356 | 28(0.83%) | 10(35.7%) | 4(14.3%) | 1998 |
| Stapfer et al [11] | 5 years | 1413 | 14(0.99%) | 9(64.3%) | 2(14.3%) | 2000 |
| Preetha et al [28] | 9 years | 4030 | 18(0.45%) | 18(100%) | 3(16.7%) | 2003 |
| Christensen et al [32] | 2 years | 1177 | 13(1.1%) | 2(15.4%) | 1(7.7%) | 2004 |
| Wu et al [33] | 6 years | 6620 | 30(0.45%) | 10(33.3%) | 5(16.7%) | 2006 |
| Fatima et al [18] | 11 years | 12427 | 76(0.6%) | 22(28.9%) | 5(6.6%) | 2007 |
| Cotton et al [4] | 12 years | 11497 | 16(0.14%) | 11(68.8%) | 1(6.3%) | 2009 |
| Morgan et al [34] | 13 years | 12817 | 24(0.2%) | 10(41.7%) | 1(4.2%) | 2009 |
| Gurung et al [35] | 2 years | 423 | 1(0.2%) | 1(100%) | 0 (0%) | 2014 |
| Katsinelos et al [36] | 7 years | 2837 | 3(0.11%) | 1(0.035) | 0 (0%) | 2014 |
| Present Series | 6 years | 2972 | 28(0.94%) | 20(71.4%) | 2 (7.1%) | 2014 |
Footnotes: ERCP: Endoscopic Retrograde Cholangiopancreatography.
Figure 2. A simple management algorithm for the ERCP-related perforations.
Conclusions
Successful management of ERCP-related perforation requires immediate diagnosis and early decision to decide whether to manage conservatively or surgically. While patients with type I perforation would invariably require immediate surgical intervention, those with type II or III, IV may often be managed conservatively. Otherwise, these types of injuries with retained stones and unrelieved bile obstruction should be explored. Although traditionally conventional surgical approaches have been suggested for the treatment of perforations, laparoscopic techniques may be used in well-chosen cases especially in type II, III and IV perforations.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper.
Funding Statement
The authors have no support or funding to report.
References
- 1. McCune WS, Shorb PE, Moscovitz H (1968) Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg 167:752–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Freeman ML (2003) Adverse outcomes of endoscopic retrograde cholangiopancreatography: avoidance and management. Gastrointest Endosc Clin N Am. 13:775–798. [DOI] [PubMed] [Google Scholar]
- 3. Lai CH, Lau WY (2008) Management of endoscopic retrograde cholangiopancreatography-related perforation. Surgeon 6:45–48. [DOI] [PubMed] [Google Scholar]
- 4. Cotton PB, Garrow DA, Gallagher J, Romagnuolo J (2009) Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc 70:80–88. [DOI] [PubMed] [Google Scholar]
- 5. Silviera ML, Seamon MJ, Porshinsky B, Prosciak MP, Doraiswamy VA, et al. (2009) Complications related to endoscopic retrograde cholangiopancreatography: a comprehensive clinical review. J Gastrointestin Liver Dis 18:73–82. [PubMed] [Google Scholar]
- 6. Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, et al. (1998) Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 48:1–10. [DOI] [PubMed] [Google Scholar]
- 7. Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, et al. (1991) Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 37:383–393. [DOI] [PubMed] [Google Scholar]
- 8. Elder JB (1988) Surgical treatment of duodenal ulcer. Postgrad Med J 64 Suppl 1: 54–59. [PubMed] [Google Scholar]
- 9. Peel AL, Hermon-Taylor J, Ritchie HD (1974) Technique of transduodenal exploration of the common bile duct. Duodenoscopic appearances after biliary sphincterotomy. Ann R Coll Surg Engl 55:236–244. [PMC free article] [PubMed] [Google Scholar]
- 10. Woods KE, Willingham FF (2010) Endoscopic retrograde cholangiopancreatography associated pancreatitis: A 15-year review. World J Gastrointest Endosc 2:165–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, et al. (2000) Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg 232:191–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, et al. (2001) Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol 96:417–423. [DOI] [PubMed] [Google Scholar]
- 13. Howard TJ, Tan T, Lehman GA, Sherman S, Madura JA, et al. (1999) Classification and management of perforations complicating endoscopic sphincterotomy. Surgery 126:658–663 discussion 664–655. [PubMed] [Google Scholar]
- 14. Enns R, Eloubeidi MA, Mergener K, Jowell PS, Branch MS, et al. (2002) ERCP-related perforations: risk factors and management. Endoscopy 34:293–298. [DOI] [PubMed] [Google Scholar]
- 15. Martin DF, Tweedle DE (1990) Retroperitoneal perforation during ERCP and endoscopic sphincterotomy: causes, clinical features and management. Endoscopy 22:174–175. [DOI] [PubMed] [Google Scholar]
