Highlights
-
•
Hydrocele of the canal of Nuck in the adult female is a rare condition.
-
•
Laparoscopic diagnosis is useful for groin mass connected with the retroperitoneal space.
-
•
TEP offers a useful alternative in selected patients with hydrocele of the canal of Nuck.
Keywords: Laparoscopy, The canal of Nuck, Hydrocele, TEP
Abstract
INTRODUCTION
Hydrocele of the canal of Nuck is a rarely encountered entity. We report a case underwent laparoscopic totally extraperitoneal (TEP) treatment for a hydrocele of the canal of Nuck extending in the extraperitoneal space mainly.
PRESENTATION OF CASE
A 37-year-old woman complained of painless and reducible swelling in her left groin, and referred to our hospital for surgical management against left inguinal hernia with the incarcerated ovary. Ultrasonography and MR images revealed a cystic mass in the retroperitoneal space, and we diagnosed as an unusual type of hydrocele of the canal of Nuck. The patient was scheduled for laparoscopic treatment. Laparoscopic findings on pneumoperitoneum showed an extraperitoneal cystic tumor with no contact with the left ovary. The fascia and peritoneum of the port site were closed, and then an extraperitoneal space was created. The cystic tumor with the round ligament of the uterus was dissected and resected by the TEP technique. The extended deep inguinal ring was repaired with polypropylene mesh. Postoperative course was uneventful.
DISCUSSION
Hydrocele of the canal of Nuck in the adult female is a rare condition. The accurate diagnosis of an inguinal hydrocele in a female is seldom made. Laparoscopic examination provides surgeons with information of inguinal swelling accompanied with retroperitoneal cyst, and consecutive treatment by laparoscopic technique, especially TEP, is useful in regard to minimal damage of the peritoneum.
CONCLUSION
Laparoscopic diagnosis and TEP treatment offers a useful alternative in selected patients with hydrocele of the canal of Nuck.
1. Introduction
In females, a peritoneal fold usually accompanies the round ligament of the uterus as it descends into the labium majus through the inguinal canal. This extension of the peritoneum obliterates into a fibrous cord by the first year of life.1 This is named the canal of Nuck, which is analogous to a patent processus vaginalis in the male. Failure of obliteration results in a communication with the peritoneal cavity through the canal of Nuck that manifests as an indirect hernia or a hydrocele. A hydrocele of the canal of Nuck is often misjudged as an incarcerated inguinal hernia followed by emergent surgery.2 Almost patients with hydrocele of the canal of Nuck have been treated by surgical excision using an anterior inguinal approach. We report a patient with hydrocele of the canal of Nuck who we diagnosed by laparoscopy and treated using a laparoscopic totally extraperitoneal (TEP) technique.
2. Presentation of case
A 37-year-old woman was referred to our department for a suspicious sliding inguinal hernia with left para-ovarian cyst. She had complained of reducible swelling in her left groin for 2 years. She noticed a slight increase in the size of the swelling after childbirth. There was no history of abdominal pain or bowel dysfunction. The palpable mass could be repositioned manually. Ultrasonographic examination revealed the mass to be hypoechoic and homogeneous without solid components. MRI showed a simple cystic lesion measuring 45 mm in its largest axis, which appeared to be in contact with the left ovary connected at its base with the parietal peritoneum (Fig. 1a and b). We diagnosed the mass as a hydrocele of the canal of Nuck and to treat the mass, we performed laparoscopic TEP excision of the hydrocele and repair of the inguinal hernia.
Fig. 1.
