Abstract
In 2001 the Environmental Protection Agency (EPA) adopted a new standard for arsenic (As) in drinking water of 10 μg/L, replacing the old standard of 50 μg/L. However, for the 12% of the U.S. population relying on unregulated domestic well water, including half of the population of Maine, it is solely the well owner’s responsibility to test and treat the water. A mailed household survey was implemented January 2013 in 13 towns of central Maine with the goal of understanding the population’s testing and treatment practices and the key behavior influencing factors in an area with high well-water dependency and frequent natural groundwater As. The response rate was 58.3%; 525 of 900 likely-delivered surveys to randomly selected addresses were completed. Although 78% of the households reported their well has been tested, for half it was more than 5 years ago. Among the 58.7% who believe they have tested for As, most do not remember results. Better educated, higher income homeowners who more recently purchased their homes are most likely to have included As when last testing. While households agree water and As-related health risks can be severe, they feel low personal vulnerability and there are low testing norms overall. Significant predictors of including As when last testing include: having knowledge that years of exposure increases As-related health risks (risk knowledge), knowing who to contact to test well water (action knowledge), believing regularly testing does not take too much time (instrumental attitude), and having neighbors who regularly test their water (descriptive norm). Homeowners in As-affected communities have the tendency to underestimate their As risks compared to their neighbors. The reasons for this optimistic bias require further study, but low testing behaviors in this area may be due to the influence of a combination of norm, ability, and attitude factors and barriers.
Keywords: well testing, As, health behavior, drinking water, private well, Maine
1. Introduction
Naturally occurring arsenic (As) in groundwater is a global public health concern. Elevated As concentrations (> 10 μg/L or EPA MCL) in well water affect an estimated 140 million people in 70 countries (Ravenscroft et al., 2009) with increased risks of cancer, cardiovascular disease, and neuropathy (Smith et al., 2000). In the United States where 12% of the population and in areas like New England up to 40% of the population rely on domestic well water for drinking (Kumar et al., 2010), exposure to As is a serious risk. In a recent Columbia University Superfund Research Program (SRP) study of schoolchildren in towns around Augusta, Maine, children consuming water >5 μg/L As showed significant reductions in full scale IQ and Index scores (Working Memory, Perceptual Reasoning, and Verbal Comprehension) compared to those with well water As levels < 5 μg/L, even after adjusting for the home environment, number of children in the home, and maternal intelligence (Wasserman et al., in press). A committee convened by the National Research Council on toxicity of inorganic As released an interim report in November 2013 which reviewed substantially expanded epidemiologic studies of associations between drinking water As exposure, particularly early-life exposure, and a variety of adverse health outcomes, noting that the studies increasingly characterize risks at the more common low to moderate As exposures (up to 100 μg/L As). Although extrapolating the well-established dose response relationship from moderate to high As exposure to low dose is a controversial aspect of As risk assessment, the committee recommends that health effects from early-life exposure be considered in updating toxicologic assessments because early-life exposure to As, even at low concentrations, increases the risk of adverse health effects and impairs development in infancy, childhood and later in life (NRC, 2013).
In 2001 the Environmental Protection Agency (EPA) adopted the current maximum level of contaminant (MCL) for As in drinking water of 10 μg/L, replacing the old MCL of 50 μg/L, giving water systems until January 2006 to comply. Although these national standards for As have been in place since the passage of the Safe Drinking Water Act in 1974, domestic wells are private, so it is solely the responsibility of the well owner to have their water tested and treated as necessary. There is no authority tasked with ensuring that private drinking water is brought into compliance with federal regulations. States have taken different approaches to alerting their residents of risks and have in some cases tried to fill the gap with further regulations such as a testing requirement at the time of real estate sale in New Jersey, but it ultimately falls to the homeowner to take action to test.
According to the 2009 American Housing Survey, 15,846,000 homes in the U.S. are served by a private well (U.S. Census Bureau, 2009), and the majority of these households are located in rural areas (Simpson, 2004). The U.S. Geological Survey (USGS) reports that more than 20% of 2100 private domestic wells sampled nationwide from 1991–2004 contained at least one contaminant at levels of potential health concern and about 7% were above the MCL for As (DeSimone et al., 2009). The samples with As concentrations most frequently greater than human-health standards were found in the crystalline-rock aquifers in New England, basin-fill aquifers in the western and south-central U.S., and basaltic-rock aquifer in Idaho. These same areas in the country often have high rates of private well water supply.
Few studies have sought to understand why homeowners in the United States and Canada do or do not test their private well water specifically for As. Studies in areas of high As occurrence in Nevada, USA with a fairly constant flow of public information about As in groundwater found substantial portions of the population are not concerned about As in wells; 40.1% rated their level of concern about As as less than “somewhat concerned” (Walker et al., 2006). Community-based interventions in Quebec, Canada have been found far more effective than mass media campaigns at motivating water testing for As, however, the testing rates in the area still remained a low 16% compared to the earlier 4% before intervention (Renaud et al., 2011). Despite these low testing rates, bivariate analysis of survey data found that well owners in this region who said they knew acquaintances who had already tested for As were up to 11 times more likely to decide to test for As themselves, demonstrating the power of social norms (Renaud et al., 2011).
Several studies attempted to understand why homeowners in the United States and Canada do or do not test their private well water for other agents of health concern. A postal survey of 246 residences in Ontario, Canada found that 80% of respondents were “very concerned” or “concerned” about the overall safety of the water from their private source, yet 21% of all households had never tested their well water and among those that did, testing for parameters other than E. coli and total coliforms was very uncommon (Jones et al., 2006). The most common reasons households gave for not testing were inconvenience, time issues, and having no health problems or noticeable water changes (Jones et al., 2006). Another study of private well owners in Ontario, Canada attempted to improve well testing rates by removing the barriers of cost and convenience, delivering well water information kits with sampling bottles directly to well owners and collecting them the following day, offering nitrate and bacteriological sampling at no charge (Hexemer et al., 2008). Yet even with these barriers removed participation rates were still disappointing, between the two study phases only 45.2% of households participated in the nitrate testing and 46.6% participated in bacteriological testing, an approximate doubling of the background testing rate in the region at the time. A follow-up telephone survey of participants and non-participants found that the groups did not differ significantly in their concern for the quality of their well water, although there was a significantly higher rate of non-response to this survey among non-participants in the testing (Hexemer et al., 2008). Taken together, these studies suggest that often awareness does not translate into concern, that concern does not translate into testing action, and that cost/convenience barriers do not fully account for low testing rates.
