Abstract
Many environmental factors contribute to the rise in prevalence of obesity in populations but one key driver is urbanization. Countries in Southeast (SE) Asia have undergone rapid changes in urbanization in recent decades. The aim of this study is to provide a systematic review of studies exploring the relationship between living in an urban or rural environment (urbanicity) and obesity in Southeast Asia. In particular, the review will investigate whether the associations are uniform across countries and ages, and by sex. The literature search was conducted up to June 2014 using five databases: EMBASE, PubMed, GlobalHealth, DigitalJournal and Open Grey. Forty-five articles representing eight of the eleven countries in SE Asia were included in the review. The review found a consistent positive association between urbanicity and obesity in countries of Southeast Asia, in all age groups and both genders. Regional differences between the associations are partly explained by gross national income (GNI). In countries with lower GNI per capita, the association between urbanicity and obesity was greater. Such findings have implications for policy makers. They imply that population level interventions need to be country or region specific, tailored to suit the current stage of economic development. In addition, less developed countries might be more vulnerable to the negative health impact of urbanization than more developed countries.
Introduction
The increasing prevalence of obesity is a phenomenon happening worldwide, with global prevalence almost doubling since 1980 [1]. Previously considered an epidemic of developed countries, in recent years the growing burden of obesity has affected most regions, including Southeast Asia [2]. In Southeast Asia, like other parts of the world, obesity is considered one of the key risk factors for chronic and non-communicable disease [3],[4]. Its burden on health is reflected by the Global Burden of Disease project report [5]. In 1990, high BMI was ranked the 23rd most important risk factor for SE Asia, and by 2010 it was 9th [6].
Many environmental factors contribute to the rise in prevalence of obesity, but one key driver is urbanization [7]. The National Institute of Health defines urbanization as “the process whereby a society changes from a rural to an urban way of life. It refers also to the gradual increase in the proportion of people living in urban areas” [8].
The framework proposed by the International Obesity Taskforce has outlined possible causal pathways between urbanization and obesity [9]. In short, factors operating at the national and international level, such as urbanization, will influence the environment of the individual at the community and family level. Such environmental influences are likely to result in lower levels of physical activity and energy expenditure, coupled with a high energy and high fat diet [10].
Countries in Southeast (SE) Asia have undergone a rapid increase in urbanization in recent decades. The proportion living in an urban area rose from 15% to 32% between 1950 and 1990. By 2010, about 50% of the 600 million people in SE Asia were living in an urban area [11].
Since most studies on the impact of urbanization on health have focused on urban-rural differences [12], the aim of this study is to provide a systematic review of studies exploring the relationship between urban and rural environments (urbanicity) and obesity in Southeast Asia. In particular, the review will investigate whether the associations are uniform across countries and ages, and by sex.
Methods
Search strategies and procedures
The literature search was conducted up to June 2014 using five databases. Three standard international databases in the field of medicine, epidemiology and public health were used: EMBASE (from 1974), PubMed (from 1946), GlobalHealth (from 1910). We used one regional database: DigitalJournal (from 2007), which is an electronic journal database from SE Asian member countries and currently health science journals from Indonesia, Myanmar and Thailand can be searched electronically [13]. We used one database for grey literature and unpublished research: Open Grey (from 1980) [14]. Full articles of relevant abstracts were retrieved through the London School of Hygiene and Tropical Medicine and Chiang Mai University's network. We also conducted an additional cited-reference search from articles included in the review to pick up relevant published and unpublished articles. The search strategy using EMBASE can be found in the supporting document. (Table S1 in File S1)
Inclusion and exclusion criteria
Criteria for articles to be included in the review were that they must:
Have a clearly defined measure for an urban environment
Have a defined measure of obesity
Have a direct control group or comparison group such as a semi-urban or rural comparison group
Report (or have data to be able to calculate) quantitative measures for the association between urban/non-urban environments and obesity
Be published in English.
The eleven countries in SE Asia included in the review were Brunei Darussalam, Cambodia, Indonesia, Laos PDR, Malaysia, Myanmar, Philippines, Thailand, Timor-Leste, and Vietnam and Singapore. However, studies from Singapore were not expected, as the entire country was considered urban. As long as the inclusion criteria were met, we did not have restrictions on the type of study design included. We excluded any studies conducted outside the SE Asian region or studies with historical controls where the prevalence of obesity was measured at different time points within the same study.
Screening and data extraction
Titles and abstracts were screened independently by two reviewers (CA and WJ) and classified into three subgroups:
Clearly not relevant,
Potentially relevant, and
Relevant to review.
Studies that were classified as ‘clearly not relevant’ by both reviewers were excluded during the initial abstract screening process. Full text articles, which were classified as ‘potentially relevant’ or ‘relevant articles’ by one of the reviewers, were retrieved and reviewed by the lead author (CA). Reasons for exclusion (if relevant) were documented (Table S2 in File S1). Authors were contacted if full text articles were not retrievable or if additional information was needed to make a decision on inclusion or exclusion.
A small sample of literature included in the review was used to derive a standard data abstraction form. Information was collected on the lead author's name and year of publication, country and year of fieldwork, study design and sample size, characteristics of the study population (such as age and gender distribution), the definition of urban and non-urban/rural environment, and how the outcome of interest was defined and measured. In addition, the per capita Gross National Income (GNI) corresponding to the country and year of fieldwork was included. If year of fieldwork was not stated, it was assumed to be three years prior to year of publication. For the results section, prevalence and odds ratios were considered to be the main summary measures of interest. Information was also collected on which factors were controlled for if adjusted ratio measures of effect were reported. (Tables S3–S15 in File S1)
Definition of variables for meta-regression
For each observation included in the meta-regression, the following definitions were used to define six variables:
Country of conduct: Based on the total number of observations from each country, the variable “country of conduct” was grouped according to geographical proximity and level of per capita GNI into four groups. They consisted of i) Malaysia and Philippines, ii) Thailand, iii) Vietnam and Laos, and iv) Indonesia and Timor-Leste
Per capita GNI (US dollar) corresponding to year of field work and county of conduct, as reported by the United Nations was obtained [15]. This was categorized into three groups: i) <1,500 dollars, ii) 1,500–2500 dollars iii) >2,500 dollars
Year of fieldwork was categorized into two groups, whether the study was conducted within i) ten years (2004–2013) or ii) earlier (up to 2003)
Age of study population was categorized into two groups: i) children (<18 years old) or ii) adults (≥18 years old)
Sex of study population was categorized into three groups: i) men only, ii) women only, or iii) both (results adjusted for sex)
Obesity classification: The obesity definition differed between individual studies. To explore the different obesity classifications as a source of heterogeneity, the variable “obesity classification” was categorized into three groups according to whether the study used a i) non BMI classification (using waist circumference), ii) a BMI classification (or corresponding percentiles) defining obesity as ≥23 kg/m2 or ≥25 kg/m2, or iii) a BMI classification (or corresponding percentiles) defining obesity as ≥30 kg/m2.