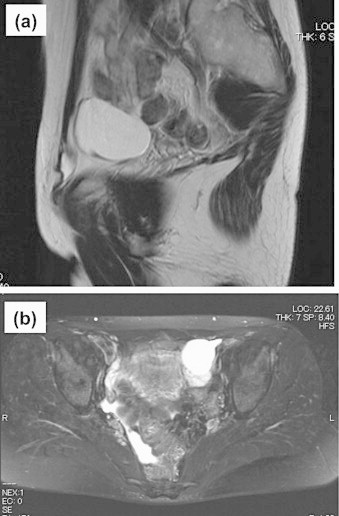
(a) Sagittal T2-weighted MR image showed that a fluid-intensity tumor led to the inguinal canal. (b) Enhanced T2-weighted MRI revealed no solid component within the cystic tumor in contact with the ovary.
An open-access method was performed to place a laparoscopic trocar into the umbilicus for carbon dioxide (CO2) pneumoperitoneum. Laparoscopic findings with the support of forceps from an accessory trocar into the right upper region showed an extraperitoneal cystic mass with no connection to the left ovary (Fig. 2). The uterus and adnexa were normal. After deflation, the posterior rectus sheath and peritoneum were closed, and then an extraperitoneal space was created through the same incision using a blunt balloon tip cannula and CO2 insufflation to maintain the operative field. Two additional trocars were placed through each lower midline region. The cystic mass was found to be present in the extraperitoneal space with communication to the left inguinal canal and was adhered to the round ligament of the uterus. All components of the wall of the cystic mass were pulled back from the deep inguinal ring into the extraperitoneal space. The distal side of the hydrocele was ligated with the round ligament and dissected. The extended deep inguinal ring was repaired with polypropylene three-dimensional mesh and a ProTack™ fixation device (Covidien, Mansfield, MA) to fix the mesh by the laparoscopic TEP approach. A dark-red serous fluid was aspirated from the cystic mass. The shrunken mass was dissected carefully and resected completely with the round ligament (Fig. 3a and b). Finally, inguinal repair was confirmed laparoscopically on pneumoperitoeum by insufflation of CO2 through an accessory intraabdominal trocar (Fig. 4). Pathological findings revealed that the resected wall of the hydrocele was lined with a single layer of mesothelial cells and consisted of fibrous components without solid components. The patient was discharged uneventfully on the 3rd postoperative day.
Fig. 2.

Laparoscopic findings showed an extraperitoneal cystic tumor (arrow) with no connection to the left ovary (arrowhead).
Fig. 3.
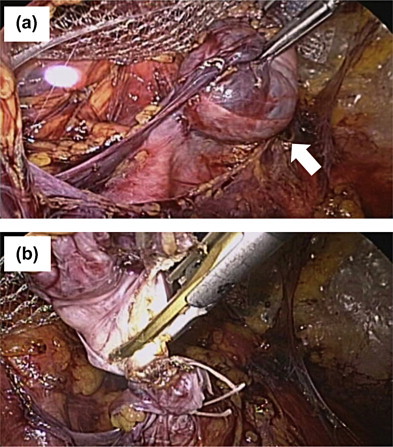
(a) Encysted tumor (arrow) was carefully dissected from the retroperitoneal space. (b) The aspirated hydrocele was ligated and resected with the round ligament completely.
Fig. 4.
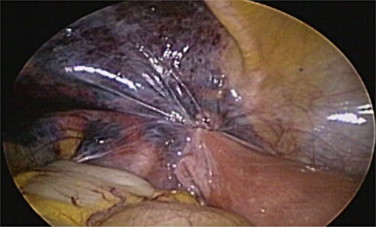
Inguinal repair was confirmed laparoscopically on pneumoperitoneum.
3. Discussion
The processus vaginalis in the female fetus usually closes and disappears long before birth. Evagination of the parietal peritoneum along with the round ligament of the uterus through the inguinal ring into the inguinal canal forms the canal of Nuck. Although complete obliteration of the canal of Nuck usually occurs,1 partial patency with peritoneal communication, allowing only fluid collection, can result in a hydrocele of the canal of Nuck. The hydrocele may present as a painless and elastic soft swelling in the inguinal region and labium majus. If the hydrocele of the canal of Nuck communicates into the peritoneal space, it often mimics an inguinal hernia in female patients because of its changeable mass. Huang et al. reported that the incidence of the hydrocele of the canal of Nuck in child was 1% (6 cases of 580 inguinal hernia in child).3 But its incidence in adult female is unclear because of its rarity.