Consumption of water not meeting drinking water quality standards, due to As or otherwise, can be a threat to health, therefore any actions to ensure water quality, reduce exposure, and prevent disease, can be viewed as health behaviors. Well water testing is a health behavior, yet because As testing only detects high levels and does not immediately reduce the risk, understanding the factors influencing testing decision-making can be more complicated than with other protective health behaviors. The closest comparison with homeowner well testing behavior may be the more well-studied behavior of home radon testing, a similar environmental health protective action. Beliefs about the costs and difficulty for mitigating the hazard if an As problem is found may necessarily weigh into decisions for initial testing. However, correlations between perceptions on ease of radon mitigation with test intention were not found significant in New Jersey (Weinstein et al., 1990), suggesting that people may not be considering the difficulty of risk reduction when deciding whether to test. Similar to the radon example, it is possible that the potential need for As mitigation is too distant from the present to be taken into consideration during testing. Instead, beliefs about the likelihood and seriousness of home radon problems were found to be strongly associated with testing intentions (Weinstein et al., 1990). Higher personal threat perceptions are correlated with testing behavior, yet individuals often are optimistically biased and tend to believe that their own risk for encountering a problem is lower than their neighbors’ (Weinstein et al., 1988; Weinstein et al., 1990), even if they live in known high-risk areas. In this way those in communities well informed of well water risks may still not feel enough personal risk to warrant taking testing action.
Studies on safe water consumption and other health behaviors have often found that risk perception alone can be a weak predictor of health behavior change, because actually testing well water is different from knowing the need for it. Sandman and Weinstein (1993) examined 4 data sets to identify the predictors of home radon testing and found that the variables are different based on the homeowner’s stage of testing behavior. General radon knowledge and knowing other people who are concerned or have tested best predict whether someone has thought about radon testing. Once having thought about it, the decision to test is most closely related to the perceived likelihood of a radon problem, which is subject to the optimism biases discussed above. Situational factors related to the difficulty of testing seem to constitute the final barrier between those who have decided to test and those who have already tested their home for radon. Recognizing the complexity in the health behavior decision making process, an integrated model of health and social psychology theories, the RANAS (Risk, Attitude, Norms, Ability, Self-regulation) Model (Mosler, 2012), goes beyond risk information as a motivator for health behavior change and outlines the blocks of determinants that must be favorable in order for a behavior, such as regular well testing, to take root. This model has already been applied to understand preferences for and uptake of various As mitigation options in rural Bangladesh (Inauen, 2012). Once the motivating factors for behaviors are identified, targeted interventions can be designed. A cluster randomized controlled trial in Bangladesh evaluated the effectiveness of an interactive household-level education intervention to increase the demand for fee-based As testing, finding that the education program increased the households’ demand for well testing by 40% compared with offering testing alone (George et al., 2013). These intervention households also had higher well switching rates after bad As test results. To the best of our knowledge, factors influencing domestic well testing behavior in the United States have not been systematically evaluated based on the RANAS model’s understanding of health and social psychology theories.
This study aims to determine barriers for well testing in central Maine, an area with high domestic well-water dependency and frequent natural groundwater As occurrence. Roughly half of the population of Maine obtains their drinking water from a private source. A study by the USGS (Nielsen et al., 2010) on a database of 11,111 individual well tests by the Maine Health and Environmental Testing Laboratory from 2005 to 2009 reported that in 44 Maine towns more than 25 percent of the wells exceeded 10 μg/L As, while overall 18 percent of wells across 531 towns exceeded 10 μg/L As. A household survey was implemented by mail in January 2013 in 13 towns of the greater-Augusta area with the goal of understanding the testing and treatment behaviors of the area population as well as the key behavior influencing factors, with a focus on As testing specifically. A better understanding of behavior barriers and influencing factors will provide a better basis for developing interventions that more effectively promote testing behaviors in at-risk communities.
2. Methods
2.1. Study Area
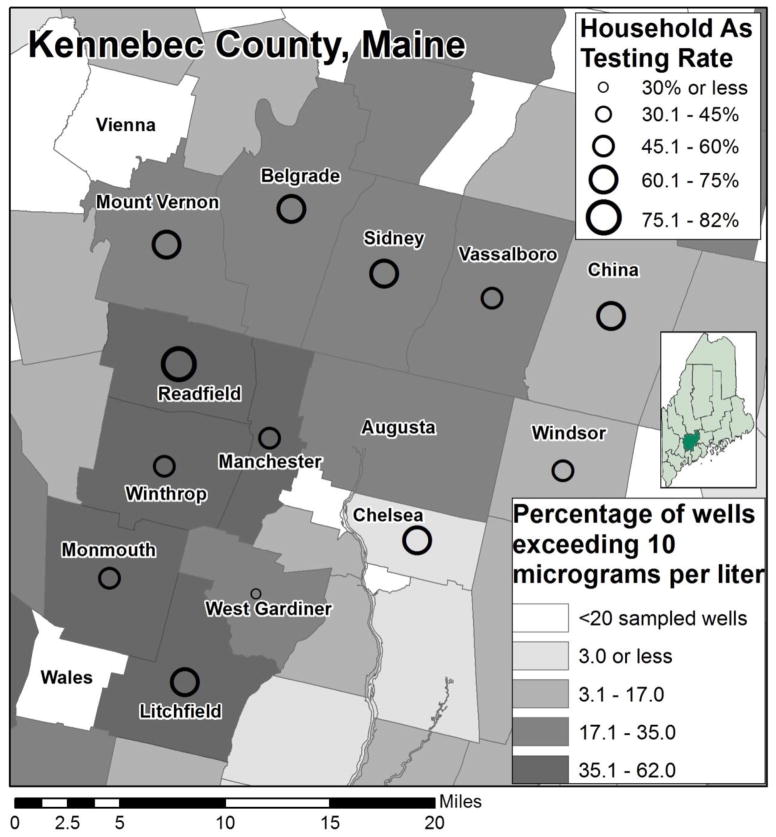
The study area comprises 13 towns of Kennebec County, central Maine with high rates of private well water supply: Belgrade, Chelsea, China, Litchfield, Manchester, Monmouth Mount Vernon, Readfield, Sidney, Vassalboro, West Gardiner, Windsor, and Winthrop (Table 1). The census data of 2010 reports 45,473 residents in these 13 towns; 15,400 (or 84%) of the total 18,300 households in the study area are estimated to be self-supplied by private wells (Nielsen et al., 2010; US Census 2010). Between 2006 and 2011, the Superfund Research Program (SRP) of Columbia University and the Maine Geological Survey tested 1,428 domestic well water samples in 17 towns of Kennebec County and found that 31% of domestic wells exceeded the EPA MCLs for As (Yang, 2010). Four towns (Augusta, Farmingdale, Hallowell, and Waterville) included in Columbia’s previous testing program were excluded from this survey because the majority of those town populations rely on public water supply.
