Abstract
Objective
To investigate clinical factors affecting the timing of delivery in twin pregnancies in order to minimize perinatal complications.
Methods
A retrospective study involved 163 twin pregnancies delivered from January 2006 to September 2011 at Gachon University Gil Medical Center. These cases were divided into three groups based on the delivery timing: less than 32 weeks' gestation (group A), between 32 and 35+6 weeks' gestation (group B), and over 36 weeks' gestation (group C). Clinical factors including maternal age, parity, presence of premature uterine contraction, presence of premature rupture of membrane, white blood cell, high sensitive C-reactive protein level, cervical dilatation, maternal complication, chorionicity, twin specific complication, and perinatal complication were analyzed for each group.
Results
In group B, the timing of delivery was postponed for 14 days or more from the time of admission, and there were fewer numbers of babies with low Apgar score at birth compared with other groups. The frequency of uterine contraction (P<0.001), presence of premature rupture of membranes (P=0.017), dilatation of cervix (P<0.001), increased white blood cell and high sensitive C-reactive protein levels (P=0.002, P<0.001) were important clinical factors during decision making process of delivery timing in twin pregnancies. Twin specific fetal conditions, such as twin-twin transfusion syndrome and discordant growth (over 25% or more) were shown more frequently in group A. However, there were no significant statistical differences among three groups (P=0.06, P=0.14).
Conclusion
Proper management for preventing premature contraction and inflammation can be essential in twin pregnancies until 32 weeks' gestation, and may decrease maternal and perinatal complications.
Keywords: Maternal complications, Perinatal complications, Timing of delivery, Twins
Introduction
The incidence of twin pregnancies has shown a significant increase over the last several decades due to advanced maternal age and the development of assisted reproduction techniques [1]. Although twins occur in approximately 1 of 80 pregnancies, corresponding to 2.6% of all newborns, they account for 12.2% of preterm births and 15.4% of neonatal deaths (NNDs) [2,3].
The major causes of perinatal complications in twin pregnancies are related to preterm delivery, fetal growth restriction, and low birth weight [4]. Preterm delivery is observed in approximately 54% of all twin pregnancies. Half of these twin births are resulted from iatrogenic origin, which may cause maternal or fetal complications. Other half consists of the cases of spontaneous premature labor or premature membrane rupture [3]. The risk of growth restriction is three times higher in twin pregnancies than those in singleton pregnancies [5]. Because of these risks, it is difficult to decide the timing of delivery for twins. Some of previous reports have recommended to offer the elective preterm birth for the apparently uncomplicated twins at 34 to 35 weeks' gestation following administration of antenatal corticosteroid [5,6]. However, another report showed that, in regard to the risk of intrauterine fetal death (IUFD), there is no indication of preterm elective delivery in twins [7]. Unfortunately, reliable guideline of optimal gestational age for twin delivery has not been established, and also there is no international agreement for delivery timing [8]. Therefore, we investigate the clinical factors that affect timing of delivery in twin pregnancies to reduce the perinatal complications.
Materials and methods
A retrospective review of 163 twin pregnancies, and 319 babies delivered at our institution between January 2006 and September 2011 was conducted. Seven babies were excluded due to co-twin deaths. Maternal and perinatal data was obtained from medical records to evaluate the relation between the timing of deliveries of twins and complication occurred. We divided total cases into three groups according to the period of delivery timing: less than 32 weeks' gestation (group A), between 32 and 35+6 weeks' gestation (group B), and over 36 weeks' gestation (group C). The maternal age, parity, presence of premature uterine contraction, presence of premature rupture of membrane (PROM), white blood cell (WBC) and high sensitive C-reactive protein (hsCRP) levels, cervical length and cervical dilatation, maternal complications (pregnancy hypertension, gestational diabetes), and chorionicity were analyzed among these three groups. The birth weight, Apgar score at 5 minutes after birth, neonatal intensive care unit admission rate, presence of jaundice, respiratory distress syndrome, congenital heart disease, and perinatal death were reviewed based on the gestational age at birth. Expected twin specific complications were twin-twin transfusion syndrome (TTTS), severe discordant growth, NND, co-twin death, and still birth. The diagnosis of TTTS was made by the standard prenatal ultrasound criteria [9]. Birth weight discordancy was calculated according to the following formula: (weight of larger twin-weight of smaller twin)×100/weight of larger twin. With ≥25% rate of birth weight discordancy, excluding the cases of IUFD, we defined them as the severe discordant growth. The optimal timing for twin deliveries was investigated to minimize the maternal and perinatal adverse influences.
