Abstract
This study, which is part of a large economic project on the overall burden and cost associated with Foetal Alcohol Spectrum Disorder (FASD) in Canada, estimated the cost of 1:1 speech-language interventions among children and youth with FASD for Canada in 2011. The number of children and youth with FASD and speech-language disorder(s) (SLD), the distribution of the level of severity, and the number of hours needed to treat were estimated using data from the available literature. 1:1 speech-language interventions were computed using the average cost per hour for speech-language pathologists. It was estimated that ˜ 37,928 children and youth with FASD had SLD in Canada in 2011. Using the most conservative approach, the annual cost of 1:1 speech-language interventions among children and youth with FASD is substantial, ranging from $72.5 million to $144.1 million Canadian dollars. Speech-language pathologists should be aware of the disproportionate number of children and youth with FASD who have SLD and the need for early identification to improve access to early intervention. Early identification and access to high quality services may have a role in decreasing the risk of developing the secondary disabilities and in reducing the economic burden of FASD on society.
Keywords: Foetal alcohol spectrum disorder, foetal alcohol syndrome, speech disorders, language disorders, intervention, economic cost
Introduction
According to the Participation and Activity Limitation Surveys, 2001 and 2006, speech disability was the third most prevalent disability (after learning and chronic disabilities) among the 5–14 years age group in the general population of Canada (Statistics Canada, 2007). In 2006, ˜ 45% of children aged 5–14 with one or more disabilities reported a speech disability, meaning that ˜ 78,240 Canadian school-age children experienced difficulty speaking and/or being understood (Statistics Canada, 2007).
Among these children (the broad term “children” will be used to refer to children and youth) with disabilities there is a special population with a very high proportion of speech-language disorders (SLD)—children who were pre-natally exposed to alcohol (CDC, 1995; Church, Eldis, Blakley, & Bawle, 1997; Egeland, Perhain-Hestet, Gessnet, Ingle, Berne, & Miclcldalgh, 1998; Elliott, Payne, Morris, Haan, & Bower, 2008; Kvigne, Leonardson, Neff-Smith, Brock, Borzelleca, & Welty, 2004; Spohr, Willms, & Steinhausen, 1994; Steinhausen, Nestler, & Spohr 1982). Alcohol is a teratogen that causes a spectrum of neurological, cognitive, and behavioural deficits in infants exposed to alcohol in utero (Stratton, Howe, & Battaglia, 1996). Foetal Alcohol Spectrum Disorder (FASD) is an umbrella term used to characterize the full range of damage caused by pre-natal alcohol exposure, varying from mild-to-severe and encompassing a broad array of physical defects as well as cognitive, behavioural, emotional, and adaptive functioning deficits (Chudley, Conry, Cook, Loock, Rosales, & LeBlanc, 2005). FASD includes the following four diagnoses: Foetal Alcohol Syndrome (FAS), Partial FAS (pFAS), Alcohol-related Neurodevelopmental Disorder (ARND), and Alcohol-related Birth Defects (ARBD; Chudley et al., 2005)—all of which may include congenital anomalies, such as malformations and dysplasia of the cardiac, skeletal, renal, ocular, auditory, and other systems. Individuals with FASD are at an increased risk for neglect, abuse, foster care, and disrupted family life (Kvigne et al., 2004), which further increase their risk of developmental adversity.
People with FASD often suffer from SLD due to brain damage caused by the teratogenic effects of pre-natal alcohol exposure (Church et al., 1997). Pre-natal alcohol exposure can disrupt both an individual’s development and their use of language (Mattson & Riley, 1998; Streissguth, Barr, Kogan, & Bookstein, 1996). Individuals with FASD may also be vulnerable to developing SLD as a result of their greater propensity for atypical or adverse social interactions (Coggins, Timler, & Olswang, 2007). Among such SLD are poor receptive and expressive language skills, phonological deficits, fluency and articulation difficulties, and associated neurocognitive abnormalities that can adversely impact speech-language development (Church et al., 1997). In addition, individuals with FASD often have other mental disorders, a well-established dimension of FASD that is also likely to affect language acquisition that may subsequently lead to difficulties with speech and articulation (Church et al., 1997).
Several studies have reported a high occurrence of SLD among individuals with FASD (Church et al., 1997; Egeland et al., 1998; Elliott et al., 2008; Kvigne et al., 2004; Pensiero, Manna, Michieletto, & Perissutti, 2007). Specifically, unspecified SLD have been reported to occur in 40% (CDC, 1995) to 90% (Church et al., 1997) of individuals with FAS, and 37% (Spohr et al., 1994) to 60% (Elliott et al., 2008) of individuals with FASD. Furthermore, Mills, McLennan, and Caza (2006) found, based on self-reports obtained from caregivers, that ˜ 79% of children with FASD under the age of 7 years have visited a speech-language pathologist, and 57% of them received speech and language therapy in Alberta, Canada.
SLD in children with FASD have been linked to learning problems and social difficulties. Due to hearing, speech, and language acquisition problems, individuals with FASD may struggle with social and interpersonal communication, behavioural problems, following social norms, social reasoning, and information processing (Carmichael Olson, 1994; Church et al., 1997; Coggins, Olswang, Carmichael Olsen, & Timler, 2003). For individuals with FASD, these impairments may persist into adolescence and adulthood. Without the crucial support required, people affected by FASD are at a high risk for developing secondary disabilities, such as school failure and drop-out, addictions, mental health problems, sexually deviant behaviour, dependent living, unemployment, homelessness, involvement with the law, and incarceration (Streissguth, Bookstein, Barr, Sampson, O’Mally, & Young, 2004). When combined with the child’s primary deficits, these secondary disabilities increase the complexity of care and result in significant social and economic costs to society (Abel and Sokol, 1987; Harwood 2000; Legge, Roberts, & Butler, 2001; Lupton, Burd, & Harwood, 2004; PHAC 2003, 2005; Popova, Stade, Bekmuradov, Lange, & Rehm, 2011; Popova, Stade, Bekmuradov, Lange, & Rehm, 2012; Stade, Ali, Bennett, Campbell, Johnston, Lens, et al., 2009).
The purpose of this study was 2-fold: first, to estimate the number of children with FASD and SLD by age group (2–4, 5–9, 10–14, 15–19 years), sex, and level of severity (mildly and moderately-to-severely impaired); and, second, to estimate the cost of 1:1 speech-language interventions associated with these disorders in Canada in 2011.
SLD fall under the communication disorders umbrella. A speech disorder refers to an impairment of the respiratory system, phonation system, and/or articulation system of speech production (Justice, 2010). This group of disorders includes articulation and phonological disorders, fluency disorders, voice disorders, and motor speech disorders. A language disorder refers to deficit(s) in the linguistic system that ultimately impacts semantics, syntax, morphology phonology, and/or pragmatics (Justice, 2010).
In the current paper, the term SLD will be used throughout to describe all of the above disorders, and it is assumed that the rates of each are comparable in regard to their treatment and the frequency at which they occur in individuals with FASD.