Table 1.
Population and As occurrence in 13 study towns, as well as As testing behaviors in the area
| Town | Total populationa | Population using domestic wellsb | Percentage of wells exceeding As 10 ug/Lc | Percentage of wells exceeding As 10 ug/Lb | As Testing rated | Surveye d HHs in analysis (N) |
|---|---|---|---|---|---|---|
| Belgrade | 3189 | 3087 | 32% | 33% | 62.1% | 38 |
| Chelsea | 2721 | 2658 | 18% | 3% | 61.8% | 35 |
| China | 4328 | 4168 | 25% | 14% | 65.9% | 41 |
| Litchfield | 3624 | 3417 | 45% | 42% | 62.4%e | 39 |
| Manchester | 2580 | 1731 | 48% | 62% | 52.1% | 21 |
| Monmouth | 4104 | 3234 | 40% | 45% | 57.5% | 41 |
| Mount Vernon | 1640 | 1609 | 32% | 35% | 71.4% | 21 |
| Readfield | 2598 | 2517 | 40% | 49% | *82.1% | 29 |
| Sidney | 4208 | 4057 | 29% | 30% | 68.6% | 51 |
| Vassalboro | 4340 | 3277 | 23% | 35% | 51.5% | 34 |
| West Gardiner | 3474 | 3411 | 31% | 24% | *30.8% | 39 |
| Windsor | 2575 | 2508 | 14% | 10% | *46.4%e | 25 |
| Winthrop | 6092 | 2772 | 47% | 46% | 52.6% | 38 |
| Total/Average | 45,473 | 38,446 | 33% | 35% | 59.0% | 452 |
| Vienna & Walesf | 2186 | 1994 | --- | --- | 58.4% | 72 |
Maine Well Water Testing and Treatment Survey 2013, considered highest likely rate of being ever-tested for As; a consistently large portion of respondents did not remember the results of their test and so may not remember accurately that an As test was in fact performed
An additional 46 and 43 HHs respectively were surveyed in Litchfield and Windsor, confirming As testing rates above within +/− 0.1%
Combined because of small populations, the As rate of these towns is unknown because <20 wells have been tested in the state lab
HH = Household
Significantly different from the population mean across towns, p<0.05.
As testing and occurrence rates not significantly correlated across towns.
2.2. Survey Instrument
Participants completed a 10-page questionnaire on their water testing and treatment practices, preferences, and opinions, as well as basic demographic information. Development of the survey was informed by small community meetings held in Belgrade and Hallowell, Maine and through voluntary pre-testing by staff members of the Maine Geological Survey and USGS Water Science Center who are also area residents and private well owners. The survey also included a section with questions designed to measure the RANAS (Risk, Attitude, Norms, Ability, Self-regulation) factors that may influence testing and treatment behaviors. The RANAS portion of the survey instrument included a series of statements that respondents indicated their agreement with on a scale of 1 to 6 from strongly disagree to strongly agree (see Appendix).
2.3. Survey Implementation
Surveys were mailed to 996 households in 13 towns of Kennebec County, Maine, randomly selected from lists of addresses obtained from town offices and the Department of Motor Vehicles; 900 were successfully delivered by US Postal Service (USPS). Stratified random sampling was used to select addresses by town in proportion to population.
An additional 100 surveys each were mailed to random households in Litchfield and Windsor, as examples of towns with relatively high and low known As occurrence rates, respectively (Table 1). A random selection of 150 households from Vienna of Kennebec County and Wales of Androscoggin County (combined population 2186 with 92% well supply), two towns that share borders with and have similar geology as Columbia SRP towns but have not been exposed to previous SRP testing activities and have unknown As occurrence rates, also received mailed surveys. Up to 321 of these extra 350 surveys were successfully delivered by USPS.
Contact strategy was based on Dillman’s Tailored Design Method (Dillman, 2000) employing repeated contact to increase the response rate. Selected addresses were mailed a pre-survey letter, a survey with cover letter, a thank you post card and a follow-up reminder with a replacement survey. Enclosed with the original survey was a $2 cash incentive for participation. The study protocol and survey instruments were approved by the Institutional Review Board of Columbia University.
2.4. Data Analysis
The descriptive analysis employed SPSS 21.0. Spearman correlations were calculated between demographic and behavior variables and testing actions. RANAS factors were analyzed for mean, standard deviation, spearman correlation, and entered into simultaneous binary logistic regression to identify significant predictors of behavior. Only surveys with fully completed RANAS factor responses were included in the regression analysis.
3. Results
3.1. Sampled and General Population Characteristics
The response rate was 58.3%; 525 out of 900 likely-delivered surveys were returned completed. Of these, 452 were suitable for our study, i.e. the households are supplied water by a private well. Another 33 households returned the survey but declined to participate and so were not included in the response rate. We estimate about 16% of households in these surveyed towns do not have well water, which could account for a portion of the non-responses. Of the respondents (Table 2): 54% were male, 28.1% had children in the home, a median age of 55 years, median education category of “technical/community college”, and median income range of $40-59,000. Nearly all were homeowners. Comparison with results of the 2010 U.S. Census indicated that the sample population is slightly older than the general population but generally similar in education, income, and child-households, reflecting the random selection of households and minimal selection bias.
