Abstract
Objective
Considering that periodontal ligament simulation may influence the stress distribution over teeth restored with intraradicular retainers, this study aimed to assess the combined effect of mechanical cycling and periodontal ligament simulation on both the bond strength between fiber posts and root dentin and the fracture resistance of teeth restored using glass fiber posts.
Material and Methods
Ninety roots were randomly distributed into 3 groups (n=10) (C-MC: control; P-MC: polyether; AS-MC: addition silicone) to test bond strength and 6 groups (n=10) (C: control; P: polyether; AS: addition silicone, without mechanical cycling, and C-MC, P-MC and AS-MC with mechanical cycling) to test fracture strength, according to the material used to simulate the periodontal ligament. For the bond strength test, fiber posts were cemented, cores were built, mechanical cycling was applied (2×106 cycles, 88 N, 2.2 Hz, and 45º incline), and the teeth cut into 3 slices (2 mm), which were then subjected to the push-out test at 1 mm/min. For the fracture strength test, fiber posts were cemented, cores were built, and half of the groups received mechanical cycling, followed by the compressive strength (45° to the long axis and 1 mm/min) performed on all groups.
Results
Periodontal ligament simulation did not affect the bond strength (p=0.244) between post and dentin. Simulation of periodontal ligament (p=0.153) and application of mechanical cycling (p=0.97) did not affect fracture resistance.
Conclusions
The materials used to simulate the periodontal ligament did not affect fracture or bond strength, therefore periodontal ligament simulation using the tested materials could be considered optional in the conditions of the study.
Keywords: Dental pins, Fatigue, Compressive strength, Dental bonding
INTRODUCTION
For the reconstruction of endodontically treated teeth, intraradicular posts are recommended to retain the restoration when there is less than 50% of the coronal structure remaining21. Among other intraradicular anchorage options, adhesively cemented fiber posts reduce the risk of root fracture because they have an elastic modulus (E=40 GPa) similar to dentin (E=18 GPa), unlike ceramic (E=200 GPa) and metallic posts (E=200 GPa)6,17. Consequently, fiber posts provide more uniform stress distribution on root dentin compared to other retainers6,13.
The clinical success of restorative treatments depends on many factors, including the amount of dental substrate7, adequate coronal reconstruction7, cavity configuration factor19, masticatory load support by the teeth and stress distribution over the bone and periodontal ligament26. The periodontal ligament, ranging between 0.1 and 0.3 mm thick16 , absorbs occlusal loads; the periodontal fiber compression provides important support when the tooth is submitted to external forces24. When a force is applied, the resistance of the periodontal membrane is initially low, but as the load increases, the resistance also increases gradually until tooth dislodgment becomes minimal. The periodontal ligament is compressive to a limited extent and partially elastic24,26. For masticatory loads up to 70 N, the periodontal ligament compresses to approximately 0.03-0.15 mm25. When the fibers reach their maximum load resistance, the periodontal ligament becomes rigid, the load is transmitted to the bone, and tensions are distributed over the root surface26.
Therefore, the properties of masticatory force absorption through the bone and periodontal ligament should be reproduced in laboratorial tests in order to simulate the clinical reality more accurately26. However, various studies that assess bond strength between root canal posts and dentin after mechanical fatigue do not simulate periodontal ligament3,8. Similarly, most studies fail to simulate the periodontal ligament in fracture resistance tests5,18, although a few studies simulate the periodontal ligament using polyether11,13 and polivynilsiloxane based elastomers7,22.
A few in vitro studies assessed the effects of periodontal ligament simulation and showed that an artificial periodontal ligament reduced the fracture strength and modified the failure modes of sound in bovine teeth26. Also, simulating the periodontal ligament significantly reduced fracture resistance of ceramic-fixed partial dentures25.
Considering that root posts reduce the area available for stress distribution, concentrating it on the remaining dental structure and the dentin-post interface14, periodontal ligament simulation may interfere in stress distribution. Therefore, the objectives of the present study were to characterize the influence of different artificial periodontal ligament materials on fiber post-root dentin bond strength after mechanical cycling, and to evaluate the effect of periodontal ligament simulation on fracture resistance of teeth restored with glass fiber posts, both with and without simultaneous mechanical cycling. Two hypotheses were tested: 1) a simulated periodontal ligament under mechanical cycling would not affect bond strength, and 2) periodontal ligament simulation would not affect fracture resistance.
MATERIAL AND METHODS
Specimen selection and adequacy
Ninety single-root bovine teeth were cleansed with periodontal curettes and stored in distilled water. Coronal portions were sectioned under water cooling to obtain a standardized 16 mm root length. The most coronal diameter of the root canal was measured with a digital caliper (Starrett 727, Starret, Itu, SP, Brazil), and any tooth with a canal diameter larger than the fiber post diameter (Φ=1.8 mm, White Post #3, FGM, Joinville, SC, Brazil) was discarded and replaced with a different specimen.
The apical foramens were sealed using a photo activated adhesive (Single Bond 2, 3M ESPE, Saint Paul, MN, USA) associated with a composite resin (Oppalis, FGM). The canals were prepared with the same drill used in the posts system (White Post DC #3, FGM) to a 12 mm length.
Experimental design: root embedment and periodontal ligament simulation
The roots were numbered from 1 to 90 and randomly distributed into 6 groups (n=15), which varied by the artificial periodontal ligament composition and the test performed (Figure 1). The number sequences were generated by Random Allocation Software (developed by M. Saghaei, Isfahan University of Medical Sciences, Isfahan, Iran).
Figure 1.