A hydrocele of the canal of Nuck in the adult female is an unusual diagnosis. Because this entity is not mentioned widely, the diagnosis of an inguinal hydrocele in a female is seldom made on the basis of clinical findings alone. Most of the cases reported in the literature were diagnosed at surgery performed for suspicious inguinal hernia. Recently it was reported that high-resolution sonography can identify the nature of groin tumors.4,5 The differential diagnosis for an inguinal mass in a female includes indirect hernia, lymphadenopathy, cold abscess, Bartholin's cyst, and post-traumatic hematoma.6,7 A hydrocele of the canal of Nuck should also be considered in the differential diagnosis in adult females presenting with inguinal swelling. In the present case, laparoscopic examination was useful for the differential diagnosis from inguinal hernia.
There are three types of hydrocele of the canal of Nuck. The most common type has no communication with the peritoneal space and forms an encysted hydrocele along the round ligament, from the inguinal canal to the vulva. The second type results when there is a persistent communication with the peritoneal space. The third type is a combination of the first two resulting from the inguinal ring constricting the hydrocele like a belt so that one part is communicating and the other part is enclosed, thus giving the name “hour-glass” type.8 The present hydrocele had no communication with the peritoneal space, but it was located in the extraperitoneal space mainly, which was extremely rare.
The recommended treatment is excision of the hydrocele and closure of the enlarged inguinal ring. This is usually performed through the inguinal canal by an anterior approach. In the present case, the laparoscopic approach was useful for diagnosis and treatment. Laparoscopic repair for inguinal hernia uses mesh prosthesis to cover the defect from behind the abdominal wall. The most popular laparoscopic procedures are the transabdominal preperitoneal (TAPP) approach and the TEP approach. A randomized, multicentric trial showed that patients who underwent laparoscopic TEP recovered earlier and had fewer recurrences than those undergoing conventional anterior surgery.9 Laparoscopic closures of a patent canal of Nuck for indirect inguinal hernia in females have been reported.2 It had been reported that laparoscopic approach of the encysted hydrocele using TAPP method had its greater diagnostic potential and excision.10 To the best of our knowledge, this is the first report in the English literature of a procedure using the TEP technique to treat a hydrocele of the canal of Nuck extending in the extraperitoneal space. Use of the TEP approach can provide surgeons with information on the origin and type of hydrocele of the canal of Nuck. Furthermore, an incision of the peritoneum for excision of hydrocele, which would avoid the bowel adhesion, is not necessary.
Some patients with endometriosis in the inguinal region have been reported.11,12 The patent canal of Nuck supports the theory of retrograde implantation or movement of endometrial tissue into the inguinal canal.13,14 When a cystic mass contains inguinal endometriosis, it should be differentiated from hydrocele of the canal of Nuck. If swelling in the inguinal region and labium majus is recognized in the adult female, fine-needle aspiration can be helpful to assist in making an accurate diagnosis. However, care must be taken when performing aspiration alleviating symptoms because aspiration may lead to cellular dissemination and subsequent growth.
4. Conclusion
Laparoscopic diagnosis and TEP approach with its advantage of a shorter recovery period could be useful in treating the patient with hydrocele of the canal of Nuck, such as extending in the extraperitoneal space.
Conflict of interest
The authors declare no conflict of interest.
Funding
None.
Ethical approval
This paper is not research study but a case report which do not require ethical approval.
Author Contributions
Toshifumi Matsumoto contributed to the writing of this paper.
Teijiro Hirashita with the corresponding author performed Lap TEP.
Takao Hara, Nobuhide Kubo, and Shoji Hiroshige were involved in collecting images and histopathological material, and reviewing the literature.