Quality appraisal
The risk of bias within individual studies was assessed according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach [16] as recommended by the Cochrane handbook [17]. In summary, information was collected on potential risk of i) selection bias, ii) confounding and residual confounding, and iii) information bias in the classification of an urban environment status and in the measurement of obesity. Information bias in exposure and outcome variables was also further assessed as likely to be differential or non-differential. Additional limitations of each study were recorded. We used the Preferred Reporting Items for Systematic Review and Meta-Analysis: The PRISMA statement as guidelines for reporting our results [18]. (Table S16 in File S1)
Data analysis
For the results (odds ratios) of an individual article to be included in the meta-analysis, it must have been adjusted for age and sex, or stratified by sex and adjusted for age. If an article presented additional results adjusting for other covariates (such as socioeconomic status), we used the age and sex adjusted results. Additional adjustments could be considered over-adjustments for factors on the causal pathway between urbanicity and obesity.
We took the effect size (odds ratio) as reported by each article. If an article reported summary measures for more than one independent dataset, all available summary measures were used. If there was more than one summary measure reported from a single dataset, such as reporting by different gradients of urbanicity or with additional stratification by sex, we used the most reliable estimate (largest sample size) and the most conservative definition of obesity using BMI classifications. If odds ratios were not directly reported, when possible, we calculated crude odds ratios and CIs based on the proportions provided. However, crude odds ratios were not included in the meta-analysis, as these were not adjusted for age and sex.
High degrees of heterogeneity among studies were expected due to differences in the age distribution and regions of the study populations. Three main subgroup meta-analyses were pre-specified: i) analysis in children; ii) analysis in adult populations; and iii) analysis by country or countries.
In the absence of statistical heterogeneity, the fixed effect model using the inverse variance method was use to summarize the measures of effect. If there was evidence for heterogeneity, the DerSimonion and Laird approach for random effect models was used [19]. Heterogeneity was evaluated using Cochran's Q and I2 statistics. Combining results with high heterogeneity may lead to misleading results [20]. If there was high heterogeneity, I2>80%, the summary measures were displayed using Forest plots without combining effects. Funnel plots were used to evaluate publication bias for the meta-analyses.
Sensitivity Analyses
Random effect meta-regression [21] was used to explore the role of age, gender, time periods, obesity classification, country of conduct, and stage of economic development as measured by per capita GNI as sources of heterogeneity for the association between urban/rural environment and obesity. In presence of potential publication bias, the trim and fill technique was used to explore the its impact [22]. Stata 12 was used in all analyses.
Results
Characteristics of studies
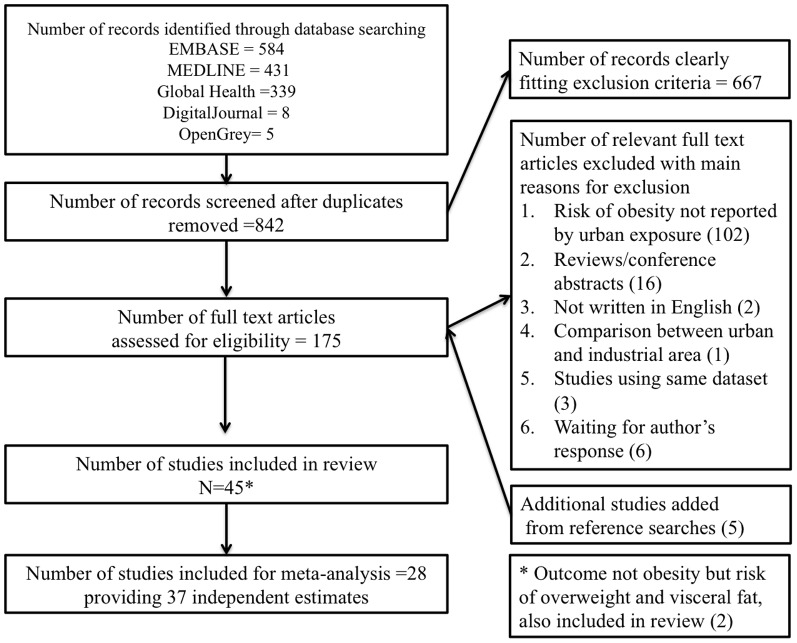
Forty-five studies met the inclusion criteria, and all were cross sectional in design (Figure 1). Eight of the eleven countries in SE Asia were covered by these 45 studies. Thirteen studies were from Malaysia, twelve from Vietnam, nine from Thailand, six from Indonesia, two from Laos, and one each from Philippines, Myanmar and Timor-Leste. Countries for which we found no studies were Brunei Darussalam, Cambodia and Singapore. Twenty-seven studies focused only on adults, seventeen focused only on children and/or adolescents (age <18 years old), and one study included both children and adults but reported estimates separately [23]. Two studies were published in1988 and 1992, the rest were published after 2000. Detailed characteristics of each study can be found in Tables S3–S8 in File S1.
Figure 1. Flow chart of articles included in the review.
The urban environment and obesity in children
Eighteen studies included children, whose ages ranged between 2 and 18. Of these studies, six were from Vietnam [23],[24],[25],[26],[27],[28], six from Malaysia [29],[30],[31],[32],[33],[34], three from Thailand [35],[36],[37], two from Indonesia [38],[39] and one from Laos [40]. All classifications of obesity were age-and-gender specific, but studies differed in the criteria and the cutoff points used for obesity. Six studies used the International Obesity Task Force definition [24],[27],[29],[30],[38],[40], eleven studies used the World Health Organization's standard [23],[24],[25],[28],[31],[32],[33],[34],[35],[37],[39], and one study from Thailand used its own National standard [36].
Sixteen studies, consisting of at least one from each of the five countries presented, reported a significant association between an urban environment and obesity in children [23],[24],[25],[26],[27],[28],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40]. The two studies that did not find a significant association were from Malaysia [29],[30]. Two studies explored a gradient effect between urbanicity and obesity. The study by Julia et al, conducted in Indonesia compared children in three different exposure groups: i) urban, ii) urban poor and iii) rural. The study found that although there were differences in obesity between urban and rural children, these differences were less pronounced when urban poor children were compared with rural children [38]. A gradient effect was also seen in the study by Tang et al, conducted in Vietnam [27]. The adjusted odds ratio for the wealthy urban population compared to the semi-rural and rural population was 5.53 (95% CI 2.42 to 14.16), and the odds ratio for less wealthy urban versus the semi-rural and rural population was 3.82 (95% CI 1.73 to 9.56). Individual results for each of the eighteen studies in children can be found in Tables S9–S11 in File S1.