Experimental design
| Groups | |||||
|---|---|---|---|---|---|
| Test | Periodontal ligament simulation | Mechanical cycling (MC) | |||
| No | |||||
| Fracture resistance | Control | C-MC | C | ||
| Addition silicone | AS-MC | AS | |||
| Push out bond strength | Control | C-MC | --- | ||
| Addition silicone | AS-MC | --- | |||
The surfaces of 60 roots were covered with baseplate wax (Lysanda, São Paulo, SP, Brazil) that was liquefied at 60°C. To simulate the biological space, each root was immersed in wax for 2 seconds up to 3 mm below the most coronal portion of the root, which created an approximately 0.3 mm thick wax layer, considered adequate in prior literature10,26. The thickness of the wax layer was confirmed by measuring the thickness of the root with a digital caliper before and after immersion.
All 90 roots were embedded in PVC cylinders (height: 14 mm; diameter: 25 mm) as described in other study4. The bur used to prepare the conduits was positioned inside the canal, and while supporting the root, attached to a surveyor. Consequently, the long axes of the bur, the root, and the cylinder were parallel to each other and perpendicular to the horizontal axis. Self-curing acrylic resin Dencrilay (Dencril, Caieiras, SP, Brazil) was mixed at 3:1 (powder:liquid) and poured inside the PVC cylinder. The most coronal 3 mm section of the root was exposed to simulate the bone limit.
After resin polymerization, the teeth covered bywax were separated from the cylinders, and the wax was removed from the root surface and acrylic resin interior using hot water and manual instruments.
Thirty roots had periodontal ligament simulated with polyether (Impregum Soft Medium Body, 3M ESPE) and 30 roots with addition silicone (Express Medium Body, 3M ESPE), according to the randomization. To create the artificial periodontal ligament, the corresponding elastomeric material was inserted along the artificial alveolus created on the acrylic resin. Then, the root was repositioned into the alveolar space and the elastomer polymerized; the elastomer in excess was then removed using a scalpel blade.
Posts cementation
The glass fiber posts were sectioned to a length of 17 mm (5 mm coronal portion and 12 mm intracanal portion). Each post was cleansed with 70% ethanol; silane coupling agent (Prosil, FGM) was applied onto the surface using a microbrush (Cavibrush, FGM), and the posts were left undisturbed for 5 minutes, according to the recommendations of the manufacturer.
The root canals were conditioned with 37% phosphoric acid (Condac 37, FGM) for 15 seconds and washed with 10 mL of distilled water. Excess water was removed with absorbent paper points (Tanari, Manacapuru, AM, Brazil). The activator of the adhesive system (Adper Scotchbond Multipurpose, 3M ESPE) was applied into the canal using a microbrush (Cavibrush, FGM); the excess material was removed with paper points (Tanari) and put to dry for 5 seconds. The adhesive system Primer and Catalyst were applied in a similar manner. Then, the resin cement RelyX ARC (3M ESPE) was applied on the post with a spatula and in the root canal with a Lentulo drill #40 (Injecta, Diadema, SP, Brazil). The posts were positioned inside the root canal, the cement in excess was removed, and photo-activation was performed for 40 seconds on the occlusal surface with a LED (Radii-Cal, SDI, Melbourne, Vic, Australia).
After the posts were cemented, the crown was reconstructed. The coronal dentin was etched with 37% phosphoric acid (Condac 37, FGM) for 15 seconds, washed with 10 mL of distilled water, and the excess removed with absorbent paper. The adhesive system (Single Bond 2, 3M ESPE) was applied using a microbrush (Cavibrush, FGM); the core was built up with composite resin (Oppallis, FGM) using matrices at standardized dimensions and anatomical confguration of an upper central incisor prepared for a full crown. The specimens were stored in distilled water at 37°C for 24 hours.
Push-out bond strength test
The groups (n=10) were divided according to the artificial periodontal ligament composition (Figure 1). All the specimens were immersed in distilled water at 37°C and submitted to 2×106 cycles in a mechanical fatigue simulator (ER 11000, Erios, São Paulo, SP, Brazil), which is equivalent to 2 years of clinical service30 at an 88 N load, 2.2 Hz frequency and 45° incline from the horizontal axis. Twenty-four hours after the mechanical cycling was fnished, the specimens were fixed on the metallic base of a cutting machine (LabCut 1010, Extec Corp., Enfeld, CT, USA) and sectioned perpendicularly to the root long axis. The first slice of approximately 1 mm was discarded, and 3 slices (2 mm) were obtained from each tooth. Each slice was positioned with the most coronal portion downward on a metallic device while a cylinder applied a load on the post directed from the apical to the coronal portion at a crosshead speed of 1 mm/min (Emic DL 2000, Emic, São José dos Pinhais, PR, Brazil).
The height and canal diameters of the coronal and apical portions were measured with a digital caliper. The bond strength (MPa) was calculated using the formula R=F/A, where F was the force of rupture (N), and A was the bonded area. The bonded area was calculated using the formula to determine the lateral area of a circular straight cone with parallel bases: A=πg.(R1+R2), where π=3.14, g=slant height, R1=smaller base radius, and R2=larger base radius. To determine the slant height, the following formula was used: g2=h2+(R2-R1)2, where h=specimen thickness and R1 and R2 were the internal diameters of the smaller and larger bases, respectively, divided by 2.
Afterwards, the specimens were examined under a Stereo Discovery V20 optical microscope (Carl Zeiss, Gbttingen, NSAC, Germany) up to 40x to determine the predominant failure pattern. Failures were classified as: adhesive failure between dentin and cement (Ad DC); adhesive failure between cement and post (Ad CP); cohesive failure of the dentin (Co D); cohesive failure of the cement (Co C); cohesive failure of the post (Co P); mixed adhesive failure of dentin/adhesive failure between post and cement (M Ad DC/PC); and mixed adhesive/cohesive failure (M Ad/Co).
