Abstract
INTRODUCTION
Defined as heterotrophic autotransplantation of splenic tissue after splenic trauma or surgery.
PRESENTATION OF CASE
We present a case of 45 years old female patient with past history of splenectomy for haemolyticanaemia. Complaining of abdominal pain the patient was investigated by abdominal CT scan which revealed a focal lesion in the left lateral section of the liver suspicious to be hepatocellular carcinoma and gall bladder stones. Serum α-fetoprotein was within normal range. Exploration revealed a well encapsulated lesion completely separable from the liver and the diaphragm. Histopathological examination confirmed the diagnosis of splenosis. Although it is a rare condition, we recommend that the diagnosis of splenosis should be put in consideration in every patient with past history of splenectomy for proper management.
DISCUSSION
Although several cases of hepatic splenosis have been reported in the literature, supra-hepatic splenosis as our case has been rarely described.
CONCLUSION
Considering patients past history of splenectomy or splenic trauma should add splenosis to the list of possible differential diagnosis to avoid unnecessary surgical intervention.
Keywords: Splenosis, Suprahepatic
1. Introduction
Defined as heterotrophic autotransplantation of splenic tissue after splenic trauma or surgery, splenosis is now considered more common that once it was thought to be.1 We present a case of splenosis on the diaphragmatic surface of the left lateral section of the liver in a patient with a 20 years history of splenectomy which may explain the seedling of the splenic tissue on the surface of the left liver. As in most cases of reported hepatic splenosis, we miss-interpreted it as hepatocellular carcinoma. Thus, awareness of the possibility of splenosis in patients with history of splenic trauma or splenectomy may help to avoid unnecessary surgical exploration.
2. Case report
A 45-years-old diabetic female patient presented to our outpatient clinic with 8 months history of dull aching abdominal pain. She had a past history of open splenectomy 20 years ago through a left para-median incision for haemolytic anaemia.
Triphasic abdominal CT scan revealed hepatic focal lesion 5 cm × 4 cm in the left lateral section of the liver with significant contrast enhancement in the arterial phase with washout in the portal and delayed phases suggestive of hepatocellular carcinoma and multiple gall bladder stones (Fig. 1).
Fig. 1.
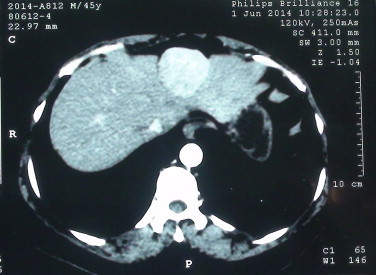
Abdominal CT scan revealed hepatic focal lesion in the left lateral section of the liver with contrast enhancement in the arterial phase suggestive of hepatocellular carcinoma.
The liver function tests revealed a serum albumin level of 3.8 g/dl (normal range 3.5–5.5 g/dl), a serum bilirubin level of 0.5 mg/dl (normal range of 0.1–1.1 mg/dl), serum alanine aminotransferase level of 20 U/ml (normal range up to 45 U/ml), International normalized ratio of 1.1 and blood picture was normal. The α-fetoprotein was 10.5 ng/ml (normal range less than 15 ng/ml). The patient was hepatitis C virus positive.
The patient underwent laparotomy through a J shaped incision. Exploration revealed healthy liver with a well encapsulated mass 5 cm in diameter between the left lateral section of the liver and the diaphragm and completely separable from both. Excision of the mass was done together with cholecystectomy (Fig. 2a and b).
Fig. 2.
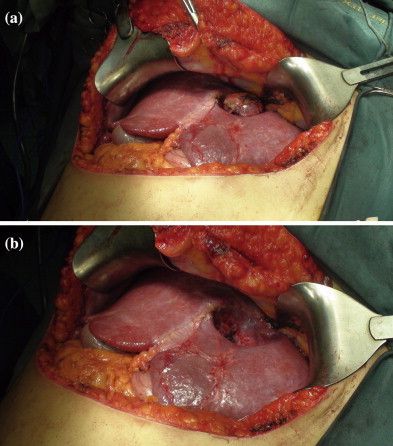
(a) Operative photo of the mass after dissection of its adhesions from the diaphragm. (b) Operative photo after excision of the lesion showing intact liver capsule in the depression made by the lesion on the diaphragmatic surface of the liver.