The current study is part of a large economic project, with multiple components, that is working towards estimating the overall burden and cost associated with FASD in Canada, including the cost of healthcare, law enforcement, children in care, productivity losses of individuals with FASD and their caregivers, along with many others (Popova, Lange, Burd, & Rehm, 2012; Popova, Lange, Mihic, Bekmuradov, & Rehm, 2011; Popova, Stade, Lange, & Rehm, 2012; Popova, Stade, Lange, Mihic, & Rehm, 2012; Popova, Lange, Burd, Chudley, Clarren, & Rehm, 2013). Until now, an estimation of the number of children with FASD and SLD and the associated cost of 1:1 speech-language interventions, at the national level, has not been undertaken in Canada, or in any other country.
Method
Estimation of the number of children with FASD by age group and sex in Canada in 2011
In order to estimate the number of children, aged 2–19, with FASD in Canada in 2011, the only available and most commonly cited prevalence of FASD (nine per 1000; Roberts & Nanson, 2000) was applied to the general population of Canada by age group and sex in 2011 (Statistics Canada, 2012). Please note that children below 2 years of age were excluded due to their natural level of speech-language development during these years. Further, this study did not estimate the cost of 1:1 speech-language interventions among individuals over the age of 19, as most treatments for children with SLD in Canada are linked to the educational system.
Estimation of the number of children with FASD and SLD by age group and sex in Canada 2011
There were three steps involved in estimating the number of children with FASD and SLD by age group and sex in Canada in 2011.
(1) Systematic literature search
A systematic literature search of available epidemiological and medical literature was performed in order to identify studies that have reported the prevalence of SLD among individuals with FASD. The search was conducted in multiple electronic bibliographic databases, including: Ovid MEDLINE, PubMed, EMBASE, Web of Science (including Science Citation Index, Social Sciences Citation Index, Arts and Humanities Citation Index), PsycINFO, ERIC, Scopus, and Social Work Abstracts. The search was conducted using multiple combinations of the following key words: foetal alcohol spectrum disorder, foetal alcohol syndrome, partial foetal alcohol syndrome, foetal alcohol effects, alcohol-related neurodevelopmental disorder, alcohol-related birth defects, pre-natal alcohol exposure, speech, language, disorder*, disabilit*, impairments*, delay*, deficit*, prevalence, frequenc*, and occurrence.
(2) Meta-analysis
The available data on the prevalence of SLD among individuals with FASD was analysed by performing a meta-analysis in order to estimate the pooled prevalence of SLD among individuals with FASD. A double arcsine transformation was applied to the prevalence estimates obtained from the epidemiological studies concerning SLD among those with FASD so that the data followed a normal distribution (Freeman & Tukey, 1950). The double arcsine-transformed prevalence estimates were weighted by the inverse variance of the double arcsine-transformed prevalence. The pooled prevalence of SLD among individuals with FASD was calculated using the Mantel-Haenszel method, assuming a random-effects model (Mantel & Haenszel, 1959). Heterogeneity between studies was assessed using the I2 statistic (Higgins & Thompson, 2002). Results of the meta-analysis were displayed using a Forest plot.
Publication bias was tested by visually inspecting a funnel plot for skewed distribution, and was adjusted for, if present, using the trim and fill method (Duval & Tweedie, 2000).
(3) Estimation
The pooled prevalence of SLD among individuals with FASD was applied to the number of children with FASD by age group and sex in Canada, in order to estimate the number of children with FASD and SLD by age group and sex in Canada in 2011.
Estimation of the number of children with FASD and SLD by level of severity in Canada 2011
The number of children with FASD and SLD by level of severity was estimated based on data from the only available study (Coggins et al., 2007). The authors of this study examined communication deficits among 393 school-aged children with FASD. These children completed numerous standardized tests of language performance, which assessed their fundamental language skills, language comprehension, language development, overall language competence, and word knowledge. Further, the authors indexed the data on a language severity scale containing three levels—normal, mildly impaired, and moderately-to-severely impaired. The data were gathered from each participant using norm-referenced, standardized language tests. The mildly impaired severity level applied to children who obtained scores that ranged between -1.25 SD and -2.00 SD from test means, while the moderately-to-severely impaired level applied to children with test scores that fell more than -2.00 SD below test means. Sixty-nine per cent of the children with FASD displayed significant language deficits, with 31% scoring in the mildly impaired range and 38% classified as moderately-to-severely impaired. This distribution of severity was applied to the total number of children with FASD and SLD in order to estimate the number of children with FASD and SLD by level of severity in Canada in 2011.
Estimation of the cost associated with 1:1 speech-language interventions among children with FASD and SLD by age group, sex, and level of severity in Canada 2011
There were two steps involved in estimating the cost associated with 1:1 speech-language interventions among children with FASD and SLD by age group, sex, and level of severity in Canada in 2011:
(1) Estimation of the average number of hours required for 1:1 speech-language interventions
In order to calculate the average number of hours required for 1:1 speech-language interventions, a systematic review and meta-analysis of randomized control trials on speech-language therapy was used (Law, Garrett, & Nye, 2003). This study revealed an overall positive effect of speech-language interventions for children with expressive phonological and expressive vocabulary difficulties. Based on the 27 studies included in the review by Law et al. (2003), the average number of hours for interventions ranged from 20–30 hours (Table I). Therefore, 20 hours was used as the number of hours needed to treat those who were mildly impaired, and 30 hours was used as the number of hours needed to treat those who were moderately-to-severely impaired.
Table I.
Length of therapy provided to participants in 27 randomized control trials for 1:1 speech-language interventions.
| Reference | Length of intervention (as reported in the original article) | Length of intervention (hours) |
|---|---|---|
| Almost & Rosenbaum (1998) | 80 minutes a week over 4 months | 21.3 |
| Barratt, Littlejohns, & Thompson (1992) | 40 minutes weekly over 6 months | 16 |
| Cole & Dale (1986) | 600 minutes a week given for 8 months | 320 |
| Dixon, Joffe, & Bench (2001) | 30 minutes a week for 10 weeks | 5 |
| Fey, Cleave, Long, & Hughes (1993) | 180 minutes a week for 4.5 months | 54 |
| Fudala, England, & Ganoung (1972) | 25 minutes a week for 4.5 months | 7.5 |
| Gibbard (1994) (study 1) | 40 minutes a week over 6 months | 16 |
| Gibbard (1994) (study 2) | 30 minutes a week for 6 months | 12 |
| Girolametto, Pearce, & Weitzman (1996a) | 150 minutes a week for 10 weeks | 25 |
| Girolametto, Pearce, & Weitzman (1996b) | 150 minutes a week for 11 weeks | 27.5 |
| Glogowska, Roulstone, Enderby, & Peters (2000) | 10 minutes a week for 8.4 months | 5.6 |
| Lancaster (1991) | 17 minutes of therapy a week over 6 months | 6.8 |
| Law, Kot, & Barnett (1999) | 450 minutes a week for 6 weeks | 45 |
| Mulac & Tomlinson (1977) | 67 minutes of therapy a week for 4 weeks | 4.47 |
| Munro (1999) | 60 minutes a week for 6 weeks | 6 |
| Reid, Donaldson, Howell, Dean, & Greive (1996) | 30 minutes given a week lasting up to 10 weeks | 5 |
| Robertson (1997) | 20 minutes of therapy a week provided over 3 weeks | 1 |
| Robertson & Weismer (1999) | 150 minutes a week for 12 weeks | 30 |
| Ruscello, Cartwright, Haines, & Shuster (1993) | 120 minutes a week for 8 weeks | 16 |
| Rvachew (1994) | 45 minutes a week over 6 weeks | 4.5 |
| Rvachew & Nowak (2001) | 30 minutes a week for 12 weeks | 6 |
| Shelton, Johnson, Ruscella, & Arndt (1978) | 57 days (listening for 5 minutes a day and reading and talking for 15 minutes a day) | 19 |
| Sommers (1962) | 200 minutes a week for 4 weeks | 13.3 |
| Sommers, Furlong, Rhodes, Fichter, Bowser, Copetas, et al. (1964) | 200 minutes a week for 4 weeks | 13.3 |
| Sommers, Schaeffer, Leiss, Gerber, Bray, Fundrella, et al. (1966) | 40 minutes of therapy a week for 8.5 months | 22.7 |
| Tufts & Holliday (1959) | 60 minutes a week for 7 months | 28 |
| Wilcox, Kouri, & Caswell (1991) | 90 minutes a week for 3 months in individual condition and 360 minutes a week in group condition for three months | 90 |
Calculated average: 20 hours (outliers removed: Robertson, 1997; Cole & Dale, 1986) to 30.4 hours (all studies).