Specimens with representative failures were analyzed using scanning electron microscopy (JEOLJSM-5400, Jeol, Tachikawa, TY, Japan).
Fracture resistance test
The groups (n=10) were divided according to the periodontal ligament composition and application of mechanical cycling (Figure 1). Specimens of groups C-MC, P-MC and AS-MC were submitted to mechanical cycling according to the same protocol used for the push-out test. The specimens that were not mechanically cycled were stored in distilled water at a temperature of 37°C during the same time period of the mechanical cycling.
Twenty-four hours after the mechanical cycling was fnished, all specimens of each group were submitted to a compressive strength test in a universal testing machine (Emic DL 2000, Emic). Each specimen was positioned on the device aligned at 45° to the tooth long axis, and a constant static load was applied at a crosshead speed of 1 mm/min until failure. Failure was defned as the point when the load (N) reached its maximum value during the test.
The failure modes were classified as favorable and unfavorable under an optical microscope (Stereo Discovery V20, Carl Zeiss). Fractures at or above the simulated bone level, fractures of the coronal portion of the core, and dislodgement of the core and/or post coronal portion were considered favorable failures. Vertical or oblique radicular fractures below the simulated bone level were classified as unfavorable failures.
Statistical analysis
Normal distribution and homoscedasticity were verified with Shapiro-Wilk and Levene tests. Bond strength values were analyzed by one-way ANOVA, with periodontal ligament material as the variable, and fracture strength values were analyzed by two-way ANOVA, with the periodontal ligament composition and application of mechanical cycling as variables. In both cases, the significance level was 5%.
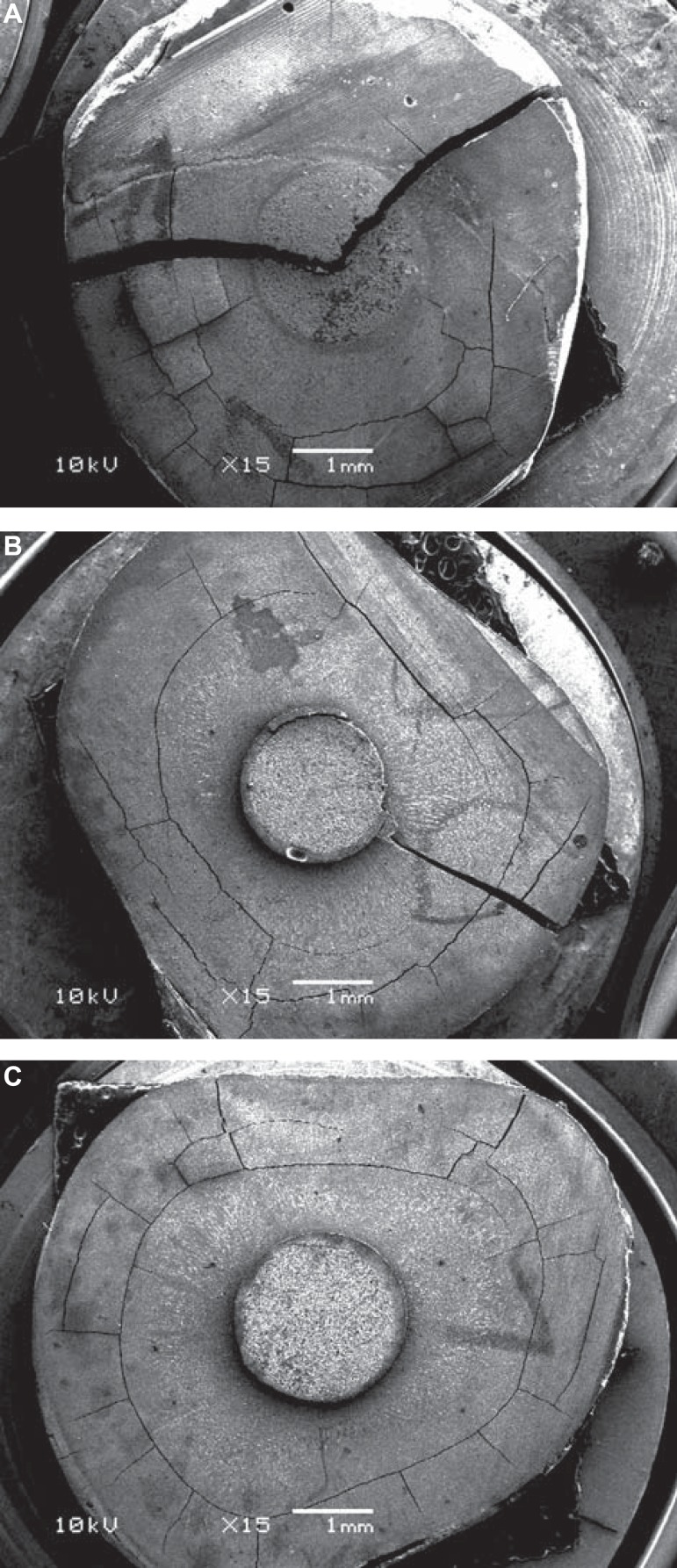
Cohesive (Figure 2A) or mixed adhesive/cohesive (Figure 2B) failure slices were excluded from the bond strength statistical analysis because they did not represent adhesive failures.
Figure 2.
Scanning electron microscopy images. (A) Cohesive failure in dentine. (B) Mixed adhesive/cohesive failure. (C) Adhesive failure between dentin and cement
RESULTS
There was no root fracture or restoration failure during the mechanical cycling.