Table 2.
Demographic Characteristics of Survey Respondents (N=525) and Population in 13 towns of Kennebec County, Maine, in 2013 and 2010, respectively.
| Demographic Characteristic | Sample (N=525) | Populationa |
|---|---|---|
| Median Age (years)b | 55 | 50 |
| Sex Ratio (M/F) | 54% / 46% | 49.4% / 50.6% |
| Homeownership (%Owners/%Renters) | 92.5% / 7.5%c | 85% / 14.4% |
| Median education | Technical/Community Colleged | Associate’s degree |
| Median income | $40,000 – 59,000e | $54,883 |
| Households with children <18 Years Old | 28.1% | 31.7% |
Survey respondents were required to be at least 18 years old; for population median age is only of those 18.≥25th and 75th percentile ages for sample are 47 and 65, respectively.
Rental units are more prevalent within the bounds of public water supply systems than private well households
25th and 75th percentile education levels for sample are high school/GED and bachelor’s degree, respectively.
18% of respondents chose not to report income. 25th and 75th percentile income levels for sample are $20,000–39,000 and $60,000–79,000, respectively.
3.2. Testing Practices
Although nearly 78% of the households reported that they have had their well tested, about half of them did so more than 5 years ago (Table 3). In the state of Maine, testing is recommended every year for bacteria, nitrates, and nitrites, and every 3 to 5 years for chemicals such as As, radon, and uranium. Additionally, 27.4% of households who have ever tested their well water reported that the last test was when they purchased the house, a common occasion for well testing, but which suggests they are not in the habit of monitoring water quality on a regular basis. Three quarters of reported well test costs were less than $70, including a large number of households that reported free testing either offered by Columbia University or as part of a real estate transaction.
Table 3.
Sample Descriptive Statistics for Key Variables (N=452 HHs with wells)
| Variables | Percentage | |
|---|---|---|
| Have you ever had your well water tested by a lab? | Yes | 77.7% |
| No | 17.9% | |
| Don’t Know | 4.4% | |
|
| ||
| Approximately when was your well water last tested? | <12 Months Ago | 10.0% |
| 1–5 Years Ago | 28.5% | |
| More than 5 Years Ago | 38.7% | |
|
| ||
| What was your water tested for the last time it was tested? | Arsenic | 43.7%a |
| Bacteria | 39.5% | |
| Fluoride | 23.1% | |
| Radon | 21.1% | |
| Uranium | 14.9% | |
| Others | 21.7% | |
| Don’t Know | 23.1% | |
|
| ||
| Has a test of your water ever shown a problem with any of the following? | Arsenic | 16.9% |
| Bacteria | 14.0% | |
| Fluoride | 1.6% | |
| Radon | 2.9% | |
| Uranium | 1.6% | |
| Others | 9.5% | |
| Don’t Know | 14.0% | |
|
| ||
| If your well was tested for arsenic, what was the highest arsenic level measured? | <10 μg/L | 18.6% |
| 10–50 μg/L | 6.2% | |
| 51–100 μg/L | 0.9% | |
| >100 μg/L | 0.4% | |
| Don’t remember | 32.6% | |
| Never tested | 41.2% | |
If the last test was before 2001, the probability it included As (23.8%) is significantly different than all more recent testing (69%, p<.01). The rate of last test including As varies between 31%–82% among the 13 towns.
Arsenic and bacteria are the most commonly tested for (Table 3), possibly because As has been included in the standard well testing package for the state of Maine since 2001 and was mentioned several times in the survey materials. Household tests that were performed more recently than 2001 were significantly more likely to include As than prior to that year (Table 3). Many households reported having a water problem with As at some time but far fewer report radon, likely due to the low testing rates in the area. Of those that have tested for As, the majority does not remember the test results, and few households report receiving a test result over the MCL of 10 μg/L.
A better educated, higher income homeowner who more recently purchased their home is most likely to have included As in their last well test (Table 4). The median length of time survey respondents have lived in their present home is 15.5 years. The longer a respondent has lived in their home the less likely they are to have tested their well at all in the last 5 years, to have had As included in their last well test if they had one, and the lower their intention to test their well currently is (Table 4). That many households have not tested since the purchase of their home indicates that regular testing behavior is low. In fact less than 7% of respondents report that they test their well water on a regular basis. Although age and years lived in home are significantly correlated with each other (r=.513, p<.001), only age is significantly and negatively associated with intention to test well water. Education is significantly and positively associated with having tested in the last 5 years and included As in the most recent test, and income is only significantly and positively associated with whether As was included in the most recent well test.
Table 4.
Associations (rs) between Demographic variables and testing behaviors
| Descriptive | Tested for anything in the last 5 Years | Last test included As | Intention to test well |
|---|---|---|---|
| Years in Home | −.171** | −.202** | −.171** |
| Age | −.034 | −.086 | −.121* |
| Education | .118* | .253** | .054 |
| Income | .058 | .205** | .063 |
Significant to the .05 level;
Significant to the .01 level
Spearman’s rank correlation coefficients were calculated between dependent behavior variable and independent demographic variable. Years in home and age are continuous variables; income and education are ordinal categorical variables.
The top 5 reasons that homeowners reported having their well tested were: “To know if my well water was safe to drink” (31%), real estate transaction (30%), new well constructed (15%), “There was a problem (smell, taste, quality) with our well” (14%), and “I read or heard about a well water quality problem in our area” (13%). When asked what would most prompt them to have their well water tested and given 11 options as well as an “other” write-in option, the top 5 prompts were: “A change in the taste, smell, or appearance of my water” (76%), “Learning that my neighbors have contaminated water” (59%), “Well testing available for free” (59%), “Unexplained health problems such as frequent diarrhea or stomachaches” (36%), and “Learning that some wells in my town are contaminated” (31%).