Adapted from Law et al. (2003).
(2) Calculation of the cost associated with 1:1 speech-language interventions
The cost per hour for a speech-language pathologist was obtained from the Canadian Association of Speech-Language Pathologists and Audiologists (CASLPA; personal communication with Joanne Charlebois, Executive Director), which was estimated to range from $75 (lower estimate) to $149 (upper estimate) in 2011. These figures were obtained from a fee survey conducted by the CASLPA of their members, and represent the average provincial responses to the survey (this survey is available to members of the association only).
In order to estimate the cost associated with 1:1 speech-language interventions, the lower ($75) and upper ($149) estimates of the cost per hour were applied to the number of hours needed to treat (20 hours for mildly impaired and 30 hours for moderately-to-severely impaired), and multiplied by the respective number of children with FASD and SLD estimated for each province/territory in Canada, by age group and sex.
To estimate the costs for Canada in 2011 associated with 1:1 speech-language interventions among children with FASD and SLD, the following assumptions were made. First, it was assumed that the incidences of FASD and SLD and of the mortality rate (especially in people of younger ages with FASD and SLD) remain stable over time. It was also assumed that the population and the percentage of the population that is screened for FASD (based on the existing clinical capacity of all FASD multidisciplinary clinics in Canada; Clarren, Lutke, & Sherbuck, 2011) and SLD are also stable over time. Furthermore, it was assumed that the screening techniques used to diagnose FASD and SLD have not changed over time in terms of their sensitivity and specificity. However, since there have been increases in the population (Statistics Canada, 2013), improvements in the use of screening techniques for FASD (Chudley et al., 2005), and stable rates of consuming alcohol while pregnant (Statistics Canada, 2011), the use of the previously-noted assumptions allowed for a conservative estimate of the cost associated with 1:1 speech-language interventions among children with FASD and SLD for Canada in 2011 to be made.
All cost figures are presented in 2011 Canadian dollars.
Sensitivity analysis
The main analysis was performed using the estimated pooled prevalence of SLD among individuals with FASD. Subsequently, a sensitivity analysis was performed using the 95% confidence interval (CI) as the lower and upper estimates.
Results
Estimated number of children with FASD by age group and sex in Canada in 2011
In Canada in 2011, it was estimated that, in total, there were 63,637 children (32,650 boys and 30,986 girls), aged 2–19, with FASD.
Estimated number of children with FASD and SLD by age group and sex in Canada in 2011
(1) Systematic literature search
The systematic literature search revealed seven studies that reported the prevalence of SLD among individuals with FASD (CDC, 1995; Church et al., 1997; Egeland et al., 1998; Elliott et al., 2008; Kvigne et al., 2004; Spohr et al., 1994; Steinhausen et al., 1982; Table II).
Table II.
Studies reporting on the prevalence of SLD among children with FASD.
| Condition/reference | ICD-10 Code | Country | Sample size/diagnosis | Age (mean) | FASD (% affected) |
|---|---|---|---|---|---|
| Specific developmental disorders of speech and language | F80 | ||||
| CDC (1995) | USA | 60 FAS | 8 | 40% | |
| Church et al. (1997) | USA | 22 FAS | 11.5 | 90% | |
| Egeland et al. (1998) | USA | 145 FAS | .6 (median) | 41% | |
| Elliott et al. (2008) | Australia | 92 FASD (25 FAS + 65 pFAS + 2 suspected FAS) | 3.3 (median) | 60% | |
| Kvigne et al. (2004) | USA | 78 FASD (43 FAS + 35 pFAS) | FAS (10.0); pFAS (9.8) | 58% | |
| Spohr et al. (1994) | Germany | 44 FASD (8 FAE + 36 FAS) | 15.3 | 37% | |
| Steinhausen et al. (1982) | Germany | 68 FAS | 4.3 | 88% | |
| Specific speech articulation disorder | F80.0 | ||||
| Church et al. (1997) | USA | 22 FAS | 11.5 | 10% | |
| Expressive language disorder | F80.1 | ||||
| Church et al. (1997) | USA | 22 FAS | 11.5 | 76% | |
| Receptive language disorder | F80.2 | ||||
| Church et al. (1997) | USA | 22 FAS | 11.5 | 82% | |
| Stuttering [stammering] | F98.5 | ||||
| Church et al. (1997) | USA | 22 FAS | 11.5 | 5% | |
| Cluttering | F98.6 | ||||
| Church et al. (1997) | USA | 22 FAS | 11.5 | 5% |
FAE, Foetal Alcohol Effects; FAS, Foetal Alcohol Syndrome; FASD, Foetal Alcohol Spectrum Disorder; ICD-10, International Classification of Diseases, Version 10; pFAS, Partial Foetal Alcohol Syndrome.
Note: Meta-analysis was based on F80 code (“Specific developmental disorders of speech and language”) only.
