Abstract
Hurricane Sandy hit New York City (NYC) on October 29, 2012. Before and after the storm, 73 temporary evacuation shelters were established. The total census of these shelters peaked at approximately 6,800 individuals. Concern about the spread of communicable diseases in shelters prompted the NYC Department of Health and Mental Hygiene (DOHMH) to rapidly develop a surveillance system to report communicable diseases and emergency department transports from shelters. We describe the implementation of this system. Establishing effective surveillance in temporary shelters was challenging and required in-person visits by DOHMH staff to ensure reporting. After system establishment, surveillance data were used to identify some potential disease clusters. For the future, we recommend pre-event planning for disease surveillance.
On October 29, 2012, Hurricane Sandy, the largest Atlantic hurricane on record, hit New York City (NYC).1 Damage and destruction left approximately 2 million NYC residents without power and 8.5 million riders without public transit.2,3 Seventy-three city-operated temporary evacuation shelters were opened in anticipation of the storm, 64 of which were in schools. They were designed to house people needing shelter for 3–5 days.4 No complete record exists for the number of people seeking shelter, but peak daily census was approximately 6,800 individuals. After the hurricane, new shelters were opened and others were closed or consolidated. The majority of shelters were open for ≤48 hours. The number of shelters open had been reduced to 15 shelters seven days after the storm (November 5), and to 12 shelters 10 days after the storm. We describe the operation of the shelters and their accompanying medical rooms and outline a surveillance system rapidly set up by the NYC Department of Health and Mental Hygiene (DOHMH) for detecting disease clusters in the shelters, the challenges encountered, and some lessons for the future.
As Hurricane Sandy approached, long-term sheltering was not anticipated, and there was no established preplanned disease surveillance system for temporary evacuation shelters. At the time, DOHMH had only limited experience with disease surveillance in shelters after such a severe weather event. In 2011, DOHMH developed a disease surveillance system in anticipation of shelters set up for Hurricane Irene, but that storm did not cause widespread damage and the shelters were quickly closed. Other jurisdictions had experience with shelters set up for other severe weather events. Shelter surveillance systems were developed following Hurricanes Hugo, Katrina, and Rita; all were established ≥4 days after the storms.5–11 Although one norovirus outbreak was detected following Hurricane Katrina, none of the surveillance systems for these storms documented any serious disease outbreaks.5–12 A survey of health staff members working in shelters following Hurricanes Katrina and Rita showed that staff members lacked recognition of public health risks, and only 59% knew how to contact public health authorities.13
Each of the Hurricane Sandy shelters in NYC had a manager in charge. Individuals were free to come and go, they did not always sign in and out of the shelters, and no computerized list of evacuees existed. No medical screening was conducted at intake. Medical rooms were established in the shelters where evacuees presented for evaluation if they had illness, although the capacity to treat patients was minimal. The medical rooms were staffed by local health-care volunteers and a variety of national and international private aid organizations. As a substantial number of medical volunteers responding to Hurricane Sandy were from outside NYC, they were likely unaware of how to report outbreaks to DOHMH. Shelters had rapid turnover of medical staff, and most medical rooms were without landline telephones. Beginning a week after the hurricane, because shelters were preparing and serving food, sanitarians from DOHMH were stationed at shelters to monitor food safety.
METHODS
DOHMH developed and implemented a disease surveillance system seven days after the storm (on November 5) as a way to identify potential disease outbreaks and emergency department (ED) transports, and implement applicable control measures. By that time, DOHMH had recognized that the shelters would need to remain open longer than the 3–5 days that had been anticipated. A major factor compelling DOHMH to set up the surveillance system was the occurrence of a small cluster of people with gastrointestinal (GI) symptoms identified in one shelter by a DOHMH medical staff volunteer 5–6 days after the storm hit (November 3–4). As a result of that cluster, it became apparent that control of future outbreaks could be difficult because the shelters had only a limited ability to isolate any individuals who became ill.