3.3. Behavior Influencing Factors
The responses to the RANAS factor survey questions are analyzed to identify other behavior-influencers beyond those self-reported by homeowners above. The mean RANAS factor response scores for the full survey sample are organized into their respective categories in Table 5. Respondents indicated their level of agreement with each statement by selecting from 1 (Strongly Disagree) to 6 (Strongly Agree), so that a mean response >3.5 suggests general agreement and <3.5 suggests general disagreement in the population. Although there is high variability in responses, the mean scores indicate that while households generally agree with the severity of water and As-related health risks (M=4.3-5.0), they feel low personal vulnerability (M=3.0–3.4). Although they agree with the benefits of testing (M=5.3) they generally disagree that regularly testing is affordable (M=3.0). There are very low testing norms overall. Households do not believe their neighbors (M=2.5), friends (M=2.3), or relatives (M=2.3) are regularly testing their well water or that they are expected to test by peers (M=1.9) or authorities (M=2.0). Most respondents do not know someone with an As well problem (M=2.9). There is high acknowledgement that well testing is a personal responsibility (M=4.9) yet feelings of personal obligation to do so are more neutral (M=3.5). In general the sample population expresses the ability (M=4.3–4.8) and strong intention to test their wells (M=4.9), but self-regulation factors like remembering (M=3.9) and action planning (M=3.6) are lower.
Table 5.
Means and Standard Deviations of RANAS Variables, Associations (N=452) and Summary of Binary Logistic Regression Analysisa (n=278) for RANAS Variables Predicting the Behavior of Having Tested Well Water and Included As in the Most Recent Test
| Variable Agree | (1 = Strongly Disagree; 6 = Strongly Agree) | Mb | SD | rs | OR | 95% CI |
Li M |
Wi M |
V/W M |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Lower Upper | ||||||||||
| I. Risk | ||||||||||
| a. | Vulnerability | |||||||||
| Family risk for drinking contaminated water | 3.0 | 1.7 | .08 | .99 | .76 | 1.28 | 2.8 | 2.9 | 2.7 | |
| Town risk for well As contamination | 4.2 | 1.5 | .19** | 1.28 | .88 | 1.86 | 4.2 | 3.7 | 3.6c | |
| Household risk for drinking As contaminated water | 3.4 | 1.7 | −.02 | .83 | .62 | 1.13 | 3.3 | 3.0 | 2.9c | |
| b. | Severity | |||||||||
| Adverse health effects from drinking well water not overblown | 4.3 | 1.5 | .16** | 1.19 | .91 | 1.56 | 4.1 | 4.3 | 4.3 | |
| As-related health effects likely serious | 5.0 | 1.2 | .13** | .60 | .36 | 1.01 | 5.2 | 5.0 | 5.2 | |
| Health risks from As exposure not overblown | 4.6 | 1.3 | .15** | 1.21 | .87 | 1.67 | 4.7 | 4.5 | 4.7 | |
| c. | Knowledge | |||||||||
| Wells in area at risk of contamination | 3.9 | 1.6 | .21** | .96 | .72 | 1.28 | 3.6 | 3.6 | 3.4 | |
| Well water quality can change overtime | 4.5 | 1.3 | .18** | 1.16 | .86 | 1.56 | 4.3 | 4.7 | 4.6 | |
| We can be exposed to As from well water | 4.9 | 1.3 | .18** | .88 | .66 | 1.17 | 5.3 | 4.8 | 4.9 | |
| Years of exposure increases As-related health risks | 5.0 | 1.1 | .16** | 1.92* | 1.11 | 3.31 | 5.2 | 5.1 | 5.2 | |
| II. Attitude | ||||||||||
| a. | Instrumental | |||||||||
| Testing results helpful to protect family health | 5.3 | 1.0 | .16** | .55* | .34 | .88 | 5.4 | 5.3 | 5.2 | |
| Regularly testing is affordable | 3.0 | 1.5 | .14** | 1.00 | .80 | 1.27 | 2.7 | 2.2c | 2.7 | |
| Regularly testing does not take too much time | 4.4 | 1.4 | .20** | 1.59** | 1.14 | 2.21 | 4.0 | 4.5 | 4.3 | |
| Concerned that bad test will hurt property value | 3.3 | 1.7 | .12* | 1.03 | .80 | 1.32 | 3.5 | 3.4 | 3.7 | |
| b. | Affective | |||||||||
| Feel safer having well tested by lab | 4.9 | 1.3 | .19** | 1.09 | .78 | 1.53 | 5.2 | 5.2 | 4.7 | |
| Feel better knowing what is in well water | 4.9 | 1.6 | .21** | 1.10 | .86 | 1.40 | 5.1 | 4.5 | 4.9 | |
| Concerned about water despite drinking long time with no problem | 3.7 | 1.7 | .24** | 1.03 | .80 | 1.32 | 3.6 | 3.6 | 3.3 | |
| III. Norms | ||||||||||
| a. | Descriptive | |||||||||
| Neighbors regularly test well water | 2.5 | 1.2 | .08 | 1.46* | 1.01 | 2.09 | 2.1c | 2.3 | 2.4 | |
| Relatives recently tested well water | 2.3 | 1.4 | .11* | 1.15 | .84 | 1.58 | 2.0 | 2.3 | 2.1 | |
| Friends recently tested well water | 2.3 | 1.3 | .08 | .82 | .54 | 1.26 | 1.9c | 2.1 | 2.1 | |
| Know someone with As well problem | 2.9 | 2.0 | .17** | 1.09 | .91 | 1.32 | 2.7 | 2.4 | 2.4c | |
| b. | Injunctive | |||||||||
| Neighbors expect me to regularly test well water | 1.9 | 1.1 | .03 | .99 | .68 | 1.45 | 1.6 | 1.7 | 1.7 | |
| Local authorities recommended to test well water | 2.0 | 1.4 | .05 | .77 | .59 | 1.01 | 1.9 | 1.8 | 1.6c | |
| c. | Personal | |||||||||
| Feel personally obligated to test well water | 3.5 | 1.7 | .18** | 1.06 | .83 | 1.34 | 3.1 | 3.7 | 3.1 | |
| My responsibility to have water tested | 4.9 | 1.4 | .11* | .80 | .62 | 1.04 | 4.8 | 4.6 | 4.6 | |
| IV. Ability | ||||||||||
| a. | Action Knowledge | |||||||||
| Know who to contact to get well tested | 4.3 | 1.8 | .37** | 1.69** | 1.31 | 2.19 | 4.0 | 3.5c | 3.9 | |
| b. | Self-efficacy | |||||||||
| Finding well testing service is easy enough | 4.4 | 1.5 | .25** | .72* | .52 | .99 | 3.9c | 3.8c | 4.0 | |
| Confident can manage regularly testing water | 4.4 | 1.4 | .30** | 1.28 | .97 | 1.69 | 4.1 | 4.0 | 4.2 | |
| Something can be done about As level in water | 4.8 | 1.4 | .26** | 1.23 | .94 | 1.63 | 5.0 | 4.7 | 4.8 | |
| V. Self-regulation | ||||||||||
| a. | Action Planning | |||||||||
| Thought about having well water tested | 4.5 | 1.7 | .36** | 1.17 | .93 | 1.48 | 4.8 | 3.9 | 4.5 | |
| Plan to have well tested within next year | 3.6 | 1.7 | .20** | 1.10 | .87 | 1.39 | 3.4 | 3.3 | 3.2 | |
| b. | Remembering | |||||||||
| No problem remembering when I want to | 3.9 | 1.8 | .13** | 1.024 | .83 | 1.27 | 3.8 | 3.7 | 3.8 | |
| c. | Commitment | |||||||||
| Committed to monitoring quality of well water | 4.1 | 1.5 | .25** | .994 | .75 | 1.32 | 4.0 | 3.2c | 3.7 | |
| Committed to drinking safe water | 5.2 | 1.0 | .22** | .932 | .63 | 1.38 | 5.0 | 5.2 | 5.2 | |