Tocolytics were used to prolong the pregnancy so that the perinatal morbidity and mortality can be decreased. Two types of tocolytics including ritodrine and atosiban were used in this study for arresting of preterm labor before 34 weeks of gestation. Postnatally, chorionicity was established by the examination of placental membrane after birth. After macroscopic examinations, microscopic sections of membranes were analyzed for determination of chorionic and amniotic types, which can be classified as dichorionic diamniotic placenta (DCDA), monochorionic diamniotic placenta (MCDA), and monochorionic monoamniotic placenta (MCMA).
The collected data were analyzed using the statistical program IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). Statistical significances were tested by one way ANOVA among groups (Table 1). Maternal complication, twin specific complication, perinatal complication were analyzed with chi-squared test or Fisher's exact test among groups. A value of P<0.05 was considered significant.
Table 1.
Baseline characteristics of twin pregnancy
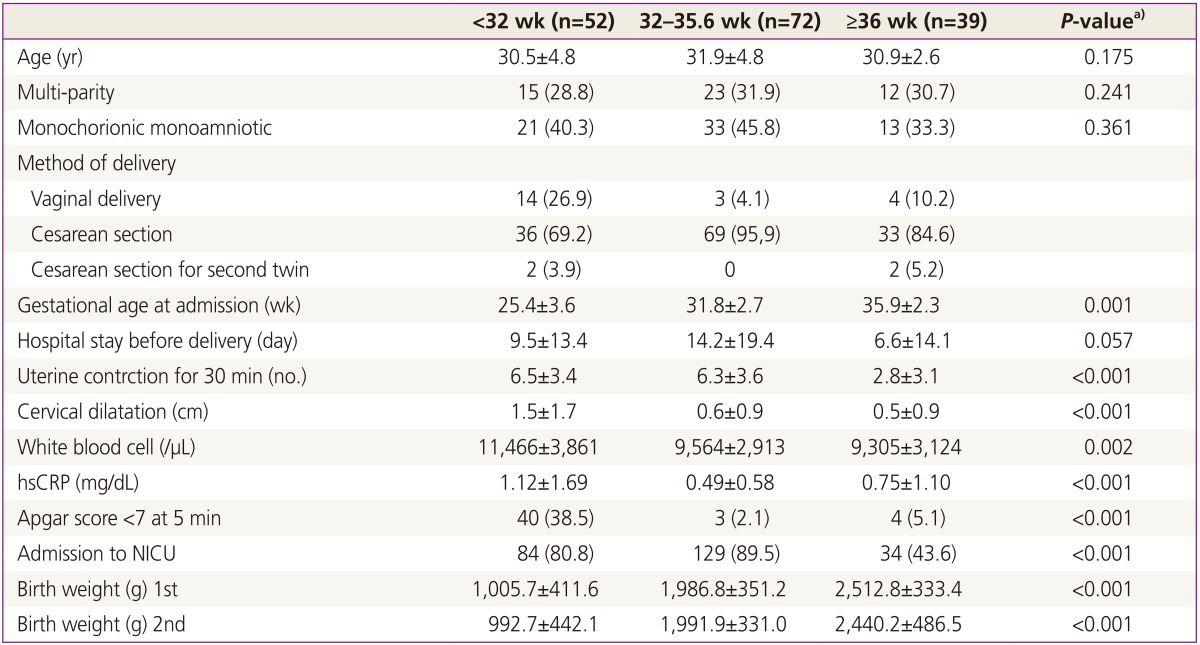
Values are presented as mean±standard deviation or number (%).
hsCRP, high sensitive C-reactive protein; NICU, neonatal intensive care unit.
a)Statistical significance were tested by one way analysis of variances among group; b)Interval means the duration of keeping pregnancy from admission to delivery.
Results
Among 163 twin deliveries, 31.9% (52/163) were in group A, 44.2% (72/163) in group B, and 23.9% (39/163) in group C. Baseline characteristics of theses pregnancies are shown in Table 1. The mean maternal age was 30.5 years. DCDA, MCDA and MCMA twin pregnancies were 94 (57.6%), 67 (41.1%), and 2 (1.3%), respectively.
The mean gestational age of admission was 30.8 weeks; 25.4 weeks in group A, 31.8 weeks in group B, and 35.9 weeks in group C. The intervals between admission and delivery represented 9.5 days in group A, 14.2 days in group B, and 6.7 days in group C, respectively (P=0.057).