Push-out bond strength test
Table 1 summarizes the bond strength means and standard deviations. One-way ANOVA revealed that the periodontal ligament simulation did not affect the bond strength (p=0.244). Most of the failures were adhesive and occurred between the dentin and resin cement (Figure 2C), followed by adhesive failures between the post and resin cement (Table 2).
Table 1.
Push-out bond strength (MPa) means ± standard deviations
| Group* | Mean ± SD |
|---|---|
| C | 10.82±2.93 |
| P | 13.06±2.38 |
| AS | 11.07±3.23 |
C: Control; P: Polyether; AS: Addition Silicone
Table 2.
Distribution of failure modes after the push-out test
| Failure mode** | |||||||
|---|---|---|---|---|---|---|---|
| Group* | Ad DC | Ad CP | Co D | Co C | Co P | M Ad DC/PC | M Ad/Co |
| C-MC | 35 | 1 | 2 | - | - | 1 | - |
| P-MC | 30 | 6 | - | - | - | 1 | 2 |
| AS-MC | 31 | 4 | - | - | - | 3 | - |
| Total | 96 (83%) | 11 (9%) | 2 (2%) | 0 | 0 | 5 (4%) | 2 (2%) |
All groups were submitted to mechanical cycling.
Ad DC: adhesive failure between dentin and resin cement;
Ad CP: adhesive failure between dentin and fiber post; Co D: cohesive failure of dentin; Co P: cohesive failure of fiber post; M Ad DC/PC: mixed failure with adhesive failure between dentin/resin cement and fiber post/resin cement; M Ad/Co: mixed failure with adhesive and cohesive failures
Fracture resistance test
Means and standard deviations are presented in Table 3. Two-way ANOVA showed that the simulation of the periodontal ligament (p=0.153), the mechanical cycling (p=0.97), and the interaction between the two factors (p=0.665) did not significantly affect fracture resistance. Favorable failures were predominant among other failure modes (Table 4).
Table 3.
Means ± standard deviation of the fracture load (N) data
| Group* | Mechanical cycling | Mean±SD |
|---|---|---|
| CP | No | 415.20±121.70 |
| P | 327.16±51.40 | |
| AS | 367.18±94.27 | |
| C-MC | Yes | 381.76±110.20 |
| P-MC | 346.69±51.08 | |
| AS-MC | 378.21±134.35 |
C, P and AS were not mechanically cycled; C: control; P: polyether; AS: addition silicone; C-MC: control submitted to mechanical cycling; P-MC: polyether submitted to mechanical cycling; AS-MC: addition silicone submitted to mechanical cycling
Table 4.
Qualitative analysis of failure patterns after the fracture resistance test
| Groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Without mechanical cycling | With mechanical cycling | ||||||||
| C | P | AS | C-MC | P-MC | AS-MC | Total | % | ||
| Failure | Favorable | 6 | 8 | 9 | 10 | 10 | 10 | 53 | 88 |
| pattern | Unfavorable | 4 | 2 | 1 | - | - | - | 7 | 12 |
| Failure place | Core fracture | 9 | 8 | 9 | 10 | 10 | 10 | 56 | |
| Post fracture* | - | - | - | - | - | - | |||
| Root fracture | 4 | 2 | 1 | - | - | - | 7 | ||
| Failure | Mesiodistal | 10 | 10 | 10 | 10 | 7 | 9 | 56 | 93 |
| direction | Buccolingual | - | - | - | - | 3 | 1 | 4 | 7 |
No post fracture was observed, however, a mesiodistal crack was observed in the posts of several specimens (Figure 4) C: control; P: polyether; AS: addition silicone
DISCUSSION
Periodontal ligament simulation may enable a more accurate in vitro reproduction of the oral environment26. In the present study, polyether and addition silicone artificially reproduced the periodontal ligament during mechanical fatigue, after the bond strength between the post and dentin was assessed, as well as the fracture resistance of bovine teeth restored using glass fiber posts, both with and without mechanical cycling.
Due to the difficulty of obtaining intact single-rooted human teeth and the ethical aspects implicated in their use for research, bovine teeth were used as substitutes for human teeth. Bovine and human teeth have macro and microscopic structural similarities, and for that reason bovine teeth have been suggested as a possible alternative12. Previous laboratorial studies also used bovine teeth as a substitute for human teeth3-5,8,18.
The results of the present study showed similar bond strength among the three groups during the push-out test, and thus, the first null hypothesis was accepted. The intraradicular retainers used in the current study were glass fiber posts, which, based on fnite element analysis, generated stress distribution on the root similar to non-restored teeth, as a consequence of its elastic modulus14,17. Based on those studies, the lack of differences between the tested groups may result from a tendency towards homogeneous force distribution during mechanical cycling, reducing stress applied on the post/dentin interface so that the load absorbed by the periodontal ligament may not have been relevant in the study conditions. By contrast, when metallic or ceramic intraradicular posts are used, concentrated tension zones are created because the reconstruction material is more rigid than dentin6,17. The present results may have been different if metallic or ceramic posts were used instead.
In endodontically treated teeth restored with posts, shear forces are present in the central region of the specimens, which can lead to adhesive failure at the dentin/post interface29. Although the finding was not statistically significant, the group lacking an artificial periodontal ligament simulation had lower bond strength than the other groups. If a higher number of cycles had been applied on the specimens during aging, perhaps a significant reduction of the bond strength could have been induced.
The push-out test generated predominantly adhesive failures at the dentin/cement interface, similarly to previous studies3,8,9,15,19. That failure pattern is probably due to the high C factor inside the canal and the difficulty visualizing and controlling the moisture of the radicular dentin15,19. Furthermore, 9% of adhesive failures between cement and post may have been caused by the strong adhesion between dentin and cement promoted by the three-step total-etch adhesive system3.