| VI. | Intention to have water tested | 4.9 | 1.5 | .21** | 4.9 | 5.2 | 4.8 | |||
Significant to the .05 level;
Significant to the .01 level
OR = Odds ratio, CI = Confidence Interval, Li = Litchfield, Wi = Windsor, V/W = Vienna and Wales
OR can be interpreted as the increase in odds of having included As in the most recent well test associated with each unit increase of agreement on the survey scale (from 1 to 6)
Nagelkerke R Square = .415; Overall predictive rate of 75.5%
<3.5 means disagreement on average, >3.5 means average agreement
Significantly different from study area mean to the .05 level
Cronbach’s alpha was calculated to test inter-item correlation within each RANAS factor block but in almost all cases was too low (<.70) to justify a combined factor for analysis, so each was kept individually. Repeating the regression analysis with a mean Vulnerability score (cronbach’s alpha = .772) and mean descriptive testing norms score (cronbach’s alpha = .744) similarly identifies knowledge that years of exposure increases As-related health risks, believing regularly testing does not take too much time, and knowing who to contact to get the well tested as significant predictors. Additionally believing that As-related health effects are likely serious and knowing someone with an As well problem emerge as significant. However, when descriptive testing norms of neighbors, relatives, and friends are combined the significance of having neighbors who regularly test their well water is lost. Nagelkerke R Square = .400, overall predictive rate of 74.8%.
These factors were analyzed further for their influence on specific testing behaviors, comparing the responses of those performing or not performing the behavior. Overall 29 of the 34 factors incorporated in the questionnaire are significantly associated with the behavior outcome of having As included in the most recent well test. Cronbach’s alpha was calculated to test the inter-item consistency within RANAS factor blocks but in almost all cases was too low (<.70) to justify combining items for analysis and so each statement was treated as an independent variable. When these 29 variables are entered into simultaneous binary logistic regression analysis, 6 emerged as being significant predictors (p<.05) of having As included in the most recent well test: having knowledge that years of exposure increases As-related health risks (risk knowledge) (OR=1.92), believing that regularly testing does not take too much time (instrumental attitude) (OR=1.59), having neighbors that regularly test their water (descriptive norm) (OR=1.46) and knowing who to contact to test well water (action knowledge) (OR=1.69) were all significant. However, those who believe that finding a well testing service is easy (self-efficacy) are less likely to have included As in their most recent well test (OR = .72). And, oddly, those who believe more strongly that testing results are helpful to protect family health are also less likely to have included As in their most recent well test (OR=.55). However, the mean response to that statement among respondents was between agree and strongly agree so the low OR must be considered within the limited variation in the population, but it is still puzzling. On the survey, respondents reported agreement with these RANAS statements on a scale from 1 Strongly Disagree, to 6 Strongly Agree; these odds ratios reported in Table 5 can be interpreted as that each unit increase in agreement on the survey scale is associated with the corresponding increased odds of a homeowner having As included in their most recent well test. Although level of agreement can be rank ordered it is not possible to assign a real value to each level, so the use of ORs in Table 5 is less about the numerical value produced by logistic regression and more about the significance and direction of the relationship between stronger agreement with a RANAS statement and increased odds of the testing behavior.
3.4. Additional Surveys
Although the small sample size of additional surveys from the non-SRP towns (Vienna and Wales, n=72) and the extra-sampled high- (Litchfield, n=45) and low- (Windsor, n=44) As occurrence towns limits analysis there are some interesting findings to note. Among those who tested their well in the last 5 years, households in SRP towns were significantly more likely to have tested for As (71% vs. 50%, p<.05) than in the non-SRP towns with unknown As-contamination rates, perhaps reflecting the success at the recent testing program in reaching a large number of households in the population. The As contamination rate in these towns is unknown because not enough wells have been tested through the state lab. As might be expected, respondents from these two towns were significantly (p<.05) more likely to disagree with the statements “I know someone with an arsenic well problem” (M=2.4) “There is a considerable risk that wells in this town are contaminated with arsenic” (M=3.6) and “Our household is at risk of drinking arsenic-contaminated well water” (M=2.9) than survey respondents in the main SRP study area (M=2.9, M=4.2, M=3.4, respectively)(Table 5).
Households in Litchfield, which we’ve estimated has 45% of wells contaminated with As (Table 1), were significantly more likely to have ever tested for As than households in the town of Windsor, estimated at 14% contamination, (62% vs. 46%, p<.05). Significant predictors of having tested well water in the last 5 years in Litchfield included believing “wells in this area are at risk of contamination” and “neighbors expect me to regularly test well water,” factors which were not significant in Windsor. Windsor respondents were significantly more likely to disagree with the statements “I know who to contact to get my well water tested,” and “I am committed to monitoring the quality of my well water” compared to the main survey sample (Table 5). Although the correlation between testing rate and As occurrence across all towns was not significant, perhaps due to sample size at town level, the difference between these extra-sampled towns demonstrates that higher risk towns may drive higher risk awareness and testing norms and in turn lead to higher testing rates.