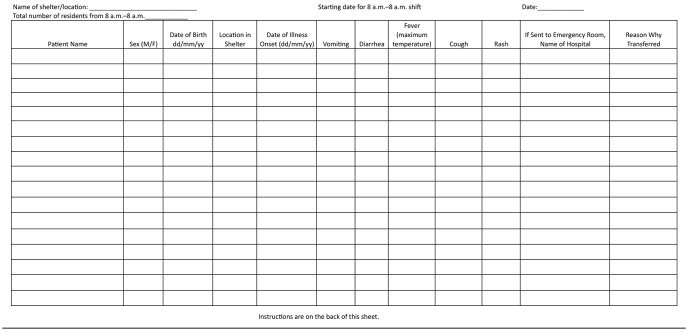
To conduct the surveillance system, beginning seven days after the storm (November 5), DOHMH began daily telephone calls to medical staff members at the 15 shelters that remained open at that time, which housed approximately 5,000 individuals. DOHMH staff members collected information on forms for each shelter, including contact information for medical staff, total shelter census, number of bathrooms, how food was prepared, and numbers of evacuees with GI or febrile respiratory illness. Ten days after the storm (November 8), DOHMH enhanced the surveillance system to include daily visits by DOHMH staff to the 12 shelters that still remained open. DOHMH trained approximately 30 epidemiology staff to visit the shelters and educate medical staff on the surveillance system. DOHMH developed a log sheet to collect basic information on individuals seen with communicable diseases or those transferred to EDs (Figure 1). DOHMH teams delivered log sheets, instructions, a letter explaining the need for the surveillance system, and infection control posters (e.g., covering a cough and hand washing) to shelter medical staff. They instructed medical staff on log sheet completion, and they returned each morning to collect the previous day's data and update contact information for the rapidly changing medical staff members in the shelters. DOHMH staff members reviewed available medical records to ensure that all relevant cases were captured on the log sheets. Shelter clinicians were instructed to call DOHMH immediately if they identified a disease cluster (i.e., ≥3 patients with similar symptoms) or with any concerns regarding patient illness. Medical staff members were supplied with stool collection kits for both viral and bacterial pathogens and instructed to distribute them if ≥3 evacuees had vomiting and diarrhea. When clusters were identified, DOHMH staff interviewed medical providers and patients and reviewed patient charts if available.
Figure 1.
Log sheet provided to each shelter during enhanced disease surveillance following Hurricane Sandy: New York City, November 8–18, 2012
Daily log sheets were entered into a Microsoft® Access® 2010 database and analyzed using SAS® version 9.2.14 Information produced on daily reports included number of shelters reporting, clusters, GI illnesses (i.e., one episode of vomiting or diarrhea), febrile respiratory illnesses (i.e., fever and cough), fever and rash, and total patients sent to an ED. The GI illness definition was highly sensitive because it was unclear how often patients presented to medical areas for symptoms. No baseline rates of illness were available for comparison, as NYC had not implemented similar disease surveillance in evacuation shelters in the past. Twenty-one days after the storm (November 19), the surveillance system was discontinued because all shelters had closed and their remaining residents had been incorporated into NYC Department of Homeless Services' shelters, which operated their own surveillance and reporting systems.
OUTCOMES
During the GI disease outbreak reported 5–6 days after the storm (November 3–4), 11 of the 167 shelter residents (7%) were identified as having vomiting or diarrhea (Figure 2). An attempt was made to isolate ill evacuees. A DOHMH team visited the shelter on November 5, six days after the storm, to identify additional cases; assist with implementing control measures; inspect kitchen and food handling practices; and provide infection control posters, hand sanitizer, and stool collection kits. Stool samples were requested but no specimens were collected. Food handling practices were examined and no deficiencies were identified. Symptoms were consistent with norovirus infection and were thought to have spread from person to person. Because residents were housed in an open gymnasium with limited means of isolation, and the school was planning to reopen following closure due to the hurricane, all evacuees were moved to another shelter with individual apartments the following day, and the school shelter was closed. No additional cases were reported.
Figure 2.