The uterine contractions occurred more frequently in group A (6.5 times/30 min) and B (6.3 times/30 min) compared with in group C (2.8 times/30 min) (P<0.001). The cervical dilatation at admission in group A was statistically significant compared with the other two groups (P<0.001). WBC and hsCRP level before delivery were also higher in group A than in the other two groups (P<0.05).
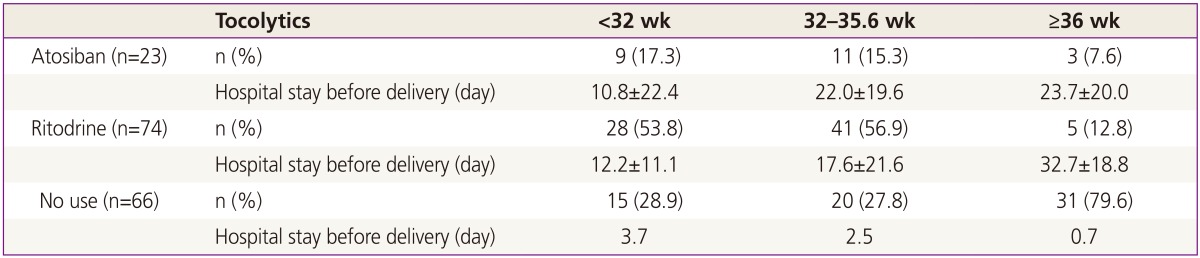
Ritodrine and atosiban were used in 74 (45.4%) and 23 (14.1%) cases, respectively. For the use of atosiban, 20 cases were primary use, but the other 3 cases were used secondary due to adverse events occurred after administration of ritodrine. Sixty-six cases (66/163, 40.5%) did not apply tocolytics because of the rapid progression of labor before use of tocolytics. There was no difference in the extension of pregnancy between two groups of ritodrine used and atosiban used. Regardless of the use of tocolytics, the extension of pregnancy was more effective in group B than in group A (Table 2).
Table 2.
Effectiveness of tocolytics in twin pregnancy
PROMs (P=0.017) and incompetent internal os of cervix (IIOC, P<0.001) were represented as major clinical factors affecting for timing of delivery in twins before 36 weeks of gestation. And all IIOC had occurred before 32 weeks of gestation. However, pregnancy induced hypertension and gestational diabetes did not affect the timing of delivery in twins in this study (Table 3).
Table 3.
Maternal complications in twin pregnancy
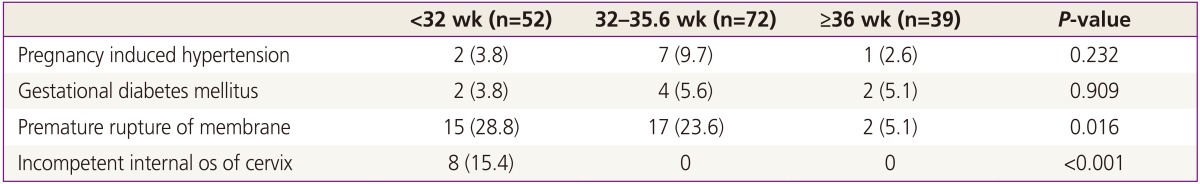
Values are presented as number (%).
There were 13 cases of TTTS (13/67, 19.4%); 9 cases in group A and 4 cases in group B. All of them were delivered before 36 weeks of gestation. Severe growth-discordant neonates, defined as more than 25% of intertwine birth weight differences, were found in 36 cases (36/163, 22.1%). All cases were delivered before 36 weeks of gestation. Co-twin deaths in group B (2 cases) and group C (3 cases) were all in dichorionic twins and continuing pregnancy from early gestation. There was one NND in group B which was diagnosed with tetralogy of fallot and none in group C. In group A, 15 cases of NNDs were occurred. Seven of them were presented with various complications related to prematurity. Other 7 neonates were associated with TTTS, and 1 neonate died of congenital anomaly (Table 4).
Table 4.