The second null hypothesis was also accepted because there was no statistical difference between the groups in fracture resistance regardless of mechanical cycling. This result contrasts with those of a previous study26 that observed a significant difference between the groups with and without a periodontal ligament after fracture strength testing; however, the study did not perform mechanical cycling, and intact bovine teeth were used, which have longer and more voluminous crowns than the specimens utilized in the present study.
Bearing in mind the aforementioned finite elements analysis studies14,17, this finding may be associated with the primarily uniform stress distribution on teeth restored with glass fiber posts. When fiber posts are used, stress concentration is lower compared to rigid retainers6, and thus, the cushioning effect provided by the impression material did not alter fracture resistance. However, if metallic or ceramic posts are used, high stress concentration is generated on the root portion due to the rigidity of the material6. Although the present study did not evaluate those intraradicular retainers, it is speculated that the periodontal ligament simulation may modify stress distribution during mechanical cycling and fracture resistance test if rigid posts are used. More studies must be performed investigating the influence of periodontal ligament simulation on fracture strength of teeth restored with rigid posts and also comparing different post systems.
The absence of difference between experimental and control groups may also be, in part, due to the design of the fracture resistance test. During the test, a load is increasingly applied by an indenter until the restoration fails, which compresses the artificial periodontal ligament between two solid structures. As the elastomer is compressed beyond its elastic limit, its cushioning function is lost1, and the load applied by the piston only has effect on the specimen after the elastomer is completely “squeezed” between the specimen and the acrylic resin.
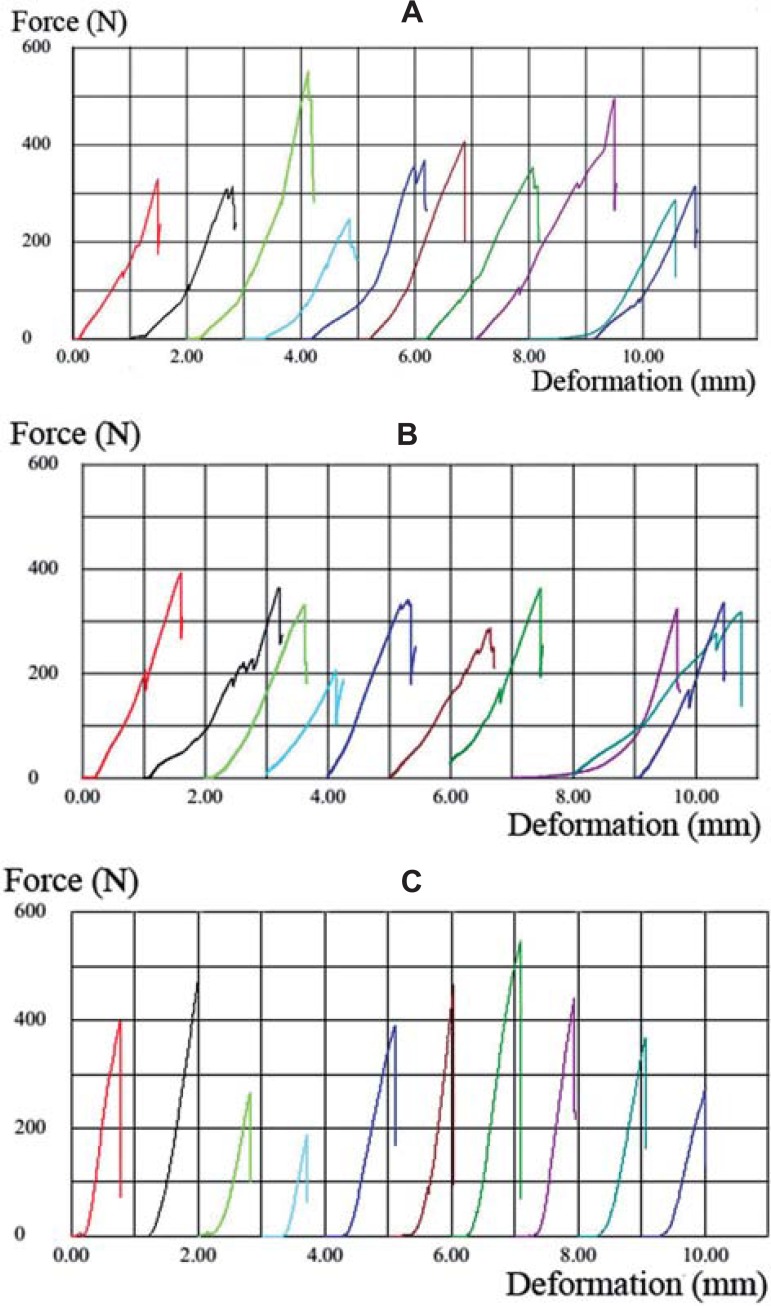
Figure 3 shows the relation between the force applied and the deformation through graphics of fracture resistance tests for groups AS, P, and C, generated by the universal testing machine. Graphics of groups AS (Figure 3A) and P (Figure 3B) present premature peaks before failure threshold, which do not indicate fracture, but an accommodation of the specimen in the artificial alveolus by the simulated periodontal ligament. This phenomenon does not occur in the specimens of the group C (Figure 3C), where the only peak illustrated is specimen fracture. Therefore, studies of fracture resistance tests simulating periodontal ligament require attention from the operator to obtain the real value of the fracture.
Figure 3.