Characteristics of patients with gastrointestinal illness at Hurricane Sandy Evacuation Shelter A: November 5, 2012, New York City
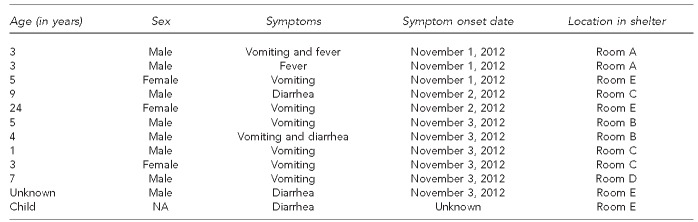
NA = not available
The initial telephone surveillance system, implemented seven days after the storm (November 5), was deemed unsuccessful because DOHMH staff members were only able to speak with someone by telephone at eight of the 15 shelters (53%). It was difficult to identify and contact medical staff, in part because turnover of medical staff was frequent. On days 8 and 9 after the storm (November 6–7), we were able to contact at least one medical provider, DOHMH sanitarian, or shelter manager at all of the shelters, but data received by telephone were still incomplete. Sanitarians and managers received little information from medical room staff. Fax machines normally used to verify DOHMH authority to collect confidential medical information were unavailable, and medical staff members were reluctant to share information by telephone. As shelters had no uniform system for recording patients seen in the medical rooms and occasionally no system at all, only general information on illness of evacuees was available rather than specific case numbers.
When DOHMH enhanced the surveillance system on day 10 after the storm (November 8) by sending DOHMH staff to the shelters, data completeness and reliability improved. Patients' names were recorded on daily log sheets, and DOHMH staff reviewed available medical records to search for additional cases of disease. Once on-site, DOHMH staff members discovered that some shelters had two medical areas, one for the general population and one for patients with special medical needs. In addition, they discovered that private aid organization staff members often were collecting data separately for surveillance systems set up by their own organizations. DOHMH staff encouraged shelter medical staff to report to the DOHMH system.
From day 10 through day 20 after the storm (November 8–18), when DOHMH operated an enhanced surveillance system incorporating in-person visits to the shelters, DOHMH documented 43 cases of GI illness, one case of febrile respiratory illness, and 25 ED transfers, including two injuries (Table). No cases of fever and rash were reported. Four cases of illness were reported among shelter volunteers. During this period, three potential disease clusters were investigated, including GI illness, rash, and conjunctivitis. On day 11 after the storm (November 9), staff members at Shelter J reported people with GI illness overnight among a population of nursing home patients housed in a gymnasium. On investigation, on-site DOHMH staff learned only one patient had vomiting and none had diarrhea. On day 16 after the storm (November 14), staff members at Shelter E reported scabies among three family members, but DOHMH staff members visited the site and did not confirm the scabies diagnosis. On day 16 after the storm, staff members at Shelter C reported conjunctivitis in three people. The patients were examined and treated, and DOHMH recommended frequent hand washing, frequent environmental cleaning in the common areas, and confinement of ill evacuees to their rooms as much as possible.
Table.
Symptoms of individuals transferred to EDs from evacuation shelters during the enhanced shelter surveillance system following Hurricane Sandy: New York City, November 8–18, 2012
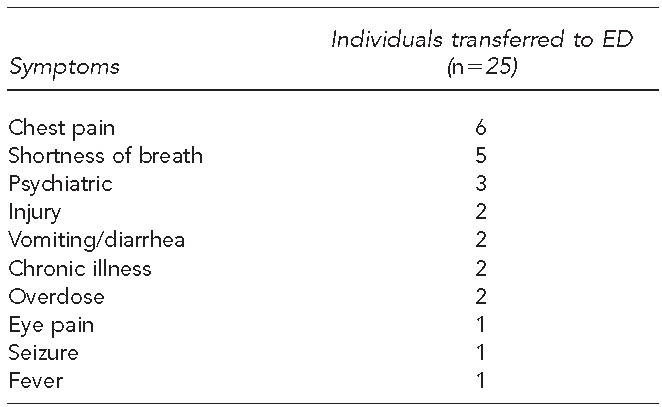
ED = emergency department
LESSONS LEARNED
Although the risk of infectious disease outbreaks after disasters is low, especially in the immediate phase,15,16 public health surveillance among individuals displaced by disasters is useful. In general, plans for surveillance should be developed pre-event.17 When Hurricane Sandy hit, NYC had not experienced a natural disaster of such magnitude in recent memory and did not expect shelters to remain open past the initial days following the storm. The occurrence of a cluster of GI illnesses, plus the realization that the shelters would have to remain open longer than anticipated, prompted DOHMH to implement disease surveillance. This system was designed to be simple and flexible.