(2) Meta-analysis
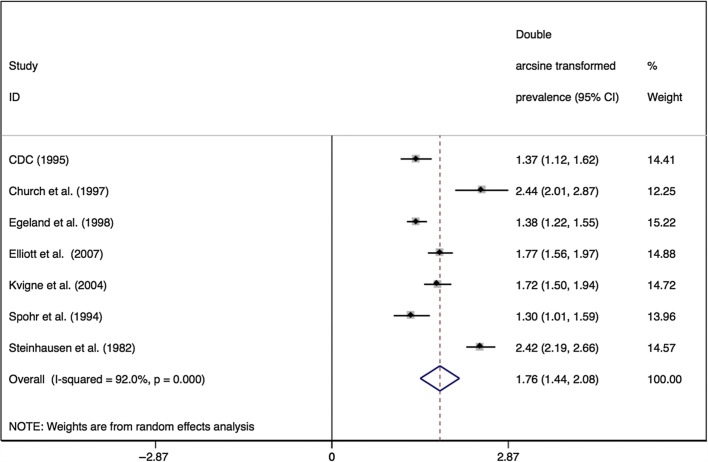
The random effects analysis of the seven studies that reported the prevalence of SLD among children with FASD indicated an overall pooled prevalence of 59.6% (95% CI = 43.4–74.8%). The I2 statistic demonstrated that heterogeneity between studies was present [I2 = 92.0%, p = .000]. Figure 1 depicts the Forest plot for the meta-analysis of the double arcsine-transformed prevalence of SLD among children with FASD with the studies presented in the order they appear in Table I.
Figure 1.
Forest plot of the seven studies that reported the prevalence of SLD among children with FASD. Note: The size of the box around the point estimate is representative of the weight of the estimate used in calculating the aggregated point estimate. CI, Confidence Interval.
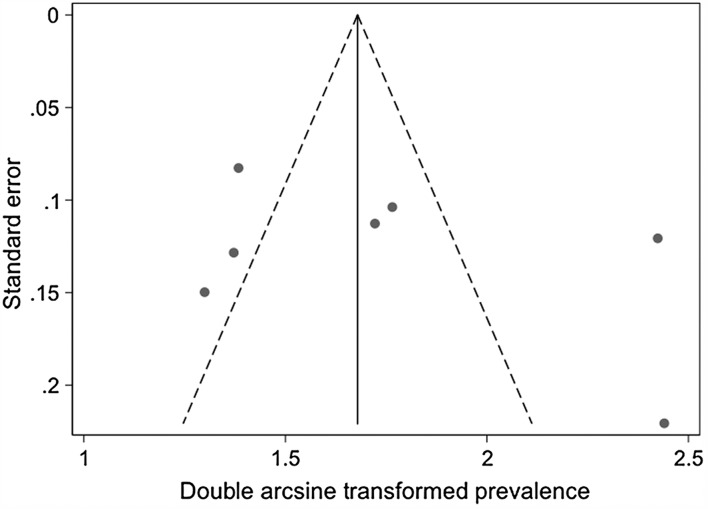
The funnel plot (see Figure 2) of all studies on the prevalence of SLD among children with FASD (with the double arcsine-transformed prevalence plotted against the standard error of the double arcsine-transformed prevalence estimates) formed a random scatter plot; since random effects were present, the funnel plot could be used to determine if publication bias was present.
Figure 2.
Funnel plot of the seven studies that measured the prevalence of SLD among children with FASD used in the meta-analysis with pseudo 95% Confidence Interval.
Estimation of the number of children with FASD and SLD by age group, sex, and level of severity in Canada in 2011
By applying the pooled prevalence of 59.6% (calculated in the meta-analysis described above), it was estimated that there were 37,928 children with FASD and SLD in Canada in 2011. There were 17,067 children with FASD who had mild SLD (8757 boys and 8311 girls), and 20,860 children with FASD who had moderate-to-severe SLD (10,703 boys and 10,157 girls; Table III).
Table III.
Total number of children with FASD and SLD, and the cost associated with 1:1 speech-language interventions by age group and sex in Canada in 2011.
| Sex | Age group; severity level of impairment | Total population (2011)a | Estimated number of children with FASDb | Number of children with FASD and SLDc,d | Total cost of 1:1 speech-language interventions for children with FASDe,f |
|
|---|---|---|---|---|---|---|
| Lower boundary (20 hours; $75 per hour) | Upper boundary (30 hours; $149 per hour) | |||||
| Boys | 2–4 years | 588,548 | 5,297 | 3,157 | $6,037,708 | $11,994,913 |
| Mildly impaired | 1,421 | $2,130,956 | $4,233,499 | |||
| Moderately-to-severely impaired | 1,736 | $3,906,752 | $7,761,414 | |||
| 5–9 years | 939,635 | 8,457 | 5,040 | $9,639,387 | $19,150,248 | |
| Mildly impaired | 2,268 | $3,402,136 | $6,758,911 | |||
| Moderately-to-severely impaired | 2,772 | $6,237,250 | $12,391,337 | |||
| 10–14 years | 975,941 | 8,783 | 5,235 | $10,011,837 | $19,890,183 | |
| Mildly impaired | 2,356 | $3,533,590 | $7,020,065 | |||
| Moderately-to-severely impaired | 2,879 | $6,478,248 | $12,870,118 | |||
| 15–19 years | 1,123,671 | 10,113 | 6,027 | $11,527,348 | $22,900,997 | |
| Mildly impaired | 2,712 | $4,068,476 | $8,082,705 | |||
| Moderately-to-severely impaired | 3,315 | $7,458,872 | $14,818,292 | |||
| Girls | 2–4 years | 560,268 | 5,042 | 3,005 | $5,747,593 | $11,418,552 |
| Mildly impaired | 1,352 | $2,028,562 | $4,030,077 | |||
| Moderately-to-severely impaired | 1,653 | $3,719,031 | $7,388,475 | |||
| 5–9 years | 885,964 | 7,974 | 4,752 | $9,088,795 | $18,056,405 | |
| Mildly impaired | 2,139 | $3,207,810 | $6,372,849 | |||
| Moderately-to-severely impaired | 2,614 | $5,880,985 | $11,683,556 | |||
| 10–14 years | 924,042 | 8,316 | 4,957 | $9,479,423 | $18,832,455 | |
| Mildly impaired | 2,230 | $3,345,679 | $6,646,749 | |||
| Moderately-to-severely impaired | 2,726 | $6,133,745 | $12,185,706 | |||
| 15–19 years | 1,072,690 | 9,654 | 5,754 | $11,004,351 | $21,861,978 | |
| Mildly impaired | 2,589 | $3,883,889 | $7,715,992 | |||
| Moderately-to-severely impaired | 3,165 | $7,120,463 | $14,145,986 | |||
| Total | 7,070,759 | 63,637 | 37,928 | $72,536,442 | $144,105,731 | |
| Sensitivity analysis, assuming 43.4% (lower estimate) of children with FASD have SLD | ||||||
| Mildly impaired | 12,428 | $18,642,459 | $37,036,352 | |||
| Moderately-to-severely impaired | 15,190 | $34,177,842 | $67,899,979 | |||
| Total | 7,070,759 | 63,637 | 27,618 | $52,820,301 | $104,936,331 | |
| Sensitivity analysis, assuming 74.8% (upper estimate) of children with FASD have SLD | ||||||
| Mildly impaired | 21,420 | $32,130,321 | $63,832,238 | |||
| Moderately-to-severely impaired | 26,180 | $58,905,589 | $117,025,770 | |||
| Total | 7,070,759 | 63,637 | 47,600 | $91,035,910 | $180,858,009 | |
FASD, Foetal Alcohol Spectrum Disorder; SLD, speech-language disorder(s).
Note: Column numbers may not add up due to rounding error.