Post-operative pathological examination of the specimen revealed normal splenic tissue with fibrous capsule (Fig. 3).
Fig. 3.
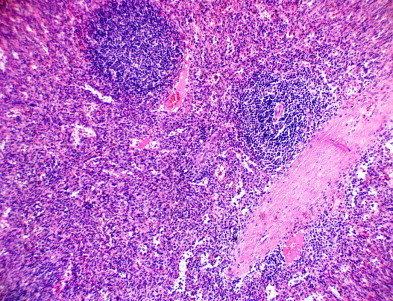
Picture showing Splenic tissue with thick capsule, H&E staining, 200×.
3. Discussion
The first case of splenosis was reported in the English literature in 1939 by Buchbinder and Lipkoff.2 Although it is believed to occur in up to 67% of cases with splenic trauma the true incidence cannot be estimated as it is usually an incidental finding during surgical exploration or autopsy.3
Splenosis should be distinguished from accessory spleen. Accessory spleens are usually located near the normal spleen in the area of the gastro-splenic and pancreatico-splenic ligaments. They usually receive blood supply from the splenic artery and histologically resemble the normal spleen with a hilus, normal pulp and splenic capsule. In contrast splenotic implants have no hilum and receive blood supply from nearby arteries at the site of implantation.4 Splenotic implants are commonly located on the serosal surface of the bowel, the mesentery, the parietal peritoneum and less commonly in the para-colic gutters, the appendix and the subcutaneous tissues of the left hemi-abdomen.5
Although several cases of hepatic splenosis have been reported in the literature, supra-hepatic splenosis as our case has been rarely described.6
In conclusion, considering patients past history of splenectomy or splenic trauma should add splenosis to the list of possible differential diagnosis to avoid unnecessary surgical intervention.
Conflict of interest
None declared.
Funding
None declared.
Ethical approval
This work was approved by the ethical committee of gastroenterology surgical center.
Author contributions
Tharwat Kandil: study concept and design, Mohamed El Sorogy, Youssif Naiem, Wagdi Elkashef: data collection and analysis, Mohamed El Sorogy: writing the paper, and Tharwat Kandil: Revision before final approval for publication.
References
- 1.Fleming C.R., Dickson E.R., Harrison E.G. Splenosis: autotransplantation of splenic tissue. Am J Med. 1976;61:414–419. doi: 10.1016/0002-9343(76)90380-6. [DOI] [PubMed] [Google Scholar]
- 2.Buchbinder J.H., Lipkoff C.J. Splenosis: multiple peritoneal splenic implant following abdominal injury. Surgery. 1939;6:927–934. [Google Scholar]
- 3.Vuysere S.D., Steenbergen W.V., Aerts R., Hauwaert H.V., Beckevoort D.V., Hoe L.V. Intrahepatic splenosis: imaging features. Abdom Imaging. 2000;25:187–189. doi: 10.1007/s002619910042. [DOI] [PubMed] [Google Scholar]
- 4.Gruen D.R., Gollub M.J. Intrahepatic splenosis mimicking hepatic adenoma. Am J Roentgenol. 1997;168:725–726. doi: 10.2214/ajr.168.3.9057523. [DOI] [PubMed] [Google Scholar]
- 5.Di Costanzo G.G., Picciotto F.P., Marsilia G.M., Ascione A. Hepatic splenosis misinterpreted as Hepatocellular carcinoma in cirrhotic patients referred for liver transplantation: report of two cases. Liver Transplant. 2004;10:706–709. doi: 10.1002/lt.20162. [DOI] [PubMed] [Google Scholar]
- 6.Kim K.A., Park C.M., Kim C.H., Choi S.Y., Park S.W., Kang E.Y. An interesting hepatic mass: splenosis mimicking a hepatocellular carcinoma. Eur Radiol. 2003;13:2713–2715. doi: 10.1007/s00330-003-1978-5. [DOI] [PubMed] [Google Scholar]