The incidence of twin specific complications based on gestational age at birth
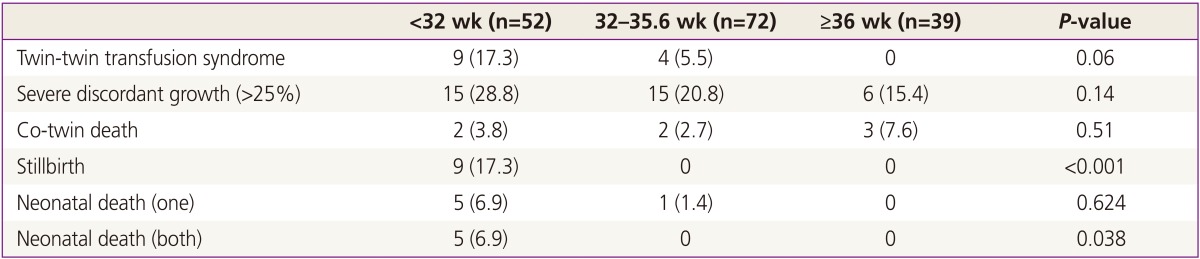
Values are presented as number (%).
The most common neonatal complication in group A was neonatal respiratory distress syndrome. But after 32 weeks of gestation, jaundice was often occurred in neonates on admission. There were 7 congenital heart diseases, such as atrial septal defect, ventricular septal defect, and coarctation of aorta in group B, and 2 of them in group C (Table 5).
Table 5.
Perinatal complications in twin pregnancy
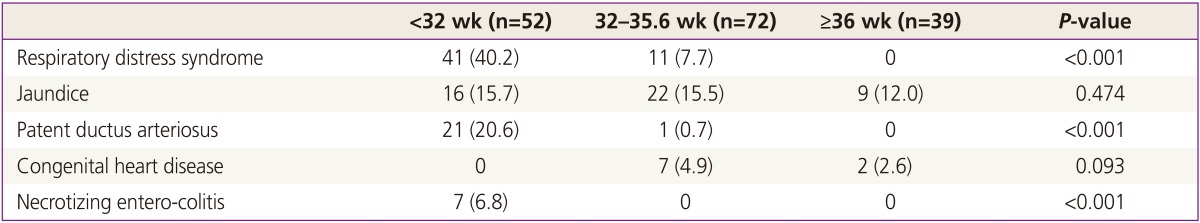
Values are presented as number (%).
Discussion
Twins are at higher risk for adverse perinatal outcomes compared to singleton gestation, predominantly due to increased risks for preterm delivery [10]. The incidence of preterm delivery and prematurity towards neonatal morbidity in twin pregnancies is significantly reduced as a result of improved neonatal care facilities [11]. Therefore, the ideal time for delivery of a pregnancy would be when the risk for perinatal morbidity and mortality is lowest, but before the risk for stillbirth begins to significantly rise.
We reviewed 163 cases of twin pregnancies delivered at a single tertiary center for 6 years. Mean duration of pregnancy for twin gestations was 29.5 weeks, and deliveries at less than 36 weeks were 124/163 (76.1%). In addition, low birth weight (<2,500 g) infants were 274/326 (84.0%), and very low birth weight (<1,500 g) infants were 99/326 (30.4%). The US National Vital Statistics reviewed 138,660 cases of twins delivered in 2008 and revealed that 58.9% were delivered as preterm (<37 weeks' gestation), 11.6% were as very preterm (<32 weeks' gestation). Also, 57% were of low birth weight (<2,500 g), and 10.1% very low birth weight (<1,500 g) [12]. Compare to the result of US National Vital Statistics, our study group showed higher rate of preterm and low birth weight deliveries.
In this study, clinical factors influencing the timing of delivery in twins were the frequency of uterine contraction, dilatation of cervix, WBC count, and hsCRP level. Also, we found out that PROM (P=0.017) and IIOC (P<0.001) among maternal complications were closely related to timing of delivery. Most importantly, the frequency of uterine contraction and dilatation of cervix are related with preterm labor. These factors should be considered treating twin pregnancies, specially at an admission and delivery. Monochorionic twins have an approximately 15% of increased risk of TTTS, which can induce perinatal mortality and morbidity in spite of the proper treatment [13]. The rate of TTTS was 13/67 (19.4%), which was higher than the incidence of 8% to 9%, reported previously [9]. We found the cases of TTTS in the group of babies born at less than 36 weeks' gestation. In Assuncao et al. [14], the proportion of twins delivered before 32 weeks was 2.5 fold higher in monochorionic than in dichorionic and was statistically significant. Gestational age is lower in the presence of complications such as fetal malformations or TTTS. And the prematurity increases perinatal mortality [14]. In Table 4, the incidence of twin-specific complications were high in the group of delivered at less than 32 weeks' gestation, but both still birth and NND were statistically significant (P<0.05).