Obtained from Statistics Canada (2012).
Calculated based on a prevalence of nine per 1000 (Roberts & Nanson, 2000).
Based on data by Coggins et al. (2007).
Calculated based on a prevalence of 596 per 1000.
Calculated using data on the average number of hours adapted from Law et al. (2003).
Calculated using data on the average cost per hour for a speech-language pathologist obtained from the Canadian Association for Speech-Language Pathologists and Audiologists (CASLPA).
Estimation of the cost association with 1:1 speech-language interventions among children with FASD and SLD by age group, sex, and level of severity in Canada in 2011
It was estimated that the total cost associated with 1:1 speech-language interventions for children with FASD with mild SLD ranged from $25.6–50.9 million. For children with FASD with moderate-to-severe SLD, the total costs associated with 1:1 speech-language interventions ranged from $46.9–94.8 million. The total cost of 1:1 speech-language interventions for children with FASD ranged from $72.5–144.1 million (Table III). Please note that the estimated number of children with FASD and SLD, and the costs associated with 1:1 speech-language interventions by age group, sex, and level of severity for each province/territory in Canada in 2011, are available from the authors.
Sensitivity analysis
Assuming that 43.4% (as the lower estimate) of children with FASD have SLD, it was estimated that there were 27,618 children with FASD and SLD (12,428 with mild SLD and 15,190 with moderate-to-severe SLD) in Canada in 2011. In turn, it was estimated that the cost associated with 1:1 speech-language interventions for these children ranged from $52.8–104.9 million. Assuming that 74.8% (as the upper estimate) of children with FASD have SLD, it was estimated that there were 47,600 children with FASD and SLD (21,420 with mild SLD and 26,180 with moderate-to-severe SLD) in Canada in 2011. The resulting estimated cost associated with 1:1 speech-language interventions for these children ranged from $91–180.9 million. The results of the sensitivity analysis are presented in Table III.
Discussion
This is the first study that has attempted to estimate the number of children with FASD and SLD and the cost associated with speech-language interventions (not only in Canada, but also in any other country of the world). The results of this study demonstrate that the number of children with FASD and SLD and the annual cost associated with 1:1 speech-language interventions in Canada is substantial. It is important to highlight that the cost of speech-language interventions is only part of the overall direct healthcare costs associated with FASD in Canada.
There are several limitations of the current study which have to be considered. To begin, it should be noted that the prevalence of FASD is unknown in Canada; therefore, for the purpose of this analysis, the only available and most commonly cited rough estimate of nine per 1000 (Roberts & Nanson, 2000) was used to estimate the number of children with FASD, which may not be accurate.
Further, the presented cost of speech-language interventions may be over-estimated due to the following reasons. First, it was assumed that all children with FASD and SLD require and receive 1:1 speech-language interventions. Second, the severity distribution of SLD was taken from the study of Coggins et al. (2007), where 69% of children with FASD had a significant language impairment. However, more than 40% of these children had experienced substantial adverse environmental conditions (e.g., abuse, neglect, negative caregiving, etc.). Such environments are likely to exert a negative influence on language development, particularly social communication, in a way that children with FASD without these adverse environments would not encounter. Third, the available literature on the prevalence of SLD among children with FASD, which was used to calculate the pooled FASD prevalence in this study, is dominated by FAS-specific data (Table II).
Furthermore, it should be considered when interpreting these findings that there is no agreement as to the number of treatment sessions or the length of the sessions that speech-language pathologists should provide for specific disorders, and it is likely that interventions are client-specific rather than disorder-specific. As such, there is the possibility that the number of hours for speech-language interventions may be much longer or shorter for some children than those used in this study. For example, according to Dr Larry Burd (Director), the North Dakota Foetal Alcohol Syndrome Centre offers younger children and intensive therapy for a longer duration. Most children with FASD in this centre receive therapy at least once a week, with many receiving therapy two or more times a week, and therapy often continues for a couple of years. For at least 15% of children with FASD at this centre, therapy will last for 4–6 years. Depending on the length of the intervention, the costs could fluctuate (can be higher or lower).
Moreover, speech-language interventions can take on many forms, for example, clinic-based or parent-administered and 1:1 sessions or group sessions. Like all types of disability, there is no cure for SLD; however, there are effective therapies. Children with SLD often qualify for an Individualized Education Plan, as well as other particular services. These services typically include 1:1 interventions with a speech-language pathologist. Even though 1:1 intervention may be advantageous for some SLD, there are other treatment models available and utilized.
The current estimates provide both national and international policy-makers and decision-makers alike with a clear perspective on the magnitude of the burden and cost associated with children with FASD and SLD. The findings of this study are important for a variety of reasons, namely: (1) early intervention may improve the outcome of children with FASD and SLD; (2) early intervention may reduce rates or risk of developing secondary disabilities; (3) speech-language pathologists have an opportunity to play a key role in first appreciating risk factors for FASD; (4) speech-language interventions settings may be one of several optimal locations to screen for FASD; (5) supporting the implementation of prevention strategies to reduce/eliminate the consumption of alcohol during pregnancy could have a cost-saving effect; (6) they will raise awareness of not only the consequences of consuming alcohol during pregnancy, but also of the wide range of impairments seen in individuals with FASD; and (7) they will lead to increased awareness of speech-language pathologists to the disproportionate number of children with FASD that they will likely work with during their careers. Moreover, the cost estimates presented can be used to promote the allocation of resources to programs specifically for children with FASD.
Given the high prevalence of SLD among children with FASD, speech-language pathologists will frequently come into contact with children affected by FASD. Speech-language pathologists working in early intervention, serving children with birth defects, behavioural problems, developmental delays, and children in foster care or juvenile corrections settings may have significantly high rates of children with FASD in their caseload. Unfortunately, FASD is not widely recognized by healthcare practitioners (Clark & Tough, 2003); therefore, FASD is largely under-diagnosed (Paintner, Williams, & Burd, 2012). Early screening may lead to early diagnosis, which can lead to early participation in developmental interventions, and this, in turn, can prevent the development of secondary disabilities and improve the quality-of-life for people with FASD and their families (see for example, Paintner et al., 2012).
Speech-language pathologists are in a unique position, as they may be one of the first contacts with the healthcare system for children with FASD; there are a number of ways in which this opportunity can be maximized. First, it would be useful to review the pre-service training and in-service training to determine if additional information on FASD may be needed, such as FASD recognition and the specific needs of children with FASD. Second, improving the capacity for speech-language pathologists to effectively screen children on their caseload for FASD and provide referrals to diagnostic clinics where a diagnosis can be established, if appropriate. The FASD Canadian Diagnostic Guidelines clearly states that speech-language pathologists should be part of the core diagnostic team (Chudley et al., 2005). Third, improved screening and increased training on FASD could increase referral rates for other related services (audiologists, occupational therapists, physical therapists, etc.). A comprehensive approach to intervention and early participation of the other disciplines, where needed, could increase the amount of early intervention and, thus, could potentially improve outcomes (Olson, Jirikowic, Kartin, & Astley, 2007).