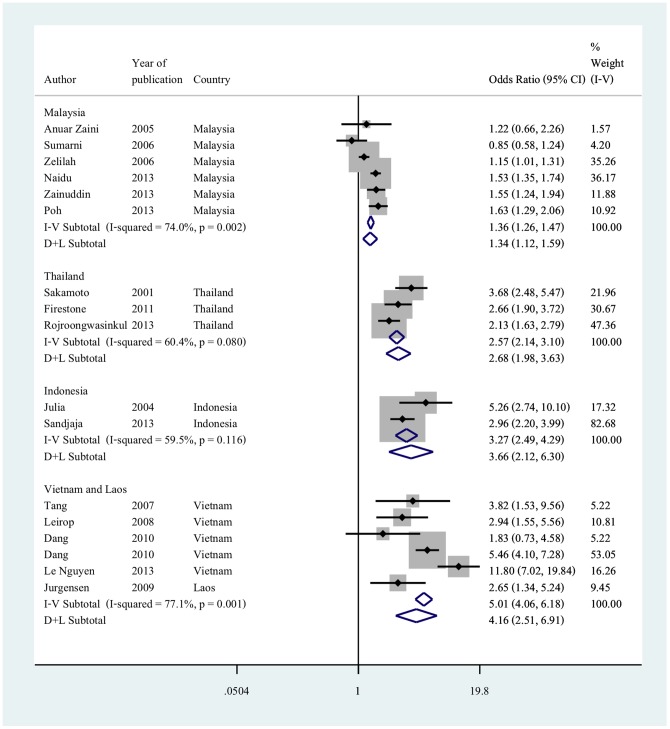
Sixteen of the eighteen studies were included in the meta-analysis [24],[25] [27] [28] [29],[30],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40]. The random effect estimates gave a pooled odds ratio of 1.34 (95% CI 1.12 to 1.59) in studies from Malaysia and 2.68 (95% CI 1.98 to 3.63) in studies from Thailand. The pooled odds ratio was 3.66 (95% CI 2.12 to 6.30) in studies from Indonesia and 4.16 (95% CI 2.51 to 6.91) in studies from Vietnam and Laos (Figure 2).
Figure 2. Adjusted odds ratio for living in an urban environment and obesity in children by country or countries.
Reference group is living in a rural environment; Odds ratios are adjusted for age and sex; countries are grouped according to geographical proximities and gross national income per capita.
The urban environment and obesity in adults
Twenty-eight studies included adults, whose ages ranged between 18 to over 80. Of these studies, seven each were from Vietnam [23],[41],[42],[43],[44],[45],[46] and Malaysia [47],[48],[49],[50],[51],[52],[53], six were from Thailand [54],[55],[56],[57],[58],[59], four from Indonesia [60],[61],[62],[63] and one each from the Philippines [64], Timor-Leste [65] and Myanmar [66] and Laos [67]. Twelve studies, representing Vietnam [23],[41],[44], Thailand [54],[55],[56],[57],[59], Malaysia [47],[49],[50] and Timor-Leste [65], were considered nationally representative of the adult population of these nations. Other study populations which were not considered representative of the national populations included an indigenous population in Malaysia [48], Thai university students [58] and an elderly Malaysian and Laotian populations [51],[67].
Most studies reported obesity as measured by BMI, although using different cut-off points to define obesity. Two reported waist circumference as the only measure of obesity [49],[54]. Fuke et al studied visceral fat in adults from Indonesia with normal BMI and did not find an association between urban-rural differences and visceral fat [62]. Seven studies did not find an association between an urban environment and obesity in adults, four from Malaysia [47],[49],[52],[53] and one each from Vietnam [43], Indonesia [63] and Philippines [64]. Of these seven studies, only two studies were adjusted for both age and gender [53],[64]. Rasiah et al additionally adjusted for level of education [53]. Dahly et al used an urbanicity score as their exposure rather than directly comparing outcomes by urban and rural status [64]. Four studies looked for a gradient effect between urbanicty and obesity in adults [42],[43],[60],[64], all of which reported higher prevalence of obesity in populations with greater levels of urbanization. Results for each of the twenty-eight studies in adults can be found in Tables S12–S15 in File S1.
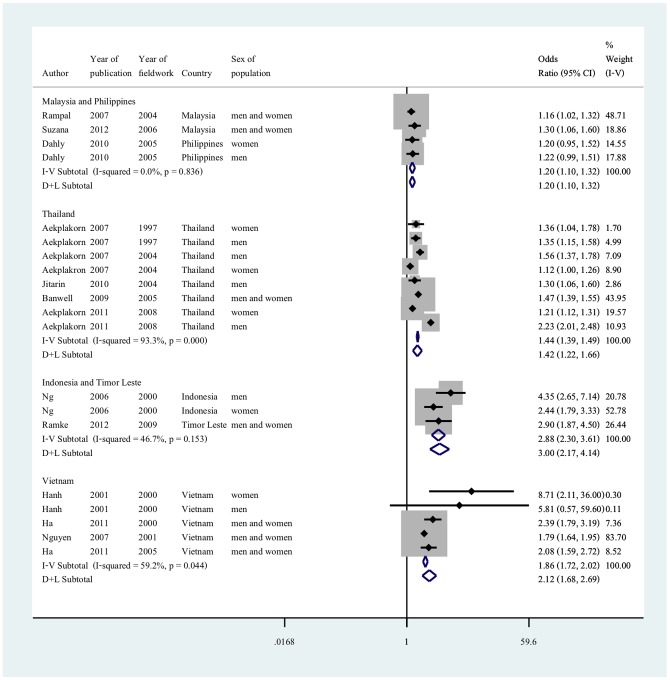
Twelve studies, from six nations, met the criteria for meta-analysis by reporting age and sex adjusted odds ratio. The six nations represented were grouped into four groups taking into consideration geographical proximities and/or similar gross national income level: i) Malaysia and Philippines, ii) Thailand, iii) Indonesia and Timor-Leste and iv) Vietnam (Figure 3). In studies from Malaysia and Philippines, there was no heterogeneity between the results (I2 = 0, p = 0.836). The pooled random effect estimates gave an odds ratio of 1.20 (95% CI 1.10 to 1.32). All adjusted estimates between urbanicity and obesity from Thailand were statistically significant, but had very high heterogeneity (I2 = 93.3, p<0.001). The results from Indonesia and Timor-Leste showed moderate heterogeneity (I2 46.7, p = 0.153), the random effect model gave an adjusted odds ratio of 3.0 (95% CI 2.17 to 4.14). There was moderate heterogeneity between the results from Vietnam (I2 = 59.2, p = 0.044), and the pooled random effect odds ratio was 2.12 (95% CI 1.68 to 2.69).
Figure 3. Adjusted odds ratio for living in an urban environment and obesity in adults by country or countries.