The most common perinatal complication was neonatal respiratory distress syndrome which is highly presented in group A (P<0.05). Cleary-Goldman and D'Alton [8] suggested that after 32 weeks' gestation, the prospective risk for fetal death in these pregnancies might be eliminated by elective preterm delivery. Therefore, the optimal delivery time of twin pregnancies is at least after 32 weeks' gestation. To prolong the pregnancy, antibiotics are necessary for preventing infection, steroid therapy may require for lung maturation, and regular follow-up of ultrasonography is essential.
In group B, we observed that using tocolytics is the important management to delay the delivery for decreasing of perinatal complications. The tocolytics used group, compared to the not used group, showed the prolongation of pregnancy more than two weeks. A 1999 meta-analysis of the largest randomized controlled trials investigating the use of tocolytics for the arrest of active preterm labor concluded that tocolytics reduced the risk of delivery within 7 days but was not associated with improved perinatal outcomes [15,16]. Atosiban, an oxytocin derivative and competitive antagonist, has been used in the treatment of preterm labor. Atosiban has been shown to completely inhibit the uterotonic action of oxytocin in a competitive and dose-dependent form, as well as to down-regulate oxytocin receptors [17]. We used atosiban as the first line treatment agent among tocolytics treating twin pregnancies (20/163). More recently, a randomized study performed in Korea demonstrated that atosiban was superior to ritodrine in both safety and efficacy [18]. Effectiveness of tocolytic agents in twin pregnancies is still controversial. However, our study carefully suggests that tocolytic agents can improve the perinatal outcomes by postponing preterm labor before 32 weeks' gestation at admission, and extend the gestation.
The twin specific complications observed in group C were severe discordant growth (15.4%) and co-twin death (7.6%). However, there was no IUFD case in this group. Perinatal mortality of singletons is increased significantly after 42 weeks whereas perinatal mortality in twins starts to increase significantly after 37 weeks [19]. Prospective risk of fetal death in twin pregnancies, however, rises with advancing gestation, and it ranges between 0.2% and 0.4% per gestational week between 32 and 38 weeks' gestation [20]. Robinson et al. [21] suggested that for women with uncomplicated monochorionic twins, the preferred timing of delivery is between 36 and 38 weeks' gestation to decrease fetal loss.
In conclusion, we found out that the clinical factors affecting the timing of delivery in twins are the frequency of uterine contraction, dilatation of cervix, WBC, and hsCRP. Other distributing factors for timing of delivery are PROM and IIOC among maternal complications. The statistical results showed that the role of these clinical factors was more significant in the group with early gestational age. An appropriate use of tocolytics could help improving perinatal outcomes in a variety of maternal and fetal complications in twin pregnancies. Therefore, physicians should regard these factors during examinations and effectively use tocolytic agents to prolong the pregnancy up to at least 32 weeks of gestation and attempt to reduce perinatal complications.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Russell RB, Petrini JR, Damus K, Mattison DR, Schwarz RH. The changing epidemiology of multiple births in the United States. Obstet Gynecol. 2003;101:129–135. doi: 10.1016/s0029-7844(02)02316-5. [DOI] [PubMed] [Google Scholar]
- 2.Ghai V, Vidyasagar D. Morbidity and mortality factors in twins: an epidemiologic approach. Clin Perinatol. 1988;15:123–140. [PubMed] [Google Scholar]
- 3.Gardner MO, Goldenberg RL, Cliver SP, Tucker JM, Nelson KG, Copper RL. The origin and outcome of preterm twin pregnancies. Obstet Gynecol. 1995;85:553–557. doi: 10.1016/0029-7844(94)00455-M. [DOI] [PubMed] [Google Scholar]