Lastly, the high rates of SLD among children with FASD suggest that there is an increased need for comprehensive treatment plans that specifically target individuals with FASD. Designing targeted interventions for children with FASD and SLD may have implications for learning and behaviour, interpersonal communication, and social skill development (Wyper & Rasmussen, 2011).
According to clinical observations, the link between SLD and behaviour problems is common. Children with SLD appear to be over-represented in the group of children with temper tantrums, sleep disturbance, increased irritability, aggression, and attention deficit hyperactivity disorder. Speech-language pathologists are often the first professionals to begin the process of managing these behavioural problems in the context of therapy. Anecdotal data suggest that this strategy is often effective. Further research to understand improved management pathways may be very useful for speech-language pathologists working with this population. Further efforts to better understand the link between SLD and behavioural disorders may have important influence on improved early intervention and decreasing the risk of developing secondary disabilities in this population.
Further studies are needed to determine the types of speech-language interventions children with FASD are currently receiving and whether children with FASD are effectively treated with the same interventions developed for children without FASD. Such information is necessary to determine if program accommodations are necessary for children with FASD. In addition, the limitations of the current study draw attention to the need for accurate prevalence estimates of SLD among individuals with FASD, and the need for cost analyses to be conducted using other delivery methods, not only in Canada, but in other countries as well.
Although this study has several limitations, it does provide a working estimate, which is a powerful tool for understanding the enormous economic burden that FASD has on the healthcare system overall—speech-language interventions being only one facet of the total healthcare cost. Additional research can refine these estimates over time.
Acknowledgements
This research was supported by the Public Health Agency of Canada (PHAC) [contract number 4500278412].
The authors would also like to thank Dr. Truman E. Coggins, Department of Speech and Hearing Sciences, University of Washington for his thoughtful comments on this paper.
Footnotes
Declaration of interest The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Notice of correction
The version of this article published online ahead of print on 18 Dec 2013 contained two errors on page 7 In Table III, the column total reported for the number of children with FASD and SLD “33,091” should have read “37,928”, and the row heading “Sensitivity analysis, assuming 74.8% (lower estimate) of children with FASD and SLD” should have read “Sensitivity analysis, assuming 74.8% (upper estimate) of children with FASD and SLD”. Lastly, the Acknowledgements were omitted. This omission and the above errors have been corrected for this version.
References
- 1.Abel E. L., Sokol R. J. Incidence of fetal alcohol syndrome and economic impact of FAS-related anomalies. Drug and Alcohol Dependence. (1987);19:51–70. doi: 10.1016/0376-8716(87)90087-1. [DOI] [PubMed] [Google Scholar]
- 2.Almost D., Rosenbaum P. Effectiveness of speech intervention for phonological disorders: A randomized controlled trial. Developmental Medicine and Child Neurology. (1998);40:319–325. [PubMed] [Google Scholar]
- 3.Barratt J., Littlejohns P., Thompson J. Trial of intensive compared to weekly speech therapy in preschool children. Archives of Disease in Childhood. (1992);671:106–108. doi: 10.1136/adc.67.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carmichael Olson C. The effects of prenatal alcohol exposure on child development. Infants & Young Children. (1994);6:10–25. [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Use of international classification of diseases coding to identify fetal alcohol syndrome–Indian Health Service facilities, 1981–1992. Morbitity and Mortality Weekly Report. (1995);44:253–261. [PubMed] [Google Scholar]
- 6.Chudley A., Conry J., Cook J., Loock C., Rosales T., LeBlanc N. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Canadian Medical Association Journal. (2005);172((Suppl. 5)):S1–S21. doi: 10.1503/cmaj.1040302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Church M. W., Eldis F., Blakley B. W., Bawle E. V. Hearing, language, speech, vestibular, and dentofacial disorders in fetal alcohol syndrome. Alcoholism: Clinical and Experimantal Research. (1997);21:227–237. [PubMed] [Google Scholar]
- 8.Clark M. E., Tough S. C. A national survey regarding the knowledge and attitudes of health professions about fetal alcohol syndrome. Ottawa, ON: Health Canada; (2003). [Google Scholar]
- 9.Clarren S. K., Lutke J., Sherbuck M. The Canadian Guidelines and the Interdisciplinary Clinical Capacity of Canada to diagnose Fetal Alcohol Spectrum Disorder. Journal of Population Therapeutics and Clinical Pharmacology. (2011);18:e494–e499. [PubMed] [Google Scholar]
- 10.Coggins T. E., Olswang L. B., Carmichael Olson H., Timler G. R. On becoming socially competent communicators: The challenge for children with Fetal Alcohol Exposure. Internation Review of Research in Mental Retardation. (2003);27:121–150. [Google Scholar]
- 11.Coggins T. E., Timler G. R., Olswang L. B. A state of double jeopardy: Impact of prenatal alcohol exposure and adverse environments on the social communicative abilities of school-age children with Fetal Alcohol Spectrum disorder. Language, Speech, and Hearing Service in Schools. (2007);38:117–127. doi: 10.1044/0161-1461(2007/012). [DOI] [PubMed] [Google Scholar]
- 12.Cole K. N., Dale P. S. Direct language instruction and interactive language instruction with language delayed preschool children: A comparison study. Journal of Speech and Hearing Research. (1986);29:206–217. doi: 10.1044/jshr.2902.206. [DOI] [PubMed] [Google Scholar]
- 13.Dixon G., Joffe B., Bench R. J. The efficacy of visualizing and verbalizing: Are we asking too much? Child Language Teaching and Therapy. (2001);17:127–141. [Google Scholar]
- 14.Duval S. J., Tweedie R. L. Trim and fill: A simple funnel plot based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000);56:276–284. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 15.Egeland G. M., Perhain-Hestet K. A., Gessnet B. D., Ingle D., Berne J. E., Miclcldalgh J. P. Alcohol syndrome in Alaska, 1977 through 1992: An administrative prevalence derived from multiple data sources. American Journal of Public Health. (1998);88:781–786. doi: 10.2105/ajph.88.5.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elliott E., Payne J. M., Morris A., Haan E., Bower C. Fetal alcohol syndrome: A prospective national surveillance study. Archives of Disease in Childhood. (2008);93:732–737. doi: 10.1136/adc.2007.120220. [DOI] [PubMed] [Google Scholar]