Reference group is living in a rural environment; Odds ratios are adjusted for age and sex (or adjusted for age if stratified by sex); countries are grouped according to geographical proximities and gross national income per capita.
Sources of heterogeneity: Results from Meta-regression
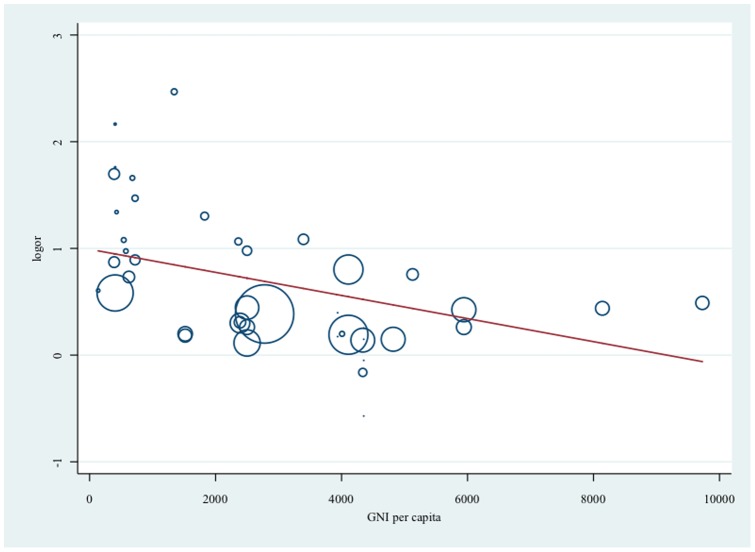
Twenty-eight studies, contributing thirty-seven independent age and sex-adjusted estimates, were included for meta-regression. Exploring six potential sources of heterogeneity separately, results suggested that there was heterogeneity in the association between urbanicity and obesity both within country and between countries of SE Asia (Table 1). Country setting drove much of the heterogeneity in these estimates, which in turn may be related to the economic output of that country at the time the studies were conducted. The pooled measure of association between urbanicity and obesity in countries such as Malaysia and Philippines (OR 1.29, 95% CI 1.14 to 1.45) was smaller than the association seen in lower income countries such as Indonesia and Timor-Leste (OR 3.14, 95% CI 2.22 to 4.46) (Table 1). Figure 4 presents the association between urbanicity and obesity by GNI per capita. There was strong evidence that the association is greater when GNI per capita was smaller. No other sources of heterogeneity were statistically significant but there was some weak evidence that effect size in children may be larger than adults (p = 0.07) (Table 1). When including per capita GNI, country/countries of conduct, and other possible sources of heterogeneity (age and sex of study population, whether the study was conducted within the past ten years or before, and the type of BMI classification for obesity used), these six variables together were able to explain 22.4% of the heterogeneity between results.
Table 1. Adjusted odds ratios (OR) for living in an urban environment and obesity using stratification by country/countries, per capita GNI, year of fieldwork, sex, age of study population and criteria for obesity.
| Stratification | Number of observations | OR for living in an urban environment (95% CI) | P-value | I2 | p-values* | F-ratio (p-value)** |
| None | 37 | 1.99 (1.64 to 2.41) | <0.001 | 92.1% | <0.001 | – |
| Country/countries | 12.16 (<0.001) | |||||
| Philippines and Malaysia | 10 | 1.29 (1.14 to 1.45) | 0.001 | 62.8% | <0.001 | |
| Thailand | 11 | 1.66 (1.30 to 2.11) | 0.001 | 93.2% | <0.001 | |
| Vietnam and Laos | 11 | 3.36 (2.14 to 5.27) | <0.001 | 90.6% | <0.001 | |
| Indonesia and Timor-Leste | 5 | 3.14 (2.22 to 4.46) | 0.001 | 40.4% | <0.001 | |
| Per capita GNI (US dollars) | 12.00 (<0.001) | |||||
| <1,500 | 14 | 3.42 (2.42 to 4.84) | <0.001 | 89.4% | <0.001 | |
| 1,500–2,500 | 10 | 1.62 (1.20 to 2.18) | <0.001 | 86.7% | <0.001 | |
| >2,500 | 13 | 1.50 (1.23 to 1.82) | 0.01 | 91.9% | <0.001 | |
| Year of field work | 0.78 (0.383) | |||||
| 2004 to 2013 | 20 | 1.85 (1.45 to 2.37) | <0.001 | 92.4% | <0.001 | |
| Up to 2003 | 17 | 2.22 (1.60 to 3.09) | <0.001 | 91.9% | <0.001 | |
| Sex of study population | 0.94 (0.407) | |||||
| Men only | 7 | 1.76 (1.14 to 2.73) | 0.020 | 90.8% | <0.001 | |
| Women only | 6 | 1.47 (0.89 to 2.43) | 0.106 | 82.8% | <0.001 | |
| Both | 24 | 2.19 (1.70 to 2.81) | <0.001 | 92.2% | <0.001 | |
| Age of population | 3.57 (0.067) | |||||
| Children | 17 | 2.43 (1.72 to 3.43) | <0.001 | 92.9% | <0.001 | |
| Adults | 20 | 1.65 (1.36 to 1.99) | <0.001 | 90.9% | <0.001 | |
| Obesity classifcation | 1.18 (0.318) | |||||
| Non BMI classifciation (using WC) | 3 | 2.10 (0.53 to 8.28) | 0.145 | 98.0% | <0.001 | |
| Obesity defined BMI≥23 or 25 | 29 | 2.13 (1.69 to 2.67) | <0.001 | 91.1% | <0.001 | |
| Obesity defined as BMI≥30 | 5 | 1.39 (0.90 to 2.16) | 0.104 | 80.9% | <.0.001 |
Twenty eight studies contributed to 37 independent age and sex adjusted estimates (Figure 1); Reference group is living in a rural environment; GNI gross national income; WC waist circumference;
* p-value for heterogeneity chi-square;
** Likelihood ratio test for heterogeneity between subgroup by meta-regression, providing F-ratio and p-values.
Figure 4. Association (log odds ratio) between living in an urban environment and obesity by GNI per capita.
Size of circles reflects sample size. Higher log odds ratio (logor) reflect larger effect size for living in an urban environment and obesity; gross national income (GNI) per capita in US dollar corresponding to year and country of fieldwork; Reference group is living in a rural environment.
Sensitivity analysis
The funnel plots suggested that there was potential for publication bias (Figure S1 and Figure S2). However, sensitivity analysis using the trim-and fill technique did not materially alter any of the results seen. (Table S17 in File S1)
Discussion
To our knowledge, this is the first systematic review to examine the association between living in an urban environment and obesity in SE Asia. The review found consistent positive associations between urbanicity and obesity in countries of Southeast Asia, in both genders and all age groups. We found that different country settings contributed strongly to the source of heterogeneity between the estimates. There was strong evidence that the association between urban environments and obesity is modified by the country's GNI per capita and this partly explained the observed heterogeneity of the estimates.