4. Discussion
Public officials have been encouraging all Maine households with private wells, roughly half of the state’s population, to have their water tested and to take steps to treat their water for As when appropriate. The campaign for testing has shown progress: The Maine CDC, using the Behavioral Risk Factor Surveillance Survey (BRFSS), has determined that the rate of well testing for As across the state has increased from 27% in 2003 to 42% in 2009. This survey finds that the ever testing rate for As in Kennebec County may now be as high as 59% although only 44% of households report that As was included in their most recent well test. Of those who report having ever had an As test, the majority (55%) does not remember the results and very few report receiving As results above 10 μg/L (13%). There may also be confusion among homeowners who received results that their water was satisfactory prior to the EPA’s change to a lower standard for drinking water, from 50 μg/L to 10 μg/L, in 2001. It is concerning that 20% of households that have ever been tested for As were last tested before 2001 and have not since retested under the new standard. Our other survey study that followed up with 256 households who had all received test results of As >10 μg/L between 2006–2010 (Flanagan et al., this issue) found similar rates of forgetting; 31% did not remember their As test results and 14% recalled incorrectly, more often underestimating their As level. In addition to As (Yang et al., 2009; Nielsen et al., 2010), state lab testing and Columbia University testing have shown that the greater-Augusta area of Central Maine has high Rn occurrence along with other natural contaminants in the groundwater. (Yang et al., 2014), so it is concerning to find that 22% of households in this area may have never tested their well water for anything. Although appropriate well testing behavior is important for any water quality parameter of concern, our discussion of well testing behavior, below, is probably most relevant to As which remains of particular concern given the frequent contamination of wells in this area.
Similar to published findings on indoor air radon testing behavior, homeowners in this study area are subject to a similar optimistic bias: aware of As dangers but more likely to agree to a town risk of well As contamination than to a household or family risk of drinking contaminated water, demonstrating low perceived personal vulnerability. Those that have lived longer in their current home have lower testing behaviors overall. This is likely due to a lowering of perceived personal vulnerability over time; indeed, the RANAS analysis revealed a significant negative association between testing behavior and the feeling of not being concerned about well water because one has been drinking it a long time with no problem. The association between years lived in home and this feeling of unconcern was significantly positive. The longer someone has lived in a home drinking from a well with no visible problems, the less concerned they are about the water quality and so less likely to seek out a well test for anything, not just As. Homeowners who may have had a well test during their initial real estate transaction likely did not have As included if it was performed more than a decade ago, and if they did, the “safety” was judged using a higher drinking water MCL for As. Unfortunately even with new state legislation to require well testing at point of sale similar to that implemented in New Jersey, it will still miss reaching these at-risk households who have been in the same house for decades and do not feel concerned enough to act.
The surveyed households reported low regular testing behavior (7%) and perceived norms for regular testing behavior (M=2.5), although most (78%) surveyed households have had their well tested at some point (real estate transactions being the most common occasion), and many may have ever tested for As (59%). The average respondent disagrees that their friends, neighbors, or relatives have recently tested their well water. Yet the logistic regression analysis revealed that believing one’s neighbors regularly test their well water is one of the most significant predictors of whether a well owner had As included in their most recent test. According to Mosler’s RANAS model, low mean scores for norms and their regression-identified significant influence on behavior suggest a strong potential for behavior improvement if interventions were selected to focus on this factor (Mosler, 2012). Communication strategies that focus on highlighting descriptive norms are therefore likely to be more effective at promoting testing behavior, although this will require further study.
Aside from the knowledge that years of exposure increase As-related health risks belonging to the Risk Block of RANAS, the most significant predictors of the testing behavior were not part of the Risk block of RANAS. Instead, norm, ability, and attitude factors all had significant influence on the behavior as well. Highlighting the ease of the testing process or addressing the perceived hassles of testing could improve attitudes towards regular testing. Simply knowing who to contact to get a well water test or being aware that your neighbors are regularly testing their well water may help to motivate test-seeking behavior as well. It is important to recognize these other factors beyond risk information that may influence target behaviors when implementing interventions to promote them.
There are limitations of this study in capturing all of the influences and barriers to home well water testing, and specifically for As. When we analyze predictors of the behavior outcome of having As included on the most recent well test, we are not able to separate those homeowners that made a conscious decision to test for As specifically from those that made the conscious decision to order the full state lab recommended testing package (inorganics/coliform for $165) which has included As since 2001. For the purposes of As mitigation, these equally beneficial testing actions produce the same result and so the influencing factors identified remain relevant. However, we are limited in being able speak directly to the specific As-related intention of the homeowner behind these actions. Lastly, since water testing as a health behavior does not in itself reduce any exposure risks that may be found, beliefs about the next step of As mitigation may still influence decision-making for testing.
5. Conclusion
In their research on home radon testing, Weinstein et al. (1990) conclude that “it appears community members frequently overestimate hazards in situations where remediation is a government or corporate responsibility, where the problem is industrial rather than natural, and where the community is outraged over what it feels is deception or unfair treatment.” Our study in central Maine suggests that the reverse is also true. Groundwater As contamination is often naturally-occurring and the government has no responsibility over private well water. Homeowners in As-affected communities have the tendency to underestimate the hazard of As despite the risks, either because they do not perceive that risk to themselves or because a combination of significant norm, ability, and attitude factors and barriers is influencing their behavior.
As long as private well testing and treatment is left up to the owners, there will always be population exposure to As through drinking water. Without significant motivation or a requirement, such as New Jersey’s real estate sale regulations, some households will never test their well for As, perhaps due to low perceived personal risk or other factors. Even with mandatory testing or intense motivation, the problem of As exposure still isn’t solved by the act of testing; testing is just the first step on the road to effective As mitigation.
Supplementary Material
Figure 1.
Study Area
Well prevalence from Nielsen et al. 2010, based on Maine Health and Environmental Laboratory testing. Testing rates for As from household survey.
Highlights.