We encountered many challenges during system implementation. Although we attempted to include all shelters in the system, identifying which shelters remained open and determining how to contact correct staff at each shelter was difficult. The contact person at the shelters changed daily and telephones were not always available to reach shelter staff. We did not have access to a central list of functioning shelters because shelters were constantly consolidating and closing. As the daily shelter census was unreliable, illness rates could not be calculated. Competing surveillance systems operated by private aid organization staff hindered our ability to collect information at some shelters. Without standardized patient encounter information, verification of cases and investigations was challenging. The busy, sometimes chaotic nature of shelter environments meant that shelter managers did not always receive information from the medical rooms or hear about rumors of illnesses. Many shelters were established in schools with evacuees housed mainly in large gymnasiums at the same time classrooms were being prepared for students to return to school. These shelters were not able to comply with all DOHMH's infection control recommendations, especially isolation. All these problems should be considered when making recommendations to disaster shelter managers and selecting sites.
Despite its limitations, the shelter surveillance system was valuable to NYC public health authorities because data from the system were used to confirm outbreaks, dispel rumors, and help gauge the success of implemented control measures. Having DOHMH visit shelters was valuable for understanding the layout of the shelters, collecting logs, investigating reported clusters, and working with shelter managers to implement control measures. Also, by its mere existence, the surveillance system increased awareness among medical staff members about the importance of reporting communicable disease clusters to DOHMH. No serious infectious disease outbreaks were identified and the surveillance data were reassuring to NYC officials during the crisis. The completeness and accuracy of the system might have been improved if it had been possible for DOHMH staff to be stationed in shelter medical areas full-time to record each patient in the log at the time of presentation.
RECOMMENDATIONS
These results and lessons learned can be useful for planning future responses to natural disasters or other public health emergencies. Effective communication and information sharing among agencies running shelters and collecting data are essential. Tools to document patient encounters and collect data for shelter surveillance, along with plans for decisions regarding what data to collect and collection logistics, should be developed pre-event so that they can be implemented quickly when needed. The system should include information beyond communicable diseases to injuries, medication needs, mental health issues, and other diseases and conditions upon which health departments can act. Pre-event exercises should include training shelter medical staff and managers on disease surveillance and communicating the health department's authority to collect this information. To receive the most reliable, accurate data, in-person visits by health department staff or assignment of full-time surveillance liaisons at each shelter will likely be required, especially initially. Staff members should be provided with basic infection control guidelines at shelter setup to prevent disease outbreaks and be educated to report disease clusters to the health department.
Footnotes
The authors thank Christopher Paquet at the New York City Department of Health and Mental Hygiene for information on New York City shelter numbers and populations. This study did not require Institutional Review Board determination. This work underwent human subjects review at the U.S. Centers for Disease Control and Prevention (CDC) and was determined to be public health practice, not research.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
REFERENCES
- 1.National Oceanic and Atmospheric Administration (US) NOAA's National Weather Service Newport/Morehead City, NC: events summaries/case studies: October 29, 2012—Hurricane Sandy [cited 2013 Sep 16] Available from: URL: http://www.erh.noaa.gov/mhx/EventReviews/20121029/20121029.php.
- 2.National Oceanic and Atmospheric Administration (US) NOAA water level and meteorological data report. Silver Spring (MD): Department of Commerce (US); 2013. Also available from: URL: http://tidesandcurrents.noaa.gov/publications/Hurricane_Sandy_2012_Water_Level_and_Meteorological_Data_Report.pdf [cited 2013 Sep 16] [Google Scholar]
- 3.City of New York. A stronger, more resilient New York: special initiative for rebuilding and resiliency. 2013. [cited 2013 Oct 4]. Available from: URL: http://www.nyc.gov/html/sirr/html/report/report.shtml.