Sources of Heterogeneity: Regional differences
Associations between urban environments and obesity were expected to vary between countries because of different cultures, and varying political and socioeconomic environments. When the data were grouped according to country or countries with close geographic proximity and similar economic status, some of the observed heterogeneity decreased. The notable exception was Thailand. However, these studies differed in other ways: one was conducted in university students [58], one used abdominal obesity [56] and another used a cut of point of BMI≥23 kg/m2 [33] as the outcome.
A systematic review from developed countries exploring the role of geographic environment on cardiometabolic risk factors, such as obesity, was conducted by Leal and Chaix [68]. The review found that living in a rural environment and areas with lower socioeconomic level was associated with higher BMI but did not look at the effect modification between these two exposures. The review by Leal and Chaix may not be generalizable to developing countries of SE Asia which may explain why we found the opposite, i.e. that the association between living in an urban environment and obesity was positive. Monteiro et al combined nationally representative data on women from 37 developing countries to examine the association between obesity and inequality [69]. The study found that there was interaction between the women's socioeconomic status (SES) and the country's Gross Nation Product (GNP), which was seen as a measure of the environmental level of economic development. Specifically, if the country's GNP per capita was less than 2,500 dollars, high SES was positively associated with obesity. If the country's GNP was greater than 2,500 dollars, the risk of obesity was highest for the poor. These observations support the findings of our review.
One explanation for an interaction between income (or SES) and urbanization (as a development process) on obesity could be sociocultural and behavioral in nature. It could be that in less developed countries people with higher incomes have easier access to a plentiful food supply. Whereas in more developed countries, people with higher income have options to counter-balance the impact of an obesogenic environment [70]. The ‘developmental origins’ theory [71] can also be used to help explain such interactions. If early life under-nutrition is associated with rapid weight gain in childhood and risk of obesity in adults, less developed countries would be more vulnerable to the obesogenic impact of urbanization.
Other sources of heterogeneity between studies
This review also examined whether the association between urban environment and obesity differed between children and adults, and by gender. We found some very weak evidence that the effects were more pronounced in children than in adults. Literature has suggested that for childhood obesity, growth and puberty may interact with the obesogenic environment associated with urbanization [72]. The size of the effect may be reduced for children around puberty as they experience a growth spurt. In SE Asia where the prevalence of obesity is relatively low, there could be a cultural expectation for women to remain slim [2]. However, we did not find evidence that gender modified the association between urban environment and obesity. The current meta-analysis may be underpowered to detect an interaction with gender, and the high heterogeneity between studies could limit generalization of a potential finding.
Strengths and limitations
The review had several limitations. It is possible that not all relevant articles on urban environment and obesity in SE Asia were included in the review. Omitted studies could have been published in other formats such as country reports or could have been published in other databases or in other languages. All studies were of cross-sectional design which, in principle, is susceptible to reverse causality. However, it is difficult to imagine how obesity would drive urbanization. All studies, except one [64], included in this review examined the association between an urban environment and obesity through comparing outcomes in rural and urban settings. Such comparisons do not reflect urbanization as a process, and offer little insight into the underlying mechanisms for the associations found. The failure to account for length of stay in an urban area, transient migration (urban migration to work during parts of the year) and economic diversity within urban areas may have caused bias in the estimates and limit the interpretation of findings. However, even if these biases existed, they are likely to lead to an underestimate of the association between exposure to an urban environment and obesity.
The strengths of the study include conducting the literature search using a regional SE Asian database and exploring the sources of heterogeneity using meta-regression. There was good inter-rater agreement between the reviewers (Kappa 0.85) (Table S18 in File S1). We also reviewed all articles classified as ‘potentially relevant’ or ‘relevant’ irrespective of agreement between the reviewers. Although there was potential for publication bias, our results did not materially alter in the sensitivity analysis. The evidence for interactions between urban living and obesity with the country's GNI per capita was unlikely to be spurious effects due to poorly conducted studies as most studies included in the meta-analysis were assessed to be at low risk of bias (Table S19 and Table S20 in File S1).
Unanswered questions and future research
A better quantification of specific environmental characteristics, carrying out migrant studies, and taking a life-course approach to examine the development of obesity within individuals over time would be useful to enable understanding of the mechanisms underlying the link between urban environments and obesity in this region [72],[73].
Conclusions and Policy Implications
This systematic review found a consistent positive association between living in an urban environment and obesity in countries of Southeast Asia, across all age groups and both genders. Regional differences between the associations are partly explained by gross national income (GNI). The association between urban environments and obesity was stronger in countries with lower GNI per capita. Exposure to an urban environment was associated with 29% higher odds of obesity in Malaysia and Philippines (pooled OR 1.29, 95% CI 1.14 to 1.45). In countries with lower GNI such as Vietnam and Laos, exposure to urban environment was associated with a three-fold increase in obesity (pooled OR 3.36, 95% CI 2.14 to 5.27).
Our findings imply that population level interventions need to be country or region specific, tailored to suit the stage of economic development [74]. Developing countries such as those in SE Asia may be more vulnerable to the negative health impacts of urbanization than more developed countries. A recent report from Malaysia in 2013 highlighted that economic growth has accelerated the problem of obesity though availability of high calorie diets and decreased physical activity in the population. The authors suggested that the creation of healthy infrastructure for active transportation, protection of natural environment, along with healthy and affordable food resources are vital for sustainable economic development [75]. Environmental interventions are recognized as a promising strategy to combat obesity and other obesity-related conditions [76],[77]. School based interventions have been successful in reducing obesity in Singapore [78].Other countries in SE Asia, such as Thailand and Indonesia, have also made progress by adopting population approaches to prevent and control obesity [79].
Supporting Information
Funnel plots of results included in meta-analysis.
(TIFF)
Funnel plots of results included in meta-analysis by country/countries.
(TIFF)
Data extraction worksheet.
(XLSX)
Supporting tables. Table S1: Search strategy using EMBASE. Table S2: List of excluded articles by main reasons for exclusion. Table S3: Study characteristics of studies conducted in children (<18) from Malaysia, Thailand and Indonesia. Table S4: Study characteristics of studies conducted in children (<18) from Laos and Vietnam. Table S5: Study characteristics of studies conducted in adults from Malaysia and Philippines. Table S6: Study characteristics of studies conducted in adults from Thailand. Table S7: Study characteristics of studies conducted in adults from Indonesia and Timor-Leste. Table S8: Study characteristics of studies conducted in adults from Laos, Vietnam and Myanmar. Table S9: Results of studies conducted in children from Malaysia. Table S10: Results of studies conducted in children from Thailand and Indonesia. Table S11: Results of studies conducted in children from Laos and Vietnam. Table S12: Results of studies conducted in adults from Malaysia and Philippines. Table S13: Results of studies conducted in adults from Thailand. Table S14: Results of studies conducted in adults from Indonesia and Timor-Leste. Table S15: Results of studies conducted in adults from Laos, Vietnam and Myanmar. Table S16: PRISMA checklist. Table S17: Sensitivity analysis: Results from random effect meta-regression and trim and fill technique. Table S18: Inter-rater agreement from abstract screening. Table S19: Summary of potential biases within studies among children. Table S20: Summary of potential biases within studies among adults.