- 4.Glinianaia SV, Rankin J, Renwick M Northern Region Perinatal Mortality Survey Steering Group. Time trends in twin perinatal mortality in northern England, 1982-94. Twin Res. 1998;1:189–195. doi: 10.1375/136905298320566159. [DOI] [PubMed] [Google Scholar]
- 5.Alexander GR, Salihu HM. Perinatal outcomes of singleton and multiple births in the United States, 1995-98. In: Blickstein I, Keith LG, editors. Multiple pregnancy: epidemiology, gestation and perinatal outcome. 2nd ed. Andover: Thompson Publishing Services; 2005. pp. 3–10. [Google Scholar]
- 6.Blickstein I, Keith LG. Multiple pregnancy: epidemiology, gestation and perinatal outcome. 2nd ed. New York: Taylor & Francis; 2005. [Google Scholar]
- 7.Simoes T, Amaral N, Lerman R, Ribeiro F, Dias E, Blickstein I. Prospective risk of intrauterine death of monochorionic-diamniotic twins. Am J Obstet Gynecol. 2006;195:134–139. doi: 10.1016/j.ajog.2006.01.099. [DOI] [PubMed] [Google Scholar]
- 8.Cleary-Goldman J, D'Alton ME. Uncomplicated monochorionic diamniotic twins and the timing of delivery. PLoS Med. 2005;2:e180. doi: 10.1371/journal.pmed.0020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acosta-Rojas R, Becker J, Munoz-Abellana B, Ruiz C, Carreras E, Gratacos E, et al. Twin chorionicity and the risk of adverse perinatal outcome. Int J Gynaecol Obstet. 2007;96:98–102. doi: 10.1016/j.ijgo.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Bajoria R, Kingdom J. The case for routine determination of chorionicity and zygosity in multiple pregnancy. Prenat Diagn. 1997;17:1207–1225. [PubMed] [Google Scholar]
- 11.Kalyoncu O, Aygun C, Cetinoglu E, Kucukoduk S. Neonatal morbidity and mortality of late-preterm babies. J Matern Fetal Neonatal Med. 2010;23:607–612. doi: 10.1080/14767050903229622. [DOI] [PubMed] [Google Scholar]
- 12.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Osterman MJ, et al. Births: final data for 2008 [Internet] Hyattsville: National Center for Health Statistics; 2010. [cited 2014 Sep 22]. Available from: http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_01.pdf. [PubMed] [Google Scholar]
- 13.Fisk NM, Galea P. Twin-twin transfusion: as good as it gets? N Engl J Med. 2004;351:182–184. doi: 10.1056/NEJMe048047. [DOI] [PubMed] [Google Scholar]
- 14.Assuncao RA, Liao AW, Brizot Mde L, Krebs VL, Zugaib M. Perinatal outcome of twin pregnancies delivered in a teaching hospital. Rev Assoc Med Bras. 2010;56:447–451. doi: 10.1590/s0104-42302010000400018. [DOI] [PubMed] [Google Scholar]
- 15.Gyetvai K, Hannah ME, Hodnett ED, Ohlsson A. Tocolytics for preterm labor: a systematic review. Obstet Gynecol. 1999;94(5 Pt 2):869–877. doi: 10.1016/s0029-7844(99)00329-4. [DOI] [PubMed] [Google Scholar]
- 16.Brubaker SG, Gyamfi C. Prediction and prevention of spontaneous preterm birth in twin gestations. Semin Perinatol. 2012;36:190–194. doi: 10.1053/j.semperi.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 17.Engstrøm T, Bratholm P, Vilhardt H, Christensen NJ. Effect of oxytocin receptor and beta2-adrenoceptor blockade on myometrial oxytocin receptors in parturient rats. Biol Reprod. 1999;60:322–329. doi: 10.1095/biolreprod60.2.322. [DOI] [PubMed] [Google Scholar]
- 18.Shim JY, Park YW, Yoon BH, Cho YK, Yang JH, Lee Y, et al. Multicentre, parallel group, randomised, single-blind study of the safety and efficacy of atosiban versus ritodrine in the treatment of acute preterm labour in Korean women. BJOG. 2006;113:1228–1234. doi: 10.1111/j.1471-0528.2006.01053.x. [DOI] [PubMed] [Google Scholar]
- 19.Dias T, Akolekar R. Timing of birth in multiple pregnancy. Best Pract Res Clin Obstet Gynaecol. 2014;28:319–326. doi: 10.1016/j.bpobgyn.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Kingdom JC, Nevo O, Murphy KE. Discordant growth in twins. Prenat Diagn. 2005;25:759–765. doi: 10.1002/pd.1262. [DOI] [PubMed] [Google Scholar]
- 21.Robinson BK, Miller RS, D'Alton ME, Grobman WA. Effectiveness of timing strategies for delivery of monochorionic diamniotic twins. Am J Obstet Gynecol. 2012;207:53.e1–53.e7. doi: 10.1016/j.ajog.2012.04.007. [DOI] [PubMed] [Google Scholar]