Hiroyuki Orita was involved in critically revising the manuscript.
All authors read and approved the final paper.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on requests.
References
- 1.Park S.J., Lee H.K., Hong H.S., Kim H.C., Kim D.H., Park J.S. Hydrocele of the canal of Nuck in a girl: ultrasound and MR appearance. Br J Radiol. 2004;77:243–244. doi: 10.1259/bjr/51474597. [DOI] [PubMed] [Google Scholar]
- 2.Yen C.F., Wang C.J., Lin S.L., Chang P.C., Lee C.L., Soong Y.K. Laparoscopic closure of patent canal of Nuck for female indirect inguinal hernia. J Am Assoc Gynecol Laparosc. 2001;8:143–146. doi: 10.1016/s1074-3804(05)60564-6. [DOI] [PubMed] [Google Scholar]
- 3.Huang C.S., Luo C.C., Chao H.C., Chu S.M., Yu Y.J., Yen J.B. The presentation of asymptomatic palpable movable mass in female inguinal hernia. Eur J Pediatr. 2003;162:493–495. doi: 10.1007/s00431-003-1226-7. [DOI] [PubMed] [Google Scholar]
- 4.Anderson C.C., Broadie T.A., Mackey J.E., Kopecky K.K. Hydrocele of the canal of Nuck: ultrasound appearance. Am Surg. 1995;61:959–961. [PubMed] [Google Scholar]
- 5.Jagdale R., Agrawal S., Chhabra S., Jewan S.Y. Hydrocele of the canal of Nuck: value of radiological diagnosis. J Radiol Case Rep. 2012;6:18–22. doi: 10.3941/jrcr.v6i6.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Block R.E. Hydrocele of the canal of Nuck: a report of five cases. Obstet Gynecol. 1975;45:464–466. [PubMed] [Google Scholar]
- 7.Schneider C.A., Festa S., Spillert C.R., Bruce C.J., Lazaro E.J. Hydrocele of the canal of Nuck. NJ Med. 1994;91:37–38. [PubMed] [Google Scholar]
- 8.Counseller V.S., Black B.M. Hydrocele of the canal of Nuck: report of seventeen cases. Ann Surg. 1941;113:625–630. doi: 10.1097/00000658-194104000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liem M.S., van der Graaf Y., van Steensel C.J., Boelhouwer R.U., Clevers G.J., Meijer W.S. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med. 1997;336:1541–1547. doi: 10.1056/NEJM199705293362201. [DOI] [PubMed] [Google Scholar]
- 10.Bunting D., Szczebiot L., Cota A. Laparoscopic hernia repair – when is a hernia not a hernia. JSLS. 2013;17:654–656. doi: 10.4293/108680813X13794522667481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bagul A., Jones S., Dundas S., Aly E.H. Endometriosis in the canal of Nuck hydrocele: an unusual presentation. Int J Surg Case Rep. 2011;2:288–289. doi: 10.1016/j.ijscr.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mesko J.D., Gates H., McDonald T.W., Youmans R., Lewis J. Clear cell (mesonephroid) adenocarcinoma of the vulva arising in endometriosis: a case report. Gynecol Oncol. 1988;29:385–391. doi: 10.1016/0090-8258(88)90241-7. [DOI] [PubMed] [Google Scholar]
- 13.Shadbolt C.L., Heinze S.B., Dietrich R.B. Imaging of the groin masses: inguinal anatomy and pathologic conditions revisted. Radiographics. 2001;21:S261–S271. doi: 10.1148/radiographics.21.suppl_1.g01oc17s261. [DOI] [PubMed] [Google Scholar]
- 14.Gaeta M., Minutoli F., Mileto A., Racchiusa S., Donato R., Bottari A. Nuck canal endometriosis: MR imaging findings and clinical features. Abdom Imaging. 2010;35:737–741. doi: 10.1007/s00261-010-9607-7. [DOI] [PubMed] [Google Scholar]