(DOCX)
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work. CA is a PhD student funded by the Faculty of Medicine Development Scholarship (Faculty of Medicine, Chiang Mai University, Thailand). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization (2013) Obesity and overweight. Available: http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 2014 Jun 30.
- 2. Prentice AM (2006) The emerging epidemic of obesity in developing countries. International Journal of Epidemiology 35:93–99. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (2000) Obesity: preventing and managing the global epidemic. World Health Organization technical report series 894. [PubMed]
- 4. Dans A, Ng N, Varghese C, Tai ES, Firestone R, et al. (2011) The rise of chronic non-communicable diseases in southeast Asia: time for action. The Lancet 377:680–689. [DOI] [PubMed] [Google Scholar]
- 5. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ (2006) Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 367:1747–1757. [DOI] [PubMed] [Google Scholar]
- 6.Institute for Health Metrics and Evaluatoin. GBD Arrow Diagram. Available: http://www.healthdata.org/data-visualization/gbd-arrow-diagram. Accessed 2013 Sep 30.
- 7. Vlahov D, Freudenberg N, Proietti F, Ompad D, Quinn A, et al. (2007) Urban as a determinant of health. J Urban Health 84:i16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.NCBI. MeSH. Available: http://www.ncbi.nlm.nih.gov/mesh/?term=urbanization. Accessed 2013 Sep 30.
- 9. Kumanyika S, Jeffery RW, Morabia A, Ritenbaugh C, Antipatis VJ (2002) Obesity prevention: the case for action. Int J Obes Relat Metab Disord 26:425–436. [DOI] [PubMed] [Google Scholar]
- 10. Popkin BM (1999) Urbanization, Lifestyle Changes and the Nutrition Transition. World Development 27:1905–1916. [Google Scholar]
- 11.United Nations, Department of Economic and Social Affairs, Population Division (2012) World Urbanization Prospects: The 2011 Revision: Highlights. New York.
- 12. Kinra S (2004) Commentary: Beyond urban–rural comparisons: towards a life course approach to understanding health effects of urbanization. International Journal of Epidemiology 33:777–778. [DOI] [PubMed] [Google Scholar]
- 13.Digital Journals ASEAN Digital Health Science Journals. About us. Available: http://www.digitaljournals.org/content/about-us. Accessed 2014 Jun 30.
- 14.OpenGrey. Database: http://www.opengrey.eu/. Accessed 2014 Jun 30.
- 15.United Nations United Nations Statistics Division. Available: http://unstats.un.org/unsd/snaama/dnllist.asp. Accessed 203 Jul 26.
- 16. Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, et al. (2011) GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). Journal of clinical epidemiology 64:407–415. [DOI] [PubMed] [Google Scholar]
- 17.Higgins JPT, Altman DG (2008) Assessing Risk of Bias in Included Studies. Cochrane Handbook for Systematic Reviews of Interventions: John Wiley& Sons, Ltd. pp. 187–241.
- 18. Moher D, Liberati A, Tetzlaff J, Altman DG, The PG (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. (2009) The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med 6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deeks JJ, Higgins JPT, Altman DG (2008) Analysing Data and Undertaking Meta-Analyses. Cochrane Handbook for Systematic Reviews of Interventions: John Wiley& Sons, Ltd.pp. 243–296.
- 21. Thompson SG, Higgins JP (2002) How should meta-regression analyses be undertaken and interpreted? Stat Med 21:1559–1573. [DOI] [PubMed] [Google Scholar]
- 22. Duval S, Tweedie R (2000) Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463. [DOI] [PubMed] [Google Scholar]
- 23. Tuan NT, Tuong PD, Popkin BM (2008) Body mass index (BMI) dynamics in vietnam. European Journal of Clinical Nutrition 62:78–86. [DOI] [PubMed] [Google Scholar]
- 24. Lierop Av, Nam NV, Doak C, Hung LQ, Binh TQ, et al. (2008) Regional clustering of anthropometric dimensions of primary school children in rural and suburban Vietnam. Asia Pacific Journal of Clinical Nutrition 17:603–607. [PubMed] [Google Scholar]
- 25. Dang CV, Day RS, Selwyn B, Maldonado YM, Nguyen KC, et al. (2010) Initiating BMI prevalence studies in Vietnamese children: changes in a transitional economy. Asia Pacific Journal of Clinical Nutrition 19:209–216. [PubMed] [Google Scholar]
- 26. Ta thi Tuyet M, Nguyen thi Kim H, Kawakami M, Van Chuyen N (2003) Macronutrient intake and nutritional status of primary school-aged girls in rural and urban areas of South Vietnam. Journal of nutritional science and vitaminology 49:13–20. [DOI] [PubMed] [Google Scholar]
- 27. Tang HK, Dibley MJ, Sibbritt D, Tran HMT (2007) Gender and socio-economic differences in BMI of secondary high school students in Ho Chi Minh City. Asia Pacific Journal of Clinical Nutrition 16:74–83. [PubMed] [Google Scholar]
- 28.Le Nguyen BK, Le Thi H, Nguyen Do VA, Tran Thuy N, Nguyen Huu C, et al.. (2013) Double burden of undernutrition and overnutrition in Vietnam in 2011: results of the SEANUTS study in 05–11-year-old children. British Journal of Nutrition 110. [DOI] [PubMed]
- 29. Anuar Zaini MZ, Lim CT, Low WY, Harun F (2005) Factors affecting nutritional status of Malaysian primary school children. Asia-Pacific Journal of Public Health 17:71–80. [DOI] [PubMed] [Google Scholar]
- 30. Sumarni Mohd G, Muhammad Amir K, Ibrahim Md S, Mohd Rodi I, Izzuna Mudla MG, et al. (2006) Obesity among schoolchildren in Kuala Selangor: a cross-sectional study. Tropical biomedicine 23:148–154. [PubMed] [Google Scholar]
- 31. Zalilah MS, Mirnalini K, Khor GL, Merlin A, Bahaman AS, et al. (2006) Estimates and distribution of body mass index in a sample of Malaysian adolescents. Medical Journal of Malaysia 61:48–58. [PubMed] [Google Scholar]
- 32. Naidu BM, Mahmud SZ, Ambak R, Sallehuddin SM, Mutalip HA, et al. (2013) Overweight among primary school-age children in Malaysia. Asia Pacific Journal of Clinical Nutrition 22:408–415. [DOI] [PubMed] [Google Scholar]
- 33. Poh BK, Ng BK, Siti Haslinda MD, Nik Shanita S, Wong JE, et al. (2013) Nutritional status and dietary intakes of children aged 6 months to 12 years: findings of the Nutrition Survey of Malaysian Children (SEANUTS Malaysia). British Journal of Nutrition 110:S21–S35. [DOI] [PubMed] [Google Scholar]