- 17.Fey M. E., Cleave P. L., Long S. H., Hughes D. L. Two approaches to the facilitation of grammar in children with language impairment: An experimental evaluation. Journal of Speech and Hearing Research. (1993);36:141–157. doi: 10.1044/jshr.3601.141. [DOI] [PubMed] [Google Scholar]
- 18.Freeman M. F., Tukey J. W. Transformations related to the angular and the square root. Annals of Mathematical Statistics. (1950);21:607–611. [Google Scholar]
- 19.Fudala J. B., England G., Ganoung L. Utilisation of parents in a speech correction programme. Exceptional Children. (1972);30:407–412. doi: 10.1177/001440297203800507. [DOI] [PubMed] [Google Scholar]
- 20.Gibbard D. Parental-based intervention with pre-school language-delayed children (Study 1 and Study 2) European Journal of Disorders of Communication. (1994);29:131–150. doi: 10.3109/13682829409041488. [DOI] [PubMed] [Google Scholar]
- 21.Girolametto L., Pearce P. S., Weitzman E. The effects of focused stimulation for promoting vocabulary in young children with delays: A pilot study. Children’s Communication Development. (1996a);17:39–49. [Google Scholar]
- 22.Girolametto L., Pearce P. S., Weitzman E. Interactive focused stimulation for toddlers with expressive vocabulary delays. Journal of Speech and Hearing Research. (1996b);39:1274–1283. doi: 10.1044/jshr.3906.1274. [DOI] [PubMed] [Google Scholar]
- 23.Glogowska M., Roulstone S., Enderby P., Peters T. J. Randomised controlled trial of community based speech and language therapy in preschool children. British Medical Journal. (2000);321:923–926. doi: 10.1136/bmj.321.7266.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harwood H. Rockville, MD: National Institutes of Health; (2000). Updating estimates of the economic costs of alcohol abuse in the United States: Estimates, Update Methods, and Data. Report prepared by the Lewin Group for the National Institute on Alcohol Abuse and Alcoholism 2000. Based on estimates, analyses, and data reported in Harwood, H., Fountain, D., and Livermore, G. The Economic Costs of Alcohol and Drug Abuse in the United States 1992. Report prepared for the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism. National Institutes of Health, Department of Health and Human Services, NIH Publication No. 98–4327. [Google Scholar]
- 25.Higgins J. P., Thompson S. G. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. (2002);21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 26.Justice L. M. Communication sciences and disorders. A comtemporary perspective. (2nd ed) Boston, MA: Pearson Allyn & Bacon; (2010). [Google Scholar]
- 27.Kvigne V. L., Leonardson G. R., Neff-Smith M., Brock E., Borzelleca J., Welty T. K. Characteristics of children who have full or incomplete fetal alcohol syndrome. Journal of Pediatrics. (2004);145:635–640. doi: 10.1016/j.jpeds.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 28.Lancaster G. The effectiveness of parent administered input training for children with phonological disorders [unpublished MSc thesis] London: City University; (1991). [Google Scholar]
- 29.Law J., Garrett Z., Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder (Review) Cochrane Database of Systematic Reviews. (2003);3:CD004110. doi: 10.1002/14651858.CD004110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Law J., Kot A., Barnett G. A comparison of two methods for providing intervention to three year old children with expressive/receptive language impairment [unpublished project] London: City University; (1999). [Google Scholar]
- 31.Legge C., Roberts G., Butler M. Situational analysis. Fetal alcohol syndrome/fetal alcohol effects and the effects of other substance use during pregnancy. Ottawa, Canada: Health Canada; (2001). [Google Scholar]
- 32.Lupton C., Burd L., Harwood R. Cost of fetal alcohol spectrum disorders. American Journal of Medical Genetics Part C Seminars in Medical Genetics. (2004);127C:42–50. doi: 10.1002/ajmg.c.30015. [DOI] [PubMed] [Google Scholar]
- 33.Mantel N., Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. Journal of National Cancer Institute. (1959);22:719–748. [PubMed] [Google Scholar]
- 34.Mattson S., Riley E. A review of the neurobehavioral deficits in children with fetal alcohol syndrome or prenatal exposure to alcohol. Alcoholism: Clinical and Experimental Research. (1998);22:279–294. doi: 10.1111/j.1530-0277.1998.tb03651.x. [DOI] [PubMed] [Google Scholar]
- 35.Mills R. M. T., McLennan J. D., Caza M. M. Mental health and other service use by young children with fetal alcohol spectrum disorder. Journal of FAS International. (2006);4:e1. [Google Scholar]
- 36.Mulac A., Tomlinson C. N. Generalisation of an operant remediation program for syntax with language delayed children. Journal of Communication Disorders. (1977);10:231–243. doi: 10.1016/0021-9924(77)90003-x. [DOI] [PubMed] [Google Scholar]
- 37.Munro J. A study of speech and language therapy for particular speech sounds in children [unpublished MSc thesis] London: City University; (1999). [Google Scholar]
- 38.Olson H. C., Jirikowic T., Kartin D., Astley S. Responding to the challenge of early intervention for fetal alcohol spectrum disorders. Infants & Young Children. (2007);20:172–189. [Google Scholar]
- 39.Paintner A., Williams A. D., Burd L. Fetal alcohol spectrum disorders—Implications for child neurology, Part 2: Diagnosis and management. Journal of Child Neurology. (2012);27:355–362. doi: 10.1177/0883073811428377. [DOI] [PubMed] [Google Scholar]
- 40.Pensiero S., Manna F., Michieletto P., Perissutti P. Cleft palate and keratoconus in a child affected by fetal alcohol syndrome: An accidental association? Cleft Palate-Craniofacial. (2007);44:95–97. doi: 10.1597/05-083. [DOI] [PubMed] [Google Scholar]
- 41.Popova S., Lange S., Burd L., Rehm J. Health care burden and cost associated with Fetal Alcohol Syndrome in Canada: Based on Official Canadian Data. PLoS One. (2012);7:e43024. doi: 10.1371/journal.pone.0043024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Popova S., Lange S., Burd L., Chudley A. E., Clarren S. K., Rehm J. Cost of Fetal Alcohol Spectrum Disorder diagnosis in Canada. PLoS One. (2013);8:e60434. doi: 10.1371/journal.pone.0060434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Popova S., Lange S., Mihic A., Bekmuradov D., Rehm J. Prevalence of Fetal Alcohol Spectrum Disorder in correctional systems: A systematic literature review. Canadian Journal of Public Health. (2011);102:336–340. doi: 10.1007/BF03404172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Popova S., Stade B., Bekmuradov D., Lange S., Rehm J. Centre for Addiction and Mental Health, Toronto, ON, Canada; (2012). Economic impact of Fetal Alcohol Syndrome and Fetal Alcohol Spectrum Disorders: A systematic literature review. http://knowledgex.camh.net/reports/Documents/economic_impact_fas_litreview12.pdf ; Available in French at: http://knowledgex.camh.net/reports/Documents/economic_impact_fas_litreview12_FR.pdf . [Google Scholar]