- 4.Gibbs LI, Holloway CF. Hurricane Sandy after action: report and recommendations to Mayor Michael R. Bloomberg. May 2013 [cited 2013 Oct 4] Available from: URL: http://www.nyc.gov/html/recovery/downloads/pdf/sandy_aar_5.2.13.pdf.
- 5.Murray KO, Kilborn C, desVignes-Kendrick M, Koers E, Page V, Selwyn BJ, et al. Emerging disease syndromic surveillance for Hurricane Katrina evacuees seeking shelter in Houston's Astrodome and Reliant Park complex. Public Health Rep. 2009;124:364–71. doi: 10.1177/003335490912400304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Illness surveillance and rapid needs assessment among Hurricane Katrina evacuees—Colorado, September 1–23, 2005. MMWR Morb Mortal Wkly Rep. 2006;55(9):244–7. [PubMed] [Google Scholar]
- 7.Surveillance for illness and injury after Hurricane Katrina—three counties, Mississippi, September 5–October 11, 2005. MMWR Morb Mortal Wkly Rep. 2006;55(9):231–4. [PubMed] [Google Scholar]
- 8.Surveillance for illness and injury after Hurricane Katrina—New Orleans, Louisiana, September 8–25, 2005. MMWR Morb Mortal Wkly Rep. 2005;54(40):1018–21. [PubMed] [Google Scholar]
- 9.Surveillance of shelters after Hurricane Hugo—Puerto Rico. MMWR Morb Mortal Wkly Rep. 1990;39(3):41–2. 47. [PubMed] [Google Scholar]
- 10.Infectious disease and dermatologic conditions in evacuees and rescue workers after Hurricane Katrina—multiple states, August–September, 2005. MMWR Morb Mortal Wkly Rep. 2005;54(38):961–4. [PubMed] [Google Scholar]
- 11.Norovirus outbreak among evacuees from Hurricane Katrina—Houston, Texas, September 2005. MMWR Morb Mortal Wkly Rep. 2005;54(40):1016–8. [PubMed] [Google Scholar]
- 12.Yee EL, Palacio H, Atmar RL, Shah U, Kilborn C, Faul M, et al. Widespread outbreak of norovirus gastroenteritis among evacuees of Hurricane Katrina residing in a large “megashelter” in Houston, Texas: lessons learned for prevention. Clin Infect Dis. 2007;44:1032–9. doi: 10.1086/512195. [DOI] [PubMed] [Google Scholar]
- 13.Brahmbhatt D, Chan JL, Hsu EB, Mowafi H, Kirsch TD, Quereshi A, et al. Public health preparedness of post-Katrina and Rita shelter health staff. Prehosp Disaster Med. 2009;24:500–5. doi: 10.1017/s1049023x00007408. [DOI] [PubMed] [Google Scholar]
- 14.SAS Institute, Inc. Cary (NC): SAS Institute, Inc.; 2010. SAS®: Version 9.2. [Google Scholar]
- 15.Ivers LC, Ryan ET. Infectious diseases of severe weather-related and flood-related natural disasters. Curr Opin Infect Dis. 2006;19:408–14. doi: 10.1097/01.qco.0000244044.85393.9e. [DOI] [PubMed] [Google Scholar]
- 16.Kouadio IK, Aljunid S, Kamigaki T, Hammad K, Oshitani H. Infectious diseases following natural disasters: prevention and control measures. Expert Rev Anti Infect Ther. 2012;10:95–104. doi: 10.1586/eri.11.155. [DOI] [PubMed] [Google Scholar]
- 17.Waring SC, Brown BJ. The threat of communicable diseases following natural disasters: a public health response. Disaster Manag Response. 2005;3:41–7. doi: 10.1016/j.dmr.2005.02.003. [DOI] [PubMed] [Google Scholar]