- 34. Zainuddin AA, Selamat R, Baharudin A, Ghaffar SA, Rahim NCA, et al. (2013) Nutritional status of Malaysian primary school children aged 8–10 years: findings from the 2008 National IDD Survey. Malaysian Journal of Nutrition 19:149–161. [Google Scholar]
- 35. Firestone R, Punpuing S, Peterson KE, Acevedo-Garcia D, Gortmaker SL (2011) Child overweight and undernutrition in Thailand: Is there an urban effect? Social Science and Medicine 72:1420–1428. [DOI] [PubMed] [Google Scholar]
- 36. Sakamoto N, Wansorn S, Tontisirin K, Marui E (2001) A social epidemiologic study of obesity among preschool children in Thailand. International Journal of Obesity 25:389–394. [DOI] [PubMed] [Google Scholar]
- 37.Rojroongwasinkul N, Kijboonchoo K, Wimonpeerapattana W, Purttiponthanee S, Yamborisut U, et al.. (2013) SEANUTS: the nutritional status and dietary intakes of 0.5–12-year-old Thai children. British Journal of Nutrition 110. [DOI] [PubMed]
- 38. Julia M, van Weissenbruch MM, de Waal HA, Surjono A (2004) Influence of socioeconomic status on the prevalence of stunted growth and obesity in prepubertal Indonesian children. Food & Nutrition Bulletin 25:354–360. [DOI] [PubMed] [Google Scholar]
- 39.Sandjaja S, Budiman B, Harahap H, Ernawati F, Soekatri M, et al.. (2013) Food consumption and nutritional and biochemical status of 05–12-year-old Indonesian children: the SEANUTS study. British Journal of Nutrition 110. [DOI] [PubMed]
- 40. Jurgensen N, Petersen PE (2009) Oral health and the impact of socio-behavioural factors in a cross sectional survey of 12-year old school children in Laos. BMC oral health 9:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ha TP, Feskens EJ, Deurenberg P, Mai B, Khan NC, et al. (2011) Nationwide shifts in the double burden of overweight and underweight in Vietnamese adults in 2000 and 2005: two national nutrition surveys. BMC Public Health 11:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hanh TTM, Komatsu T, Hung NT, Chuyen VN, Yoshimura Y, et al. (2001) Nutritional status of middle-aged Vietnamese in Ho Chi Minh City. Journal of the American College of Nutrition 20:616–622. [DOI] [PubMed] [Google Scholar]
- 43.Ly KA, Ton TGN, Ngo QV, Vo TT, Fitzpatrick AL (2013) Double burden: a cross-sectional survey assessing factors associated with underweight and overweight status in Danang, Vietnam. BMC Public Health 13. [DOI] [PMC free article] [PubMed]
- 44. Nguyen MD, Beresford SAA, Drewnowski A (2007) Trends in overweight by socio-economic status in Vietnam: 1992 to 2002. Public Health Nutrition 10:115–121. [DOI] [PubMed] [Google Scholar]
- 45. Hanh TTM, Komatsu T, Hung NTK, Chuyen NV, Yoshimura Y, et al. (2001) Blood pressure, serum cholesterol concentration and their related factors in urban and rural elderly of Ho Chi Minh City. Journal of Nutritional Science & Vitaminology 47:147–155. [DOI] [PubMed] [Google Scholar]
- 46. Thu Hien VT, Thi Lam N, Cong Khan N, Wakita A, Yamamoto S (2013) Monosodium glutamate is not associated with overweight in Vietnamese adults. Public Health Nutrition 16:922–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Azmi MY, Junidah R, Siti Mariam A, Safiah MY, Fatimah S, et al. (2009) Body mass index (BMI) of adults: findings of the Malaysian Adult Nutrition Survey (MANS). Malaysian Journal of Nutrition 15:97–119. [PubMed] [Google Scholar]
- 48. Jinam TA, Elvira Phipps M, Indran M, Rani Kuppusamy U, Ameen Mahmood A, et al. (2008) An update of the general health status in the indigenous populations of Malaysia. Ethnicity and Health 13:277–287. [DOI] [PubMed] [Google Scholar]
- 49. Mohamud WNW, Ismail AAS, Khir ASM, Ismail IS, Musa KI, et al. (2012) Prevalence of metabolic syndrome and its risk factors in adult Malaysians: Results of a nationwide survey. Diabetes Research and Clinical Practice 96:91–97. [DOI] [PubMed] [Google Scholar]
- 50. Rampal L, Rampal S, Geok LK, Zain AM, Ooyub SB, et al. (2007) A national study on the prevalence of obesity among 16,127 Malaysians. Asia Pacific Journal of Clinical Nutrition 16:561–566. [PubMed] [Google Scholar]
- 51. Suzana S, Kee C, Jamaludin A, Noor Safiza M, Khor G, et al. (2012) The Third National Health and Morbidity Survey: Prevalence of Obesity, and Abdominal Obesity Among the Malaysian Elderly Population. Asia-Pacific Journal of Public Health 24:318–329. [DOI] [PubMed] [Google Scholar]
- 52. Shariff ZM, Sulaiman N, Jalil RA, Yen WC, Yaw YH, et al. (2014) Food insecurity and the metabolic syndrome among women from low income communities in Malaysia. Asia Pacific Journal of Clinical Nutrition 23:138–147. [DOI] [PubMed] [Google Scholar]
- 53.Rasiah R, Yusoff K, Mohammadreza A, Manikam R, Tumin M, et al.. (2013) Cardiovascular disease risk factors and socioeconomic variables in a nation undergoing epidemiologic transition. BMC Public Health 13. [DOI] [PMC free article] [PubMed]
- 54. Aekplakorn W, Chongsuvivatwong V, Tatsanavivat P, Suriyawongpaisal P (2011) Prevalence of metabolic syndrome defined by the International Diabetes Federation and National Cholesterol Education Program criteria among Thai adults. Asia Pacific Journal of Public Health 23:792–800. [DOI] [PubMed] [Google Scholar]
- 55. Aekplakorn W, Hogan MC, Chongsuvivatwong V, Tatsanavivat P, Chariyalertsak S, et al. (2007) Trends in obesity and associations with education and Urban or rural residence in Thailand. Obesity 15:3113–3121. [DOI] [PubMed] [Google Scholar]
- 56.Aekplakorn W, Kessomboon P, Sangthong R, Chariyalertsak S, Putwatana P, et al.. (2011) Urban and rural variation in clustering of metabolic syndrome components in the Thai population: results from the fourth National Health Examination Survey 2009. BMC Public Health 11. [DOI] [PMC free article] [PubMed]
- 57. Jitnarin N, Kosulwat V, Rojroongwasinkul N, Boonpraderm A, Haddock CK, et al. (2010) Risk factors for overweight and obesity among Thai adults: Results of the national Thai food consumption survey. Nutrients 2:60–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Banwell C, Lim L, Seubsman SA, Bain C, Dixon J, et al. (2009) Body mass index and health-related behaviours in a national cohort of 87 134 Thai open university students. Journal of Epidemiology and Community Health 63:366–372. [DOI] [PubMed] [Google Scholar]