Private wells serving 43 million Americans are the owner’s responsibility to test
41% of well owners in the Central Maine study area have never tested for arsenic
Better educated and higher income households are more likely to have tested
Risk, ability, attitude and norm factors influenced testing behavior
Well owners perceive lower arsenic risk for themselves than for their neighbors
Acknowledgments
This research is funded by the U.S. National Institute of Environmental Health Sciences Superfund Research Program 3 P42 ES10349 to Y. Zheng. We thank A. Smith and colleagues of Maine Center for Disease Control and Prevention and J. Inauen of University of Zurich for helpful discussions. Thanks also to Q. Yang for sharing unpublished groundwater data for the study area and to the staff of Maine Geological Survey for assistance in survey implementation. This is LDEO contribution ####.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- DeSimone LA, Hamilton PA, Gilliom RJ. Quality of Ground Water from Private Domestic Wells. Water Well Journal. 2009 Apr;:33–37. [Google Scholar]
- Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2. New York: Wiley; 2000. [Google Scholar]
- George CM, Inauen J, Rahman MS, Zheng Y. The effectiveness of educational interventions to enhance the adoption of fee-based arsenic testing in Bangladesh: A cluster randomized controlled trial. American Journal of Tropical Medicine & Hygiene. 2013;89(1):138–144. doi: 10.4269/ajtmh.12-0664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hexemer AM, Pintar K, Bird TM, Zentner SE, Garcia HP, Pollari F. An investigation of bacteriological and chemical water quality and the barriers to private well water sampling in a Southwestern Ontario Community. Journal of Water and Health. 2008;6(4):521–525. doi: 10.2166/wh.2008.070. [DOI] [PubMed] [Google Scholar]
- Inauen J. Theory-based promotion of safe water consumption. University of Zurich; Zurich, Switzerland: 2012. [Google Scholar]
- Jones AQ, Dewey CE, Doré K, Majowicz SE, McEwen SA, Waltner-Toews D, Mathews E, Carr DJ, Henson SJ. Public perceptions of drinking water: a postal survey of residents with private water supplies. BMC Public Health. 2006;6(94) doi: 10.1186/1471-2458-6-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A, Adak P, Gurian PL, Lockwood JR. Arsenic exposure in US public and domestic drinking water supplies: A comparative risk assessment. J Expo Anal Environ Epidemiol. 2010;20:245–254. doi: 10.1038/jes.2009.24. [DOI] [PubMed] [Google Scholar]
- Mosler H-J. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: a conceptual model, a review, and a guideline. International Journal of Environmental Health Research. 2012;22(5):431–449. doi: 10.1080/09603123.2011.650156. [DOI] [PubMed] [Google Scholar]
- Nielsen MG, Lombard PJ, Schalk LF. US Geological Survey Scientific Investigations Report 2010–5199. 2010. Assessment of arsenic concentrations in domestic wells by town in Maine 2005–2009. [Google Scholar]
- NRC. Critical Aspect of Environmental Protection Agency's Integrated Risk Information System Assessment of Inorganic Arsenic: Interim Report. The National Academies Press; Washington DC: 2013. [Google Scholar]
- Ravenscroft P, Brammer H, Richards K. Arsenic Pollution: A Global Synthesis. John-Wiley & Sons; Oxford: 2009. [Google Scholar]
- Renaud J, Gagnon F, Michaud C, Boivin S. Evaluation of the effectiveness of arsenic screening promotion in private wells: a quasi-experimental study. Health Promotion International. 2011;26(4):465–476. doi: 10.1093/heapro/dar013. [DOI] [PubMed] [Google Scholar]
- Sandman PM, Weinstein ND. Predictors of home radon testing and implications for testing promotion programs. Health Education & Behavior. 1993;20(4):471–487. doi: 10.1177/109019819302000408. [DOI] [PubMed] [Google Scholar]
- Simpson H. Promoting the management and protection of private water wells. J Toxicol Environ Health A. 2004;67(20–22):1679–704. doi: 10.1080/15287390490492296. [DOI] [PubMed] [Google Scholar]
- Smith AH, Lingas EO, Rahman M. Contamination of drinking-water by arsenic in Bangladesh: a public health emergency. Bulletin of the World Health Organization. 2000;78(9) [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. American housing survey for the United States: 2009. 2009 Retrieved June 2013 from < http://www.census.gov/prod/2011pubs/h150-09.pdf>.
- U.S. Census Bureau. 2010 Census. 2010 < http://www.census.gov/2010census/data/>.
- Walker M, Shaw WD, Benson M. Arsenic consumption and health risk perceptions in a rural Western U.S. area. Journal of the American Water Resources Association. 2006;42(5):1363–1370. [Google Scholar]
- Wasserman GA, Liu X, LoIacono N, Kline J, Factor-Litvak P, van Geen A, Mey JL, Levy D, Abramson R, Schwartz A, Graziano JH. Exposure to arsenic from household wells and intelligence, in Maine schoolchildren. Environmental Health. doi: 10.1186/1476-069X-13-23. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND, Klotz ML, Sandman PM. Optimistic biases in public perceptions of the risk from radon. American Journal of Public Health. 1988;78(7):796–800. doi: 10.2105/ajph.78.7.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND, Sandman PM, Roberts NE. Determinants of self-protective behavior: Home radon testing. Journal of Applied Social Psychology. 1990;20(10):783–801. [Google Scholar]
- Yang Q, Jung HB, Culbertson CW, Marvinney RG, Loiselle MC, Locke DB, Cheek H, Thibodeau H, Zheng Y. Spatial Pattern of Groundwater Arsenic Occurrence and Association with Bedrock Geology in Greater Augusta, Maine. Environmental Science & Technology. 2009;43(8):2714–2719. doi: 10.1021/es803141m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Q. Arsenic in fractured bedrock aquifers in Greater Augusta, Maine, USA, Earth and Environmental Sciences. City University of New York; New York: 2010. [Google Scholar]
- Yang Q, Smitherman P, Hess CT, Culbertson CW, Marvinney RG, Smith AE, Zheng Y. Uranium and radon in private bedrock well water in Maine: Geospatial analysis at two scales. Environmental Science and Technology. 2014 doi: 10.1021/es405020k. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.