- 45.Popova S., Stade B., Bekmuradov D., Lange S., Rehm J. Economic impact of Fetal Alcohol Syndrome and Fetal Alcohol Spectrum Disorders: A systematic literature review. Alcohol and Alcoholism. (2011);46:490–497. doi: 10.1093/alcalc/agr029. [DOI] [PubMed] [Google Scholar]
- 46.Popova S., Stade B., Lange S., Rehm J. A model for estimating the economic impact of Fetal Alcohol Spectrum Disorder. Journal of Population Therapeutics and Clinical Pharmacology. (2012);19:e51–e65. [Google Scholar]
- 47.Popova S., Stade B., Lange S., Mihic A., Rehm J. Methodology for estimating the economic impact of Fetal Alcohol Spectrum Disorder. Centre for Addiction and Mental Health; Toronto, ON, Canada: (2012). http://knowledgex.camh.net/reports/Documents/Popova_etalMethodologySummary_March30_12Final_E.pdfhttp://knowledgex.camh.net/reports/Documents/Popova_etalMethodologySummary_March30_12Final_FR.pdf [Google Scholar]
- 48.Public Health Agency of Canada (PHAC) Fetal alcohol spectrum disorder (FASD): A framework for action. Ottawa, ON: PHAC; (2003). [Google Scholar]
- 49.Public Health Agency of Canada (PHAC) Alcohol use and pregnancy: An important Canadian public health and social issue. Ottawa, ON: PHAC; (2005). [Google Scholar]
- 50.Reid J., Donaldson M. L., Howell J., Dean E. C., Greive R. The effectiveness of therapy for child phonological disorder: The Metaphon approach. In: Aldridge M., editor. Child language. Clevedon, UK: Multilingual Matters; (1996). [Google Scholar]
- 51.Roberts G., Nanson J. Best practices. Fetal alcohol syndrome/fetal alcohol effects and the effects of other substance use during pregnancy. In Canada’s Drug Strategy Division. Ottawa, ON: Health Canada; (2000). [Google Scholar]
- 52.Robertson S. B. The influence of peer models on the play scripts of children with specific language impairment. Journal of Speech, Language, and Hearing Research. (1997);40:49–61. doi: 10.1044/jslhr.4001.49. [DOI] [PubMed] [Google Scholar]
- 53.Robertson S. B., Weismer S. E. Effects of treatment on linguistic and social skills in toddlers with delayed language development. Journal of Speech, Language, and Hearing Research. (1999);42:1234–1248. doi: 10.1044/jslhr.4205.1234. [DOI] [PubMed] [Google Scholar]
- 54.Ruscello D. M., Cartwright L. R., Haines K. B., Shuster L. I. The use of different service delivery models for children with phonological disorders. Journal of Communication Disorders. (1993);26:193–203. doi: 10.1016/0021-9924(93)90008-x. [DOI] [PubMed] [Google Scholar]
- 55.Rvachew S. Speech perception training can facilitate sound production learning. Journal of Speech and Hearing Research. (1994);37:347–357. doi: 10.1044/jshr.3702.347. [DOI] [PubMed] [Google Scholar]
- 56.Rvachew S., Nowak M. The effect of target-selection strategy on phonological learning. Journal of Speech, Language, and Hearing Research. (2001);44:610–623. doi: 10.1044/1092-4388(2001/050). [DOI] [PubMed] [Google Scholar]
- 57.Shaywitz S. E., Caparulo B. K., Hodgson E. S. Developmental language disability as a consequence of prenatal exposure to ethanol. Pediatrics. (1981);68:850–855. [PubMed] [Google Scholar]
- 58.Shelton R. L, Johnson A. F., Ruscello D. M., Arndt W. B. Assessment of parent-administered listening training for preschool children with articulation deficits. Journal of Speech and Hearing Disorders. (1978);18:242–254. doi: 10.1044/jshd.4302.242. [DOI] [PubMed] [Google Scholar]
- 59.Sommers R. K. Factors in the effectiveness of mothers trained to aid in speech correction. Journal of Speech and Hearing Disorders. (1962);27:178–186. doi: 10.1044/jshd.2702.178. [DOI] [PubMed] [Google Scholar]
- 60.Sommers R. K., Furlong A. K., Rhodes F. E., Fichter G. R., Bowser D. C., Copetas F. G., et al. Effects of maternal attitudes upon improvement in articulation when mothers are trained to assist in speech correction. Journal of Speech and Hearing Disorders. (1964);29:126–132. doi: 10.1044/jshd.2902.126. [DOI] [PubMed] [Google Scholar]
- 61.Sommers R. K., Schaeffer M. H., Leiss R. H., Gerber A. J., Bray M. A., Fundrella D., et al. The effectiveness of group and individual therapy. Journal of Speech and Hearing Research. (1966);9:219–225. doi: 10.1044/jshr.0902.219. [DOI] [PubMed] [Google Scholar]
- 62.Spohr H. L., Willms J., Steinhausen H. C. The fetal alcohol syndrome in adolescence. Acta Paediatrics. (1994);404:19–26. doi: 10.1111/j.1651-2227.1994.tb13379.x. [DOI] [PubMed] [Google Scholar]
- 63.Stade B., Ali A., Bennett D., Campbell D., Johnston M., Lens C., et al. The burden of prenatal exposure to alcohol: Revised measurement of cost, 2007. Canadian Journal of Clinical Pharmacology. (2009);16:e91–e102. [PubMed] [Google Scholar]
- 64.Statistics Canada. Participation and Activity limitation survey 2006: Analytical report. Ottawa, ON: Statistics Canada; (2007). [Google Scholar]
- 65.Statistics Canada. Canadian Community Health Survey: Public use microdata file. Ottawa, ON; Statistics Canada; (2011). [Google Scholar]
- 66.Statistics Canada. Ottawa ON: Statistics Canada; (2012). Table 051-0001 - Estimates of population, by age group and sex for July 1, Canada, provinces and territories, annual (persons unless otherwise noted)http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo10a-eng.htm [Google Scholar]
- 67.Statistics Canada. Ottawa, ON: Statistics Canada; (2013). Population by year, by province and territory.http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo02a-eng.htm [Google Scholar]
- 68.Steinhausen H. C., Nestler V., Spohr H. L. Development and psychopathology of children with the fetal alcohol syndrome. Developmental and Behavioral Pediatrics. (1982);3:49–54. [PubMed] [Google Scholar]
- 69.Stratton K., Howe C., Battaglia F. Fetal alcohol syndrome: Diagnosis, epidemiology, prevention, and treatment. Washington, DC: National Academies Press; (1996). [Google Scholar]
- 70.Streissguth A., Barr H., Kogan J., Bookstein F. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE): Final report to the Centers for Disease Control and Prevention on Grant No. R04/ CCR008515. Seattle, WA: University of Washington, Fetal Alcohol and Drug Unit; (1996). [Google Scholar]
- 71.Streissguth A. P., Bookstein F. L., Barr H. M., Sampson P. D., O’Mally D., Young J. K. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. Journal of Development and Behavioral Pediatrics. (2004);25:228–238. doi: 10.1097/00004703-200408000-00002. [DOI] [PubMed] [Google Scholar]
- 72.Tufts L. C., Holliday A. R. Effectiveness of trained parents as speech therapists. Journal of Speech and Hearing Disorders. (1959);24:395–401. doi: 10.1044/jshd.2404.395. [DOI] [PubMed] [Google Scholar]
- 73.Wilcox M. J., Kouri T. A., Caswell S. B. Early language intervention: A comparison of classroom and individual treatment. American Journal of Speech-Language Pathology. (1991);1:49–61. [Google Scholar]
- 74.Wyper K. R., Rasmussen C. R. Language impairments in children with Fetal Alcohol Spectrum Disorder. Journal of Population Therapeutics and Clinical Pharmacology. (2011);18:e364–e376. [PubMed] [Google Scholar]