- 59. Suriyawongpaisal P (2003) Cardiovascular risk factor levels in urban and rural Thailand - The International Collaborative Study of Cardiovascular Disease in Asia (InterASIA). European Journal of Cardiovascular Prevention and Rehabilitation 10:249–257. [DOI] [PubMed] [Google Scholar]
- 60. Ng N, Stenlund H, Bonita R, Hakimi M, Wall S, et al. (2006) Preventable risk factors for noncommunicable diseases in rural Indonesia: Prevalence study using WHO STEPS approach. Bulletin of the World Health Organization 84:305–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Sartika RAD (2011) Dietary Trans fatty acids intake and its relation to dyslipidemia in a sample of adults in Depok city, West Java, Indonesia. Malaysian Journal of Nutrition 17:337–346. [PubMed] [Google Scholar]
- 62. Fuke Y, Okabe S, Kajiwara N, Suastika K, Budhiarta AAG, et al. (2007) Increase of visceral fat area in Indonesians and Japanese with normal BMI. Diabetes Research and Clinical Practice 77:S224–S227. [DOI] [PubMed] [Google Scholar]
- 63. Koyama H, Moji K, Suzuki S (1988) Blood pressure, urinary sodium/potassium ratio and body mass index in rural and urban populations in West Java. Human Biology 60:263–272. [PubMed] [Google Scholar]
- 64. Dahly DL, Gordon-Larsen P, Popkin BM, Kaufman JS, Adair LS (2010) Associations between multiple indicators of socioeconomic status and obesity in young adult Filipinos vary by gender, urbanicity, and indicator used. Journal of Nutrition 140:366–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Ramke J, Brian G (2012) BMI among Timorese aged> = 40 years. Public Health Nutrition 15:2118–2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Myo Thet H, Thein N, Nyan T, May Mon K (1992) Prevalence of cardiovascular diseases in rural area of Hmawbi and urban Yangon city. Asia-Pacific journal of public health/Asia-Pacific Academic Consortium for Public Health 6:188–194. [DOI] [PubMed] [Google Scholar]
- 67. Nambooze J, Fujimura M, Inaoka T (2014) Nutritional status and functional capacity of community-dwelling elderly in southern Laos. Environmental Health and Preventive Medicine 19:143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Leal C, Chaix B (2011) The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obesity Reviews 12:217–230. [DOI] [PubMed] [Google Scholar]
- 69. Monteiro CA, Conde WL, Lu B, Popkin BM (2004) Obesity and inequities in health in the developing world. Int J Obes Relat Metab Disord 28:1181–1186. [DOI] [PubMed] [Google Scholar]
- 70.World Health Organization (2003) Diet, nutrition and the prevention of chronic diseases. WHO technical report series 916. [PubMed]
- 71. Barker DJ (2007) The origins of the developmental origins theory. J Intern Med 261:412–417. [DOI] [PubMed] [Google Scholar]
- 72. Canoy D, Buchan I (2007) Challenges in obesity epidemiology. Obesity Reviews 8:1–11. [DOI] [PubMed] [Google Scholar]
- 73. Allender S, Foster C, Hutchinson L, Arambepola C (2008) Quantification of Urbanization in Relation to Chronic Diseases in Developing Countries: A Systematic Review. J Urban Health 85:938–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ebrahim S, Pearce N, Smeeth L, Casas JP, Jaffar S, et al. (2013) Tackling Non-Communicable Diseases In Low- and Middle-Income Countries: Is the Evidence from High-Income Countries All We Need? PLoS Med 10:e1001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Davey TM, Allotey P, Reidpath DD (2013) Is obesity an ineluctable consequence of development? A case study of Malaysia. Public Health 127:1057–1062. [DOI] [PubMed] [Google Scholar]
- 76. Narain JP, Garg R, Fric A (2011) Non-communicable diseases in the South-East Asia region: burden, strategies and opportunities. Natl Med J India 24:280–287. [PubMed] [Google Scholar]
- 77. Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, et al. (2008) Population-Based Prevention of Obesity: The Need for Comprehensive Promotion of Healthful Eating, Physical Activity, and Energy Balance: A Scientific Statement From American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (Formerly the Expert Panel on Population and Prevention Science). Circulation 118:428–464. [DOI] [PubMed] [Google Scholar]
- 78. Toh CM, Cutter J, Chew SK (2002) School based intervention has reduced obesity in Singapore. BMJ 324:427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Leowski J, Krishnan A (2009) Capacity to control noncommunicable diseases in the countries of South-East Asia. Health Policy 92:43–48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Funnel plots of results included in meta-analysis.
(TIFF)
Funnel plots of results included in meta-analysis by country/countries.
(TIFF)
Data extraction worksheet.
(XLSX)
Supporting tables. Table S1: Search strategy using EMBASE. Table S2: List of excluded articles by main reasons for exclusion. Table S3: Study characteristics of studies conducted in children (<18) from Malaysia, Thailand and Indonesia. Table S4: Study characteristics of studies conducted in children (<18) from Laos and Vietnam. Table S5: Study characteristics of studies conducted in adults from Malaysia and Philippines. Table S6: Study characteristics of studies conducted in adults from Thailand. Table S7: Study characteristics of studies conducted in adults from Indonesia and Timor-Leste. Table S8: Study characteristics of studies conducted in adults from Laos, Vietnam and Myanmar. Table S9: Results of studies conducted in children from Malaysia. Table S10: Results of studies conducted in children from Thailand and Indonesia. Table S11: Results of studies conducted in children from Laos and Vietnam. Table S12: Results of studies conducted in adults from Malaysia and Philippines. Table S13: Results of studies conducted in adults from Thailand. Table S14: Results of studies conducted in adults from Indonesia and Timor-Leste. Table S15: Results of studies conducted in adults from Laos, Vietnam and Myanmar. Table S16: PRISMA checklist. Table S17: Sensitivity analysis: Results from random effect meta-regression and trim and fill technique. Table S18: Inter-rater agreement from abstract screening. Table S19: Summary of potential biases within studies among children. Table S20: Summary of potential biases within studies among adults.
(DOCX)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.