Graphics of groups addition silicone (A), polyether (B), and control (C) illustrating the force (N) and deformation (mm) of each specimen during the fracture strength test. In the groups with an artificial periodontal ligament, the specimens are accommodated when a load is applied. This is not observed in group C because of the rigidity of the acrylic resin, and the graphic is a crescent line until the failure threshold of the restorative assembly is reached
Mechanical cycling did not affect fracture resistance in any group. Presumably, the protocol used to mechanically cycle the specimens was not sufficient to decrease fracture resistance. These results are in accordance with other studies18,22 that also did not find a difference in the fracture resistance of teeth restored with fiber posts before and after mechanical aging.
The failures occurring in the fracture strength test were mainly favorable (88%) and likely related to the glass fiber posts and composite resin, which have rigidity similar to that of dentin and provide a relatively uniform stress distribution to the root6. In addition, the adhesion between the post and restorative materials (adhesive, cement and composite resin) of similar properties tends to generate a homogeneous stress distribution17. Other studies performed in similar conditions also found mostly favorable failures5,13,22,29.
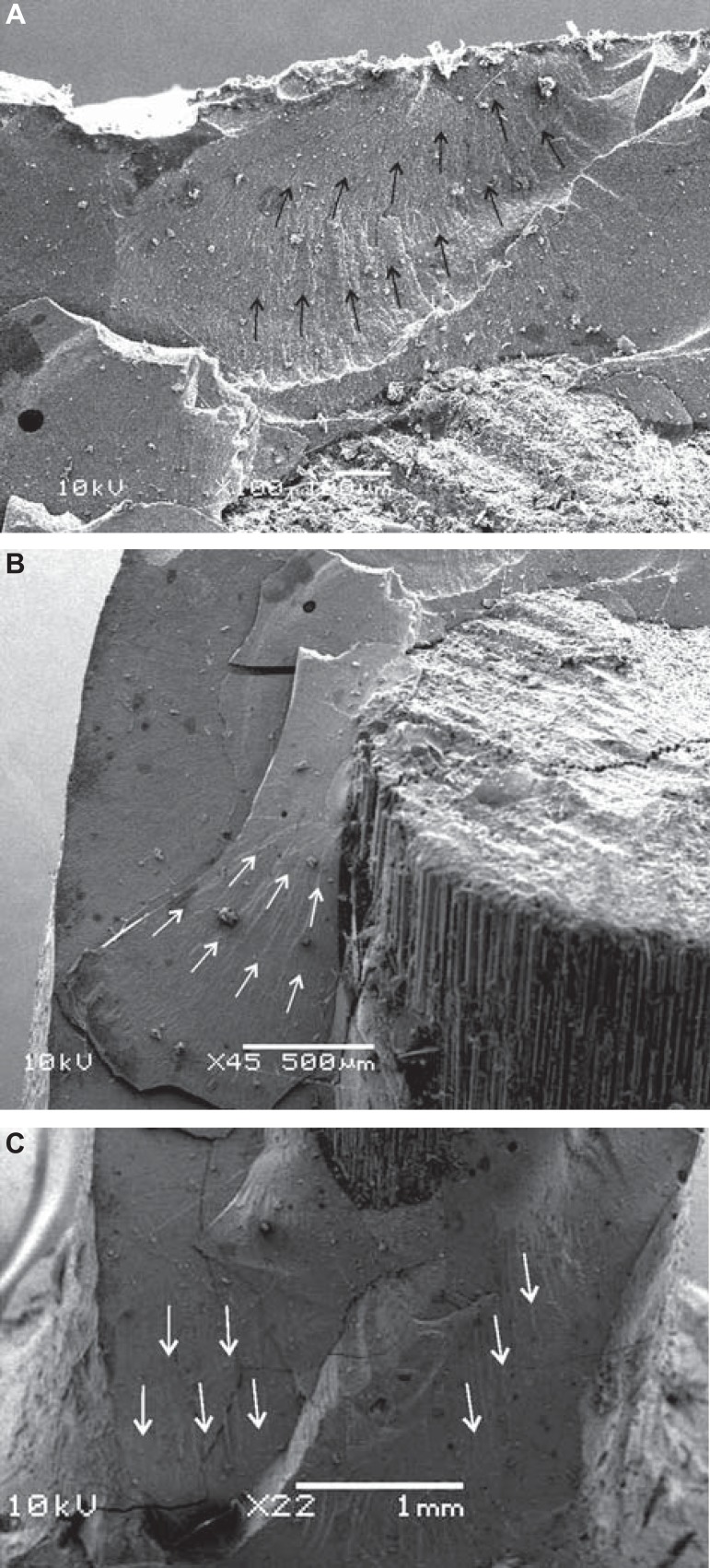
Failures were predominantly in the core in a mesiodistal direction, which can be explained by the loading applied in a 45° angle to the palatal surface. The specimens bend and experience tensile, and compressive stresses that are maximal externally and minimum centrally. Shear stress also acts on the specimens; howewer, it is maximal in the center and minimal in the external portions29. Coronal failures were fractures occurring in the buccal region of the cores with post exposition mesiodistally because of the interaction of tensile, compressive and shear forces. The coronal reconstruction presents a minimal thickness zone of composite resin (Figure 4A), and therefore, the failure tends to initiate in that area (Figure 5A) where tensile stresses are more evident. After failure due to tensile stress, the buccal surface is displaced as a result of the compressive and shear stresses acting on the composite/post interface, and hence, the post becomes exposed (Figure 4B and Figure 5B). Mesiodistal root fractures are also explained by the same failure mechanism (Figure 4C). The beginning and propagation of the fracture are shown in Figure 5B and 5C, respectively.
Figure 4.
(A) Schematic diagram of the specimen positioned for the test, indicating the minimal thickness area (lingual portion) of the core where the fracture initiates. (B) Stereomicroscope representative image of specimen fractured in the mesiodistal direction (group C). (C) Root fracture associated with core fracture (group addition silicone) after the fracture resistance test
Figure 5.
Scanning electron microscopy image of control group. There is displacement of the buccal surface of the core, exposing the post. The fiber post suffers a crack in the mesiodistal direction, which is a consequence of shear stress above the post. (A) Minimal thickness area and hackle lines (black arrows) indicating the start of the fracture. (B) Hackle lines (white arrows) initiating at the composite/post interface. (C) Hackle lines (white arrows) indicated in the buccal surface showing the fracture propagation
For the control group without mechanical cycling, there was a higher number of unfavorable failures than in the other groups. When the roots are embedded directly in acrylic resin, there seems to be a stress concentration on the cervical region of the tooth. On the other side, when periodontal ligament simulation is performed, the stress distribution is altered and, instead of occurring stress concentration on a specific region, tension is distributed along the entire root surface26.
In the present study, polyether and addition silicone were used to reproduce the periodontal ligament, consistent with other studies performing simulation and using similar elastomeric materials10,11,26,27. However, current literature lacks a standardized protocol, and as a result, a wide range of materials, such as condensation silicone23, addition silicone7,22, polysulfide26, polyurethane26,28 and an industrial rubber material20 have been used, as well as other consistencies of the elastomers used in the present study1,26,27. Furthermore, several studies did not indicate the viscosity of the material used10,13,25, while others failed to clearly identify the material comprising the artificial periodontal ligament2. Additional studies assessing the use of diverse materials and different consistencies are recommended.
Bearing in mind the limitations of the present study, the teeth were restored with composite resin cores instead of crowns, which are not consistent with clinical performance; however, without core protection, the condition generated by load application in the adhesive interface is more hostile8, which is an interesting aspect since the present study assessed the bond strength. Also, survival studies, investigation under a longer period of mechanical cycling and fnite element analysis could be interesting options for future studies to assess the long-term behavior of endodontically treated teeth restored with intraradicular posts using different simulated periodontal ligaments. Studies evaluating other types of posts are also recommended to validate the influence of an artificial periodontal ligament on the behavior of endodontically treated teeth.
CONCLUSION
The simulation of the periodontal ligament using elastomeric materials does not affect the bond strength and the fracture resistance of the teeth restored with fiber posts and composite cores, and therefore it may not be necessary to perform periodontal ligament simulation in those tests in the experimental conditions of the study.
References
- 1.Aboushelib MN. Simulation of cumulative damage associated with long term cyclic loading using a multi-level strain accommodating loading protocol. Dent Mater. 2013;29:252–258. doi: 10.1016/j.dental.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 2.Aggarwal V, Singla M, Miglani S, Kohli S. Comparative evaluation of fracture resistance of structurally compromised canals restored with different dowel methods. J Prosthodont. 2012;21:312–316. doi: 10.1111/j.1532-849X.2011.00827.x. [DOI] [PubMed] [Google Scholar]
- 3.Amaral M, Rippe MP, Bergoli CD, Monaco C, Valandro LF. Multistep adhesive cementation versus one-step adhesive cementation: push-out bond strength between fiber post and root dentin before and after mechanical cycling. Gen Dent. 2011;59:e185–e191. [PubMed] [Google Scholar]
- 4.Amaral M, Santini MF, Wandscher V, Amaral R, Valandro LF. An in vitro comparison of different cementation strategies on the pull-out strength of a glass fiber post. Oper Dent. 2009;34:443–451. doi: 10.2341/08-113. [DOI] [PubMed] [Google Scholar]
- 5.Amaral M, Santini MF, Wandscher V, Zogheib LV, Valandro LF. Effect of coronal macroretentions and diameter of a glass-FRC on fracture resistance of bovine teeth restored with fiber posts. Minerva Stomatol. 2009;58:99–106. [PubMed] [Google Scholar]
- 6.Asmussen E, Peutzfeldt A, Sahaf A. Finite element analysis of stresses in endodontically treated, dowel-restored teeth. J Prosthet Dent. 2005;94:321–329. doi: 10.1016/j.prosdent.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Ayad MF, Bahannan SA, Rosenstiel SF. Influence of irrigant, dowel type, and root-reinforcing material on fracture resistance of thin-walled endodontically treated teeth. J Prosthodont. 2011;20:180–189. doi: 10.1111/j.1532-849X.2011.00687.x. [DOI] [PubMed] [Google Scholar]
- 8.Bergoli CD, Amaral M, Boaro LC, Braga RR, Valandro LF. Fiber post cementation strategies: effect of mechanical cycling on push-out bond strength and cement polymerization stress. J Adhes Dent. 2012;14:471–478. doi: 10.3290/j.jad.a28389. [DOI] [PubMed] [Google Scholar]
- 9.Bergoli CD, Lima JM, Melo RM, Bottino MA, Valandro LF. Effect of the interfacial area measurement parameters on the push-out strength between fiber post and dentin. Int J Adhes Adhes. 2014;50:7–10. [Google Scholar]
- 10.Bortoluzzi EA, Souza EM, Reis JM, Esberard RM, Tanomaru-Filho M. Fracture strength of bovine incisors after intra-radicular treatment with MTA in an experimental immature tooth model. Int Endod J. 2007;40:684–691. doi: 10.1111/j.1365-2591.2007.01266.x. [DOI] [PubMed] [Google Scholar]
- 11.Brito-Junior M, Braga NM, Rodrigues DC, Camilo CC, Faria-e-Silva AL. Effect of the simulated periodontal ligament on cast post-and-core removal using an ultrasonic device. J Appl Oral Sci. 2010;18:528–532. doi: 10.1590/S1678-77572010000500017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Camargo CH, Siviero M, Camargo SE, Oliveira SH, Carvalho CA, Valera MC. Topographical, diametral, and quantitative analysis of dentin tubules in the root canals of human and bovine teeth. J Endod. 2007;33:422–426. doi: 10.1016/j.joen.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 13.Clavijo VG, Reis JM, Kabbach W, Silva AL, Oliveira OB, Junior, Andrade MF. Fracture strength of fared bovine roots restored with different intraradicular posts. J Appl Oral Sci. 2009;17:574–578. doi: 10.1590/S1678-77572009000600007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coelho CS, Biff JC, Silva GR, Abrahao A, Campos RE, Soares CJ. Finite element analysis of weakened roots restored with composite resin and posts. Dent Mater J. 2009;28:671–678. doi: 10.4012/dmj.28.671. [DOI] [PubMed] [Google Scholar]
- 15.Erdemir U, Mumcu E, Topcu FT, Yildiz E, Yamanel K, Akyol M. Micro push-out bond strengths of 2 fiber post types luted using different adhesive strategies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:534–544. doi: 10.1016/j.tripleo.2010.05.049. [DOI] [PubMed] [Google Scholar]
- 16.Hohmann A, Kober C, Young P, Dorow C, Geiger M, Boryor A, et al. Influence of different modeling strategies for the periodontal ligament on finite element simulation results. Am J Orthod Dentofacial Orthop. 2011;139:775–783. doi: 10.1016/j.ajodo.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 17.Lanza A, Aversa R, Rengo S, Apicella D, Apicella A. 3D FEA of cemented steel, glass and carbon posts in a maxillary incisor. Dent Mater. 2005;8:709–715. doi: 10.1016/j.dental.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 18.Marchi GM, Mitsui FH, Cavalcanti AN. Effect of remaining dentine structure and thermal-mechanical aging on the fracture resistance of bovine roots with different post and core systems. Int Endod J. 2008;41:969–976. doi: 10.1111/j.1365-2591.2008.01459.x. [DOI] [PubMed] [Google Scholar]
- 19.Mazzoni A, Marchesi G, Cadenaro M, Mazzotti G, Di Lenarda R, Ferrari M, et al. Push-out stress for fibre posts luted using different adhesive strategies. Eur J Oral Sci. 2009;117:447–453. doi: 10.1111/j.1600-0722.2009.00656.x. [DOI] [PubMed] [Google Scholar]
- 20.McLaren JD, McLaren CI, Yaman P, Bin-Shuwaish MS, Dennison JD, McDonald NJ. The effect of post type and length on the fracture resistance of endodontically treated teeth. J Prosthet Dent. 2009;101:174–181. doi: 10.1016/S0022-3913(09)60024-X. [DOI] [PubMed] [Google Scholar]
- 21.Mitsui FH, Marchi GM, Pimenta LA, Ferraresi PM. In vitro study of fracture resistance of bovine roots using different intraradicular post systems. Quintessence Int. 2004;35:612–616. [PubMed] [Google Scholar]
- 22.Nishimura Y, Tsubota Y, Fukushima S. Influence of cyclic loading on fiber post and composite resin core. Dent Mater J. 2008;27:356–361. doi: 10.4012/dmj.27.356. [DOI] [PubMed] [Google Scholar]
- 23.Palamidakis FD, Panou A, Papadokostaki KG, Leontakianakos G, Stathopoulos VN, Kontakiotis EG. Device and materials for in vitro evaluation of forces developed to teeth and periodontal structures during dental practices. J Dent Biomech. 2013;4 doi: 10.1177/1758736013503648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pini M, Wiskott HW, Scherrer SS, Botsis J, Belser UC. Mechanical characterization of bovine periodontal ligament. J Periodontal Res. 2002;37:237–244. doi: 10.1034/j.1600-0765.2002.00344.x. [DOI] [PubMed] [Google Scholar]
- 25.Rosentritt M, Behr M, Scharnagl P, Handel G, Kolbeck C. Influence of resilient support of abutment teeth on fracture resistance of all- ceramic fixed partial dentures: an in vitro study. Int J Prosthodont. 2011;24:465–468. [PubMed] [Google Scholar]
- 26.Soares CJ, Pizi EC, Fonseca RB, Martins LR. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res. 2005;19:11–16. doi: 10.1590/s1806-83242005000100003. [DOI] [PubMed] [Google Scholar]
- 27.Soros C, Zinelis S, Lambrianidis T, Palaghias G. Spreader load required for vertical root fracture during lateral compaction ex vivo: evaluation of periodontal simulation and fracture load information. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e64–e70. doi: 10.1016/j.tripleo.2008.03.027. [DOI] [PubMed] [Google Scholar]
- 28.Sterzenbach G, Kalberlah S, Beuer F, Frankenberger R, Naumann M. In-vitro simulation of tooth mobility for static and dynamic load tests: a pilot study. Acta Odontol Scand. 2011;69:316–318. doi: 10.3109/00016357.2011.563244. [DOI] [PubMed] [Google Scholar]
- 29.Wandscher VF, Bergoli CD, Limberger IF, Ardenghi TM, Valandro LF. Preliminary results of the survival and fracture load of roots restored with intracanal posts: weakened vs non-weakened roots. Oper Dent. 2014;39(5):541–556. doi: 10.2341/12-465. [DOI] [PubMed] [Google Scholar]
- 30.Wiskott HW, Nicholls JI, Belser UC. Stress fatigue: basic principles and prosthodontic implications. Int J Prosthodont. 1995;8:105–116. [PubMed] [Google Scholar]