- 16. Mao Z, Zhu Q, Wu W, Wang M, Li J, et al. (2008) Duodenal perforations after endoscopic retrograde cholangiopancreatography: experience and management. J Laparoendosc Adv Surg Tech A 18:691–695. [DOI] [PubMed] [Google Scholar]
- 17. Knudson K, Raeburn CD, McIntyre RC Jr, Shah RJ, Chen YK, et al. (2008) Management of duodenal and pancreaticobiliary perforations associated with periampullary endoscopic procedures. Am J Surg 196:975–981 discussion 981-972. [DOI] [PubMed] [Google Scholar]
- 18. Fatima J, Baron TH, Topazian MD, Houghton SG, Iqbal CW, et al. (2007) Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg 142:448–454 discussion 454-445. [DOI] [PubMed] [Google Scholar]
- 19. Avgerinos DV, Llaguna OH, Lo AY, Voli J, Leitman IM (2009) Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg Endosc 23:833–838. [DOI] [PubMed] [Google Scholar]
- 20. Scarlett PY, Falk GL (1994) The management of perforation of the duodenum following endoscopic sphincterotomy: a proposal for selective therapy. Aust N Z J Surg 64:843–846. [DOI] [PubMed] [Google Scholar]
- 21. Sarr MG, Fishman EK, Milligan FD, Siegelman SS, Cameron JL (1986) Pancreatitis or duodenal perforation after peri-Vaterian therapeutic endoscopic procedures: diagnosis, differentiation, and management. Surgery 100:461–466. [PubMed] [Google Scholar]
- 22. Dunham F, Bourgeois N, Gelin M, Jeanmart J, Toussaint J, et al. (1982) Retroperitoneal perforations following endoscopic sphincterotomy; clinical course and management. Endoscopy 14:92–96. [DOI] [PubMed] [Google Scholar]
- 23. Chung RS, Sivak MV, Ferguson DR (1993) Surgical decisions in the management of duodenal perforation complicating endoscopic sphincterotomy. Am J Surg 165:700–703. [DOI] [PubMed] [Google Scholar]
- 24. Sezgin O, Ulker A, Temucin G (2000) Retroperitoneal duodenal perforation during endoscopic sphincterotomy: sonographic findings. J Clin Ultrasound 28:303–306. [DOI] [PubMed] [Google Scholar]
- 25. Zissin R, Shapiro-Feinberg M, Oscadchy A, Pomeranz I, Leichtmann G, et al. (2000) Retroperitoneal perforation during endoscopic sphincterotomy: imaging findings. Abdom Imaging 25:279–282. [DOI] [PubMed] [Google Scholar]
- 26. Genzlinger JL, McPhee MS, Fisher JK, Jacob KM, Helzberg JH (1999) Significance of retroperitoneal air after endoscopic retrograde cholangiopancreatography with sphincterotomy. Am J Gastroenterol 94:1267–1270. [DOI] [PubMed] [Google Scholar]
- 27. Baron TH, Gostout CJ, Herman L (2000) Hemoclip repair of a sphincterotomy-induced duodenal perforation. Gastrointest Endosc 52:566–568. [PubMed] [Google Scholar]
- 28. Preetha M, Chung YF, Chan WH, Ong HS, Chow PK, et al. (2003) Surgical management of endoscopic retrograde cholangiopancreatography-related perforations. ANZ J Surg 73:1011–1014. [DOI] [PubMed] [Google Scholar]
- 29. Sarli L, Porrini C, Costi R, Regina G, Violi V, et al. (2007) Operative treatment of periampullary retroperitoneal perforation complicating endoscopic sphincterotomy. Surgery 142:26–32. [DOI] [PubMed] [Google Scholar]
- 30. Koc B, Karahan S, Adas G, Tutal F, Guven H, et al. (2013) Comparison of laparoscopic common bile duct exploration and endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for choledocholithiasis: a prospective randomized study. Am J Surg 206:457–463. [DOI] [PubMed] [Google Scholar]
- 31. Chaudhary A, Aranya RC (1996) Surgery in perforation after endoscopic sphincterotomy: sooner, later or not at all? Ann R Coll Surg Engl 78:206–208. [PMC free article] [PubMed] [Google Scholar]
- 32. Christensen M, Matzen P, Schulze S, Rosenberg J (2004) Complications of ERCP: a prospective study. Gastrointest Endosc 60:721–731. [DOI] [PubMed] [Google Scholar]
- 33. Wu HM, Dixon E, May GR, Sutherland FR (2006) Management of perforation after endoscopic retrograde cholangiopancreatography (ERCP): a population-based review. HPB (Oxford) 8:393–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Morgan KA, Fontenot BB, Ruddy JM, Mickey S, Adams DB (2009) Endoscopic retrograde cholangiopancreatography gut perforations: when to wait! When to operate!. Am Surg. 75:477–483 discussion 483-474. [PubMed] [Google Scholar]
- 35. Gurung RB, Purbey B, Koju R, Bedi TR (2014) Endoscopic Retrograde Cholangiopancreatography at Dhulikhel hospital: Outcome Analysis. Kathmandu Univ Med J (KUMJ) 12:55–59. [DOI] [PubMed] [Google Scholar]
- 36. Katsinelos P, Lazaraki G, Chatzimavroudis G, Gkagkalis S, Vasiliadis I, et al. (2014) Risk factors for therapeutic ERCP-related complications: an analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol 27:65–72. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper.